Abstract
Introduction
Image sharing technologies may reduce unneeded imaging by improving provider access to imaging information. A systematic review and meta-analysis were conducted to summarize the impact of image sharing technologies on patient imaging utilization.
Methods
Quantitative evaluations of the effects of PACS, regional image exchange networks, interoperable electronic heath records, tools for importing physical media, and health information exchange systems on utilization were identified through a systematic review of the published and gray English-language literature (2004–2014). Outcomes, standard effect sizes (ESs), settings, technology, populations, and risk of bias were abstracted from each study. The impact of image sharing technologies was summarized with random-effects meta-analysis and meta-regression models.
Results
A total of 17 articles were included in the review, with a total of 42 different studies. Image sharing technology was associated with a significant decrease in repeat imaging (pooled effect size [ES] = −0.17; 95% confidence interval [CI] = [−0.25, −0.09]; P < .001). However, image sharing technology was associated with a significant increase in any imaging utilization (pooled ES = 0.20; 95% CI = [0.07, 0.32]; P = .002). For all outcomes combined, image sharing technology was not associated with utilization. Most studies were at risk for bias.
Conclusions
Image sharing technology was associated with reductions in repeat and unnecessary imaging, in both the overall literature and the most-rigorous studies. Stronger evidence is needed to further explore the role of specific technologies and their potential impact on various modalities, patient populations, and settings.
Keywords: Health information exchange, radiology information systems, utilization, evaluation, data sharing
INTRODUCTION
Patients often seek care from multiple providers, which spreads information, including imaging studies and reports, across various health care organizations. Clinicians want access to these studies and results, for accurate interpretation and diagnoses [1–3], but often, they are difficult to obtain in a timely manner [4]. This lack of access may result in additional imaging [5], thereby increasing radiation exposure of the patient [6] and creating avoidable costs [7,8]. In addition, searching for studies from other sources wastes provider time [9–12] and delays treatment [13]. Finally, imaging has high utility in the diagnosis and treatment of disease, but inaccessible studies cannot support clinical decision making [11,14].
Image sharing technologies are a potential intervention to improve access to imaging studies and reports [15]. Various technologies allow providers to electronically access patients’ external imaging information (ie, outside the organization), such as that contained in a health information exchange (HIE), regional PACS, regional image exchange networks, interoperable electronic health records (EHRs), and tools for importing physical media (eg, CDs) [4,16,17]. Reports and qualitative studies suggest that these technologies improve provider access to patients’ imaging information [4,18–21].
Whether these technologies will result in changes to imaging utilization is less well understood. Several quantitative evaluations indicate that use of image sharing technologies reduces imaging utilization, particularly that for repeat and unnecessary imaging [14,22–25]. However, other studies show inconsistent results, or no effect at all [26–28].
Identification of effective interventions to improve access to images and reports is critical [3,11] for several reasons: utilization of imaging is on the rise [29,30]; repeat imaging is common [15]; and costs are increasingly drawing the attention of payers and policymakers. In this systematic review and meta-analysis, we sought to summarize the impact of image sharing technologies on imaging utilization, particularly repeat imaging.
METHODS
Searching
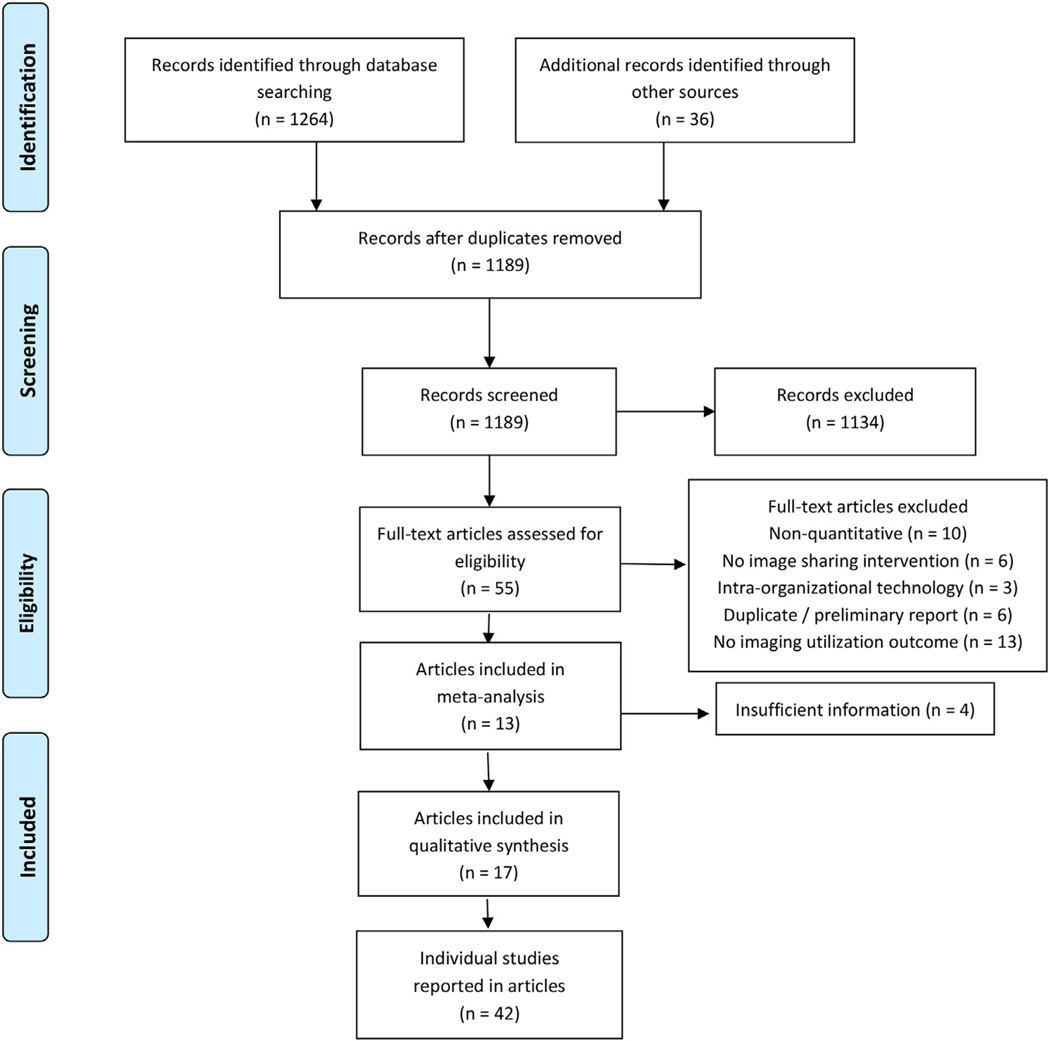
Relevant studies were identified, with adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [31], summarized in Figure 1.
Fig 1.
Article identification strategy with inclusion and exclusion criteria.
We reviewed the English-language medicine and health services research literature from the past decade (2004–2014) for original quantitative research and evaluation studies of the impact of image sharing technology on utilization. Radiology search terms were combined with keywords for image sharing technologies (Appendix 1), in Medline, ISI, CINAHL, EMBASE, Open Grey (grey literature archive), and the National Technical Reports Library (government reports). We manually reviewed citations, and the citing articles, from several recent image sharing evaluations, to identify additional articles. The initial search yielded 1,189 unduplicated records.
Selection
Based on abstracts, we excluded the following types of publications: editorials, practice guidelines, reviews, and those that had no indication that the topic was the impact of image sharing technology. Our primary search and screening process resulted in identification of 55 articles for a full-text review (kappa [К] = 0.65).
Articles were retained if they met the following criteria after full-text review: (1) reported on original research; (2) provided a quantitative measure of the effect of image sharing technology on utilization of imaging; and (3) technology involved allowed for access to external images or reports (eg, image sharing was interorganizational and not intraorganizational). In addition, we reassessed all full-text articles according to our previous exclusion criteria. We did not restrict inclusion on the basis of study design. Qualitative investigations, and surveys measuring perceptions and/or attitudes, were not included. Three of the investigators independently read each article and determined its inclusion status. Agreement on inclusion was high (К = 0.97). Remaining differences were resolved by consensus. A total of 17 articles met the inclusion criteria [14,23–28,32–41].
Abstraction
From each included article, we abstracted the following information: study design; patient population; setting; modality (specific, multiple, basic, or advanced); outcome; sample size; effect size (with variances); and technology type. Given the small sample, we grouped HIEs and EHRs into a single category, because they are both information systems that contain (and can share) a broad range of clinical, demographic, and administrative data. We grouped PACS and physical media importation systems into a single category, because these are radiology-specific systems, and in the PACS studies, authors often mentioned that physical media importation was still an available option.
For five articles [23,28,32,38,40], we reanalyzed reported frequencies or means, to determine the effect sizes, using Student’s t tests, and correlations, with standard formulas to derive missing information if necessary [42–44]. Effect sizes could not be determined for four of the articles [33,36,37,41], either because of the study design or because the article did not contain sufficient statistical information for analysis. We included the characteristics of these articles in our overall descriptions of the literature, but they did not contribute to the meta-analysis. We converted all reported results to standard effect sizes and 95% confidence intervals (CIs) [45].
Some of the articles in the final set (n = 13) contained multiple research findings (ie, more than one “study” within a single article). Individual studies were defined as follows: stratified samples (eg, imaging utilization reported separately for primary versus specialty care settings); independent assessments of different modalities (eg, CTs and radiographs measured separately); and/or different outcomes. We selected the best-fitting models, or the adjusted effect sizes if multiple regression estimates or sensitivity analyses on the same outcomes were reported.
To describe the possibility of bias, we noted the presence, versus absence, of the following safeguards to internal validity: adjustment for potential confounding; inclusion of an appropriate comparison group; inclusion of preintervention observations; measurement of technology usage (not just adoption); adjustment for repeated or clustered measures; and robustness checks (eg, formal tests or stratified analyses). We characterized studies involving multiple institutions or settings as being more generalizable (ie, a safeguard against bias) than single-institution studies. The number of indicators present, from these seven, was used as a measure of potential risk of bias: studies with only three or fewer indicators were at moderate or high risk for bias; those with four or more indicators were at lower risk.
Statistical Analysis
We characterized the articles by type of technology, using frequencies and Fisher’s exact test. We summarized the research on the impact of image sharing technologies with a random-effects model meta-analysis [46,47]. Pooled estimates of effect size, and forest plots, for all findings were obtained using Stata (StataCorp LP version 13.1, College Station, Texas) with the I2 statistic, to describe the extent of statistical heterogeneity of the findings [48]. In addition, we stratified the pooled effect sizes by use outcome (unnecessary imaging was combined with repeat imaging, owing to small sample size).
To explore the relationship between study characteristics and observed effects on utilization, we performed a meta-regression using the individual study findings as the units of analysis (with inverse variance weights) and robust SEs to account for multiple study findings per article. Finally, we assessed risk of bias, by limiting the pooled analyses to those studies that were found to have the lowest risk for bias, and by examining the full sample of studies, using funnel plots (Appendix 1, Fig A1) and Egger’s test for publication bias [49].
RESULTS
Characteristics of Included Articles and Studies
A total of 17 articles described the quantitative effects of image sharing technologies on utilization, with nine focusing on repeat imaging, and eight using any imaging as the outcome (Table 1; Appendix 1, Table A1). Most articles evaluated HIEs or EHRs (58.8%), were set in emergency departments (EDs; 58.8%), included the general patient population (52.9%), and considered both advanced and basic modalities (70.6%). Articles did vary significantly by the type of image sharing technology used in the study. With PACS, the sharing was more likely to be of actual images, and the focus on patients with a specific condition. The risk of bias tended to be lower in studies that evaluated HIEs and/or EHRs. All the studies focusing on PACS had a moderate or high risk of bias. The 13 articles that had sufficient information to contribute to the meta-analysis included 42 different studies.
Table 1.
Characteristics of articles on the quantitative effect of image sharing technologies on utilization
| Total | HIE or EHR | PACS or Physical Media | p value | |
|---|---|---|---|---|
| Articles | 17 | 10 | 7 | |
| Outcome | ||||
| Repeat imaging* | 9 (52.9) | 5 (50.0) | 3 (42.9) | .581 |
| Any imaging | 8 (47.1) | 5 (50.0) | 4 (57.1) | |
| Imaging modality | ||||
| Advanced only | 5 (29.4) | 1 (10.0) | 4 (57.1) | .060 |
| Advanced and basic | 12 (70.6) | 9 (90.0) | 3 (42.9) | |
| Information content | ||||
| Images† | 9 (52.9) | 2 (20.0) | 7 (100.0) | .003 |
| Reports | 6 (35.3) | 6 (60.0) | 0 (0.0) | |
| Not specified | 2 (11.8) | 2 (20.0) | 0 (0.0) | |
| Setting | ||||
| Emergency department | 10 (58.8) | 6 (60.0) | 4 (57.1) | .767 |
| Inpatient | 1 (5.9) | 0 (0.0) | 1 (14.3) | |
| Office-based | 2 (11.8) | 1 (10.0) | 1 (14.3) | |
| Community-wide | 4 (23.5) | 3 (30.0) | 1 (14.3) | |
| Patient population | ||||
| General | 9 (52.9) | 8 (80.0) | 1 (14.3) | .008 |
| Specific condition | 4 (23.5) | 0 (0.0) | 4 (57.1) | |
| Transfer/trauma | 4 (23.5) | 2 (20.0) | 2 (28.6) | |
| Study design | ||||
| Cohort | 7 (41.2) | 4 (40.0) | 3 (42.9) | .091 |
| Quasi-experimental | 2 (11.8) | 2 (20.0) | 0 (0.0) | |
| Cross-sectional | 2 (11.8) | 1 (10.0) | 1 (14.3) | |
| Pretest–posttest | 3 (17.6) | 0 (0.0) | 3 (42.9) | |
| Posttest only/case series | 3 (17.6) | 3 (30.0) | 0 (0.0) | |
| Risk of bias | ||||
| Low | 7 (41.2) | 7 (70.0) | 0 (0.0) | .010 |
| Moderate or high | 10 (58.8) | 3 (30.0) | 7 (100.0) | |
| Insufficient information for inclusion‡ | 4 (23.5) | 2 (20.0) | 2 (28.6) | |
| Total number of findings abstracted | 42 | 27 | 15 |
EHR = electronic health record; HIE = health information exchange.
Includes “unnecessary” or “avoidable” imaging.
Also gave access to reports.
Excluded from the meta-analysis.
Estimated Effect of Image Sharing Technology on Imaging Utilization
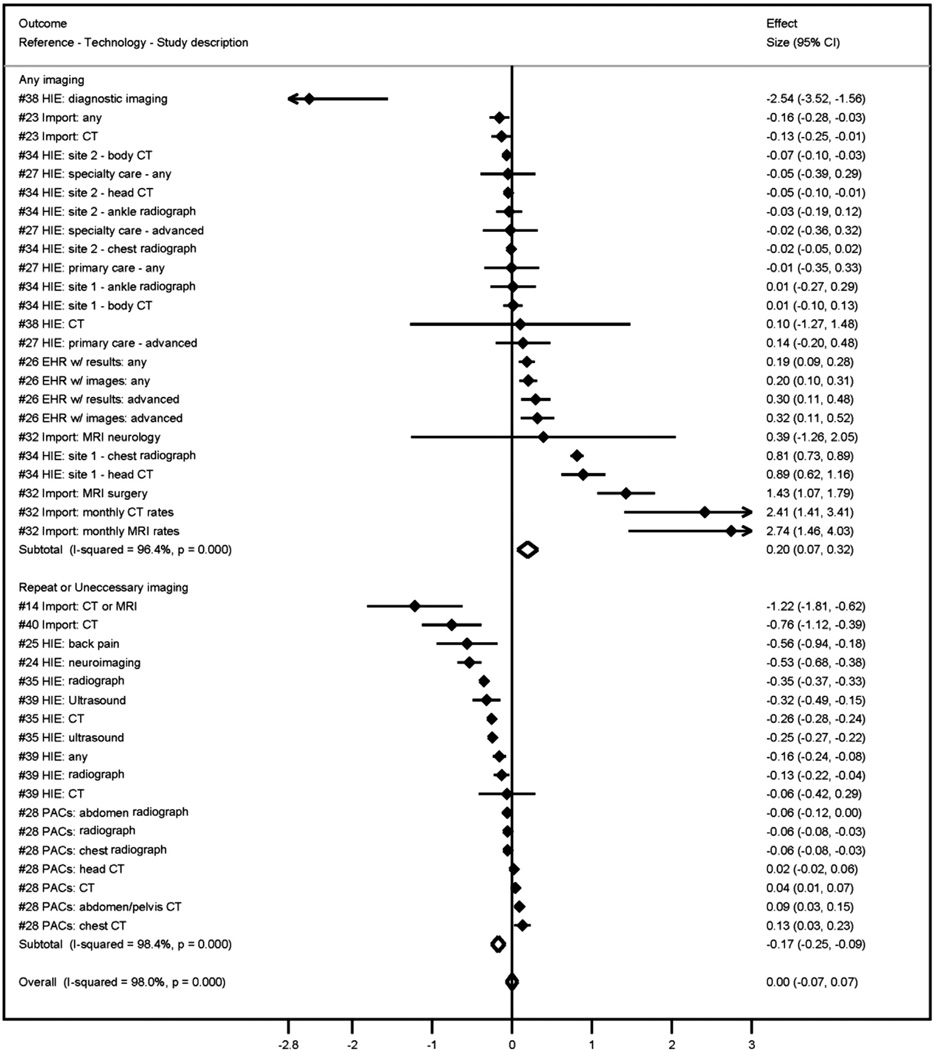
A total of 57% of all studies found some reduction in imaging utilization when image sharing technology was available. However, in the overall pooled analysis (Fig 2), image sharing technologies were not associated with reductions in imaging utilization (effect size (ES) = 0.00; 95%CI[−0.07, 0.07]; P = .991 Substantial heterogeneity was found in the results of the studies (I2 = 98%).
Fig 2.
Association (standard effect size) between image sharing technologies and any imaging, repeat imaging, and all outcomes: systematic review and meta-analysis, 2004 to 2014. HIE = health information exchange; EHR = electronic health records.
The effect of image sharing technology did differ significantly depending on the outcome studied (Fig 2). If the outcome was any imaging, image sharing technology was associated with a significant increase in utilization (pooled ES = 0.20; 95% CI [0.07, 0.32]; P = .002). In contrast, image sharing technology was associated with a significant decrease in repeat imaging (pooled ES = −0.17; 95% CI [−0.25, −0.09]; P < .001).
Study Characteristics and Observed Effects on Imaging Utilization
Negative coefficients in the adjusted meta-regression model (Table 2) indicate that the study characteristic was associated with reductions in utilization. Studies in the ED setting were more likely to indicate reductions in utilization (β = −0.34; 95% CI [−0.66, −0.01]), as were studies that looked at the occurrence of repeat (including unnecessary) imaging as an outcome (β = −0.58; 95% CI [−0.84, −0.33]). Given the highly variable effect sizes and the small sample size, we were more interested in the direction of the estimated associations than in the point estimates. Due to collinearity, not all of the abstracted information could be included in the model.
Table 2.
Adjusted associations between study characteristics and effect sizes of image sharing technology on imaging utilization: systematic review and meta-analysis, 2004–2014
| Characteristic | β (95% Confidence interval) | P Value |
|---|---|---|
| Outcome | ||
| Repeat imaging versus any imaging | −0.58 (−0.84, −0.33) | <.001 |
| Technology | ||
| Health
information exchange and/or electronic health record versus PACS and/or CD importation |
−1.08 (−2.48, 0.32) | .125 |
| Setting | ||
| Emergency department versus all other settings | −0.34 (−0.66, −0.01) | .043 |
| Patient population | ||
| General patients versus all other patient populations | −0.32 (−1.16, 0.52) | .451 |
| Evidence quality score | 0.31 (−0.19, 0.82) | .213 |
Note: Estimates with inverse variance weights and robust SEs.
The type of image sharing technology was not statistically associated with effect size; however, studies examining HIE and/or EHRs did reveal more negative effect estimates than did studies of PACS. For example, HIE was negatively associated with the occurrence of repeat (or unnecessary) imaging in all of the included studies [24,25,35,39] (Appendix 1, Table A1). The effect of HIE on any utilization was more ambiguous: eight studies found reductions, but five found increases in imaging [27,34,38]. Additionally, those studies that did not meet the meta-analysis inclusion requirements suggested reductions in utilization [36,41]. Additionally, the occurrence of repeat imaging was lower in one study that used a shared PACS system [28], and in two that examined physical media importation [14,40].
Risk of Bias
Most studies used a cohort or cross-sectional design, without true before and after measurements; this factor was the most common for risk of bias (Appendix 1, Table A1). These design choices were further weakened by the frequent lack of a comparison group. The lack of a definable comparison group was a problem only among the PACS and/or importation technology articles; all HIE and/or EHR articles had a comparison group. Generally, the HIE and/or EHR articles included features that better guarded against bias, such as study designs with stronger internal validity, adjustment for confounding, adjustment for repeated measures, and findings from multiple institutions. Analysis of only those studies that had the lowest risk of bias produced results that did not vary substantially from the main findings. Image sharing technology was not associated with reductions in overall imaging utilization or in utilization of any imaging, but it was associated with reductions in repeat utilization (Appendix 1, Table A1).
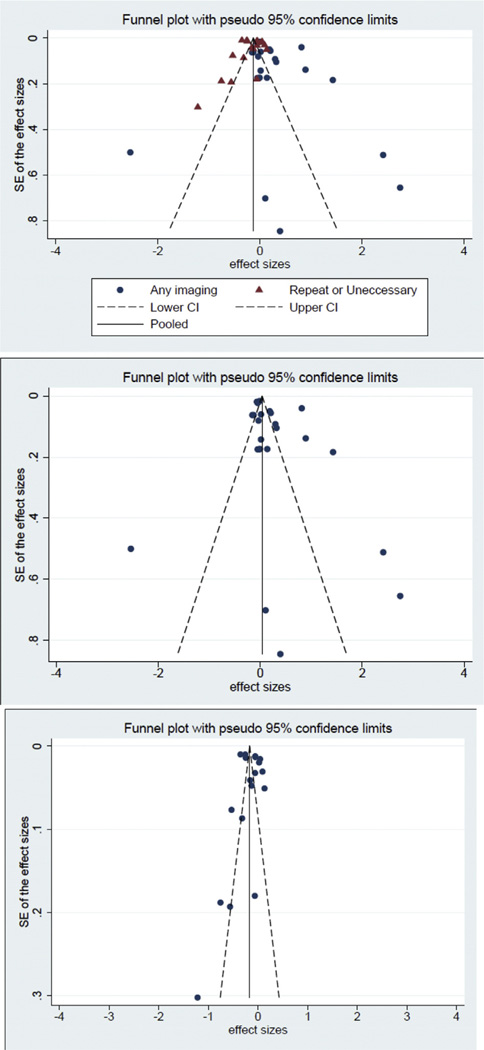
The potential for publication bias cannot be ruled out. Visual examination of the funnel plots of effect sizes, for all studies and by outcome (Appendix 1, Fig A1), did not suggest any overt publication bias, but the small sample size complicates interpretation. In addition, Egger’s test did not suggest publication bias, but the test has a high type 1 error rate (ie, it is susceptible to false positives).
DISCUSSION
Image sharing technology utilization was associated with reductions in repeat and unnecessary imaging, in the overall literature and in the most rigorous studies. Not all repeated imaging is avoidable, but repeating imaging solely because an earlier image is inaccessible at the time of care is likely avoidable [50]. When providers have sufficient access to relevant imaging, they are more likely to forego repeat imaging [41,51].
Image sharing technologies were designed to address this issue [15]. Although payers (including Medicare) often do not reimburse providers for reviewing an external study, image sharing technologies can make the process of accessing earlier studies easier for physicians. Additionally, repeat imaging and unnecessary imaging are clearly important to target for cost-saving efforts that can simultaneously improve care and the patient experience [15,50]. The potential impact on repeat imaging is particularly promising in the context of fee-for-service reimbursement, the dominant payment model used in the United States, which does not penalize providers for inappropriate utilization. However, even integrated delivery systems (in which incentives are theoretically aligned) are not immune from inappropriate imaging, so image sharing technologies could play a role in quality strategies in those settings, or for any organization preparing for value-based payments [52].
In contrast, image sharing technology was not effective in reducing any (eg, overall) imaging utilization. For many studies, once image sharing technology was introduced into a setting or used by health care professionals, imaging utilization increased. Unlike the case of repeat and/or unnecessary imaging, no clear link was found between reductions in overall imaging and utilization of image sharing technology. Many instances of imaging may be unavoidable, or should be expected as appropriate diagnostic procedures, treatment regimens, or in light of changes to patients’ condition [53]. In these cases, access to prior imaging could improve the accuracy of diagnoses, monitor disease progression, or aid in decision making, but it would have little role in utilization.
Alternatively, the actual increase in imaging utilization may be a product of technology that, although it increases access to existing images, simultaneously makes it easier for providers to order imaging studies [26], particularly for EHRs, which have viewing and ordering within the same application [54]. The same might be true for PACS, if a system were introduced at the same time, or interfaced tightly with the radiology information system in which the image ordering takes place [55]. Another possibility is that the increase in imaging is attributable to increases in work efficiency that result from PACS adoption [56].
The opportunities to use image sharing technology are growing, through projects such as the RSNA’s Image Share [57], and federal policies that encourage technology adoption, such as the Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs, commonly called Meaningful Use [58]. The expectation that these technologies will be used will grow, as public recognition of the potential value of access to images increases [59,60]. Nonetheless, the evidence demonstrating effectiveness of image sharing technologies is limited. This meta-analysis supports the hypothesis that image sharing technologies can be useful, but given the small number of quantitative studies, and the frequent risk of bias, many important questions remain unanswered.
A critical limitation on acquiring such evidence is that effects reported in the literature cannot be stratified by modality, patient characteristics, or conditions. Imaging rates vary according to patient populations, and the ability to easily access prior studies reportedly varies by modality [61]. We do not have any conclusive insights into the relative effectiveness of various image sharing technologies. For example, comparing PACS to HIEs would provide insights as to whether access to imaging information alone is sufficient to change subsequent utilization, or if access to imaging information in conjunction with broader patient information is more useful.
The current study suggests that HIE was the technology most likely to reduce utilization, but the sample size and risk of bias in the other image sharing technology studies prevented further investigation. Lastly, the available quantitative research does not sufficiently capture the differences in provider workflows and information needs. For example, a primary care provider may prefer access to a report that has accompanying clinical information, whereas a subspecialty physician, such as a neurosurgeon, may prioritize access to the image.
The evidence base can be improved in several ways. Stronger research designs are required, to allow causal inferences to be drawn and better control of confounding. Opportunities are available to select and use better designs. For example, interrupted time series designs fit well with technology implementations. Implementation planning takes time, including the collection of baseline data.
In addition, as part of the implementation plan, institutions may roll out or stagger implementation dates across various sites, allowing for natural comparison groups. Alternatively, the system vendors could assist in identifying other customers going through the process of implementation, to both add as comparisons and increase the generalizability of findings. Additionally, multidisciplinary research teams could help strengthen studies: Health services researchers could provide expertise to address the issues of selection and confounding present in many studies, informaticists understand the actual usage of systems, and clinicians provide the conceptual linkage between imaging information and clinical care.
In general, health IT research and evaluation needs to be strengthened and made more generalizable [62–64]. For example, evaluations outside of ED settings are a clear gap in the literature. Available methods and designs could improve the quality of research; but those who fund research (ie, government agencies, health systems, or vendors) must be willing to invest the necessary resources and time to make higher-quality research possible.
Limitations
First, this analysis does not address all the potential effects of image sharing technology, such as efficiency gains, satisfaction, or cost [63,64]. Second, we did not explore barriers that prevent organizations from adopting these technologies into their clinical workflow. Even when such technologies are available, it may always just be “easier” to order the image. Third, this review is not about clinical decision support. Evidence suggests that this too may be a technology-enabled approach to improving utilization [65]. Fourth, generalizability may be limited, because many of the included articles analyzed data that were from only one organization or a single technology. Given the variation among vendor products, and differences in the levels of adoption and integration among organizations, these findings may not translate to all settings. Lastly, even though our search strategy included multiple databases, and the gray literature, we may be missing studies, and our overall findings may be limited by publication bias.
CONCLUSIONS
Image sharing technologies have the potential to improve provider access to existing imaging studies and reports. Usage of image sharing technology was associated with reductions in repeat and unnecessary imaging utilization in both the overall literature and in the most-rigorous studies. Stronger evidence is needed to identify the role of specific technologies and the potential impact on various modalities, patient populations, and settings.
TAKE-HOME POINTS.
-
■
Image sharing technologies (health information exchange, PACS, EHRs, and media import) are a potential intervention to improve access to previous imaging studies and reports.
-
■
Across multiple technologies, and in the most-rigorous studies, image sharing was associated with a modest, but statistically significant, decrease in repeat imaging.
-
■
The literature on the impact of image sharing technology is small, so that no specific conclusions can be drawn about the effects of a specific modality, technology, or patient population.
-
■
The literature would benefit from stronger research designs and better control of confounding. Those funding the research must be willing to invest the necessary resources and time needed to make higher-quality research possible.
Acknowledgments
This work was funded under a grant by the Harvey L. Neiman Health Policy Institute (to J.R.V. and H-Y.J.). We thank the many investigators and authors who supplied us with additional information about their work.
APPENDIX 1
Table A1.
List of articles and studies
| Article (Year) [Reference Number] |
Outcome | Technology | Setting | Patient Population |
In Meta- analysis? |
Studies | Description | Risk
of Bias Score |
Comparison Group |
Pre- post |
Measured Usage |
Adjust for Confounding |
Adjusted for Correlation |
Robustness Check |
>1 Institution |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bailey (2013) [24] |
Unnecessary | HIE | ED | Headache | Y | 1 | Unnecessary neuroimaging |
5 | Y | N | Y | Y | Y | N | Y |
| Bailey (2013) [25] |
Repeat | HIE | ED | Back pain | Y | 1 | Duplicative imaging for back pain |
5 | Y | N | Y | Y | Y | N | Y |
| Cheponis (2013) [32] |
Any imaging | Physical media import |
Office- based |
Neurology | Y | 4 | Monthly CT and MRI rates overall and for repeat patients |
2 | N | Y | N | N | N | Y | N |
| Flanagan (2012) [33] |
Repeat | Shared PACS |
ED | Transfer | N | – | Repeat imaging among transfer patients |
1 | N | Y | N | N | N | N | N |
| Frisse (2012) [34] |
Any imaging | HIE | ED | General | Y | 8 | Radiograph and CT utilization at different sites |
6 | Y | N | Y | Y | Y | Y | Y |
| Lammers (2014) [35] |
Repeat | HIE | ED | General | Y | 3 | Repeat CT, ultrasound and radiograph |
6 | Y | Y | N | Y | Y | Y | Y |
| Lu (2012) [14] |
Repeat | Physical media import |
Inpatient | Cancer | Y | 1 | CT or MRI at transfer |
3 | Y | N | Y | Y | N | N | N |
| Mäenpää (2011) [36] |
Any imaging | HIE | Community- wide |
General | N | – | Population study of regional HIE |
1 | N | N | N | N | N | N | Y |
| McCormick (2012) [26] |
Any imaging | EHR | Community- wide |
General | Y | 4 | Any and advanced imaging based on results or image sharing |
5 | Y | N | N | Y | Y | Y | Y |
| Psoter (2014) [37] |
Any imaging | Shared PACS |
ED | Transfer | N | – | Any imaging among transfer patients |
2 | N | Y | N | Y | N | N | N |
| Ross (2013) [27] |
Any imaging | HIE | Office- based |
General | Y | 4 | Primary and specialty care; any and advanced imaging rates |
6 | Y | Y | N | Y | Y | Y | Y |
| Sodickson (2011) [23] |
Any imaging | Physical media import |
ED | Transfer | Y | 2 | Importation of CT only, or all images |
2 | Y | N | Y | N | N | N | N |
| Tzeel (2011) [38] |
Any imaging | HIE | ED | General | Y | 2 | CT or
diagnostic imaging utilization |
3 | Y | N | N | Y | N | N | Y |
| Vest (2014) [39] |
Repeat | HIE | Community- wide |
General | Y | 4 | Repeat of any,
CT, ultrasound, or radiograph at 90 days |
6 | Y | N | Y | Y | Y | Y | Y |
| Whiteman (2014) [40] |
Repeat | Physical media import |
ED | Trauma | Y | 1 | CT utilization | 1 | N | Y | N | N | N | N | N |
| Winden (2014) [41] |
Avoided | HIE | ED | General | N | – | Avoided imaging from HIE |
1 | N | N | Y | N | N | N | N |
| You (2008) [28] |
Repeat | Shared PACS |
Community- wide |
General | Y | 7 | Repeat of CT and radiograph at 30 days, by body location* |
3 | N | Y | N | N | N | Y | Y |
ED = emergency department; EHR = electronic health record; HIE = health information exchange; N = no; Y = yes.
Also reported 7-day and 60-day repeat rates, but not abstracted.
Fig A1. Funnel plot of effect sizes from image sharing technology systematic review and meta-analysis, 2004–2014.
Example Search Strategy
MEDLINE
All-field search of “image sharing technology”
All-field search of “Picture Archiving and Communications Systems”
All-field search of “electronic health record”
All-field search of “image exchange network”
All-field search of “physical media”
All-field search of “health information exchange”
MESH term “Radiology Information Systems”
#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7
MESH term “Radiography/utilization”
All-field search of imaging
All-field search of “repeat imaging”
All-field search of “imaging cost”
All-field search of “radiology cost”
All-field search of “unnecessary imaging”
#9 OR #10 OR #11 OR #12 OR #13 OR #14
Limits: English. Year 2005/1/1 — 2014/12/31. Abstract. Humans.
Not orthodontics. Not dental.
-
Number retrieved =746
MESH = medical subject heading.
Secondary Analysis to Assess Risk of Bias
To examine the risk of bias in the pooled analyses, we restricted the sample to those studies (n = 25) with the lowest risk of bias (with ≥4 of the 7 possible quality indicators). Overall, no statistical association between image sharing technology and utilization was found (pooled ES = −0.01; 95% CI [−0.09, 0.09]; P < .963). For studies with any imaging utilization as the outcome, image sharing technology was associated with an increase in utilization (pooled ES = 0.17; 95% CI [0.04, 0.30]; P= .012). Again, image sharing technology was associated with a reduction in repeat imaging (pooled ES = −0.27; 95% CI [−0.33, −0.21]; P < .001).
Footnotes
The other authors have no conflicts of interest related to the material discussed in this article.
REFERENCES
- 1.Stevenson CA. Problems in radiology of today and the future. AJR Am J Roentgenol. 1966;98:777–781. doi: 10.2214/ajr.98.4.777. [DOI] [PubMed] [Google Scholar]
- 2.White K, Berbaum K, Smith WL. The role of previous radiographs and reports in the interpretation of current radiographs. Invest Radiol. 1994;29:263–265. doi: 10.1097/00004424-199403000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Reiner BI. Medical imaging data reconciliation, part 3: reconciliation of historical and current radiology report data. J Am Coll Radiol. 2011;8:768–771. doi: 10.1016/j.jacr.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 4.Sandberg JC, Ge Y, Nguyen HT, et al. Insight into the sharing of medical images: physician, other health care providers, and staff experience in a variety of medical settings. Appl Clin Inform. 2012;3:475–487. doi: 10.4338/ACI-2012-06-RA-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency department transfer patients. J Am Coll Radiol. 2009;6:626–632. doi: 10.1016/j.jacr.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Amis ES, Butler PF, Applegate KE, et al. ACR white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4:272–284. [Google Scholar]
- 7.Jones AC, Woldemikael D, Fisher T, Hobbs GR, Prud’homme BJ, Bal GK. Repeated computed tomographic scans in transferred trauma patients: indications, costs, and radiation exposure. J Trauma Acute Care Surg. 2012;73:1564–1569. doi: 10.1097/TA.0b013e31826fc85f. [DOI] [PubMed] [Google Scholar]
- 8.Kalbhen CL, Yetter EM, Olson MC, Posniak HV, Aranha GV. Assessing the resectability of pancreatic carcinoma: the value of reinterpreting abdominal CT performed at other institutions. AJR Am J Roentgenol. 1998;171:1571–1576. doi: 10.2214/ajr.171.6.9843290. [DOI] [PubMed] [Google Scholar]
- 9.Bagg SA, Steenburg SD, Ravenel JG. Handling of outside trauma studies: a survey of program directors. J Am Coll Radiol. 2008;5:657–663. doi: 10.1016/j.jacr.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Dreyer KJ. [Accessed October 26, 2015];Need for image, data portability opens door for electronic answers. Available at: http://www.diagnosticimaging.com/articles/need-image-data-portability-opens-door-electronic-answers.
- 11.Robinson J, McNeeley M. Transfer patient imaging: a survey of members of the American Society of Emergency Radiology. Emerg Radiol. 2012;19:447–454. doi: 10.1007/s10140-012-1047-y. [DOI] [PubMed] [Google Scholar]
- 12.Yeager D. Swamped with CDs. Radiol Today. 2011;12:12–14. [Google Scholar]
- 13.Emick DM, Carey TS, Charles AG, Shapiro ML. Repeat imaging in trauma transfers: a retrospective analysis of computed tomography scans repeated upon arrival to a Level I trauma center. J Trauma Acute Care Surg. 2012;72:1255–1262. doi: 10.1097/TA.0b013e3182452b6f. [DOI] [PubMed] [Google Scholar]
- 14.Lu MT, Tellis WM, Fidelman N, Qayyum A, Avrin DE. Reducing the rate of repeat imaging: import of outside images to PACS. AJR Am J Roentgenol. 2012;198:628–634. doi: 10.2214/ajr.11.6890. [DOI] [PubMed] [Google Scholar]
- 15.Hendee WR, Becker GJ, Borgstede JP, et al. Addressing overutilization in medical imaging. Radiology. 2010;257:240–245. doi: 10.1148/radiol.10100063. [DOI] [PubMed] [Google Scholar]
- 16.Mendelson DS, Bak PR, Menschik E, Siegel E. Image exchange: IHE and the evolution of image sharing. RadioGraphics. 2008;28:1817–1833. doi: 10.1148/rg.287085174. [DOI] [PubMed] [Google Scholar]
- 17.Mendelson DS, Erickson BJ, Choy G. Image sharing: evolving solutions in the age of interoperability. J Am Coll Radiol. 2014;11(12, Part B):1260–1269. doi: 10.1016/j.jacr.2014.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee J. Share ware. Mod Healthcare. 2012;42:32–34. [PubMed] [Google Scholar]
- 19.Landro L. Health & wellness—the informed patient: image sharing seeks to reduce repeat scans. The Wall Street Journal. 2013 [Google Scholar]
- 20.Morey D. Image sharing moves up a level. [Accessed January 2, 2015];Orlando Medical News. 2010 Available at: http://orlando.medicalnewsinc.com/image-sharing-moves-up-a-level-cms-1098.
- 21.Kierkegaard P, Kaushal R, Vest J. Patient information retrieval in multiple care settings: examining methods of exchange in emergency departments, primary care practices, and public health clinics? Am J Manag Care. 2014;20(11 Spec No. 17):SP494–SP501. [PubMed] [Google Scholar]
- 22.Ip IK, Mortele KJ, Prevedello LM, Khorasani R. Repeat abdominal imaging examinations in a tertiary care hospital. Am J Med. 2012;125:155–161. doi: 10.1016/j.amjmed.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sodickson A, Opraseuth J, Ledbetter S. Outside imaging in emergency department transfer patients: CD import reduces rates of subsequent imaging utilization. Radiology. 2011;260:408–413. doi: 10.1148/radiol.11101956. [DOI] [PubMed] [Google Scholar]
- 24.Bailey JE, Wan JY, Mabry LM, et al. Does health information exchange reduce unnecessary neuroimaging and improve quality of headache care in the emergency department? J Gen Intern Med. 2013;28:176–183. doi: 10.1007/s11606-012-2092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bailey JE, Pope RA, Elliott EC, Wan JY, Waters TM, Frisse ME. Health information exchange reduces repeated diagnostic imaging for back pain. Ann Emerg Med. 2013;62:16–24. doi: 10.1016/j.annemergmed.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 26.McCormick D, Bor DH, Woolhandler S, Himmelstein DU. Giving office-based physicians electronic access to patients’ prior imaging and lab results did not deter ordering of tests. Health Aff. 2012;31:488–496. doi: 10.1377/hlthaff.2011.0876. [DOI] [PubMed] [Google Scholar]
- 27.Ross SE, Radcliff TA, LeBlanc WG, Dickinson LM, Libby AM, Nease DE., Jr Effects of health information exchange adoption on ambulatory testing rates. J Am Med Inform Assoc. 2013;20:1137–1142. doi: 10.1136/amiajnl-2012-001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.You JJ, Yun L, Tu JV. Impact of PACS on rates of duplicate imaging: a before-after study. BMC Health Serv Res. 2008;8:234. doi: 10.1186/1472-6963-8-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith-Bindman R, Miglioretti D, Larson E. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff. 2008;27:1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy. Washington, DC: 2014. http://www.medpac.gov/documents/reports/mar14_entirereport.pdf?sfvrsn=0. [Google Scholar]
- 31.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheponis J, Weathers A, Amin D, Sims S, Ouyang B. Does the ability to incorporate images from external radiology studies into an electronic health record (EHR) change the ordering practices of academic neurologists and neurosurgeons? Neurology 2013; 80(Meeting Abstracts 1): S27.005. Available at: http://www.neurology.org/cgi/content/meeting_abstract/80/1_MeetingAbstracts/S27.005.
- 33.Flanagan PT, Relyea-Chew A, Gross JA, Gunn ML. Using the Internet for image transfer in a regional trauma network: effect on CT repeat rate, cost, and radiation exposure. J Am Coll Radiol. 2012;9:648–656. doi: 10.1016/j.jacr.2012.04.014. [DOI] [PubMed] [Google Scholar]
- 34.Frisse ME, Johnson KB, Nian H, et al. The financial impact of health information exchange on emergency department care. J Am Med Inform Assoc. 2012;19:328–333. doi: 10.1136/amiajnl-2011-000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lammers EJ, Adler-Milstein J, Kocher KE. Does health information exchange reduce redundant imaging? Evidence from emergency departments. Med Care. 2014;52:227–234. doi: 10.1097/MLR.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 36.Mäenpää T, Asikainen P, Gissler M, et al. Outcomes assessment of the regional health information exchange: a five-year follow-up study. Meth Inform Med. 2011;50:308–318. doi: 10.3414/ME10-01-0048. [DOI] [PubMed] [Google Scholar]
- 37.Psoter KJ, Roudsari BS, Vaughn M, Fine GC, Jarvik JG, Gunn ML. Effect of an image-sharing network on CT utilization for transferred trauma patients: a 5-year experience at a level I trauma center. J Am Coll Radiol. 2014;11:616–622. doi: 10.1016/j.jacr.2013.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tzeel A, Lawnicki V, Pemble KR. The business case for payer support of community-based health information exchange: a humana pilot evaluating its effectiveness in cost control for plan members seeking emergency department care. Am Health Drug Ben. 2011;4:207–216. [PMC free article] [PubMed] [Google Scholar]
- 39.Vest J, Kaushal R, Silver M, Hentel K, Kern L for the HITEC investigators. Health information exchange and the frequency of repeat medical imaging. Am J Manag Care. 2014;20(11 Spec No. 17):eSP16–esp24. [PubMed] [Google Scholar]
- 40.Whiteman C, Kiefer C, D’Angelo J, Davidov D, Larrabee H, Davis S. The use of technology to reduce radiation exposure in trauma patients transferred to a level I trauma center. W Virginia Med J. 2014;110:14–18. [PubMed] [Google Scholar]
- 41.Winden TJ, Boland LL, Frey NG, Satterlee PA, Hokanson JS. Care everywhere, a point-to-point HIE tool. Appl Clin Informat. 2014;5:388–401. doi: 10.4338/ACI-2013-12-RA-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hozo S, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Meth. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Altman DG, Bland JM. How to obtain the P value from a confidence interval. Br Med J. 2011;343:d2304. doi: 10.1136/bmj.d2304. [DOI] [PubMed] [Google Scholar]
- 44.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wilson DB. [Accessed February 10, 2015];Practical meta-analysis effect size calculator. Available at: http://www.campbellcollaboration.org/escalc/html/EffectSizeCalculator-Home.php.
- 46.Ringquist EJ. Meta-analysis for public management & policy. San Francisco, CA: Jossey-Bass; 2013. [Google Scholar]
- 47.Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 48.Harris R, Bradburn M, Deeks J, Harbord R, Altman D, Sterne J. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. [Google Scholar]
- 49.Harbord RM, Harris RJ, Sterne JAC. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9:197–210. [Google Scholar]
- 50.Rao VM, Levin DC. The overuse of diagnostic imaging and the Choosing Wisely initiative. Ann Intern Med. 2012;157:574–576. doi: 10.7326/0003-4819-157-8-201210160-00535. [DOI] [PubMed] [Google Scholar]
- 51.Carr CM, Gilman CS, Krywko DM, Moore HE, Walker BJ, Saef SH. Observational study and estimate of cost savings from use of a health information exchange in an academic emergency department. J Emerg Med. 2014;46:250–256. doi: 10.1016/j.jemermed.2013.05.068. [DOI] [PubMed] [Google Scholar]
- 52.Burwell SM. Setting value-based payment goals—HHS efforts to improve U.S. health care. N Engl J Med. 2015;372:897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 53.Cascade PN. The ACR. ACR APPROPRIATENESS CRITERIA® project. Radiology. 2000;(214 Suppl):3–46. doi: 10.1148/radiology.214.1.r00ja493. [DOI] [PubMed] [Google Scholar]
- 54.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008;359:50–60. doi: 10.1056/NEJMsa0802005. [DOI] [PubMed] [Google Scholar]
- 55.Paré G, Trudel M-C. Knowledge barriers to PACS adoption and implementation in hospitals. Int J Med Inform. 2007;76:22–33. doi: 10.1016/j.ijmedinf.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 56.Reiner BI, Siegel EL, Hooper FJ, Pomerantz S, Dahlke A, Rallis D. Radiologists’ productivity in the interpretation of CT scans. AJR Am J Roentgenol. 2001;176:861–864. doi: 10.2214/ajr.176.4.1760861. [DOI] [PubMed] [Google Scholar]
- 57.RSNA. [Accessed March 23, 2015];RSNA image share. Available at: https://www.rsna.org/Image_Share.aspx.
- 58.Heisey-Grove D, Patel V. Physician motivations for adoption of electronic health records. Washington, DC: Office of the National Coordinator for Health Information Technology; 2014. [Google Scholar]
- 59.Landro L. Image sharing seeks to reduce repeat scans. [Accessed November 5, 2015];The Wall Street Journal. 2013 Available at: http://www.wsj.com/article_email/SB10001424127887323296504578396442302663234-lMyQjAxMTAzMDAwMjEwNDIyWj.html?mod=wsj_valettop_email.
- 60.Yeager D. Sharing images—a hospital and a radiology group tell how they utilize VNA to meet different needs. Radiol Today. 2013;14:18–21. [Google Scholar]
- 61.Kalia V, Carrino JA, Macura KJ. Policies and procedures for reviewing medical images from portable media: survey of radiology departments. J Am Coll Radiol. 2011;8:39–48. doi: 10.1016/j.jacr.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144:742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 63.Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Aff. 2015;34:477–483. doi: 10.1377/hlthaff.2014.0729. [DOI] [PubMed] [Google Scholar]
- 64.Rudin RS, Motala A, Goldzweig CL, Shekelle PG. Usage and effect of health information exchange: a systematic review. Ann Intern Med. 2014;161:803–811. doi: 10.7326/M14-0877. [DOI] [PubMed] [Google Scholar]
- 65.Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, Thrall JH. Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology. 2009;251:147–155. doi: 10.1148/radiol.2511081174. [DOI] [PubMed] [Google Scholar]