Abstract
Introduction
Initiation of class III anti-arrhythmic medications requires telemetric monitoring for ventricular arrhythmias and QT prolongation to reduce the risk of torsades de pointes (TdP). Heart rate-corrected QT interval (QTc) is an indicator of risk, however it is imperfect, and subtle abnormalities of repolarization have been linked with arrhythmogenesis.
Purpose
Identification of electrocardiographic predictors of torsadogenic risk through the application of a novel T wave analysis tool
Methods
Among all patients admitted to Mayo Clinic for initiation of dofetilide or sotalol, we identified 13 cases who developed drug-induced TdP and 26 age and sex matched controls that did not develop TdP. The immediate pre-TdP ECG of those with TdP was compared to the last ECG performed prior to hospital discharge in controls using a novel T wave program that quantified subtle changes in T wave morphology.
Results
The QTc and 12 T wave parameters successfully distinguished TdP cases from controls. The top performing parameters were the QTc in lead V3 (mean case vs control 480 vs 420 msec, p < 0.001, r=0.72) and T wave right slope in lead I (mean case vs control −840.29 vs −1668.71 mV/sec, p= 0.002, r=0.45). The addition of T wave right slope to QTc improved prediction accuracy from 79 to 88%.
Conclusion
Our data demonstrate that, in addition to QTc, the T wave right slope is correlated strongly with TdP risk. This suggests that a computer-based repolarization measurement tool that integrates additional data beyond the QTc may identify patients with the greatest torsadogenic potential.
Keywords: Class III antiarrhythmics, torsade de pointes, risk stratification, T wave analysis, electrocardiography
Introduction
Sotalol and dofetilide (Class III anti-arrhythmic drugs [AADs]) are used commonly to maintain sinus rhythm in patients with atrial fibrillation [1]. Initiation of these medications requires serial 12-lead ECGs with QTc measurement until a steady-state drug level is achieved in order to reduce the risk of torsades de pointes (TdP), a potentially fatal side effect of these medications [2]. The risk of TdP with sotalol and dofetilide is 1–4% [3–5] and 2–3% [6, 7], respectively. The QTc is a well-established indicator of TdP risk but it does not fully account for all risk [2, 8, 9].
T wave changes are described in patients taking Class III agents [10, 11], but the relationship between individual T wave abnormalities and torsadogenic risk is unknown. The T wave arises due to differential repolarization characteristics of endocardial, midmyocardial and epicardial myocytes. While QTc provides useful information, it reduces to a single measurement complex three dimensional myocardial electrophysiological voltage gradients that change in response to a drug. We hypothesize that novel digital signal processing-based T wave morphologic analysis of the surface ECG may provide insight into subtle changes in T waves that may be linked to arrhythmogenesis [12–14]. The aim of this project was to improve risk stratification of patients loaded with sotalol and dofetilide by identifying novel electrocardiographic predictors of TdP.
Methods
Study Population
We performed a retrospective analysis of patients admitted to the Mayo Clinic in Rochester, MN, for initiation of dofetilide and sotalol from 1st January 2004– 1st January 2014. Cases were identified by a keyword search of the electronic medical record using a query-building tool (Data Discovery and Query Builder). The following keywords were combined with “sotalol” and “dofetilide”; “torsade de pointes”, “torsade de pointe”, “torsade”, “torsades”, “polymorphic ventricular tachycardia”, and “polymorphic VT”. Patients were included if they met all of the following criteria: 1) admitted for initiation of either sotalol or dofetilide as their AAD, 2) serial ECGs performed, 3) documentation of TdP. Patients were excluded if the ECG had a paced rhythm, if the drug was stopped due to excessive QT prolongation, or patients were taking the drug chronically. Age- and sex-matched controls were identified in a 2:1 ratio from a population of patients who received sotalol or dofetilide loading but did not develop TdP. Echocardiogram data closest to admission date was collected. The Mayo Clinic Institutional Review Board approved this study.
Electrocardiographic analysis
All ECGs obtained during the admission for AAD loading were selected and analyzed. The ECG recorded closest to the TdP event among the cases was selected for the primary analysis. For the controls (i.e. AAD loaded but without TdP), the ECG before discharge (at steady state of the maximum tolerated dose) was compared with pre-TdP ECG in the cases. The ECG analysis was performed using software that we developed specifically for this study (detailed below). The following ECG features were analyzed:
T-wave left/right slope, T-wave amplitude, T-wave enclosed area, x/y coordinates of the center of gravity (COG) of the first 25% of a T-wave (T1), x/y coordinates of COG of the last 25% of a T-wave (T4), QT interval, QTc value (Bazett’s heart rate corrected) and Tpeak-Tend (Tpe) interval.
Software development
We developed a software package in MATLAB (version 2013b, Mathworks Inc. Natick, MA) to facilitate the T-wave analysis. The software provides automatic 12-lead ECG feature extraction followed by an intuitive and interactive way to analyze the T-wave properties of short-term 12-lead ECG data sets measured under current clinical conditions. The block diagram of the workflow is shown in Figure 1 (supplementary file).
The raw, 12-lead ECG tracings (10 second duration, fs = 500 samples/second) collected from the General Electric MUSE ECG management system (GE Healthcare, Waukesha, WI) were uploaded into our software tool [15]. Pre-processing procedures are applied including de-noising and baseline correction, both based on wavelet transformations described by Clifford et al [16]. Pre-processing is followed by ECG feature extraction using our software program. ECG features (mentioned above) from the ECG are detected by a Bayesian statistical peak delineation algorithm [17]. The COGx is calculated by a polygonal method (Figure 2 -supplemental file). Detected T-waves with inconsistent locations (outliers) compared to other cardiac cycles were excluded manually from the analysis (Figure 3- supplemental file, shows an example of such manual adjustments). When all the outliers are removed, ECG features are calculated and exported to CSV file for statistical analysis.
Statistical Analysis
A univariate two-sample t-test was used to pre-select features that showed statistically significantly different means by case status. Features whose mean significantly (p < 0.05) differed between cases and controls underwent further analysis. In order to select independent features, Pearson’s correlation coefficient was used to examine correlation between pre-selected features. A filter approach was used to find the features with highest correlation with case status (i.e. dofetilide/sotalol-induced TdP) while having low mutual correlation between features. A mutual correlation threshold of features was chosen to be |ρ<0.6|. Multivariable analysis was performed on the features selected via the filter approach. Simultaneously, an advanced method for feature selection using linear discriminant analysis (LDA) as a wrapper was used in order to compare results with the previous method. The LDA method calls a Forward Sequential Feature Selection (FSFS) in a wrapper fashion. The performance of LDA was tested using 10×10 fold cross-validation. To evaluate and compare performance of features selected by the filter approach and FSFS a 10×10 fold cross-validation using the LDA classifier was also used for features selected by filter approach.
Results
Patient Characteristics
Thirty-nine dofetilide/sotalol-loaded patients (13 cases, 26 controls) underwent advanced T wave analysis for assessment of TdP predictive markers. There were no statistically significant baseline differences observed between cases and controls (Table 1). This cohort was predominantly female (75% in the sotalol group and 80% in the dofetilide group), and had an average age of 60.3 ± 14.5 years (sotalol group) and 68.0 ± 5.5 years (dofetilide group). All patients had sinus rhythm documented on the ECG preceding TdP. 26 patients (66.7%) received either sotalol or dofetilide for atrial fibrillation, 7 (17.9%) for atrial flutter, 4 (10.2%) for ventricular ectopy and 2 (5.1%) for ventricular tachycardia. The mean dose received before the event was 95 ± 19 mg in the sotalol group and 375 ± 158 mg in the dofetilide group. No patient had a previous history of TdP. Average duration before TdP occurred was 3.2 days (±1.8). The average time from analyzed ECG to occurrence of Tdp was 160 minutes (range, 9–568). Mean ejection fraction was 43.1% (±18.2) in the sotalol group that experienced TdP and 48% (±14.5) in dofetilide.
Table 1.
Baseline Characteristics
| Sotalol (n = 24) |
Dofetilide (n= 15) |
|||
|---|---|---|---|---|
| Cases | Controls | Cases | Controls | |
| n | 8 | 16 | 5 | 10 |
| Age, years (±SD) | 60.3 (14.5) | 61.4 (14.0) | 68.4 (5.5) | 68.0 (5.4) |
| Women, n (%) | 6 (75%) | 12 (75%) | 4 (80%) | 8 (80%) |
| Ejection Fraction, % (±SD) | 43.1 (18.2) | 52.0 (11.5) | 48.0 (14.5) | 68.7 (18.2) |
| Mean drug dose before event/discharge (±SD) | 95(19.4) | 104.6(26.1) | 375(158.1) | 400(122.5) |
| Index rhythm, n (%) | ||||
| Atrial Fibrillation | 2 (25%) | 6 (37.5%) | 4 (80%) | 5 (50 %) |
| Atrial Flutter | 3 (37.5%) | 1 (6.25%) | 1 (20%) | 1 (10 %) |
| Sinus Rhythm | 3 (37.5%) | 5 (31.25%) | 0 (0%) | 4 (40%) |
| Rhythm before event | ||||
| Sinus Rhythm | 8 (100%) | - | 5 (100%) | - |
| Time to event/discharge, days (±SD) | 3.1 (1.8) | 2.6(0.7) | 3.3(2.3) | 2.2(0.4) |
| Time from analyzed ECG to Tdp, mins (range) | 113.5 (13-207) | 199.3 (9-568) | ||
| Lab values, (±SD) | ||||
| Potassium, mmol/L | 4.2 (0.5) | 4.2 (0.3) | 4.4 (0.4) | 4.2 (0.3) |
| Magnesium, mg/dL | 2.0 (0.3) | 2.0 (0.2) | 2.0 (0.2) | 2.0 (0.2) |
| Medications (%) | ||||
| Beta Blockers | 3 (37.5%) | 7 (43.75%) | 1 (20%) | 5 (50%) |
| ACE inhibitors | 1 (12.5%) | 7 (43.75%) | 1 (20%) | 5 (50%) |
| Calcium Channel Blocker | 1 (12.5%) | 2 (25%) | 0 (0%) | 3 (33.3%) |
| Digoxin | 1 (12.5%) | 1 (6.25%) | 2 (40%) | 1 (10%) |
| Thiazide Diuretic | 1 (12.5%) | 0 (0%) | 0 (0%) | 4 (40%) |
| Loop Diuretic | 3 (37.5%) | 5 (31.3%) | 4 (26.7%) | 3 (33.3%) |
T Wave Characteristics
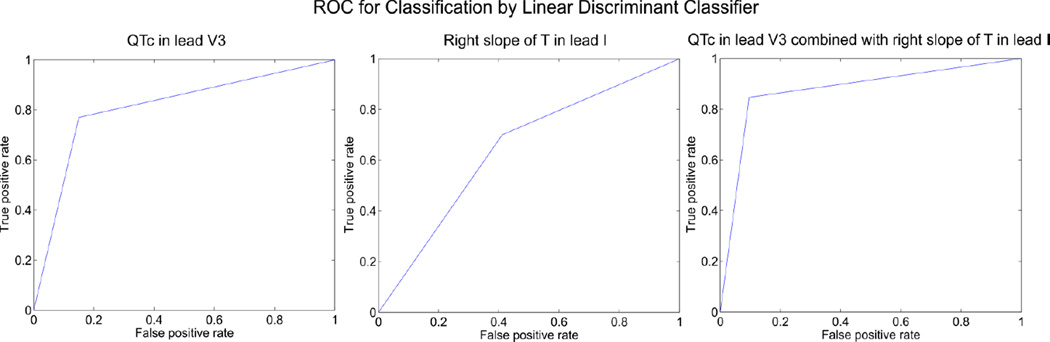
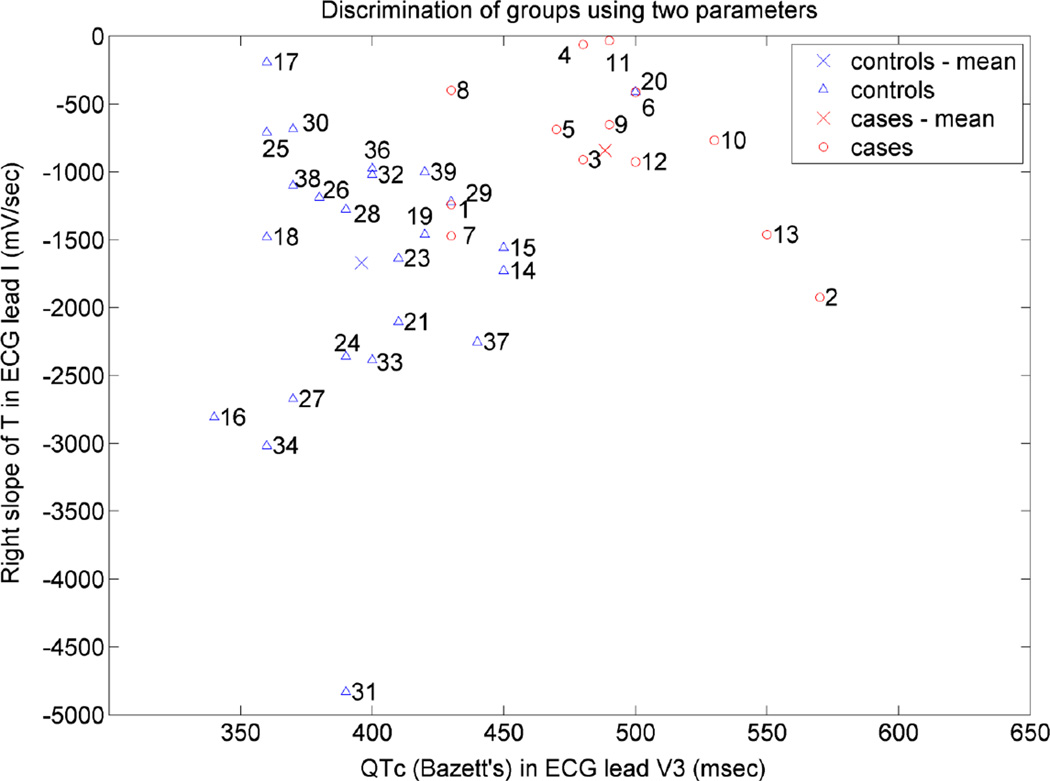
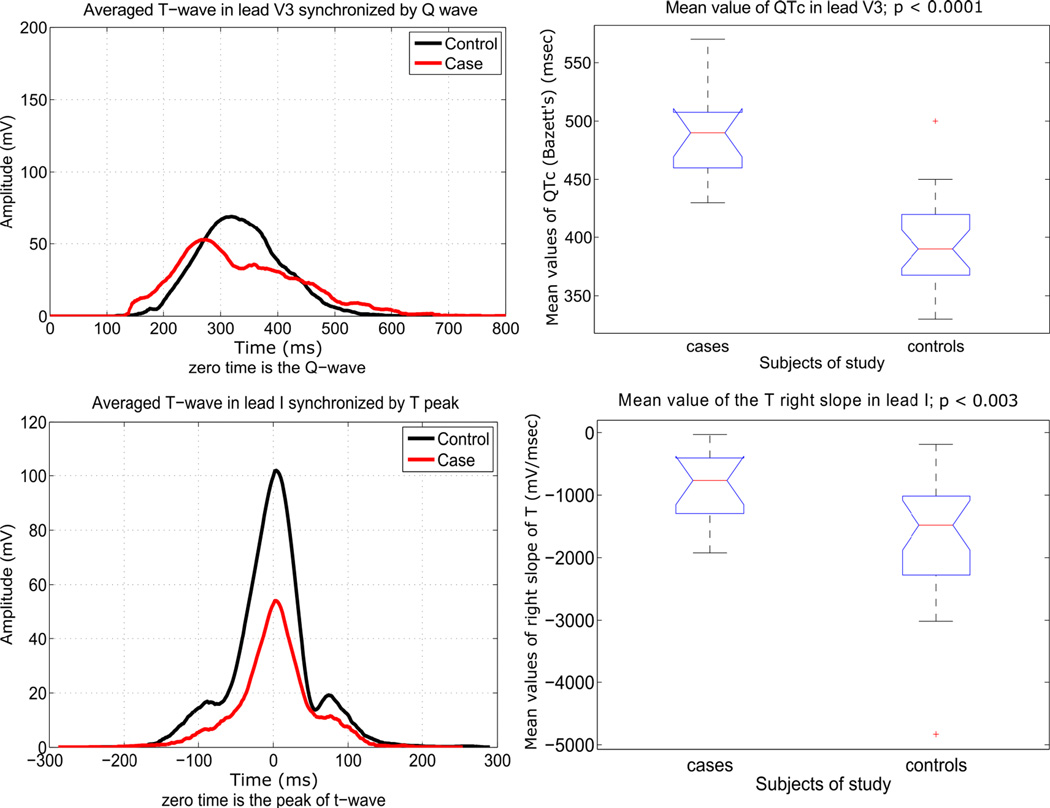
Significant differences in T wave repolarization were observed across 13 study variables (Table 1 - Supplemental file). QTc, QT, COG x-axis (COGx) and COGxT4 were the only variables that had differences observed in all 12 ECGs leads (except Lead I QTc). The QTc and QT interval were longer and the COGx larger (further) on the x-axis in those that experienced TdP compared to controls. Notably, eight of 13 (61.5%) cases did not have a QTc > 500msec on the ECG preceding TdP. T wave parameters were correlated strongly to TdP and the top selected parameters were the QTc in lead V6 (mean case vs. control 500 ± 44 vs. 410 ± 38 msec, p<0.001, r=0.77) and the T wave right slope in aVR (mean case vs. control −682.88 ± 38 vs −1509.53 ± 44 mV/sec, p<0.001, r=0.56). Lead V3 QTc (mean case vs control 480 ± 48 vs 420 ± 30 msec, p < 0.001, r=0.72) and T wave right slope in lead I (mean case vs control 840.29 ± 565 vs −1668.71 ± 933 mV/sec, p= 0.002, r=0.45) produced parallel strong correlation (classification ability 88%) and were selected for further discriminatory analysis. QTc alone could only discriminate torsadogenic cases from non-torsadogenic controls in 79%. With addition of the T wave right slope, this discrimination increased to 88%, suggesting an additive value in risk prediction with the use of T wave right slope (Figure 4 - Supplemental figure shows the LDA equation giving such classification). Receiver Operating Curve (ROC) analysis of the 2 selected variables, a QTc of 434 msec and T wave right slope of −1199 mV/sec provided a 92.1% sensitivity and 81.4% specificity in the prediction of TdP. The positive and negative predictive values were 90.3% and 84.6%, respectively. By themselves, QTc had a sensitivity of 88.1 %, 72.0 % specificity, a PPV of 85.0% and NPV of 76.9%. T wave right slope was 79.7 % sensitivity, 46.0% % specificity in predicting TdP with a PPV of 58.9%, NPV 70.0%. Figure 1 highlights the ability of QTc in Lead V3 and T wave right slope Lead I to discriminate cases and controls. Figure 2 further provides a visual representation of the distribution of QTc in Lead V3 and T wave right slope Lead I in cases and controls. At baseline the QTc and T wave right slope could not differentiate between cases and controls (p>0.05) with Figure 5 – Supplementary file showing the longitudinal changes in QTc and T wave right slope over time.
Figure 1.
ROC classification of the ECG features
A. ROC curve for QTc, AUC= 0.8096
B. ROC curve for T wave right slope. AUC =0.6442
C. ROC curve for QTc and T wave right slope. AUC =0.8750
Comparison of mean values of Lead V3 - QTc and Lead I - T wave right slope, cases vs controls. This is data analysed from the ECG closest to the Tdp event (case) or dismissal (control)
Figure 2.
ECG average tracings and box plots. Above, QTc (synchronised by Q wave), below T wave right slope (synchronised by T wave)
Discussion
Using our newly developed T wave analysis tool, we found electrocardiographic markers of TdP risk in patients being loaded with sotalol or dofetilide. Several T wave indices significantly differ from controls. Specifically, the QTc in Lead V3 and the right slope of the T wave in Lead I were most strongly correlated with TdP, and, together, could discriminate the majority of TdP cases from controls (classification error 12%). These indices have the potential to augment current risk stratification, which is based primarily on serial QTc measurements.
Sotalol and dofetilide prolong repolarization through inhibition of KCNH2-encoded Kv11.1 (HERG) channels (IKr currents) and confer an increased risk of drug-induced-TdP. Although the degree of QT prolongation is an imperfect surrogate for torsadogenic potential [15, 18–20] (the risk of TdP is neither a linear function of the baseline QT interval nor of the extent of QT-interval prolongation during drug administration) [9], it is important to note that the QTc strongly correlated with TdP events in our cohort. In general, a QTc > 500 ms is associated with a higher risk of lethal arrhythmias [21–23], and a QTc > 500ms 2 hours after dosing is an indication to stop or reduce the dose of sotalol or dofetilide. However, 8/13 (61.5%) of the TdP cohort did not have a QTc > 500msec on the ECG preceding TdP. Thus, this 500 msec QTc threshold may not completely identify those at risk. The average QTc in our cohort across all leads in the ECG preceding TdP was 480 msec (most patients were female, in whom the guideline definition of a prolonged QTc is 460ms). This supports the hypothesis that although the QTc is a partial surrogate marker (able to successfully distinguish torsadogenic cases vs non-torsadogenic controls in 79%), there is a need for additional risk factor identification.
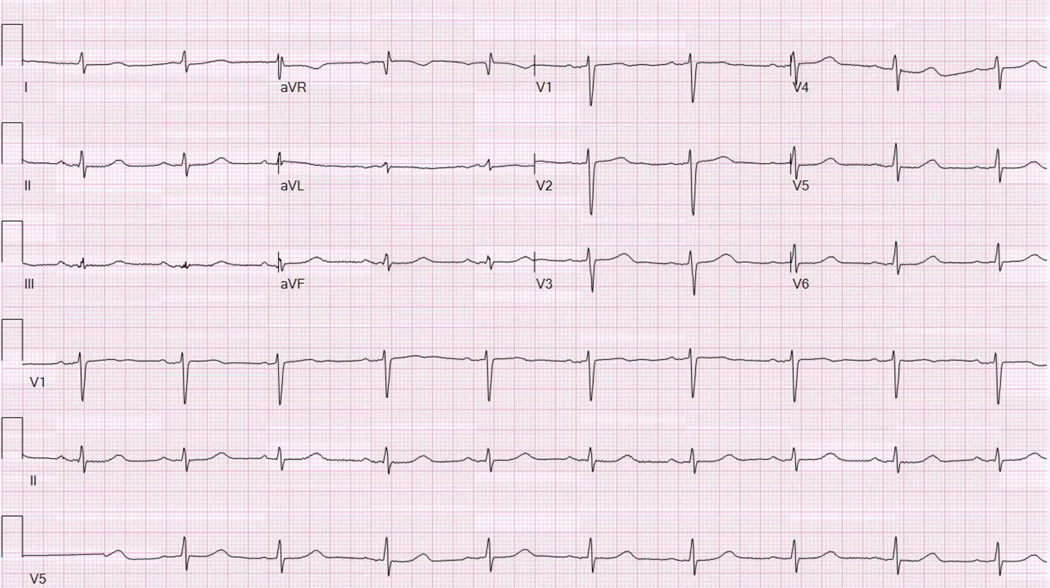
The T wave right slope in Lead I is a novel marker for sotalol/dofetilide induced-TdP. In our cohort, T wave right slope in Lead I correlated highly with arrhythmia risk and provided an additive effect in discriminating cases from controls. The additive ability of T wave right slope lays in its ability to out rule individuals at risk of Tdp due to its high sensitivity and negative predictive value. This slope is essentially a function of the amplitude of the T wave as well as the duration of the terminal portion of the wave. The TdP patients in the cohort had shallow or ‘less steep’ right slopes compared to their age and sex matched controls (r= 0.45). Figure 3 A and B provide a visual representation of this shallow T wave. The shallow T wave may reflect greater dispersion of refractoriness in both the repolarisation of the transmural gradients (endocardial, midmyocardial, and epicardial cells) with a contributory role-played by apicobasal gradient. With regard to the components that make up the slope of the T wave, we did observe a nonsignificant trend towards lower T wave amplitudes in those who experienced TdP. Reduction in T wave amplitude has been well described with sotalol administration [10, 24, 25], and also reported in congenital LQT2 patients [26–28] (who have IKr loss-of-function), but we are the first to propose its potential to predict arrhythmia risk. The reason for the reduction in the T wave has yet to be defined. Bhuiyan et al [29] suggested that flattening of the T wave is a reflection of prolongation of action potential triangulation. Triangulation is defined by the time between 30% repolarization and 90% repolarization of the monophasic action potential. A study using the HERG blocker Sertindole showed that the T wave attained minimum height just before the onset of TdP [30]. A shallow right T slope would also suggest that there is prolonged repolarization of the end of the T wave. The Tpe interval is considered a good marker for arrhythmogenic risk [31, 32]. Prolongation of this interval increases the period when potential fatal re-entry ventricular tachycardias can occur and has been shown to be associated with increased risk of mortality and ventricular arrhythmias in long QT syndromes [33], hypertrophic cardiomyopathy [34], patients receiving primary percutaneous coronary intervention for an MI [35], and Brugada syndrome [31]. Here, however, Tpe failed to distinguish cases from controls (Table 2 –supplementary file). While it is unclear why the T wave right slope proved superior to Tpe, one possibility may be that the end of the T wave can be difficult to define consistently, particularly in the setting of antiarrhythmic drugs, and the slope determination may be more robust in this regard.
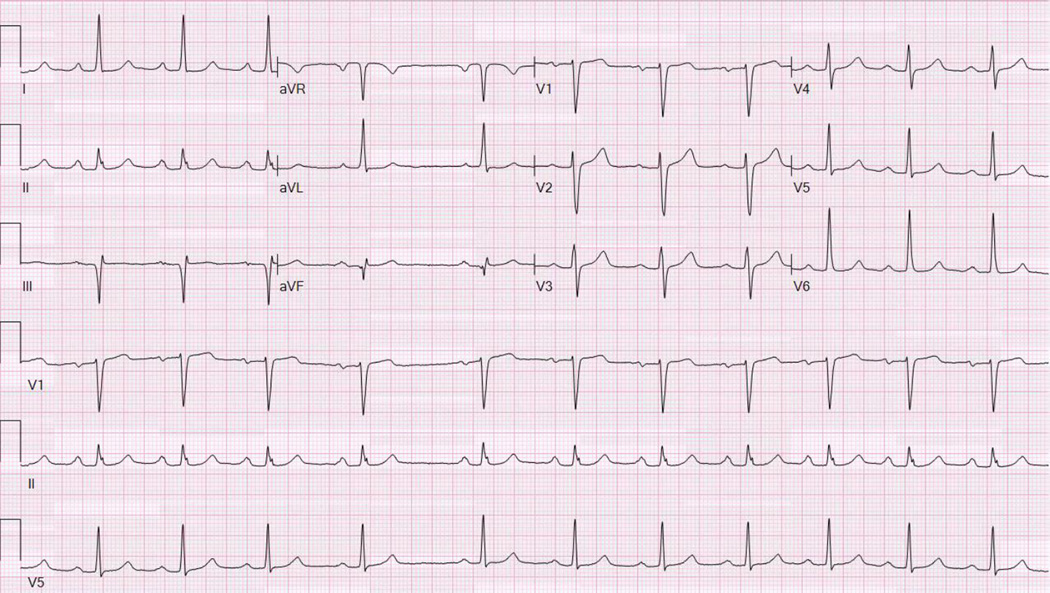
Figure 3.
A - ECG from Tdp case. This highlights a shallow T wave right slope, especially visible in Lead I (when compared to ECG of age and sex match control of Figure 3 B)
B - ECG from age and sex matched control. Note the T wave right slope is steeper when compared to Figure 3A (Tdp case).
It is important to note that there were no differences in QTc and T wave right slope at baseline between cases and controls. This would suggest that the risk of Tdp is due to an individual’s response to class III AADs rather than baseline electrical substrate abnormalities. Figure 5 – Supplementary file highlights this concept, as it shows subtle differences that exist between cases and controls in the analysis of serial ECGs. The top two graphs show the QTc over time. In those that experienced TdP, the average tracing shows an initially gradual, logarithmic increase in QTc towards TdP compared to those that did not experience TdP, in which the QTc has a fairly steady and predictable course. The bottom two graphs show changes in the T wave right slope of Lead I. This shows a clustering to the top right of the graph in those that experienced TdP, suggestive of a “shallow” T wave, compared to controls, which showed a varied response, and no clear underlying pattern.
The Center of gravity (COG), which is derived from mean x and y coordinates of the T wave, is an innovative T wave index that we have demonstrated has potential to account for subtle variations in the T wave [36]. Although the COGx was not selected as our top two correlated variables, there were statistically significant differences between the TdP cases and controls across all ECG leads, where the COGx was longer in all cases (Table 1 – Supplementary File). We postulate that the increase in COG on the x axis in TdP is due to a T wave that is flatter and slightly longer, and thus the COG is able to take into account subtle repolarization variations. This new index has the potential to be a significantly more comprehensive predictor of arrhythmogenic risk. It seems to account for small changes in repolarization in the complete T wave, which other indices fail to do.
Female sex is considered a classic risk factor for TdP [3, 37]. This sex disparity is reflected in our cohort, in which a large majority of the patients who experienced TdP were females (10/13, 77%). The reasons for this increased risk is unknown but may be due to hormonal factors [38]. Pathophysiology aside, clinicians should be aware of this increased predisposition in women. Hypokalemia and hypomagnesaemia are further risk factors for TdP, but all patients in our study had normal electrolyte values (documented normal potassium and magnesium are required per our protocol for AAD drug loading). Interestingly, all patients who experienced TdP were in sinus rhythm on the preceding ECG. It has been reported that there is increased sensitivity to the QT prolonging effects of class III agents after restoration of sinus rhythm [39].
Limitations
This study was performed retrospectively on a relatively small number of TdP patients and requires validation in a larger cohort. While we matched on sex and age (within 2 years), there is a potential for confounding by other clinical factors that differ between groups. For example, we did not match on ejection fraction or serum electrolyte levels, which also are independent risk factors for TdP. However there was no calculated statistically significant difference between cases and controls for these variables. Given that the mean time between TdP and the ECG recording of approximately 120 mins, a direct correlation is difficult to completely assess in this context. Extrapolation to a population with paced rhythms is unknown as we excluded them from out cohort. Lastly, this new software program has not been validated in other populations outside of our study.
Conclusion
The combination of a lead V3-derived QTc and a lead I derived T wave right slope discriminated the torsadogenic cases from the non-torsadogenic controls exposed to virtually identical sotalol/dofetilide loads with near 90% accuracy. Consideration of T wave parameters in addition to the QTc has significant potential to enhance risk stratification in patients.
Supplementary Material
Table 2.
Correlation ECG variables to Torsades
| ECG lead | Correlation Coefficient | P value |
|---|---|---|
| Lead V3 QTc | 0.72 | < 0.0001 |
| Lead I Right Slope | 0.45 | 0.0002 |
Clinical Perspective.
Class III antiarrhythmics (sotalol and dofetilide) are common medications used in the management of atrial fibrillation. Initiation of these medications requires serial QTc measurements to help reduce the risk of lethal ventricular arrhythmias. However QTc is an imperfect marker of this risk. Sophisticated T wave analysis could have the potential to predict proarrhythmia, thereby guiding safer patient selection for specific drugs, or prediction of proarrhythmic events to enable drug dose modification or discontinuation. In this study, we aimed to identify T wave morphological changes with the use of a novel T wave analysis program in those patients loaded with class III antiarrhythmics. The main observation is that in addition to QTc, the T wave right slope is correlated strongly with TdP risk. Our findings suggest that measurement of T wave parameters (in particular T wave right slope) in addition to the QTc has significant potential to enhance torsade risk stratification.
Acknowledgments
None
Funding Sources:
C.V.D. is supported by an NIH T32 Training Grant HL 007111
V.K. is supported by funding from Czech Science Foundation GACR #P103/11/P106.
Dr Ackerman is a consultant for: Boston Scientific, Medtronic, St. Jude Medical, Transgenomic. Royalties and Intellectual Property from Transgenomic. Dr Asirvatham is a consultant for Abiomed, Atricure, Biotronik, Biosense Webster, Boston Scientific, Medtronic, Spectranetics, St Jude Medical, Sanofi-Aventis, Wolters Kluwer, and Elsevier.
Footnotes
Disclosures
The other authors report no disclosures.
References
- 1.Zimetbaum P. Antiarrhythmic drug therapy for atrial fibrillation. Circulation. 2012;125(2):381–389. doi: 10.1161/CIRCULATIONAHA.111.019927. [DOI] [PubMed] [Google Scholar]
- 2.Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Journal of the American College of Cardiology. 2010;55(9):934–947. doi: 10.1016/j.jacc.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehmann MH, Hardy S, Archibald D, quart B, MacNeil DJ. Sex difference in risk of torsade de pointes with d,l-sotalol. Circulation. 1996;94(10):2535–2541. doi: 10.1161/01.cir.94.10.2535. [DOI] [PubMed] [Google Scholar]
- 4.Soyka LF, Wirtz C, Spangenberg RB. Clinical safety profile of sotalol in patients with arrhythmias. The American journal of cardiology. 1990;65(2):74A–81A. doi: 10.1016/0002-9149(90)90207-h. discussion 2A–3A. [DOI] [PubMed] [Google Scholar]
- 5.Pacifico A, Hohnloser SH, Williams JH, Tao B, Saksena S, Henry PD, et al. Prevention of implantable-defibrillator shocks by treatment with sotalol. d,l-Sotalol Implantable Cardioverter-Defibrillator Study Group. The New England journal of medicine. 1999;340(24):1855–1862. doi: 10.1056/NEJM199906173402402. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen HS, Elming H, Seibaek M, Burchardt H, Brendorp B, Torp-Pedersen C, et al. Risk factors and predictors of Torsade de pointes ventricular tachycardia in patients with left ventricular systolic dysfunction receiving Dofetilide. The American journal of cardiology. 2007;100(5):876–880. doi: 10.1016/j.amjcard.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Norgaard BL, Wachtell K, Christensen PD, Madsen B, Johansen JB, Christiansen EH, et al. Efficacy and safety of intravenously administered dofetilide in acute termination of atrial fibrillation and flutter: a multicenter, randomized, double-blind, placebo-controlled trial. Danish Dofetilide in Atrial Fibrillation and Flutter Study Group. American heart journal. 1999;137(6):1062–1069. doi: 10.1016/s0002-8703(99)70363-7. [DOI] [PubMed] [Google Scholar]
- 8.Malik M. Problems of heart rate correction in assessment of drug-induced QT interval prolongation. Journal of cardiovascular electrophysiology. 2001;12(4):411–420. doi: 10.1046/j.1540-8167.2001.00411.x. [DOI] [PubMed] [Google Scholar]
- 9.Roden DM. Drug-induced prolongation of the QT interval. The New England journal of medicine. 2004;350(10):1013–1022. doi: 10.1056/NEJMra032426. [DOI] [PubMed] [Google Scholar]
- 10.Brennan T, Fink M, Stokeley D, Rodriguez B, Tarassenko L, editors. Computers in Cardiology. Vol. 2007. IEEE; 2007. Modelling effects of sotalol on T-wave morphology. [Google Scholar]
- 11.Houltz B, Darpo B, Edvardsson N, Blomstrom P, Brachmann J, Crijns HJ, et al. Electrocardiographic and clinical predictors of torsades de pointes induced by almokalant infusion in patients with chronic atrial fibrillation or flutter: a prospective study. Pacing and clinical electrophysiology : PACE. 1998;21(5):1044–1057. doi: 10.1111/j.1540-8159.1998.tb00150.x. [DOI] [PubMed] [Google Scholar]
- 12.Jacobson I, Carlsson L, Duker G. Beat-by-beat QT interval variability, but not QT prolongation per se, predicts drug-induced torsades de pointes in the anaesthetised methoxamine-sensitized rabbit. Journal of pharmacological and toxicological methods. 2011;63(1):40–46. doi: 10.1016/j.vascn.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Thomsen MB, Verduyn SC, Stengl M, Beekman JD, de Pater G, van Opstal J, et al. Increased short-term variability of repolarization predicts d-sotalol-induced torsades de pointes in dogs. Circulation. 2004;110(16):2453–2459. doi: 10.1161/01.CIR.0000145162.64183.C8. [DOI] [PubMed] [Google Scholar]
- 14.Shah RR, Hondeghem LM. Refining detection of drug-induced proarrhythmia: QT interval and TRIaD. Heart rhythm : the official journal of the Heart Rhythm Society. 2005;2(7):758–772. doi: 10.1016/j.hrthm.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 15.Antzelevitch C, Shimizu W. Cellular mechanisms underlying the long QT syndrome. Current opinion in cardiology. 2002;17(1):43–51. doi: 10.1097/00001573-200201000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Clifford GD, Azuaje F, McSharry PE. Advanced Methods and Tools for ECG Data Analysis: Artech House. 2006 [Google Scholar]
- 17.Lin C, Mailhes C, Tourneret J-Y. P- and T-wave delineation in ECG signals using a Bayesian approach and a partially collapsed Gibbs sampler. IEEE transactions on bio-medical engineering. 2010;57(12):2840–2849. doi: 10.1109/TBME.2010.2076809. [DOI] [PubMed] [Google Scholar]
- 18.Hondeghem LM. Thorough QT/QTc not so thorough: removes torsadogenic predictors from the T-wave, incriminates safe drugs, and misses profibrillatory drugs. Journal of cardiovascular electrophysiology. 2006;17(3):337–340. doi: 10.1111/j.1540-8167.2006.00347.x. [DOI] [PubMed] [Google Scholar]
- 19.Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart. 2003;89(11):1363–1372. doi: 10.1136/heart.89.11.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomsen MB, Volders PG, Beekman JD, Matz J, Vos MA. Beat-to-Beat variability of repolarization determines proarrhythmic outcome in dogs susceptible to drug-induced torsades de pointes. Journal of the American College of Cardiology. 2006;48(6):1268–1276. doi: 10.1016/j.jacc.2006.05.048. [DOI] [PubMed] [Google Scholar]
- 21.Roden DM, Woosley RL, Primm RK. Incidence and clinical features of the quinidine-associated long QT syndrome: implications for patient care. American heart journal. 1986;111(6):1088–1093. doi: 10.1016/0002-8703(86)90010-4. [DOI] [PubMed] [Google Scholar]
- 22.Woosley RL, Chen Y, Freiman JP, Gillis RA. Mechanism of the cardiotoxic actions of terfenadine. Jama. 1993;269(12):1532–1536. [PubMed] [Google Scholar]
- 23.De Bruin ML, Langendijk PN, Koopmans RP, Wilde AA, Leufkens HG, Hoes AW. In-hospital cardiac arrest is associated with use of non-antiarrhythmic QTc-prolonging drugs. British journal of clinical pharmacology. 2007;63(2):216–223. doi: 10.1111/j.1365-2125.2006.02722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Couderc JP, Vaglio M, Xia X, McNitt S, Wicker P, Sarapa N, et al. Impaired T-amplitude adaptation to heart rate characterizes I(Kr) inhibition in the congenital and acquired forms of the long QT syndrome. Journal of cardiovascular electrophysiology. 2007;18(12):1299–1305. doi: 10.1111/j.1540-8167.2007.00960.x. [DOI] [PubMed] [Google Scholar]
- 25.Graff C, Andersen MP, Xue JQ, Hardahl TB, Kanters JK, Toft E, et al. Identifying drug-induced repolarization abnormalities from distinct ECG patterns in congenital long QT syndrome: a study of sotalol effects on T-wave morphology. Drug safety. 2009;32(7):599–611. doi: 10.2165/00002018-200932070-00006. [DOI] [PubMed] [Google Scholar]
- 26.Couderc JP, Xia X, Peterson DR, McNitt S, Zhao H, Polonsky S, et al. T-wave morphology abnormalities in benign, potent, and arrhythmogenic I(kr) inhibition. Heart rhythm : the official journal of the Heart Rhythm Society. 2011;8(7):1036–1043. doi: 10.1016/j.hrthm.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moss AJ, Zareba W, Benhorin J, Locati EH, Hall WJ, Robinson JL, et al. ECG T-wave patterns in genetically distinct forms of the hereditary long QT syndrome. Circulation. 1995;92(10):2929–2934. doi: 10.1161/01.cir.92.10.2929. [DOI] [PubMed] [Google Scholar]
- 28.Yan GX, Antzelevitch C. Cellular basis for the normal T wave and the electrocardiographic manifestations of the long-QT syndrome. Circulation. 1998;98(18):1928–1936. doi: 10.1161/01.cir.98.18.1928. [DOI] [PubMed] [Google Scholar]
- 29.Bhuiyan TA, Graff C, Kanters JK, Thomsen MB, Struijk JJ, editors. Computing in Cardiology Conference (CinC) Vol. 2013. IEEE; 2013. Flattening of the electrocardiographic T-wave is a sign of proarrhythmic risk and a reflection of action potential triangulation. [Google Scholar]
- 30.Nielsen J, Graff C, Hardahl T, Andersen MP, Kristoffersen J, Struijk JJ, et al. Sertindole causes distinct electrocardiographic T-wave morphology changes. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2009;19(10):702–707. doi: 10.1016/j.euroneuro.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 31.Letsas KP, Weber R, Astheimer K, Kalusche D, Arentz T. Tpeak-Tend interval and Tpeak-Tend/QT ratio as markers of ventricular tachycardia inducibility in subjects with Brugada ECG phenotype. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2010;12(2):271–274. doi: 10.1093/europace/eup357. [DOI] [PubMed] [Google Scholar]
- 32.Gupta P, Patel C, Patel H, Narayanaswamy S, Malhotra B, Green JT, et al. T(p-e)/QT ratio as an index of arrhythmogenesis. Journal of electrocardiology. 2008;41(6):567–574. doi: 10.1016/j.jelectrocard.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 33.Topilski I, Rogowski O, Rosso R, Justo D, Copperman Y, Glikson M, et al. The morphology of the QT interval predicts torsade de pointes during acquired bradyarrhythmias. Journal of the American College of Cardiology. 2007;49(3):320–328. doi: 10.1016/j.jacc.2006.08.058. [DOI] [PubMed] [Google Scholar]
- 34.Shimizu M, Ino H, Okeie K, Yamaguchi M, Nagata M, Hayashi K, et al. T-peak to T-end interval may be a better predictor of high-risk patients with hypertrophic cardiomyopathy associated with a cardiac troponin I mutation than QT dispersion. Clinical cardiology. 2002;25(7):335–339. doi: 10.1002/clc.4950250706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haarmark C, Hansen PR, Vedel-Larsen E, Pedersen SH, Graff C, Andersen MP, et al. The prognostic value of the Tpeak-Tend interval in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Journal of electrocardiology. 2009;42(6):555–560. doi: 10.1016/j.jelectrocard.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 36.Dillon JJ, DeSimone CV, Sapir Y, Somers VK, Dugan JL, Bruce CJ, et al. Noninvasive potassium determination using a mathematically processed ECG: proof of concept for a novel "blood-less, blood test". Journal of electrocardiology. 2015;48(1):12–18. doi: 10.1016/j.jelectrocard.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Somberg JC, Preston RA, Ranade V, Cvetanovic I, Molnar J. Gender differences in cardiac repolarization following intravenous sotalol administration. Journal of cardiovascular pharmacology and therapeutics. 2012;17(1):86–92. doi: 10.1177/1074248411406505. [DOI] [PubMed] [Google Scholar]
- 38.Lehmann MH, Timothy KW, Frankovich D, Fromm BS, Keating M, Locati EH, et al. Age-Gender Influence on the Rate-Corrected QT Interval and the QT-Heart Rate Relation in Families With Genotypically Characterized Long QT Syndrome. Journal of the American College of Cardiology. 1997;29(1):93–99. doi: 10.1016/s0735-1097(96)00454-8. [DOI] [PubMed] [Google Scholar]
- 39.Choy AM, Darbar D, Dell'Orto S, Roden DM. Exaggerated QT prolongation after cardioversion of atrial fibrillation. Journal of the American College of Cardiology. 1999;34(2):396–401. doi: 10.1016/s0735-1097(99)00226-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.