Abstract
Major depressive symptoms represent a significant risk for suicidal ideation and behavior. Given that suicide is fearsome, the interpersonal theory of suicide proposes that individuals who engage in suicidal behavior possess not only the desire to die, but also the acquired capability (AC) for suicide. This study examined whether major depressive episodes (MDEs) may be particularly relevant to suicidal behavior when considered in the context of AC. History of MDEs, AC, and suicide attempt history were examined in a large (n=3,377) sample of military members. Data were analyzed using hierarchical multiple regression. Results indicated that among individuals with high AC, the number of MDEs was significantly, positively associated with number of previous suicide attempts; MDEs were not significantly related to suicide attempt history among individuals with low AC. Findings held in the presence of robust covariates associated with suicidal behavior. Findings suggest that a history of MDEs alone may not indicate severe suicide risk – increased AC for suicide appears necessary for increased suicide risk. Implications for suicide treatment and prevention in military personnel are discussed.
Keywords: military, suicide, major depressive episodes, acquired capability for suicide
Since early 2000, deaths by suicide in the United States (US) Army have maintained an upward trajectory (LeardMann et al., 2013) – suicide rates in the military doubled between 2003 and 2008 and, despite a recent decrease, exceed the rates of suicide in matched civilian populations (Kessler et al., 2013; Kuehn, 2009; Schoenbaum et al., 2014; Street et al., 2015; World Health Organization, 2014). Given the pervasiveness of suicide-related behaviors and deaths in the military (Kang & Bullman, 2009), identification of individuals who are most likely to engage in suicide-related behaviors is a high priority so these individuals can be more closely monitored, assessed, and treated.
Major depressive disorder, which is characterized by the occurrence of one or more major depressive episodes (MDEs) lasting a minimum of two weeks (American Psychiatric Association [APA], 2000), is a frequently cited and significant risk factor for suicidal ideation and behavior in the military (Gadermann et al., 2012). Despite evidence supporting the role of MDEs in conferring risk for suicide in the military, few people who experience MDEs go on to attempt or die by suicide (Harkavy-Friedman, Nelson, Venarde, & Mann, 2004; see also Klonsky & May, 2014 for discussion of ideation to action). Evidence from large epidemiological studies suggest that while a history of MDEs distinguishes individuals with no history of suicidal symptoms from those who think about suicide, MDEs are poor indicators of the transition between suicidal thoughts and suicidal behaviors (Kessler, Borges, & Walters, 1999; Nock, Borges, & Ono, 2012; Nock et al., 2013). Consequently, there is a need for a greater understanding of the role of MDEs in conferring risk for suicidal ideation and behaviors in military members.
The interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010), which distinguishes suicidal desire and capability, provides a useful framework for understanding the role of MDEs in suicidal ideation and behavior. The interpersonal theory of suicide postulates that lethal or near-lethal suicide attempts occur when individuals express suicidal desire, which the theory posits stems from thwarted belongingness and perceived burdensomeness, and have the capability to enact a serious suicide attempt. This capability for suicide exists partially through genetic traits and may be further developed through exposure to painful and provocative events that increase pain tolerance and decrease fear of death (Ribeiro et al., 2014; Smith et al., 2012; Van Orden et al., 2010). Importantly, the capability for suicide has been found to differentiate those who desire suicide but never attempt from those who desire suicide and do attempt and/or die by suicide (Smith, Cukrowicz, Poindexter, Hobson, & Cohen, 2010; Van Orden et al., 2010).
Military-related experiences, which may be both violent and life threatening, are exemplars of painful and provocative experiences that can increase pain tolerance and reduce fear of death. Therefore, it would follow that levels of acquired capability are particularly elevated in military populations. Indeed, compared to the general population, above average levels of acquired capability have been reported in military members (Bryan, Cukrowicz, West, & Morrow, 2010) and combat exposure has been proposed to increase risk for suicide through habituation to pain and fear of death (Anestis et al., 2009; Selby et al., 2010). Though military members have generally higher average levels of acquired capability, there is significant variability in levels of acquired capability among military members due to individual differences in experiences that fearlessness about death and pain tolerance (Smith & Cukrowicz, 2010). Higher levels of acquired capability among military personnel with a history of MDEs may influence the transition between suicidal ideation and suicidal behaviors.
Given that suicide attempt history is a strong predictor of future suicidal behavior (Nock, Hwang, Sampson, & Kessler, 2010), we analyzed the independent and interactive effects of MDEs and acquired capability on suicide attempt history in a large sample of military members. We hypothesized that the relationship between MDEs and previous suicide attempts would be dependent upon individual variation in capability for suicide, such that MDEs would be associated with increased suicide attempts in the presence of increased acquired capability. Furthermore, we expected that MDEs would be unrelated to suicide attempt history at low levels of capability for suicide. Additionally, we hypothesized that results would hold even after controlling for other prominent suicide risk factors (e.g., agitation, suicide-specific hopelessness).
Method
Participants and Setting
Participants included 3,377 military members (91.9% male, 8.1% female). Average age was 29.92 years (SD = 4.94; range 20 to 57). A majority (64.7%) of participants identified as White/Caucasian, 14.6% as Black/African-American, 13.2% as Hispanic/Latino, 2.7% as Asian, 1.5% as Native Hawaiian/Other Pacific Islander, and 1.1% as American Indian/Alaskan Native. Most (75.6%) participants were married, with 12.7% single, 7.9% divorced, and 1.5% engaged.
Procedure
Study participants were soldiers attending the United States Army Recruiting and Retention School at Ft. Jackson, South Carolina (e.g., Army Recruiters Course, Health Care Recruiters Course, Company Commanders’ Course). Data have suggested that this subset of military members may be particularly vulnerable to suicide (United States Army, 2010). No compensation was provided. All participants received a full explanation of study procedures and provided informed consent before participating in the study. Potential participants were given the option of completing study measures during the recruiter course orientation. Study participants completed a series of self-report measures as a part of a larger battery of orientation assessments. Both the Medical Research and Materiel Command Institutional Review Board (IRB) and Florida State University IRB approved all study procedures.
Materials
The following data were captured either from electronic records or from a basic computerized assessment: basic demographics (age, gender, ethnicity/race, marital status); existing “status” quo suicide risk assessment (including lifetime history of suicide attempts); and, current mental health diagnoses.
Major Depressive Episodes (MDEs)
Major depressive episodes were defined according to the DSM-IV-TR as periods of at least two weeks when an individual has a significantly depressed mood or loss of interest in enjoyable activities accompanied by several other symptoms including, but not limited to, sleep and appetite problems, feelings of guilt or worthlessness, and thoughts of suicide (APA, 2000). Chart diagnoses of lifetime history of MDEs based on a detailed clinical interview performed by a behavioral health provider (or psychiatrist, psychologist or clinical social worker) were derived from participant medical charts. Number of MDEs ranged from 0 to 13 (M = .17, SD = .57). Although the reliability of the chart diagnoses used in this study are unknown, previous research has indicated relatively high concordance between research and chart depressive diagnoses (e.g., Fennig, Craig, Tanenberg-Karant, & Bromet, 1994) and others have found similarly high concordance rates between chart and structured research diagnoses (Lonigan, Carey, & Finch, 1994; Joiner & Lonigan, 2000). In the present study, MDEs were entered as the predictor variable.
Acquired Capability for Suicide Scale (ACSS; Bender, Gordon, Bresin, & Joiner, 2011)
The ACSS was initially developed as a 20-item measure assessing self-reported fearlessness about death and physiological pain on a five-point Likert scale (0 = Not at all like me to 4 = Very much like me). The scale has recently been revised as a 7-item scale (ACSS-Fearlessness About Death [FAD]; Ribeiro et al., 2014). Higher total scores reflect greater capability for suicide. Previous research has supported the construct validity, convergent/divergent validity, and internal consistency of the 20-item (Bender et al., 2011) and abbreviated 5-item (Van Orden, Witte, Gordon, Bender, & Joiner, 2008) scale, as well as the newly revised ACSS-FAD (Ribeiro et al., 2014). An abbreviated four-item version of the ACSS was used in the current study and entered as a predictor variable. Internal consistency was acceptable (α = .76) in this study.
Brief Agitation Measure (BAM; Ribeiro et al., 2011)
The BAM was used as a self-report scale of agitation. The measure consists of three items rated on a 7-point Likert scale (1 = Not at all true for me to 7 = Very true for me), with higher scores indicating higher levels of agitation. Previous research has found strong internal consistency and validity (Ribeiro et al., 2011). Internal consistency was good (α = .85) in the current study. In the present study, the BAM was used to account for the relationship between agitation and suicide attempt history (Ribeiro et al., 2011).
Depressive Symptom Inventory – Suicidality Subscale (DSI-SS; Metalsky & Joiner, 1997)
The DSI-SS is a 4-item self-report measure assessing degree and severity of suicidal thoughts, plans, and urges. Items consist of a group of statements ranging on a scale from 0 to 3. Participants are asked to select the statement that best described them in the past two weeks. The DSI-SS has displayed strong psychometric properties (Metalsky & Joiner, 1997; Joiner, Pfaff, & Acres, 2002; Ribeiro, Braithwaite, Pfaff, & Joiner, 2012) among adolescents, young adults, and older adults. The DSI-SS demonstrated acceptable (α = .60) internal consistency in the current study.1 The DSI-SS was used to account for the relationship between suicidal ideation and suicide attempt history.
Insomnia Severity Index (ISI; Bastien, Vallières, & Morin, 2001)
The ISI is a 7-item measure designed to assess the severity of sleep difficulties in the past week. Respondents answer questions assessing insomnia, sleep satisfaction, noticeability of impairment, sleep problem-related worry/distress, and interference with daily functioning on a 5-point Likert scale ranging from 0 to 4. Adequate internal consistency and reliability has been reported for the ISI, as well as convergent validity and sensitivity in detecting sleep difficulty changes (Bastien et al., 2001; Morin, Belleville, Bélanger, & Ivers, 2011). An abbreviated 5-item version of the ISI was used in the current study (i.e., items assessing noticeability and worry/distress were not included) assessing sleep patterns in the last month. Internal consistency was good (α = .87) in the current study. The ISI was included as a covariate in the present analyses due to the relationship between insomnia and suicidal behavior (Pompili et al., 2013).
Suicide Cognition Scale (SCS; Rudd, Joiner, & Rajab, 2001)
The SCS is a 20-item measure of suicidal thinking and suicide-specific hopelessness, including core beliefs about helplessness, unlovability, and poor distress tolerance. Items are rated on a 5-point Likert scale, ranging from 1 (Strongly disagree) to 5 (Strongly agree). Higher total scores represent greater suicide-specific hopelessness. An abbreviated 10-item version of the SCS was used in the current study. Internal consistency was good (α = .86). The SCS was entered as a covariate given the relationship between suicide-specific hopelessness and suicide attempt history (Ellis & Rufino, 2015).
Statistical Approach
All analyses were conducted using SPSS Statistics 22. Missing data, which were minimal (< 3%), were addressed using listwise deletion. Bivariate correlations between all study variables were examined. Descriptive analyses were used to determine the presence of over-dispersion in our study variables. Hierarchical linear regressions predicting number of past suicide attempts were conducted.2 At the first step, number of past suicide attempts was predicted from the following covariates: age, gender, agitation, suicidal ideation, insomnia, and suicide-specific hopelessness. As described above, covariates were selected based on previous research indicating a link between these variables and suicide attempt history. At the second step, we added number of MDEs, acquired capability, and their centered interaction. To interpret the interaction, the simple effect of the number of MDEs on suicide attempt history was probed at high (1.5 SD above the mean) and low (1.5 SD below the mean) levels of acquired capability using hierarchical linear regressions.3
Results
Descriptive analyses indicated that the conditional variances of our main study variables were similar to their conditional means, which does not indicate that there is over-dispersion. Bivariate correlations among all variables, and variable means and standard deviations are presented in Table 1. Inter-correlations were found between many of the suicide predictors, though all were of small to moderate size. Notably, however, number of past suicide attempts significantly correlated only with number of MDEs (r = .114, p < .001) and levels of acquired capability (r = .052, p = .003). MDEs, in turn, correlated with all other variables except level of acquired capability. Acquired capability correlated only with number of past suicide attempts and insomnia (r = .102, p < .001).
Table 1.
Means, Standard Deviations, and Correlations between Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Suicide Attempts | - | ||||||
| 2. AC | .052* | - | |||||
| 3. MDE | .114** | −.011 | - | ||||
| 4. BAM | −.011 | .034 | .103** | - | |||
| 5. DSI-SS | .006 | .027 | .054* | .232** | - | ||
| 6. ISI | −.005 | .102** | .111** | .413** | .105** | - | |
| 7. SCS | −.007 | −.007 | .063** | .424** | .514** | .217** | - |
| Mean | .006 | 9.528 | .165 | 4.321 | .026 | 4.429 | 10.341 |
| Standard Deviation | .094 | 3.248 | .570 | 2.498 | .254 | 3.730 | 1.630 |
| n | 3385 | 3390 | 3384 | 3391 | 3387 | 3391 | 3391 |
Note.
p < 0.01
p < 0.001
AC = Acquired Capability; MDE = Major Depressive Episode; BAM = Brief Agitation Measure; DSI-SS = Depressive Symptom Inventory - Suicidality Subscale; ISI = Insomnia Severity Index; SCS = Suicide Cognitions Scale.
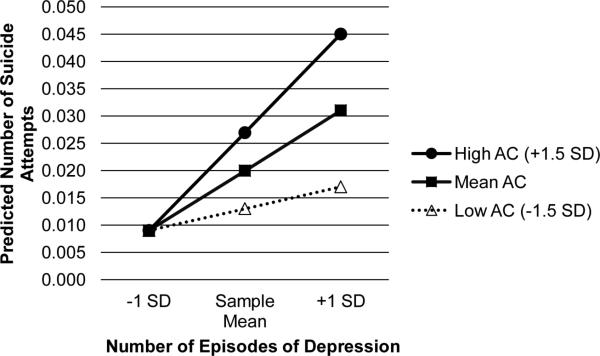
In the full model, findings indicated that MDEs (b = .019, p < .001, squared partial correlation (pr2) = .013) and level of acquired capability (b = .002, p = .001, pr2 = .002) significantly predicted number of past suicide attempts, above and beyond other suicide-related variables. As predicted, the interaction between number of MDEs and number of past suicide attempts was positive and significant, beyond main effects and covariates (b = .003, p = .009, pr2 = .002; see Table 2). First, the interaction was probed at high levels of acquired capability. In Step 1, covariates were entered, and in Step 2, number of MDEs, high levels of acquired capability, and their centered interaction were entered. As seen in Figure 1, at high levels of acquired capability, number of MDEs was a significant predictor of past suicide attempts (b = .032, p = <.001, pr2 = .013). Next, the interaction was probed at low levels of acquired capability. In Step 1, covariates were entered, and in Step 2, number of MDEs, low levels of acquired capability, and their centered interaction were entered. At low levels of acquired capability, number of MDEs was a non-significant predictor of past suicide attempts (b = .007, p = .25). Issues of multicollinearity between the covariates were likely not problematic, as all tolerance and VIF values in the models were greater than .10 and less than 10, respectively.
Table 2.
Hierarchical Linear Regression Predicting Number of Past Suicide Attempts
| Step 1 |
Step 2 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor Variables | b | SE | β | p | pr2 | b | SE | β | p | pr2 |
| Constant | .013 | (.012) | .26 | .014 | (.012) | .24 | ||||
| Age | <.001 | (<.001) | −.024 | .17 | <.001 | (<.001) | −.021 | .22 | ||
| Gender | .006 | .006 | .017 | .31 | .007 | .006 | .020 | .25 | ||
| BAM | <.001 | (.001) | −.009 | .66 | −.001 | .001 | −.018 | .38 | ||
| DSI-SS | .005 | (.007) | .013 | .50 | .002 | .007 | .006 | .75 | ||
| ISI | <.001 | (<.001) | −.056 | .96 | <.001 | <.001 | −.016 | .39 | ||
| SCS | −.001 | (.001) | −.010 | .63 | <.001 | .001 | −.006 | .79 | ||
| MDE | .019 | (.003) | .116 | < .001 | .013 | |||||
| AC | .002 | (.001) | .058 | .001 | .003 | |||||
| MDE × AC | .003 | (.001) | .045 | .008 | .002 | |||||
| R2 | .001 | .020 | ||||||||
| R2 Change | .001 | .018 | ||||||||
| F Change | .599 | 21.022 | ||||||||
| Significance F Change | .731 | <.001 | ||||||||
Note. Significant associations (i.e., p < .05) presented in bold; pr2 = squared partial correlation
Gender coded 0 = male, 1 = female; BAM = Brief Agitation Measure; DSI-SS = Depressive Symptom Inventory - Suicidality Subscale; ISI = Insomnia Severity Index; SCS = Suicide Cognitions Scale; MDE = Major Depressive Episodes; AC = Acquired Capability.
Figure 1.
Plot of the predicted number of past suicide attempts versus number of major depressive episodes (MDEs) at high (1.5 standard deviations below the mean) and low (1.5 standard deviations below the mean) levels of acquired capability (AC). At high levels of AC, number of MDEs was a significant predictor of past suicide attempts (b = .032, p = <.001, pr2 = .013). At low levels of AC, number of MDEs did not significantly predict past suicide attempts (b = .007, p = .25), as indicated by a dashed line.
Discussion
Major depressive symptoms represent a significant risk for suicide-related behaviors (Nock, Hwang, Sampson, & Kessler, 2010); however, less is known about the mechanisms contributing to this increased risk. Given that suicidal behaviors are fearsome, the interpersonal theory of suicide suggests that individuals who engage in lethal or near-lethal suicidal behavior possess not only the desire to die, but also the capability for suicide (i.e., fearlessness about death, increased pain tolerance; Joiner, 2005; Van Orden et al., 2010). Based on the interpersonal theory of suicide, the guiding hypothesis of this manuscript was that there would be a significant interaction between number of past MDEs and level of acquired capability in predicting number of past suicide attempts, such that number of past MDEs would predict past suicide attempts among those with high (but not low) levels of acquired capability. The present findings supported our a priori hypotheses.
As predicted, number of past suicide attempts increased as a function of the interaction between MDE history and acquired capability, such that number of past MDEs was only associated with number of past suicide attempts among those with high levels of acquired capability. For individuals with low level of acquired capability, the number of past MDEs was not significantly associated with number of past suicide attempts. Notably, findings held in the presence of robust covariates associated with suicidal behavior, including insomnia, agitation, suicide-specific hopelessness, and suicidal desire.
Several limitations should be considered when interpreting the present study findings. First, small effect sizes emerged for the main study findings. Despite small effect sizes for the association between the number of past suicide attempts and the interaction of MDEs and acquired capability (i.e., a total of only 2% of the variance in number of past suicide attempts was accounted for), the interaction was significant while controlling for several robust covariates. Additionally, caution should be exercised when generalizing the present findings to populations outside of military settings. Although higher levels of acquired capability are associated with the male gender (Bryan, Cukrowicz, West, & Morrow, 2010), due to the relatively low proportion of female participants (8.1%), our ability to test possible gender effects is limited. Additional studies are needed to test whether these results are replicable among other populations, including those with higher levels of acquired capability (e.g., female military personnel, police officers, other military samples), and civilian community and clinical samples. Furthermore, in the present study, acquired capability was measured currently, whereas number of MDEs and suicide attempts were assessed retrospectively. Therefore, we were unable to determine whether similar levels of acquired capability were present at the time of past MDEs. Although not available in the present study, future studies should account for the age of first suicide attempt as additional time may allow for a greater number of suicide attempts and, in turn, may directly influence acquired capability. While cross-sectional studies are valuable given the relatively low base rates of suicidal behavior, future studies replicating these results prospectively, using simultaneous measurements of these constructs over multiple time points, would be informative regarding temporal or causal associations.
Moreover, issues concerning perceived stigma or fear of the potential for negative consequences of reporting current or past suicide-related behavior have been found in some studies (e.g., Greene-Shortridge, Britt, & Castro, 2007). This may have contributed to under-reporting of suicide and suicide-related constructs in the present study. Consequently, it is also possible that soldiers who report higher acquired capability also report a greater number of past suicide attempts than those with lower capability. Given previous studies relying on self-report measures of suicide-related symptoms among military service members have repeatedly shown significant findings despite the potential for reporting bias (Bryan, Clemans, & Hernandez, 2012; Nademin et al., 2008), the effect is likely minimal. Nonetheless, future studies adopting approaches that minimize under-reporting in this population would be informative.
Moving forward, in addition to studies that extend the sample diversity, the duration and number of assessment time points, studies assessing the relationship between MDEs and suicidal behavior may benefit from integrating behavioral and self-report measures of the two components of acquired capability, fearlessness about death and pain tolerance (Van Orden et al., 2010), into experimental designs. For example, others have used a behavioral approach task designed to index fearlessness about death and a cold pressor task or computerized pressure algometer to measure pain tolerance (Franklin, Hessel, & Prinstein, 2011; Ribeiro, 2013). Further, research examining competing perspectives regarding the relationship between MDEs and suicidal ideation and behavior will be useful for furthering our understanding of their relationship (e.g., O'Connor, 2011).
Limitations considered, this study also had a number of strengths. This study's findings are based on a large sample size, which ensured this study had sufficient power ([1- β] > .99) despite small effect sizes. Furthermore, this study's sample restriction to military members, though potentially limiting generalizability, provides a critical spotlight of research on a specific population that may be at particularly high risk for suicide (United States Army, 2010). The findings of this study are directly applicable to military soldiers and military suicide in particular. Additionally, its implications may extend to other special populations that share similar demographic and cultural norms as the Army, including other mostly-male professions that involve high levels of risk and service, such as police officers, firefighters, and paramedics. Finally, this study demonstrated that findings were robust to the potential effects of a number of covariates, which themselves were all well associated with suicidal behavior.
The present results, should they be supported by future research, have important implications for treatment and prevention of suicide in military personnel. According to our results, a history of MDEs may not necessarily be indicative of high suicide risk, in the absence of high levels of acquired capability. However, importantly, the presence of a significant history of MDEs and high levels of acquired capability may signal the need for the regular assessment and monitoring of suicide risk. Therefore, although military members may be more capable of suicidal behaviors, it is only those who also believe they are a burden on others and are socially isolated who are most likely to engage in suicidal behaviors (Van Orden et al., 2010). From a clinical standpoint, given that combat veterans have a higher capability for suicide, endorsement of the experiences associated with suicidal desire should be considered an indication of significant suicide risk. Consequently, clinicians evaluating patients with a history of MDEs should routinely assess suicidal desire, particularly in military settings (e.g., Bryan, 2011). It would also be useful to consider using clinical interventions that treat or decrease the impact of major depressive symptoms and reduce the desire for suicide despite an increased acquired capability among patients with a history of MDEs.
Overall, the present study represents an effort to examine the role of major depressive symptoms in conferring risk for suicidal behavior from the perspective of the interpersonal theory of suicide. Many risk factors for suicide fail to distinguish those who think about suicide from those who engage in suicidal behaviors (Klonsky & May, 2014). However, this study provided evidence that while MDEs are associated with high levels of suicidal ideation (Kessler et al., 1999), high levels of acquired capability may distinguish military members with a history of MDEs who exhibit suicidal ideation from those who engage in suicidal behaviors. With the goal of improving suicide prevention and intervention in mind, we encourage future studies to examine and enhance our knowledge of the relationship between depressive symptoms, the capability for suicide, and suicidal behavior.
Acknowledgments
This work was in part supported by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-10-2-0181). Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the MSRC or the Department of Defense. This research was also partially supported by grants from the National Institute of Mental Health to Carol Chu (5 T32 MH093311-04) and Jennifer M. Buchman-Schmitt (5 T32 MH093311-04).
Footnotes
Disclosures: The authors declare that they have no conflicts of interest. Of note, these data have not been previously presented elsewhere.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the university and the United Stated Army Medical Department's institutional research boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Given previous research indicating strong internal consistency (Joiner, Pfaff, & Acres, 2002; Ribeiro, Braithwaite, Pfaff, & Joiner, 2012), a moderate alpha coefficient is notable. The lower alpha in the given sample may suggest an underreporting of suicide symptom severity (Nock et al., 2008).
Given that suicide attempt history may be treated as a count variable, we examined our data using a poisson regression. In this model, the predictors (acquired capability, MDEs, and their interaction), the criterion variable (suicide attempt history), and covariates were entered. The results from the poisson regression supported our findings: significant effects of acquired capability, MDEs, and their interaction were found (all p <.001). However, the goodness-of-fit chi-squared test was statistically significant, which suggests that the poisson regression does not fit our data well (Deviance =123.99, df = 3289, p = .038). Thus, multiple regression was selected to characterize the relationship between study variables.
Levels of acquired capability are traditionally higher among military personnel (Bryan, Cukrowicz, West, & Morrow, 2010). Thus, the interaction was probed at 1.5 SD to capture individuals with lower and higher levels of acquired capability. Notably, interactions were probed at 1 SD, and the pattern of results was the same, such that the simple effect of number of MDEs on suicide attempt history was greater at high levels of acquired capability.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders, text revision (DSM-IV-TR) American Psychiatric Association; 2000. [Google Scholar]
- Anestis MD, Bryan CJ, Cornette MM, Joiner TE. Understanding suicidal behavior in the military: An evaluation of Joiner's interpersonal-psychological theory of suicidal behavior in two case studies of active duty post-deployers. Journal of Mental Health Counseling. 2009;31(1):60–75. [Google Scholar]
- Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bender TW, Gordon KH, Bresin K, Joiner TE. Impulsivity and suicidality: The mediating role of painful and provocative experiences. Journal of Affective Disorders. 2011;129:301–307. doi: 10.1016/j.jad.2010.07.023. [DOI] [PubMed] [Google Scholar]
- Bryan CJ. The clinical utility of a brief measure of perceived burdensomeness and thwarted belongingness for the detection of suicidal military personnel. Journal of Clinical Psychology. 2011;67(10):981–992. doi: 10.1002/jclp.20726. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Clemans TA, Hernandez AM. Perceived burdensomeness, fearlessness of death, and suicidality among deployed military personnel. Personality and Individual Differences. 2012;52(3):374–379. [Google Scholar]
- Bryan CJ, Cukrowicz KC, West CL, Morrow CE. Combat experience and the acquired capability for suicide. Journal of Clinical Psychology. 2010;66(10):1044–1056. doi: 10.1002/jclp.20703. [DOI] [PubMed] [Google Scholar]
- Ellis TE, Rufino KA. A psychometric study of the Suicide Cognitions Scale with psychiatric inpatients. Psychological Assessment. 2015;27(1):82–89. doi: 10.1037/pas0000028. [DOI] [PubMed] [Google Scholar]
- Fennig S, Craig TJ, Tanenberg-Karant M, Bromet EJ. Comparison of facility and research diagnoses in first-admission psychotic patients. The American Journal of Psychiatry. 1994;151:1423–1429. doi: 10.1176/ajp.151.10.1423. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Hessel ET, Prinstein MJ. Clarifying the role of pain tolerance in suicidal capability. Psychiatry Research. 2011;189(3):362–367. doi: 10.1016/j.psychres.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Gadermann AM, Engel CC, Naifeh JA, Nock MK, Petukhova M, Santiago LPN, Wu B, Zaslavsky AM, Kessler RC. Prevalence of DSM-IV major depression among US military personnel: meta-analysis and simulation. Psychological Health and Traumatic Brain Injury. 2012;177(8):47–59. doi: 10.7205/milmed-d-12-00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene-Shortridge TM, Britt TW, Castro CA. The stigma of mental health problems in the military. Military Medicine. 2007;172(2):157–161. doi: 10.7205/milmed.172.2.157. [DOI] [PubMed] [Google Scholar]
- Harkavy-Friedman JM, Nelson EA, Venarde DF, Mann JJ. Suicidal behavior in schizophrenia and schizoaffective disorder: examining the role of depression. Suicide and Life-Threatening Behavior. 2004;34(1):66–76. doi: 10.1521/suli.34.1.66.27770. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Joiner TE, Lonigan CJ. Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology. 2000;29(3):372–382. doi: 10.1207/S15374424JCCP2903_8. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Pfaff JJ, Acres JG. A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behaviour Research and Therapy. 2002;40:471–481. doi: 10.1016/s0005-7967(01)00017-1. [DOI] [PubMed] [Google Scholar]
- Kang HK, Bullman TA. Is there an epidemic of suicides among current and former US military personnel? Annals of Epidemiology. 2009;19(10):757–760. doi: 10.1016/j.annepidem.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56(7):617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Colpe LJ, Fullerton CS, Gebler N, Naifeh JA, Nock MK, Heeringa SG. Design of the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). International Journal of Methods in Psychiatric Research. 2013;22(4):267–275. doi: 10.1002/mpr.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research. Suicide and Life-Threatening Behavior. 2014;44(1):1–5. doi: 10.1111/sltb.12068. [DOI] [PubMed] [Google Scholar]
- Kuehn BM. Soldier suicide rates continue to rise. JAMA: The Journal of the American Medical Association. 2009;301(11):1111–1113. doi: 10.1001/jama.2009.342. [DOI] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hoge CW. Risk factors associated with suicide in current and former US military personnel. JAMA. 2013;310(5):496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Carey MP, Finch AJ. Anxiety and depression in children and adolescents: negative affectivity and the utility of self-reports. Journal of Consulting and Clinical Psychology. 1994;62(5):1000–1008. doi: 10.1037//0022-006x.62.5.1000. [DOI] [PubMed] [Google Scholar]
- Metalsky GI, Joiner TE. The hopelessness depression symptom questionnaire. Cognitive Therapy and Research. 1997;21:359–384. [Google Scholar]
- Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nademin E, Jobes DA, Pflanz SE, Jacoby AM, Ghahramanlou-Holloway M, Campise R, Johnson L. An investigation of interpersonal-psychological variables in air force suicides: A controlled-comparison study. Archives of Suicide Research. 2008;12(4):309–326. doi: 10.1080/13811110802324847. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Ono Y, editors. Suicide: Global perspectives from the WHO World Mental Health Surveys. Cambridge University Press; New York: 2012. [Google Scholar]
- Nock MK, Deming CA, Fullerton CS, Gilman SE, Goldenberg M, Kessler RC, Ursano RJ. Suicide among soldiers: A review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. doi: 10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor RC. Towards an integrated motivational–volitional model of suicidal behaviour. International handbook of suicide prevention: Research, policy and practice. 2011:181–198. [Google Scholar]
- Pompili M, Innamorati M, Forte A, Longo L, Mazzetta C, Erbuto D, Girardi P. Insomnia as a predictor of high-lethality suicide attempts. International Journal of Clinical Practice. 2013;67(12):1311–1316. doi: 10.1111/ijcp.12211. [DOI] [PubMed] [Google Scholar]
- Ribeiro J. Acute overarousal and the acquired capability for suicide: understanding acute suicide risk through the lens of the interpersonal theory of suicide (Unpublished doctoral dissertation) Florida State University; Tallahassee, FL.: 2013. [Google Scholar]
- Ribeiro JD, Bender TW, Selby EA, Hames JL, Joiner TE. Development and validation of a brief self-report measure of agitation: The brief agitation measure. Journal of Personality Assessment. 2011;93:597–604. doi: 10.1080/00223891.2011.608758. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Braithwaite SR, Pfaff JJ, Joiner TE. Examining a brief suicidal screening tool in older adults engaging in risky alcohol use. Suicide and Life-Threatening Behavior. 2012;42:405–415. doi: 10.1111/j.1943-278X.2012.00099.x. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Witte TK, Van Orden KA, Selby EA, Gordon KH, Bender TW, Joiner TE. Fearlessness about death: The psychometric properties and construct validity of the revision to the acquired capability for suicide scale. Psychological Assessment. 2014;26:115–126. doi: 10.1037/a0034858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd MD, Joiner TE, Rajab MH. Treating suicidal behavior: An effective, time-limited approach. Guilford Press; 2004. [Google Scholar]
- Schoenbaum M, Kessler RC, Gilman SE, Colpe LJ, Heeringa SG, Stein MB, Cox KL. Predictors of suicide and accident death in the army study to assess risk and resilience in servicemembers (Army STARRS): Results from the army study to assess risk and resilience in servicemembers (Army STARRS). JAMA Psychiatry. 2014;71(5):493–503. doi: 10.1001/jamapsychiatry.2013.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, Ribeiro JD, Nock MK, Rudd MD, Joiner TE. Overcoming the fear of lethal injury: Evaluating suicidal behavior in the military through the lens of the Interpersonal-Psychological Theory of Suicide. Clinical Psychology Review. 2010;30(3):298–307. doi: 10.1016/j.cpr.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PN, Cukrowicz KC. Capable of suicide: A functional model of the acquired capability component of the interpersonal-psychological theory of suicide. Suicide and Life-Threatening Behavior. 2010;40(3):266–274. doi: 10.1521/suli.2010.40.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PN, Cukrowicz KC, Poindexter EK, Hobson V, Cohen LM. The acquired capability for suicide: A comparison of suicide attempters, suicide ideators, and non-suicidal controls. Depression and Anxiety. 2010;27(9):871–877. doi: 10.1002/da.20701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AR, Fink EL, Anestis MD, Ribeiro JD, Gordon KH, Davis H, Joiner TE. Exercise caution: Over-exercise is associated with suicidality among individuals with disordered eating. Psychiatry Research. 2013;206(2):246–255. doi: 10.1016/j.psychres.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Gilman SE, Rosellini AJ, Stein MB, Bromet EJ, Cox KL, Kessler RC. Understanding the elevated suicide risk of female soldiers during deployments. Psychological Medicine. 2015;45:717–726. doi: 10.1017/S003329171400258X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Army Health promotion, risk reduction, and suicide prevention report. 2010 Available at: http://csf.army.mil/downloads/HP-RR-SPReport2010.pdf.
- Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the interpersonal needs questionnaire. Psychological Assessment. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Curkrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- World Health Organization [Feb. 26, 2015];Preventing suicide: A global imperative. 2014 Retrieved from: http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/