Diarrheal disease is the world’s second leading cause of death among young children. It claims more than half a million lives of children under five years old each year, accounting for 9% of global child deaths [1,2]. It is also a leading cause of morbidity in children, including chronic malnutrition [3].
The original United Nations Millennium Development Goals included a target to reduce the mortality rate among children under five by two-thirds by 2015. Although tremendous progress has been made in reducing the rate by 47% to date [4], more work is urgently needed. Pursuing this target as part of the new Sustainable Development Goals [5] will require new approaches. These should include the wider use of oral rehydration solution (ORS) and expanded use of safe, effective, and affordable drugs such as antisecretory compounds [6] and antimicrobials targeting prominent causes of diarrheal disease in young children [7]. Further investment in research and development (R&D) focused on new drugs that are effective against some of the most important pathogens is also required.
The Global Enteric Multicenter Study (GEMS) was a multiyear study that analyzed moderate-to-severe diarrheal disease in children at seven sites across Africa and Asia using a case-control design [8]. Complementing the approach taken by GEMS, investigators from A Global Network for the Study of Malnutrition and Enteric Diseases (MAL-ED) conducted an equally ambitious birth cohort study over five years at eight community sites in Africa, Asia, and South America and assessed pathogen-specific burdens in diarrheal and nondiarrheal stool specimens [9].
Despite important differences in study design, both GEMS and MAL-ED call attention to the frequent and important role played by Cryptosporidium spp. (especially C. hominis and C. parvum) in causing morbidity and mortality among young children. In GEMS, Cryptosporidium spp. were identified as the second leading pathogen associated with moderate-to-severe diarrhea (MSD) in children under two years old and the leading pathogen associated with death in toddlers (ages 12 to 23 months) [8]. In the MAL-ED cohort, Cryptosporidium spp. were among the pathogens with the highest attributable burden of diarrhea among children one year old or younger and were also associated with persistent diarrhea [9]. The frequent or chronic insults to the gastrointestinal system by enteric pathogens including Cryptosporidium, alone or by coinfection, are thought to result in a condition known as environmental enteropathy, which manifests itself in malnutrition, stunting, perturbation of the gut microbiome, impaired cognitive development, diminished oral vaccine efficacy, and increased susceptibility to infections [10–13].
Although the diarrhea associated with Cryptosporidium infection can be life-threatening, it is only part of the problem. In a longitudinal study of slum dwellers in southern India, Ajjampur et al. [14] found that half of children were shedding oocysts well before or after episodes of cryptosporidial diarrhea, indicating the presence of asymptomatic infections. These asymptomatic infections are likely to contribute significantly to the long-term impact of cryptosporidiosis on malnutrition and stunted growth. This finding also has important implications for the control of Cryptosporidium and begs the question as to whether the problem should be addressed with a mass drug administration (MDA) strategy.
In considering the total effects of diarrheal disease in children—including cryptosporidiosis—we must also consider the tremendous financial burden borne by families with children experiencing multiple bouts of diarrheal disease each year. A study by Rheingans et al. [15] looked at African sites participating in GEMS and found that the total cost of treatment per episode of diarrhea ranged from US$6.01 in Mali to US$8.83 in Kenya, which is a huge amount in countries where more than one-third of the population lives below the international poverty line (of less than US$1.25 per day) and where total annual per capita health expenditure is US$53 and US$45, respectively [16–19].
Although Cryptosporidium was originally identified in 1907 [20], it was not until the late 1970s that its role as a serious, and sometimes lethal, human pathogen was elucidated by the careful work of Nime [21], Bird and Smith [22], Tzipori [23,24], and others [25,26]. In particular, the morbidity and potential mortality associated with cryptosporidiosis came into focus through the lens of the evolving HIV/AIDS epidemic in the 1980s [27]. Likewise, Cryptosporidium was demonstrated to be a common cause of diarrheal disease in children in Central Africa in the 1980s [28].
Despite the role of Cryptosporidium as an important human pathogen, there are currently few effective options for treatment. As reviewed by Checkley et al. [29], a variety of diagnostic methods exist, but they are best suited for epidemiological studies and are not routinely used in limited-resource settings. In addition, no vaccine is currently available to protect against Cryptosporidium infection and, based on the limited understanding of the Cryptosporidium-specific biology and challenges encountered in developing vaccines for other parasites, it is highly unlikely that a vaccine will be available within the next decade [29–31]. Moreover, although prevention for some enteric pathogens may be bolstered through programs focused on clean water and effective sanitation, such approaches will only go so far in preventing many cases of cryptosporidiosis, and person-to-person transmission further complicates the overall approach [32,33].
ORS-based treatment is a highly efficacious and cost-effective way to counteract the effects and relieve some of the symptoms associated with acute secretory diarrheas such as that caused by Cryptosporidium. However, use of ORS (particularly among children living in especially poor and rural areas) remains quite low, in part because treatment is labor-intensive and requires large volumes of ORS to be administered in order to rehydrate and then maintain hydration [34]. Furthermore, ORS has no role in the treatment of asymptomatic but insidious Cryptosporidium infections, which can only be addressed through drug treatment. Thus, to reduce the duration and impact of the Cryptosporidium infection, an antimicrobial drug is an important complement to ORS.
Only one drug, nitazoxanide (Alinia; Romark Laboratories, Tampa, Florida, United States), is currently approved by the US Food and Drug Administration (FDA) for treatment of Cryptosporidium infection. It is approved for use in children one year old or older [35]. The drug is available in many middle-income countries in Latin America, as well as in some low- and middle-income countries in Asia, including India and Bangladesh. Nonetheless, its actual use is limited, and empiric treatment with ORS alone remains the standard of care for diarrhea caused by Cryptosporidium.
Clinical studies have demonstrated the effectiveness of nitazoxanide against Cryptosporidium in otherwise healthy individuals. In addition, clinical studies have provided evidence suggesting the drug’s activity against rotavirus, helminths, and other enteric protozoan parasites [36–38]. Thus, there are sufficient reasons for considering wider use of this drug, even as a candidate for use in MDA programs as proposed by Hotez [39] and others.
The drug’s efficacy profile is variable, with cure rates reported to range from more than 80% in otherwise healthy adults to only 56% in malnourished children [40]. One significant shortcoming of nitazoxanide is that it does not appear to be beneficial in individuals who are immunocompromised [41] and is less effective in children who are malnourished—a key limitation given the prevalence of immunosuppression in children who are HIV-positive and/or malnourished.
We support an expanded global role for nitazoxanide in addressing cryptosporidiosis in children under five years of age if the global community is to meet established goals for reducing childhood mortality. We intend to investigate the possibility of lowering the approved age for treatment by testing the drug’s safety and effectiveness in children between six and 12 months of age, to explore rational combinations with other drugs (see Table 1), and to have the drug included on the World Health Organization’s Model List of Essential Medicines.
Table 1. Drugs and drug candidates for treating Cryptosporidium infection in young children.
| Compound | Development stage | Activity against Cryptosporidium | References |
|---|---|---|---|
| Nitazoxanide | FDA approved for Cryptosporidium, launched | Clinical | [40,44–46] |
| Nitazoxanide + Azithromycin | Proposed combination therapy | Anecdotal clinical evidence | [47–48] |
| Pyrvinium pamoate | Repurposing candidate (FDA approved for pinworm infections) | Animal model | [49] |
| Pitavastatin | Repurposing candidate (FDA approved for hypercholesterolemia) | In vitro only (yet to be tested in an animal model) | [50] |
| Auranofin | Repurposing candidate (FDA approved for rheumatoid arthritis) | In vitro only (yet to be tested in an animal model) | [51] |
| Calcium-dependent protein kinase 1 inhibitors | Preclinical | Animal model | [52] |
| Inosine 5’- monophosphate dehydrogenase (IMPDH) inhibitors | Preclinical | Animal model | [53] |
| Fatty acyl-CoA synthetase inhibitor Triacsin C | Preclinical | Animal model | [54] |
| Oleylphosphocholine | Preclinical | Animal model | [55] |
| Medicines for Malaria Venture (MMV) Malaria Box compounds | Preclinical | In vitro only (yet to be tested in an animal model) | [56] |
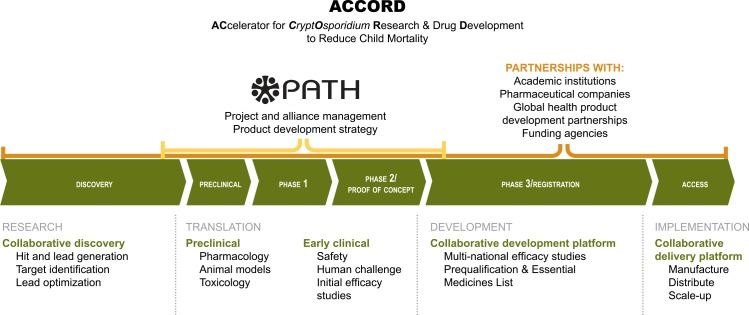
While the wider use of nitazoxanide would help relieve the burden of Cryptosporidium infection, we also see an urgent need for new drugs that provide an alternative to nitazoxanide and address its shortcomings. Several groups have identified existing drugs in clinical use for other indications that have the potential to be repurposed for the treatment of Cryptosporidium infection (Table 1). In addition, there are a number of preclinical leads in the pipeline, but more are needed. Now is the time to develop a bold, integrated program to accelerate funding, research, and development of needed Cryptosporidium drugs. Taking as a guiding model the Tuberculosis Drug Accelerator established by the Bill & Melinda Gates Foundation, we propose an approach that we call ACCORD (ACcelerator for CryptOsporidium Research & Drug Development to Reduce Child Mortality) to help accelerate the development of new therapeutics for Cryptosporidium (Fig 1).
Fig 1. Proposed ACCORD (ACcelerator for CryptOsporidium Research & Drug Development to Reduce Child Mortality) structure and function.
The ACCORD approach is an integrated partnership among pharmaceutical companies, research institutions, product development partnerships, and funders to accelerate research and development of needed Cryptosporidium drugs to reduce child mortality.
ACCORD will be successful only with investments and commitments from pharmaceutical companies, private foundations, governments, academic institutions, and nongovernmental organizations. In 2014, the authors of the G-FINDER report meticulously studied and analyzed global diarrheal disease R&D funding [42]. The authors found that, in 2013, investment specific to Cryptosporidium was limited to US$2.7 million in basic research and US$1.7 million in R&D focused on drugs. This is a paltry sum when compared to the amount spent on R&D for tuberculosis drugs (US$248 million) or a rotavirus vaccine (more than US$200 million) [43]. We believe that at least US$10 million of new funding per year is required for the next decade in order to develop the next generation of drugs. With this increased investment in drug development for diarrheal disease, and through collaborative partnerships across sectors, we will be able to align and accelerate the efforts needed to achieve further progress in meeting global targets for reductions in child mortality.
Funding Statement
The authors (DAS, ELdH, and RKMC) have received funding from the Department for International Development of the United Kingdom (Grant No. 204139 [2013], www.gov.uk/government/organisations/department-for-international-development). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UNICEF. Committing to Child Survival: A Promise Renewed—Progress Report 2013. New York: UNICEF; 2013. http://www.unicef.org/publications/index_70354.html. [Google Scholar]
- 2.Bhutta ZA, Black RE. Global Maternal, Newborn, and Child Health—So Near and Yet So Far. N Engl J Med. 2013;369: 2226–35. doi: http://www.nejm.org/doi/full/10.1056/NEJMra1111853 [DOI] [PubMed] [Google Scholar]
- 3.Keusch GT, Fontaine O, Bhargave A, Boschi-Pinto C, Bhutta ZA, Gotuzzo E, et al. Diarrheal diseases In: Jamison DT, Breman JG, Measham AR, et al., eds. Disease Control Priorities in Developing Countries. 2nd ed. Washington, DC: World Bank; 2006: 371–87. [Google Scholar]
- 4.United Nations. The Millennium Development Goals Report. New York: United Nations; 2015. http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf. [Google Scholar]
- 5.United Nations. Open Working Group Proposal for Sustainable Development Goals. New York: United Nations; 2013. http://undocs.org/A/68/970. [Google Scholar]
- 6.De Hostos EL, Choy RK, Nguyen T. Developing novel antisecretory drugs to treat infectious diarrhea. Future Med Chem. 2011;3(10): 1317–25. 10.4155/fmc.11.87 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization, UNICEF. End Preventable Deaths: Global Action Plan for Prevention and Control of Pneumonia and Diarrhoea. Geneva: World Health Organization; 2013. http://www.unicef.org/media/files/Final_GAPPD_main_Report-_EN-8_April_2013.pdf. [Google Scholar]
- 8.Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382(9888): 209–22. 10.1016/S0140-6736(13)60844-2 [DOI] [PubMed] [Google Scholar]
- 9.Platts-Mills JA, Babji S, Bodhidatta L, Gratz J, Haque R, Havt A, et al. Pathogen-specific burdens of community diarrhoea in developing countries: a multisite birth cohort study (MAL-ED). Lancet Glob Health. 2015;3(9): e564–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agnew DG, Lima AA, Newman RD, Wuhib T, Moore RD, Guerrant RL, et al. Cryptosporidiosis in northeastern Brazilian children: association with increased diarrhea morbidity. J Infect Dis. 1998;177(3): 754–60. [DOI] [PubMed] [Google Scholar]
- 11.Guerrant DI, Moore SR, Lima AA, Patrick PD, Schorling JB, Guerrant RL. Association of early childhood diarrhea and cryptosporidiosis with impaired physical fitness and cognitive function four–seven years later in a poor urban community in northeast Brazil. Am J Trop Med Hyg. 1999;61: 707–13. [DOI] [PubMed] [Google Scholar]
- 12.Alcantara CS, Yang CH, Steiner TS, Barrett LJ, Lima AA, Chappell CL, et al. Interleukin-8, tumor necrosis factor-α, and lactoferrin in immunocompetent hosts with experimental and Brazilian children with acquired cryptosporidiosis. Am J Trop Med Hyg. 2003;68(3): 325–28. [PubMed] [Google Scholar]
- 13.Lang D, MAL-ED Network Investigators. Opportunities to assess factors contributing to the development of the intestinal microbiota in infants living in developing countries. Microb Ecol Health Dis. 2015;26: 28316 10.3402/mehd.v26.28316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajjampur SS, Sarkar R, Sankaran P, Kannan A, Menon VK, Muliyil J, et al. Symptomatic and asymptomatic Cryptosporidium infections in children in a semi-urban slum community in southern India. Am J Trop Med Hyg. 2010;83(5): 1110–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rheingans R, Kukla M, Adegbola RA, Debasish S, Omore R, Breiman RF, et al. Exploring household economic impacts of childhood diarrheal illnesses in 3 African settings. Clin Infect Dis. 2012;55(Suppl 4): S317–26. 10.1093/cid/cis763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UNICEF. At a glance: Gambia. New York: UNICEF; updated 2013 December 26. http://www.unicef.org/infobycountry/gambia_statistics.html. [Google Scholar]
- 17.UNICEF. Kenya. New York: UNICEF; updated 2013 December 27. http://www.unicef.org/infobycountry/kenya_statistics.html. [Google Scholar]
- 18.UNICEF. Mali. New York: UNICEF; updated 2013 December 27. http://www.unicef.org/infobycountry/mali_statistics.html. [Google Scholar]
- 19.The World Bank Group. Health expenditure per capita (current US$) Washington: The World Bank Group; updated 2014. http://data.worldbank.org/indicator/SH.XPD.PCAP. [Google Scholar]
- 20.Tyzzer EE. A sporozoon found in the peptic glands of the common mouse. Pro Soc Exp Biol Med. 1907;5: 12–13. [Google Scholar]
- 21.Nime FA, Burek JD, Page DL, Holscher MA, Yardley JH. Acute enterocolitis in a human being infected with the protozoan Cryptosporidium. Gastroenterology. 1976;70(4): 592–98. [PubMed] [Google Scholar]
- 22.Bird RG, Smith MD. Cryptosporidiosis in man: parasite life cycle and fine structural pathology. J Pathol. 1980;132(3): 217–33. [DOI] [PubMed] [Google Scholar]
- 23.Tzipori S, Smith M, Birch C, Barnes G, Bishop R. Cryptosporidiosis in hospital patients with gastroenteritis. Am J Trop Med Hyg. 1983;32(5): 931–34. [DOI] [PubMed] [Google Scholar]
- 24.Tzipori S. Cryptosporidium: notes on epidemiology and pathogenesis. Parasitol Today. 1985;1(6): 159–65. [DOI] [PubMed] [Google Scholar]
- 25.Current WL, Reese NC, Ernst JV, Bailey WS, Heyman MB, Weinstein WM. Human cryptosporidiosis in immunocompetent and immunodeficient persons. Studies of an outbreak and experimental transmission. N Engl J Med. 1983;308(21): 1252–7. [DOI] [PubMed] [Google Scholar]
- 26.Holley HP Jr, Dover C. Cryptosporidium: a common cause of parasitic diarrhea in otherwise healthy individuals. J Infect Dis. 1986;153(2): 365–8. [DOI] [PubMed] [Google Scholar]
- 27.Casemore DP, Sands RL, Curry A. Cryptosporidium species a “new” human pathogen. J Clin Pathol. 1985;38(12): 1321–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bogaerts J, Lepage P, Rouvroy D, Vandepitte J. Cryptosporidium spp., a frequent cause of diarrhea in Central Africa. J Clin Microbiol. 1984;20(5): 874–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Checkley W, White AC Jr, Jagnath D, Arrowood MJ, Chalmers RM, Chen XM, et al. A review of the global burden, novel diagnostics, therapeutics, and vaccine targets for cryptosporidium. Lancet Infect Dis. 2015;15(1): 85–94. 10.1016/S1473-3099(14)70772-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ryan U, Hijjawi N. New developments in Cryptosporidium research. Int J Parasitol. 2015;45(6): 367–73. 10.1016/j.ijpara.2015.01.009 [DOI] [PubMed] [Google Scholar]
- 31.Mead JR. Prospects for immunotherapy and vaccines against Cryptosporidium. Hum Vaccin Immunother. 2014;10(6): 1505–13. 10.4161/hv.28485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Egger M, Mäusezahl D, Odermatt P. Symptoms and transmission of intestinal cryptosporidiosis. Arch Dis Child. 1990;65(4): 445–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarkar R, Ajjampur SS, Prabakaran AD, Geetha JC, Sowmyanarayanan TV, Kane A, et al. Cryptosporidiosis among children in an endemic semiurban community in southern India: does a protected drinking water source decrease infection? Clin Infect Dis. 2013;57: 398–406. 10.1093/cid/cit288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zwisler G, Simpson E, Moodley M. Treatment of diarrhea in young children: results from surveys on the perception and use of oral rehydration solutions, antibiotics, and other therapies in India and Kenya. J Glob Health. 2013;3(1): 010403 10.7189/jogh.03.010403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Parasites—Cryptosporidium. Treatment—Nitazoxanide. Atlanta: Centers for Disease Control and Prevention; updated 2010 November 2. http://www.cdc.gov/parasites/crypto/health_professionals/tx.html. [Google Scholar]
- 36.Rossignol JF, El-Gohary YM. Nitazoxanide in the treatment of viral gastroenteritis: a randomized double-blind placebo-controlled clinical trial. Aliment Pharmacol Ther. 2006;24(10): 1423–30. [DOI] [PubMed] [Google Scholar]
- 37.Rossignol JF, Abu-Zekry M, Hussein A, Santoro G. Effect of nitazoxanide for treatment of severe rotavirus diarrhoea: randomised double-blind placebo-controlled trial. Lancet. 2006;368(9350): 124–9. [DOI] [PubMed] [Google Scholar]
- 38.Rossignol JF, Lopez-Chegne N, Julcamoro LM, Carrion ME, Bardin MC. Nitazoxanide for the empiric treatment of pediatric infectious diarrhea. Trans R Soc Trop Med Hyg. 2012;106(3): 167–73. 10.1016/j.trstmh.2011.11.007 [DOI] [PubMed] [Google Scholar]
- 39.Hotez PJ. Could nitazoxanide be added to other essential medicines for integrated neglected tropical disease control and elimination? PLoS Negl Trop Dis. 2014;8(3): e2758 10.1371/journal.pntd.0002758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amadi B, Mwiya M, Musuku J, Watuka A, Sianongo S, Ayoub A, et al. Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: a randomised controlled trial. Lancet. 2002;360(9343): 1375–80. [DOI] [PubMed] [Google Scholar]
- 41.Abubakar I, Aliyu SH, Arumugam C, Usman NK, Hunter PR. Treatment of cryptosporidiosis in immunocompromised individuals: systematic review and meta-analysis. Br J Clin Pharmacol. 2007;63(4): 387–93. 10.1111/j.1365-2125.2007.02873.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Policy Cures. G-FINDER 2014 Neglected Disease Research and Development: Emerging Trends. Sydney: Policy Cures; 2014. http://www.policycures.org/downloads/Y7%20GFINDER%20full%20report%20web%20.pdf. [Google Scholar]
- 43.Light DW, Andrus JK, Warburton RN. Estimated research and development costs of rotavirus vaccines. Vaccine. 2009;27(47): 6627–33. 10.1016/j.vaccine.2009.07.077 [DOI] [PubMed] [Google Scholar]
- 44.Rossignol JF, Ayoub A, Ayers MS. Treatment of diarrhea caused by Cryptosporidium parvum: a prospective randomized, double-blind, placebo-controlled study of nitazoxanide. J Infect Dis. 2001;184(1): 103–6. [DOI] [PubMed] [Google Scholar]
- 45.Rossignol JF, Kabil SM, El-Gohary Y, Younis AM. Effect of nitazoxanide in diarrhea and enteritis caused by Cryptosporidium species. Clin Gastroenterol Hepatol. 2006;4(3): 320–24. [DOI] [PubMed] [Google Scholar]
- 46.Amadi B, Mwiya M, Sianongo S, Payne L, Watuka A, Katubulushi M, et al. High dose prolonged treatment with nitazoxanide is not effective for cryptosporidiosis in HIV positive Zambian children: a randomised controlled trial. BMC Infect Dis. 2009;9: 195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Legrand F, Grenouillet F, Larosa F, Dalle F, Saas P, Millon L, et al. Diagnosis and treatment of digestive cryptosporidiosis in allogeneic haematopoietic stem cell transplant recipients: a prospective single centre study. Bone Marrow Transplant. 2011;46(6): 858–62. 10.1038/bmt.2010.200 [DOI] [PubMed] [Google Scholar]
- 48.Hong DK, Wong CJ, Gutierrez K. Severe cryptosporidiosis in a seven-year-old renal transplant recipient: case report and review of the literature. Pediatr Transplant. 2007;11(1): 94–100. [DOI] [PubMed] [Google Scholar]
- 49.Downey AS, Chong CR, Graczyk TK, Sullivan DJ. Efficacy of pyrvinium pamoate against Cryptosporidium parvum infection in vitro and in a neonatal mouse model. Antimicrob Agents Chemother. 2008;52(9): 3106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bessoff K, Sateriale A, Lee KK, et al. Drug repurposing screen reveals FDA-approved inhibitors of human HMG-CoA reductase and isoprenoid synthesis that block Cryptosporidium parvum growth. Antimicrob Agents Chemother. 2013;57(4): 1808–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Debnath A, Ndao M, Reed SL. Reprofiled drug targets ancient protozoans: drug discovery for parasitic diarrheal diseases. Gut Microbes. 2013;4(1): 66–71. 10.4161/gmic.22596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Castellanos-Gonzalez A, White AC Jr, Ojo KK, Vidadala RS, Zhang Z, Reid MC, et al. A novel calcium-dependent protein kinase inhibitor as a lead compound for treating cryptosporidiosis. J Infect Dis. 2013;208(8): 1342–8. 10.1093/infdis/jit327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gorla SK, McNair NN, Yang G, Gao S, Hu M, Jala VR, et al. Validation of IMP dehydrogenase inhibitors in a mouse model of cryptosporidiosis. Antimicrob Agents Chemother. 2014;58(3): 1603–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guo F, Zhang H, Fritzler JM, et al. Amelioration of Cryptosporidium parvum infection in vitro and in vivo by targeting parasite fatty acyl-coenzyme A synthetasis. J Infect Dis. 2014:209(8): 1279–87. 10.1093/infdis/jit645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sonzogni-Desautels K, Renteria A, Camargo F, et al. Oleylphosphocholine (OIPC) arrests Cryptosporidium parvum growth in vitro and prevents lethal infection in interferon gamma receptor knock-out mice. Front Microbiol. 2015;6: 973 10.3389/fmicb.2015.00973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bessoff K, Spangenberg T, Foderaro JE, Jumani RS, Ward GE, Huston CD. Identification of Cryptosporidium parvum active chemical series by Repurposing the open access malaria box. Antimicrob Agents Chemother. 2014;58(5): 2731–9. [DOI] [PMC free article] [PubMed] [Google Scholar]