Abstract
Nurse practitioners and physician assistants can alleviate some of the primary care shortage facing the United States, but their scope-of-practice is limited by state regulation. This study reports both cross-sectional and longitudinal trends in state scope-of-practice regulations for nurse practitioners and physician assistants over a 10-year period. Regulations from 2001 to 2010 were compiled and described with respect to entry-to-practice standards, physician involvement in treatment/diagnosis, prescriptive authority, and controlled substances. Findings indicate that most states loosened regulations, granting greater autonomy to nurse practitioners and physician assistants, particularly with respect to prescriptive authority and physician involvement in treatment and diagnosis. Many states also increased barriers to entry, requiring high levels of education before entering practice. Knowledge of state trends in nurse practitioner and physician assistant regulation should inform current efforts to standardize scope-of-practice nationally.
Keywords: nurse practitioners, physician assistants, primary care, public policy, workforce
Introduction
There is a dearth of primary care providers in the United States, the effects of which may be exacerbated by the Patient Protection and Affordable Care Act, which increases access to health insurance coverage without necessarily increasing the supply of providers (Cassidy, 2013; Christensen, 2013). Indeed, the impact of the primary care shortage in Massachusetts became more salient with the advent of health care reform, as not enough physicians were available to meet the primary care needs of large numbers of newly insured state residents (Fitzgerald, 2013). Primary care serves a variety of functions, including initial diagnosis and evaluation, disease prevention and screening, and ongoing management of chronic conditions. As the point in which most Americans interface with the health care system, primary care plays a prominent role in ensuring access and quality and in promoting lower cost service delivery through the application of preventative medicine and screening.
Increased use of primary care is associated with decreased risk of morbidity and mortality and with reductions in hospitalizations and costs (Cassidy, 2013). However, one in five Americans live in primary care shortage areas, where the ratio of the population to primary care providers is greater than 2,000 to 1 (Bodenheimer & Pham, 2010). Without concerted action, this ratio is unlikely to change in the immediate future. Just 37% of doctors serve in primary care although it accounts for 56% of physician office visits (Health Resources and Services Administration, Bureau of Health Professions, 2008). Furthermore, only one in four medical students is planning a career in primary care (Schwartz, 2012). It is expected that by 2015, the United States will face a shortage of 33,100 primary care practitioners (Association of American Medical Colleges, 2012). The primary care physician workforce is also unevenly distributed. Rural and inner-city areas with high proportions of low income and minority populations, who often have greater health needs, have lower supplies of primary care providers than their higher income, less racially/ethnically diverse counterparts (Goodell, Dower, & O’Neil, 2011). Although there was a slight reduction in regional workforce variation from 1979 to 1999 due to a 51% growth in the aggregate supply per capita, most physicians practiced in regions with an already high supply of doctors (Goodman, 2004).
Using nurse practitioners (NPs) and physician assistants (PAs) to fill the gap between service need and care capacity may alleviate the primary care crisis, as they provide a cost efficient means of supplying much of the hands-on care otherwise provided by better paid, and more highly trained physicians (Cooper, 2007). Nurse practitioners are registered nurses with graduate degrees, who have also completed additional clinical training. In 2010, 84% of NPs had a master’s degree, 4% had a doctorate; the remaining 12% only had a bachelor’s degree, having begun practicing before additional graduate work was required (Health Resources and Services Administration, Department of Health and Human Services, 2010). States license NPs and/or require that they pass a national board certification exam. Physician assistants are part of a physician-led team; thus in contrast to NPs, they rarely practice independently but instead perform tasks delegated by physician supervisors. Forty percent of PAs hold bachelor’s degrees; 43% master’s degrees; the remainder (17%) qualify to practice through on-the-job training or prior experience (Cunningham, 2010). PAs must pass a national certification exam and, like NPs, are licensed by the states (Kaiser Commission on Medicaid and the Uninsured, 2011).
In contrast to physicians, NPs and PAs commonly enter primary care. Estimates vary but suggest that between 52% and 60% of NPs and 43% and 50% of PAs work in primary care (Agency for Healthcare Research and Quality, 2011; American Academy of Nurse Practitioners, 2012; Hooker, 2006). Indeed, rural practices often rely on NPs and PAs in place of physicians, since physicians less commonly elect to work in these otherwise underserved areas (Krein, 1997; Larson, Palazzo, Berkowitz, Pirani, & Hart, 2003). The same is true for nursing homes, community health centers, and other settings where physician presence is more limited (Aigner, Drew, & Phipps, 2004; Bakerjian & Harrington, 2012; Hing, Hooker, & Ashman, 2011; Mezey et al., 2005).
Research confirms that the quality of care provided by NPs is high (Naylor & Kurtzman, 2010). Indeed, patients who receive primary care from NPs are often more satisfied with the care provided than those served by physicians (Horrocks, Anderson, & Salisbury, 2002). Research also suggests that in addition to increasing access to care, PAs provide care comparable in quality to that provided by their physician supervisors (Halter et al., 2013; Hooker & Everett, 2012). Moreover, greater presence of NPs and PAs results in equal or better quality of nursing home care, including fewer potentially avoidable hospitalizations and other favorable outcomes (Aigner et al., 2004; Intrator, Zinn, & Mor, 2004; Xing, Mukamel, & Temkin-Greener, 2013). One study suggests that NPs and PAs contribute to improvements in nursing home quality by providing care that complements rather than substitutes for care provided by physicians (Intrator et al., 2005). Although patients may initially prefer physicians, they often choose an NP or PA rather than wait longer to see a physician. In fact, according to one recent survey, substantial numbers of patients prefer NPs and PAs even when wait time is not a factor (Dill, Pankow, Erikson, & Shipman, 2013). Furthermore, although half of patients surveyed would prefer a physician as their primary care provider, 22% would choose an NP or PA; the remainder indicated no preference. Additionally, results suggest racial/ethnic minorities have more favorable views towards NPs and PAs than their non-Hispanic White counterparts.
Although NPs and PAs are certified nationally, state scope-of-practice laws determine the extent to which they may practice independently. These laws regulate the level of educational attainment needed, the amount of prescriptive authority available, and the level of physician involvement required. Potentially problematic is substantial variability in restrictiveness, “With barriers to full deployment of [NPs/PAs] in some states, full utilization of [NPs/PAs] in others, and many shades in between” (Lugo, O’Grady, Hodnicki, & Hanson, 2010, p. 29). The Institute of Medicine recently called for regulatory standardization (Institute of Medicine, 2010). This recommendation reflects recognition that scope-of-practice legislation in some states is very specific and detailed, while in others it is vague and open to interpretation. It also reflects recognition that some states regularly update their scope-of-practice regulations in light of broader health care system changes but most do not. Of primary concern is that the scope with which NPs and PAs may practice depends largely on idiosyncratic political and regulatory considerations, rather than practitioner ability and education.
Considerable cross-state variation in NP and PA authority makes understanding their potential role in reducing the primary care shortage difficult. Recent calls for regulatory standardization emphasize the need to understand the variety of practice regulations, their impact on health system performance, and their effects on patient access and quality (Dentzer, 2010; Institute of Medicine, 2010; Naylor & Kurtzman, 2010). Before such standardization can take place, however, it is necessary to document the evolution of the regulatory landscape. The purpose of this article, therefore, is to describe trends in state regulation of NPs and PAs during the 2000s.
New Contribution
The literature on NP and PA regulations across states and over time is limited and incomplete. “No single source provides an accounting of the changes in NP and PA authority,” according to Perry (2009, p. 493). Several studies have synthesized state NP regulations but focus only on individual years and/or a limited range of regulatory characteristics. Cassidy (2013) used data from the 2012 Pearson Report (which catalogs NP regulations by state) to present NP regulations in that year, as part of a discussion of proposals to increase NP authority intended to reduce the primary care shortage. Lugo et al. (2010) used the 2007 Pearson Report and found that states that had only the state’s Board of Nursing as a regulator granted NPs more authority than states where the Board of Nursing shared regulatory authority with other groups (usually physician led). Kaas et al. (2002) consulted each state’s Board of Nursing to characterize NP regulations in 2001. They found that many states had recently broadened NPs’ scope-of-practice, specifically granting greater prescriptive authority. Traczynski and Udalova (2013) examined NP regulations over time, specifically those addressing NP ability to practice without physician oversight, and found that in states that allow independent NP practice there were more frequent routine checkups and less emergency room usage. The authors attribute these positive outcomes to decreased administrative burden that comes from physician/NP interaction, as well as to decreased costs to patients from accessing medical care.
Other studies look at the relationship between state NP regulation and various labor market outcomes but, again, only for individual years and/or a limited range of regulatory characteristics (Kuo, Loresto, Rounds, & Goodwin, 2013; Reagan & Salsberry, 2013). Reagan and Salsberry (2013), for example, used the 2008 Pearson Report to look at the relationship between state regulations and growth in the NP workforce. Kuo et al. (2013) used Pearson data from 1998 to 2012 to examine the relationship between NP regulation of independent practice and/or prescription authority and receipt of primary care from NPs by Medicare beneficiaries, finding that beneficiaries residing in less restrictive states had a greater likelihood of receiving care from NPs. Because state NP regulations were classified into three general levels of restrictiveness, detailed information on state regulation of NPs was not reported.
Research on PA regulations is especially limited. One exception is a study by Larson and Hart (2007), which examined PA demographics and entry-to-practice regulations from 1967 to 2000. Results indicate that PAs were increasing in number, increasingly female, and increasingly subject to more stringent educational requirements. Few investigations examined trends in both NP and PA regulations (Dueker, Jacox, Kalist, & Spurr, 2007; Perry, 2009), and in few instances is detailed information regarding specific regulations provided. Wing, Salsberg, and Continelli (2002) are an exception. This thorough examination of NP and PA regulations across states over the 1990s found that NP and PA scope-of-practice increased over the 1990s, as did their use. Our article continues in this vein, examining both NP and PA regulations across all states, over an extended time period, the decade following that reported in the Wing article (2001–2010), and across multiple dimensions of regulation.
We assume that NP and PA scope-of-practice laws, if liberalized, would increase entry-to-practice, with positive benefits for patient outcomes. Thus, it is expected that providing NPs and PAs with increased prescriptive authority and the ability to practice with reduced levels of physician involvement should both enhance their ability to provide care and draw additional entrants into the field, thereby improving patient access to primary care.
It is possible that concomitant adoption of more stringent educational requirements could, over the short term, serve as a barrier to aspiring NPs and PAs, thereby, reducing entry-to-practice, with adverse implications for patient access. On the other hand, since demand for professional services and inability of the medical profession to supply the demand has contributed to the development of the NP and PA professions (Aigner et al., 2004; Bakerjian & Harrington, 2012; Hing et al., 2011; Krein, 1997; Larson et al., 2003; Mezey et al., 2005), it is possible that in the future there could be graded levels of these midlevel professionals, akin to the distinction between associates degree-level physical/occupational therapy assistants from doctoral-level physical/occupational therapists.
Method
Data
Data on state NP and PA regulations were compiled from 2001 to 2010. Data on state NP regulations derive from the Pearson Report (Pearson, 2003, 2009), published annually by the Nurse Practitioner journal and the American Journal of Nurse Practitioners. However, the Pearson Report was not published in 2010, so regulations were abstracted from the websites of individual states to obtain the data for that year. Data on state PA regulations derive from the “State Regulation of Physician Assistant Practice” report, published annually by the American Academy of Physician Assistants (AAPA; 2010). Because AAPA did not publish this report in 2009, state laws were abstracted from individual state websites to complete the time series. From these sources, dimensions of state regulation were chosen that captured variability in state regulatory practice in quantifiable ways and were available for/applicable to both NPs and PAs, across each of the years analyzed. These include entry-to-practice qualifications, physician involvement in treatment and diagnosis, and prescriptive authority.
Measurement
Entry-to-Practice Qualifications
An entry-to-practice variable was created for both NP and PA data. For NPs, entry-to-practice qualifications included a bachelor of science in nursing, and/or master of science in nursing degree, and/or maintenance of national certification. For PAs, entry-to-practice qualifications included passing the National Commission on Certification of Physician Assistants exam and completion of an accredited PA program and either a bachelor of science or a master of science degree.
Physician Involvement in Treatment/Diagnosis
For NPs, physician involvement in treatment/diagnosis was assessed in two steps; first, whether or not a relationship with a physician was required for treatment and diagnosis, and, if so, the nature of that involvement. Physician involvement was always required for PA practice, though its specific nature was specified as well.
Physician involvement was categorized as collaboration, delegation, direction, or supervision. These four terms were chosen because they were used in the Pearson Report starting in 2005 to describe the types of relationships required between NPs and physicians, both for purposes of general practice and for purposes of making prescriptions. However, the Pearson Report from 2001 through 2004 and the AAPA document did not report these categorizations, but instead reported excerpts from the pertinent legislation from each state. In order to make the data consistent and quantifiable, we coded the legislation for NPs from 2001 to 2004 (and for the year the Pearson Report was not published, 2010) and for PAs from 2001 to 2010 into these four categories. Although the Pearson Report applied these four terms in later years, they did not provide operational definitions. Definitions were instead derived from the Federation of State Medical Boards (FSMB, 2005) and from articles on scope-of-practice (American Academy of Family Physicians [AAFP], 2014; Klein, 2005). The definitions, which were consistent across the sources consulted, were then applied to the 2001 to 2004 Pearson Report, the 2001 to 2010 AAPA documents, and directly to state NP legislation in 2010, based on the language of the legislation that was provided.
The operational definitions for the four categories of physician involvement are defined as follows:
Collaboration occurs when “physicians and other health care practitioners plan and practice together as colleagues, working interdependently within the boundaries of their scopes of practice” (FSMB, 2005, p. 18).
Delegation occurs when physicians permit specific functions to be performed, as long as such functions are within the scope-of-practice of the practitioner to whom those functions are assigned (Klein, 2005).
Direction refers to the responsibility of physicians to “ensure that appropriate directions are given, understood, and executed. These directions may take the form of written protocols, in person, over the phone, or by some other means of electronic communication” (AAFP, 2014). These protocols describe practitioner roles and responsibilities, including actions that can be undertaken by the NP/PA in “commonly encountered clinical situations and, especially, under what circumstances physician consultation is to be immediately obtained” (AAFP, 2014).
Supervision specifies that the physician “direct and review the work, records, and practice of the [practitioner] on a continuous basis to ensure that appropriate directions are given and understood and that appropriate treatment is rendered consistent with applicable state law” (AAFP, 2014), which includes regular practice and chart review, continuous availability of communication, emergency planning, and a plan for controlled substance prescribing and formulary compliance (AAFP, 2014).
Prescriptive Authority
For both NPs and PAs, physician involvement in prescriptions was assessed; first, whether or not a physician was required for prescribing medications, and, if so, the nature of that involvement (collaboration, delegation, direction, or supervision). In addition to the four categories of involvement in treatment and diagnosis, prescriptive authority was described using two additional categories: “minimal” and “authorization.” Authorization means that a drug may be prescribed if explicit permission is granted by the involved physician, while minimal means that physicians must be involved in prescription in an unspecified but nominal way (FSMB, 2005). It was also determined whether or not NPs and PAs could prescribe controlled substances and, if so, the schedules allowed (II–V). According to the Drug Enforcement Agency Office of Diversion Control (2012), Schedule I substances have high potential for abuse and have no accepted medical use in treatment in the United States (i.e., heroin, LSD, ecstasy). Schedule II substances have high potential for abuse, which can lead to severe dependence (i.e., morphine, opium, amphetamine). Schedule III substances have a lesser potential for abuse but may lead to high psychological dependence or moderate or low physical dependence (i.e., Vicodin, Tylenol with codeine, ketamine, anabolic steroids). Schedule IV substances have lower potential for abuse than III (i.e., Xanax, Valium, Ativan). Schedule V substances have low potential for abuse and contain limited narcotics (i.e., cough preparations with codeine).
Analysis
State regulations were coded from the Pearson and “State Regulation of Physician Assistant Practice” reports, as well as directly from state websites. State regulations for NPs and PAs in 2010 are presented in depth to provide detailed description of the regulatory landscape at the end of the decade analyzed. This is followed by identification of all states making particular changes in the regulation of NPs and PAs between 2001 and 2010. Scatter plots are also presented that describe the number of states employing different types of state regulations over time.
Results
State Regulation in 2010
Nurse Practitioners
Table 1 reports state regulation of NPs as of 2010. Forty-two states stipulated that NPs have master’s degrees in nursing and retain national certification in order to practice. The remainder required either a more general Master’s degree or national certification alone. Twenty-four states granted NPs the authority to practice without physician involvement in diagnosis and treatment. The remainder required that NPs work with physicians, most commonly, collaboratively (18 states). Very few states required delegation of duties (three states) or supervision (four states) of NPs by physicians.
Table 1.
Nurse Practitioner Regulations, 2010.
| State | Entry-to-practice | MD required for diagnosis/treatment | Nature | MD involvement in NP Rx | Nature | Controlled substances Rx authorization | Schedules allowed |
|---|---|---|---|---|---|---|---|
| AL | MSN, NC | Y | CO | Y | CO | N | NA |
| AK | MSN, NC | N | — | N | — | Y | II–V |
| AZ | MSN, NC | N | — | N | — | Y | II–V |
| AR | MSN for ANP, NC | Y | CO | Y | CO | Y | III–V |
| CA | POST, C, and MSa | Y | CO | Y | AU | Y | II–V |
| CO | POSTb, NC | N | — | N | — | Y | II–V |
| CT | MSN, NC | Y | CO | Y | CO | Y | II–V |
| DE | MSN or POST, NC | Y | CO | Y | CO | Y | II–V |
| DC | NC | N | — | N | — | Y | II–V |
| FL | MSN, NC | Y | SU | Y | SU | N | NA |
| GA | MSN, NC | Y | DE | Y | DE | Y | III–V |
| HI | MSN or NCc | N | — | Y | CO | Y | II–V |
| ID | NC | N | — | Y | MI | Y | II–V |
| IL | MSN, NC | Y | CO | Y | AU | Y | III–V |
| IN | MSN or NC | Y | CO | Y | CO | Y | II–V |
| IA | MSN, C | N | — | N | — | Y | II–V |
| KS | MSN | Y | CO | Y | SU | Y | II–V |
| KY | MSNd, NC | N | — | Y | CO | Y | II–V |
| LA | MSN, NC | Y | CO | Y | DI | Y | II–V |
| ME | MSNe, NC | Nf | — | Ng | — | Y | II–V |
| MD | NC | Y | CO | Y | AU | Y | II–V |
| MA | MS, NC | Y | DI | Y | SU | Y | II–V |
| MI | MSN, NC | N | — | Y | DE | Y | II–V |
| MN | NC | Y | CO | Y | DE | Y | II–V |
| MS | MSN, NC | Y | CO | Y | CO | Y | II–V |
| MO | MSN, NC | Y | DE | Y | DE | Y | III–V |
| MT | MSN, NC | N | — | N | — | Y | II–V |
| NE | MSN, NC | Y | CO | Y | CO | Y | II–V |
| NV | MSNh | Y | CO | Y | CO | Y | II–V |
| NH | MSNi, NC | N | — | N | — | Y | II–V |
| NJ | MSN, NC | N | — | Y | CO | Y | II–V |
| NM | MSN, NC | N | — | N | NA | Y | II–V |
| NY | NA | Y | CO | Y | CO | Y | II–IV |
| NC | MSN, NC | Y | SU | Y | CO | Y | II–V |
| ND | MSN | N | — | N | — | Y | II–V |
| OH | MSN, NC | Y | CO | Y | CO | Y | II–V |
| OK | MSNj, NC | N | — | Y | SU | Y | III–V |
| OR | MSN | N | — | N | — | Y | II–V |
| PA | MSNk, NC | Y | CO | Y | CO | Y | II–IV |
| RI | MSN, NC | N | — | N | — | Y | II–V |
| SC | MSN, NC | Y | SU | Y | SU | Y | III–V |
| SD | MSN, NC | Y | CO | Y | CO | Y | II–V |
| TN | MSNl, NC | N | — | Y | SU | Y | II–V |
| TX | MSN, NC | Y | DE | Y | DE | Y | III–V |
| UT | MSN, NC | N | — | Y | SU | Y | II–V |
| VT | MSN, NC | N | — | Y | CO | Y | II–V |
| VA | MSN, NC | Y | CO | Y | SU | Y | II–V |
| WA | MSNm, NC | N | — | N | — | Y | II–V |
| WV | MSN, NC | N | — | Y | CO | Y | III–V |
| WI | MSN, NC | Y | SU | Y | CO | Y | II–V |
| WY | MSN, NC | N | — | N | — | Y | II–V |
Note. Y = yes; N = no; CO = collaboration; DE = delegation; SU = supervision; DI = direction; MI = minimal; AU = authorization; NC = national certification; SC = state certification; C = certification (where jurisdiction not specified); MSN = masters of science in nursing or advanced practice nursing, POST = postbasic program.
MS after January 2008.
Postbasic program after July 1, 2008.
MSN for prescription, MSN or national certification for practice.
MSN after January 2005.
MSN after January 1, 2006.
No MD involvement after first 2 years of practice, supervision until.
No MD involvement after first 2 years of practice, direction until.
MSN after June 2005. National certification if no BSN or MSN before June 2005.
MSN after July 1, 2004.
MSN for prescription.
MSN after February 2005.
MSN after July 2006.
MSN after January 1, 1995.
Of the states that did not allow NPs to practice independently, most required physician involvement or oversight of NP prescriptive authority. Most commonly, this relationship was collaborative (19 states), though some required direction (1 state, Alabama), delegation (5 states), supervision (8 states), or outright authorization (3 states). All states except Florida and Alabama allowed NPs to prescribe controlled substances II through V in 2010.
Physician Assistants
Table 2 reports state regulation of PAs in 2010. All states except Minnesota and North Dakota required PAs to complete an accredited PA program and pass the National Commission on Certification of Physician Assistants exam. Some states required a bachelor’s degree as well (eight states). Just four states (Mississippi, Missouri, Ohio, and West Virginia) required a master’s degree. Physician supervision of diagnosis and treatment of patients was required in all states except Alaska (which required collaboration). All states allowed PAs to prescribe as long as a physician was directly involved, most commonly through delegation (19 states) and authorization (18 states). Many states specified a physician be involved in a supervisory nature (13 states); only Arizona specified collaboration. Most states allowed PAs to prescribe controlled substances, typically schedules II through V (34 states) or III through V (15 states).
Table 2.
Physician Assistant Regulations, 2010.
| State | Entry-to-practice | MD required for practice | Nature | MD involvement in PA Rx | Nature | Controlled substances Rx authorization | Schedules allowed |
|---|---|---|---|---|---|---|---|
| AL | ACC, EX | Y | SU | Y | AU | Y | III–V |
| AK | ACC, EX | Y | CO | Y | DE | Y | II–V |
| AZ | ACC, EX | Y | SU | Y | CO | Y | II–V |
| AR | BS, ACC, EX | Y | SU | Y | DE | Y | III–V |
| CA | ACC, EX | Y | SU | Y | DE | Y | II–V |
| CO | ACC, EX | Y | SU | Y | DE | Y | II–V |
| CT | BS, ACC, EX | Y | SU | Y | DE | Y | II–V |
| DE | ACC, EX | Y | SU | Y | SU | Y | II–V |
| DC | ACC, EX | Y | SU | Y | SU | Y | II–V |
| FL | ACC, EX | Y | SU | Y | AU | N | — |
| GA | ACC, EX | Y | SU | Y | DE | Y | III–V |
| HI | ACC, EX | Y | SU | Y | SU | Y | III–V (II in hospitals) |
| ID | BS, ACC, EX | Y | SU | Y | SU | Y | II–V |
| IL | ACC, EX | Y | SU | Y | DE | Y | II–V |
| IN | ACC, EX | Y | SU | Y | DE | Y | III–V (II in emergency) |
| IA | ACC, EX | Y | SU | Y | SU | Y | III–V (and II stimulants) |
| KS | ACC, EX | Y | SU | Y | AU | Y | II–V |
| KY | ACC, EX | Y | SU | Y | DE | N | — |
| LA | ACC, EX | Y | SU | Y | DE | Y | III–V |
| ME | ACC, EX | Y | SU | Y | SU | Y | III–V (II with AU) |
| MD | BSa, ACC, EX | Y | DE | Y | DE | Y | II–V |
| MA | BS, ACC, EX | Y | SU | Y | SU | Y | II–V |
| MI | ACC, EX | Y | SU | Y | DE | Y | III–V (II if 7 day supply at discharge) |
| MN | EX, AGREE | Y | SU | Y | AU | Y | II–V |
| MS | MSb, ACC, EX | Y | SU | Y | AU | Y | II–V |
| MO | MSc, ACC, EX | Y | SU | Y | AU | Y | III–V |
| MT | ACC, EX | Y | SU | Y | DE | Y | II–V |
| NE | ACC, EX | Y | SU | Y | DE | Y | II–V |
| NV | ACC, EX | Y | SU | Y | AU | Y | II–V |
| NH | ACC, EX | Y | SU | Y | DE | Y | II–V |
| NJ | ACC, EX | Y | SU | Y | DE | Y, if AU | II–V |
| NM | ACC, EX | Y | SU | Y | DI | Y | II–V |
| NY | ACC, EX | Y | SU | Y | SU | Y | II–V |
| NC | ACC, EX | Y | SU | Y | SU | Y | II–V |
| ND | EX | Y | SU | Y | DE | Y | II–V |
| OH | MSd, ACC, EX | Y | SU | Y | AU | Y | III–V |
| OK | ACC, EX | Y | SU | Y | AU | Y | III–V (II if DE) |
| OR | ACC, EX | Y | SU | Y | AU | Y | II–V |
| PA | BS, ACC, EX | Y | SU | Y | AU | Y | II–V |
| RI | ACC, EX | Y | SU | Y | SU | Y | II–V |
| SC | ACC, EX | Y | SU | Y | AU | Y | III–V |
| SD | ACC, EX | Y | SU | Y | AU | Y | II–V |
| TN | ACC, EX | Y | SU | Y | AU | Y | II–V |
| TX | ACC, EX | Y | SU | Y | AU/DE | Y | III–V |
| UT | ACC, EX | Y | DE | Y | AU | Y | II–V |
| VT | ACC, EX | Y | SU | Y | AU | Y | II–V |
| VA | ACC, EX | Y | SU | Y | SU | Y | II–V |
| WA | ACC, EX | Y | SU | Y | SU | Y | II–V |
| WV | BS or MS, ACC, NCCPA | Y | SU | Y | AU | Y | III–V |
| WI | ACC, EX | Y | SU | Y | SU | Y | II–V |
| WY | ACC, EX | Y | SU | Y | DE | Y | II–V |
Note. Y = yes; N = no; CO = collaboration; DE = delegation; SU = supervision; DI = direction; MI = minimal, AU = authorization; ACC = accredited; PA = program; EX = NCCPA exam; BS = bachelor of science; MS = masters of science; AGREE = MD/PA practice agreement.
BS required after October 1, 2003.
BS through 2004, MS starting in 2005.
MS after January 1, 2008.
MS after January 1, 2008.
Changes in State Regulation
Nurse Practitioners
Table 3 summarizes changes in state regulation of NPs between 2001 and 2010. Four states—Arkansas, Colorado, New Hampshire, and Tennessee—increased training requirements, requiring an MSN to enter practice during this time period. Ten states loosened requirements for physician involvement in diagnosis and treatment. Arizona, Colorado, Hawaii, Idaho, Michigan, Rhode Island, Washington, and Wyoming went from requiring collaborative relationships between NPs and physicians to requiring no physician involvement at all. California and South Carolina lowered the level of physician involvement from supervision to collaboration.
Table 3.
Changes in Nurse Practitioner Regulations From 2001 to 2010.
| Change | State | Year of change |
|---|---|---|
| Entry-to-practice requirement | ||
| Began requiring an MSN | Arkansas | 2003 |
| Colorado | 2008 | |
| New Hampshire | 2004 | |
| Tennessee | 2006 | |
| Physician involvement | ||
| Collaborative relationship to no relationship | Arizona | 2006 |
| Colorado | 2010 | |
| Hawaii | 2005 | |
| Idaho | 2005 | |
| Michigan | 2005 | |
| Rhode Island | 2009 | |
| Washington | 2006 | |
| Wyoming | 2006 | |
| Supervision to collaboration | California | 2007 |
| South Carolina | 2006 | |
| Prescriptive authority | ||
| No prescription of controlled substances to schedules III–V | Georgia | 2007 |
| Missouri | 2009 | |
| Texas | 2003 | |
| No prescription of controlled substances to schedules II–V | Hawaii | 2009 |
| Kentucky | 2007 | |
| Virginia | 2002 = IV–V, 2003 = III–V, 2007 = II–V | |
| Schedules III–V to II–V | Louisiana | 2006 |
| Maine | 2002 | |
| Ohio | 2002 | |
| Schedule V to III–V | South Carolina | 2004 |
Ten states increased the prescriptive authority of NPs between 2001 and 2010. Georgia, Missouri, and Texas moved from not allowing NPs to prescribe controlled substances to allowing prescription of schedules III through V, while Hawaii, Kentucky, and Virginia moved from no controlled substance prescription to permitting prescription of schedules II through V. Louisiana, Maine, and Ohio loosened controlled substance regulations from III through V to II through V, and South Carolina from just schedule V to schedules III through V.
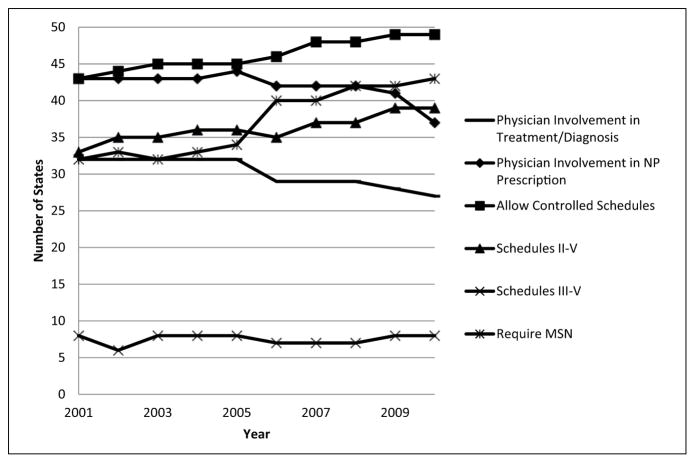
Figure 1 characterizes NP regulation across states over the 10 years examined. Over the decade, fewer states required physician involvement in treatment and diagnosis (32 states in 2001 to 27 states in 2010), be it through supervision (8 to 4), collaboration (3 to 29), direction (1 across the decade), or delegation (4 to 3). There was a decrease in the number of states that required physician involvement in NP prescription over the 10 years (from 43 states to 37 states), while the number of states allowing the prescription of controlled substances increased (from 43 to 49), and specifically the number of states allowing schedules II through V (33 to 39). The number of states allowing schedules III through V was consistent across years (eight states). There was a substantial increase in the number of states that required an MSN of NPs (32 states in 2001 to 43 states in 2010).
Figure 1.
Number of states characterized by a specific nurse practitioner regulation from 2001 to 2010.
Physician Assistants
Table 4 summarizes changes in state regulation of PAs between 2001 and 2010. Two states—Maryland and Pennsylvania—began requiring a BS in order to enter practice during the years examined; three states—Mississippi, Missouri, and Ohio—began requiring an MS. No state changed the level of physician involvement required for practice.
Table 4.
Changes in Physician Assistant Regulations from 2001 to 2010.
| Change | State | Year of change |
|---|---|---|
| Entry-to-practice requirement | ||
| Began requiring a BS | Maryland | 2003 |
| Pennsylvania | 2004 | |
| Began requiring an MS | Mississippi | 2005 |
| Missouri | 2008 | |
| Ohio | 2008 | |
| Prescriptive authority | ||
| No prescription of controlled substances to schedules III–V | Alabama | 2010 |
| Indiana | 2007 | |
| Louisiana | 2004 | |
| Missouri | 2010 | |
| Ohio | 2006 | |
| Texas | 2003 | |
| No prescription of controlled substances to schedules II–V | Mississippi | 2005 |
| New Jersey | 2005 | |
| Washington, D.C. | 2007 | |
| Schedules III–V to II–V | Alaska | 2003 |
| Idaho | 2002 | |
| Illinois | 2010 | |
| New York | 2008 | |
| Oregon | 2004 | |
| Pennsylvania | 2007 | |
| Schedule V to III–V | South Carolina | 2006 |
| Schedule V to II–V | Virginia | 2003 = IV–V, 2004 = III–V, 2007 = II–V |
Seventeen states increased the prescriptive authority of PAs between 2001 and 2010. Alabama, Indiana, Louisiana, Missouri, Ohio, and Texas moved from not allowing PAs to prescribe controlled substances to allowing the prescription of schedules III through V, while Mississippi, New Jersey, and Washington, D.C., went from no controlled substance prescription to permitting prescription of schedules II through V. Alaska, Idaho, Illinois, New York, Oregon, and Pennsylvania loosened regulations from III through V to II through V, South Carolina from schedule V to III through V and Virginia from schedule V to II through V.
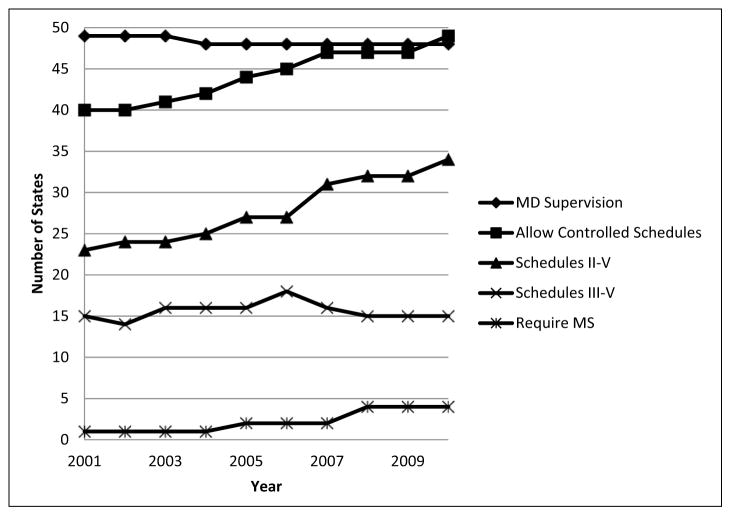
Figure 2 characterizes PA regulation across states over the decade examined. Because a relationship with a physician is a requirement of PA practice, there were little changes in the different relationships with physicians required—virtually all required supervision, except Alaska, which required collaboration from 2001 to 2010, Utah, which required delegation from 2001 to 2010, and Maryland, which started requiring delegation in 2004. The largest change in PA regulation was the increase in the number of states that allowed the prescription of controlled substances (40 states to 49 states between 2001 and 2010). There was also a substantial increase in the number of states that allowed the prescription of schedules II through V (from 23 states in 2001 to 34 in 2010), while the number of states allowing PAs to prescribe schedules III through V remained steady (at 15). There was little change in the educational requirements of PAs from 2001 to 2010, although there was a slight trend toward more stringent requirements. As evidenced by the figure, just one state (West Virginia) required an MS in 2001, two states (West Virginia and Mississippi) required an MS as of 2005, and four states (West Virginia, Mississippi, Missouri, and Ohio) required an MS as of 2008.
Figure 2.
Number of states characterized by a specific physician assistant regulation from 2001 to 2010.
Discussion
This study was among the first to systematically examine trends in state regulation of the two most commonly used nonphysician practitioner groups, NPs and PAs, since 2000. Results indicated that by 2010, Alaska, Iowa, Montana, New Hampshire, New Mexico, Oregon, and Washington, D.C., were the least restrictive in regulating NPs, and at no point during the years studied required a relationship with a physician in order for NPs to practice. By contrast, Alabama and Florida were most restrictive: never permitting NPs to prescribe controlled substances. Alaska, as the only state to require collaboration with a physician (as opposed to direction, supervision, or delegation), was the least restrictive in regulating PAs. Florida, Kentucky, and Missouri, as the only states never permitting PAs to prescribe controlled substances, were most restrictive.
Results extend the findings of Wing et al. (2002), who found scope-of-practice expansions for NPs and PAs during the 1990s. Between 2001 and 2010 states loosened regulations and granted greater authority for both NPs and PAs. At the same time, many states increased entry-to-practice requirements. Institution of more stringent educational requirements of NPs and PAs may improve quality and efficiency, while increased practice authority may facilitate greater use of NPs and PAs as a strategy for addressing the primary care gap facing the nation. Since this gap is expected to grow as health insurance coverage becomes more widely available, monitoring the regulatory trends in NP and PA practice is important.
This study demonstrates that NP and PA regulations have varied widely across states and over time. This variation permits studies that assess the impact of state policies affecting NP and PA practice on patient access, cost, and quality. Such studies are needed in order to understand how to best shape regulations to achieve better patient care. Some research along this line has already been conducted; for example, previous research suggests that states with restrictive NP regulations had lower rates of NP workforce growth (Reagan & Salsberry, 2013), whereas states with less restrictive regulations had more patients who received primary care from NPs (Kuo et al., 2013).
Additionally, research has examined labor market impacts of NP regulation. One study using Current Population Survey data found that in states where NPs had higher levels of autonomy, physicians and NPs earned less, while PAs earned more (Dueker et al., 2005). The authors hypothesized that this happens because when NPs were granted high levels of autonomy, physicians were less likely to hire them and more likely to hire PAs because they did not want to share responsibility for providing care with NPs. On the other hand, PAs were more likely to be hired as they are required to be under the supervision of a physician. Other research, also relying on nationally representative data sources, found that greater NP authority increases NP income, reduces physician income, and has a differential impact on PA income (Perry, 2009). In contrast, increased PA authority had little effect on PA income but was associated with reduced NP and increased physician income. Importantly, cross-state variation may impact overall system performance to the extent that states with more stringent regulations do not benefit as much from the high quality, low cost care that NPs and PAs provide (Pohl, Hanson, Newland, & Cronenwett, 2010; Nelson, 2012).
It is important to note that the extent to which NPs and PAs provide patient care depends, in part, on factors other than scope-of-practice, including, for example, the impact of insurance reimbursement practices on provider income. Future research should consider the relative importance of NP and PA reimbursement, scope-of-practice, and other considerations in impacting both the attractiveness of entering the profession to potential NPs and PAs, as well as the extent to which NPs and PAs can be used to meet national needs. It may be the prevailing mix of payment and regulation that results in differential use of NPs and PAs across states, and that keeps NPs and PAs from practicing up to their fullest potential in helping to meet the nation’s primary care needs.
This research has several limitations. The regulation of NPs and PAs differs, and as a consequence, the information available for the two varies somewhat, with, for example, participation in an accredited program being a dimension of PA but not NP regulation. Differences such as this preclude uniform apple-to-apple comparisons of state regulatory regimes toward NPs and PAs. Another limitation of this research is that the Pearson Report was not published in 2010 and the “State Regulation of Physician Assistant Practice” was not published in 2009, which meant that it was necessary to examine the regulations of individual states in order to fill in the gaps. This was problematic because the published reports presented regulations in consistent, and thus comparable and more quantifiable ways, but the laws and regulations the reports were abstracted from were less clear and easily interpretable. It is possible that the compilers of these reports and the authors of this article interpreted specific laws in different ways.
Nevertheless, the data reported in this article present a detailed picture of how state practice regulations developed during the first decade of the 21st century. It provides researchers with a more nuanced sense of regulatory change than the older, more limited data used in prior investigations. The current data are also important because they permit a better understanding of the different regulations of NPs and PAs. Future research could use this information to develop an overall measure of regulatory stringency which can be tracked over time. Research could also use this information to better understand the political, economic, social, and programmatic factors that result in the adoption of specific NP and PA regulations, or changes in overall regulatory stringency, across states over time. This would result in a better understanding of the characteristics of states that lead to more or less restrictive regulatory policies affecting the use of NPs and PA. The great deal of regulatory variability described in this study could also be used to study relationships among overall regulatory stringency and specific state regulations, the primary care workforce, and other indicators of system performance such as cost, quality, and access. Results from these studies could inform policy about best practices, with respect to regulatory regimes that lead to the most desirable outcomes, including closing the gap between demand and supply in primary care.
Conclusion
This study is among the first to address state regulations of the two most common nonphysician primary care provider groups: nurse practitioners and physician assistants, and also among the first to include all states over a 10-year period for purposes of examining trends in this area. Overall, results reveal movement toward less restrictive regulations and higher entry-to-practice requirements for both NPs and PAs. Variability across states was large, and this has been found in previous studies to have significant labor market impacts. It is important to continue to study why states make regulatory changes such as those seen from 2001 to 2010, and if those changes achieve what they are intended to achieve. Knowledge of state trends in NP and PA regulation and their impact should, in turn, inform current efforts to standardize scope-of-practice nationally.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a National Institute on Aging Program Project titled “Shaping Long Term Care in America” (NIA 1P01 AG027296-01A1).
Footnotes
This work was done while Dr. Intrator was an associate professor (research) at Brown University School of Public Health.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency for Healthcare Research and Quality. The number of nurse practitioners and physician assistants practicing primary care in the United States: Primary care workforce facts and stats no. 2. 2011 Retrieved from http://www.ahrq.gov/research/findings/factsheets/primary/pcwork2/index.html.
- Aigner MJ, Drew S, Phipps J. A comparative study of nursing home resident outcomes between care provided by nurse practitioners/physicians versus physicians only. Journal of the American Medical Directors Association. 2004;5(1):16–23. [PubMed] [Google Scholar]
- American Academy of Family Physicians. Guidelines on the supervision of certified nurse midwives, nurse practitioners and physician assistants. 2014 Retrieved from http://www.aafp.org/about/policies/all/guidelines-nurses.html.
- American Academy of Nurse Practitioners. AANP membership survey report. 2012 doi: 10.1111/j.1745-7599.2009.00456.x. Retrieved from https://www.aanp.org/images/documents/research/2012%20membership%20survey%20report.pdf. [DOI] [PubMed]
- American Academy of Physician Assistants. State regulation of physician assistant practice. Alexandria, VA: Author; 2010. [Google Scholar]
- Association of American Medical Colleges. Physician workforce policy recommendations. Washington, DC: Author; 2012. [Google Scholar]
- Bakerjian D, Harrington C. Factors associated with the use of advanced practice nurses/physician assistants in a fee-for-service nursing home practice: A comparison with primary care physicians. Research in Gerontological Nursing. 2012;5:163–173. doi: 10.3928/19404921-20120605-01. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Pham HH. Primary care: Current problems and proposed solutions. Health Affairs. 2010;29:799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- Cassidy A. Health policy brief: Nurse practitioners and primary care (updated) Health Affairs. 2013 May 15; Retrieved from http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=92.
- Christensen J. Doctor shortage, increased demand could crash health care system. 2013 Oct 2; Retrieved from http://www.cnn.com/2013/10/02/health/obamacare-doctor-shortage/
- Cooper RA. New directions for nurse practitioners and physician assistants in the era of physician shortages. Journal of the Association of American Medical Colleges. 2007;82:827–828. doi: 10.1097/ACM.0b013e31812f7939. [DOI] [PubMed] [Google Scholar]
- Cunningham R. Tapping the potential of the health care workforce: Scope-of-practice and payment policies for advanced practice nurses and physician assistants (Background Paper No. 76) Washington, DC: National Health Policy Forum; 2010. Jul 6, [Google Scholar]
- Dentzer S. Geisinger chief Glenn Steele: Seizing health reform’s potential to build a superior system. Health Affairs (Project Hope) 2010;29:1200–1207. doi: 10.1377/hlthaff.2010.0517. [DOI] [PubMed] [Google Scholar]
- Dill MJ, Pankow S, Erikson C, Shipman S. Survey shows consumers open to a greater role for physician assistants and nurse practitioners. Health Affairs. 2013;32:1135–1142. doi: 10.1377/hlthaff.2012.1150. [DOI] [PubMed] [Google Scholar]
- Drug Enforcement Agency Office of Diversion Control. Controlled substance schedules. 2012 Retrieved from http://www.deadiversion.usdoj.gov/schedules/index.html#define.
- Dueker MJ, Jacox AK, Kalist DE, Spurr SJ. The practice boundaries of advanced practice nurses: An economic and legal analysis. Journal of Regulatory Economics. 2005;27:309–329. [Google Scholar]
- Federation of State Medical Boards. Assessing scope of practice in health care delivery: Critical questions in assuring public access and safety. 2005 Retrieved from http://www.fsmb.org/pdf/2005_grpol_scope_of_practice.pdf.
- Fitzgerald M. Why is it so hard to find a doctor? The Boston Globe. 2013 Oct 13; Retrieved from http://www.bostonglobe.com/magazine/2013/10/12/why-hard-find-doctor/AZmAhh8DJowD63cIVF0vPO/story.html.
- Goodell S, Dower C, O’Neil E. Primary care workforce in the United States (Robert Wood Johnson Foundation Policy Brief No. 22) 2011 Retrieved from http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2011/rwjf402104.
- Goodman DC. Twenty-year trends in regional variations in the U.S. physician work-force. Health Affairs. 2004;23:90–97. doi: 10.1377/hlthaff.var.90. [DOI] [PubMed] [Google Scholar]
- Halter M, Drennan V, Chattopadhyay K, Carneiro W, Yiallouros J, de Lusignan S, …Grant R. The contribution of physician assistants in primary care: A systematic review. BMC Health Services Research. 2013;13:223–236. doi: 10.1186/1472-6963-13-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration, Bureau of Health Professions. The physician workforce. Rockville, MD: Author; 2008. [Google Scholar]
- Health Resources and Services Administration, Department of Health and Human Services. Registered nurse population: Findings from the 2008 National Sample Survey of Registered Nurses. 2010 Retrieved from http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsur-veyfinal.pdf.
- Hing E, Hooker RS, Ashman JJ. Primary health care in community health centers and comparison with office-based practice. Journal of Community Health. 2011;36:406–413. doi: 10.1007/s10900-010-9322-x. [DOI] [PubMed] [Google Scholar]
- Hooker RS. Physician assistants and nurse practitioners: The United States experience. Medical Journal of Australia. 2006;185(1):4–7. doi: 10.5694/j.1326-5377.2006.tb00438.x. [DOI] [PubMed] [Google Scholar]
- Hooker RS, Everett CM. The contributions of physician assistants in primary care systems. Health and Social Care in the Community. 2012;20(1):20–31. doi: 10.1111/j.1365-2524.2011.01021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. British Medical Journal. 2002;324:819–823. doi: 10.1136/bmj.324.7341.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. The future of nursing: Focus on scope of practice. 2010 Retrieved from http://www.iom.edu/~/media/Files/Report%20Files/2010/The-Future-of-Nursing/Nursing%20Scope%20of%20Practice%202010%20Brief.pdf.
- Intrator O, Feng Z, Mor V, Gifford D, Bourbonniere M, Zinn J. The employment of nurse practitioners and physician assistants in U.S. nursing homes. The Gerontologist. 2005;45:486–495. doi: 10.1093/geront/45.4.486. [DOI] [PubMed] [Google Scholar]
- Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. Journal of the American Geriatrics Society. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- Kaas MJ, Moller MD, Markley JM, Billings C, Haber J, Hamera E, …Zimmerman M. Prescriptive authority for advanced practice psychiatric nurses: State of the states, 2001. Journal of the American Psychiatric Nurses Association. 2002;8:99–105. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Improving access to adult primary care in Medicaid: Exploring the potential role of nurse practitioners and physician assistants. 2011 Retrieved from http://kff.org/medicaid/issue-brief/improving-access-to-adult-primary-care-in/
- Klein TA. Scope of practice and the nurse practitioner: Regulation, competency, expansion, and evolution. Topics in Advanced Practice Nursing. 2005;5(2):1–8. [Google Scholar]
- Krein SL. The employment and use of nurse practitioners and physician assistants by rural hospitals. Journal of Rural Health. 1997;13(1):45–58. doi: 10.1111/j.1748-0361.1997.tb00833.x. [DOI] [PubMed] [Google Scholar]
- Kuo Y, Loresto FL, Jr, Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Affairs. 2013;32:1236–1243. doi: 10.1377/hlthaff.2013.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson EH, Hart LG. Growth and change in the physician assistant workforce in the United States, 1967–2000. Journal of Allied Health. 2007;36:121–130. [PubMed] [Google Scholar]
- Larson EH, Palazzo L, Berkowitz B, Pirani MJ, Hart LG. The contribution of nurse practitioners and physicians assistants to generalist care in Washington State. Health Services Research. 2003;38:1033–1050. doi: 10.1111/1475-6773.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugo NR, O’Grady ET, Hodnicki D, Hanson C. Are regulations more consumer-friendly when boards of nursing are the sole regulators of nurse practitioners. Journal of Professional Nursing. 2010;26(1):29–34. doi: 10.1016/j.profnurs.2009.09.001. [DOI] [PubMed] [Google Scholar]
- Mezey M, Burger SG, Bloom HG, Bonner A, Bourbonniere M, Bowers B, …Ter Maat M. Experts recommend strategies for strengthening the use of advanced practice nurses in nursing homes. Journal of the American Geriatrics Society. 2005;53:1790–1797. doi: 10.1111/j.1532-5415.2005.53556.x. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Affairs. 2010;29:893–899. doi: 10.1377/hlthaff.2010.0440. [DOI] [PubMed] [Google Scholar]
- Nelson R. In the final stretch: Standardizing APRN practice. American Journal of Nursing. 2012;112(7):21–22. doi: 10.1097/01.NAJ.0000415950.08815.13. [DOI] [PubMed] [Google Scholar]
- Pearson LJ. Annual legislative update. How each state stands on legislative issues affecting advanced nursing practice. Nurse Practitioner. 2003;28(1):26–32. doi: 10.1097/00006205-200401000-00010. [DOI] [PubMed] [Google Scholar]
- Pearson LJ. The Pearson report: The annual state-by-state national overview of nurse practitioner legislation and healthcare issues. American Journal for Nurse Practitioners. 2009;13(2) Retrieved from http://www.npwh.org/files/public/PEARSON.pdf. [Google Scholar]
- Perry JJ. The rise and impact of nurse practitioners and physician assistants on their own and cross-occupation incomes. Contemporary Economic Policy. 2009;27:491–511. [Google Scholar]
- Pohl JM, Hanson C, Newland JA, Cronenwett L. Unleashing nurse practitioners’ potential to deliver primary care and lead teams. Health Affairs. 2010;29:900–905. doi: 10.1377/hlthaff.2010.0374. [DOI] [PubMed] [Google Scholar]
- Reagan PB, Salsberry PJ. The effects of state-level scope-of-practice regulations on the number and growth of nurse practitioners. Nursing Outlook. 2013;61:392–399. doi: 10.1016/j.outlook.2013.04.007. [DOI] [PubMed] [Google Scholar]
- Schwartz MD. The US primary care workforce and graduate medical education policy. Journal of the American Medical Association. 2012;308:2252–2253. doi: 10.1001/jama.2012.77034. [DOI] [PubMed] [Google Scholar]
- Traczynski J, Udalova V. Nurse practitioner independence, health care utilization, and health outcomes (Working paper) 2013 doi: 10.1016/j.jhealeco.2018.01.001. Retrieved from http://www.lafollette.wisc.edu/research/health_economics/Traczynski.pdf. [DOI] [PubMed]
- Wing PLM, Salsberg ES, Continelli TA. The changing scope of practice of physician assistants, nurse practitioners, and certified nurse midwives in the fifty states, 1992–2000. Rensselaer, NY: Center for Health Workforce Studies, School of Public Health, University of Albany; 2002. [Google Scholar]
- Xing J, Mukamel DB, Temkin-Greener H. Hospitalizations of nursing home residents in the last year of life: Nursing home characteristics and variation in potentially avoidable hospitalizations. Journal of the American Geriatrics Society. 2013;61:1900–1908. doi: 10.1111/jgs.12517. [DOI] [PMC free article] [PubMed] [Google Scholar]