Abstract
AKI is associated with high mortality rates and the development of CKD. Ischemia/reperfusion (IR) is an important cause of AKI. Unfortunately, there is no available pharmacologic approach to prevent or limit renal IR injury in common clinical practice. Renal IR is characterized by diminished nitric oxide bioavailability and reduced renal blood flow; however, the mechanisms leading to these alterations are poorly understood. In a rat model of renal IR, we investigated whether the administration of the novel nonsteroidal mineralocorticoid receptor (MR) antagonist BR-4628 can prevent or treat the renal dysfunction and tubular injury induced by IR. Renal injury induced by ischemia was associated with increased oxidant damage, which led to a cysteine sulfenic acid modification in endothelin B receptor and consequently decreased endothelial nitric oxide synthase activation. These modifications were efficiently prevented by nonsteroidal MR antagonism. Furthermore, we demonstrated that the protective effect of BR-4628 against IR was lost when a selective endothelin B receptor antagonist was coadministered. These data describe a new mechanism for reduced endothelial nitric oxide synthase activation during renal IR that can be blocked by MR antagonism with BR-4628.
Keywords: acute renal failure, aldosterone, ischemia-reperfusion, nitric oxide
AKI is one of the most common complications in hospitalized and intensive care unit patients and is associated with adverse outcomes such as increased mortality rates and CKD development.1 An important cause of AKI is renal ischemia/reperfusion (IR).2 Currently, there are not any effective pharmacological approaches to treat or prevent AKI despite recent advances in the understanding of the mechanisms involved.3,4 Ischemic AKI is a complex entity in which multiple processes are involved, including tubular cell injury, endothelial alterations, increased oxidant stress, and inflammation.5,6 One of the hallmarks of ischemic AKI is the reduction in the renal blood flow.7 This alteration is mediated by numerous factors such as an increase in the production of vasoconstriction mediators and/or a reduction in the levels of vasodilator agents.5 It has been proposed that a reduction in the nitric oxide (NO) bioavailability makes an important contribution to the sustained vasoconstriction observed in renal IR, which perpetuates the injury as a consequence of worsened renal ischemia.8
Of particular interest is the role of mineralocorticoid receptor (MR) activation in modulating the blood flow during renal ischemia: previous studies have shown that MR antagonism with spironolactone protects against renal IR injury by preventing the reduction in the renal blood flow.9,10 The mechanisms by which MR antagonism leads to kidney protection remain unclear. Although the blockade of MR may be a promising therapeutic approach, the use of spironolactone in renal ischemia is limited by the increased risk of hyperkalemia, especially in patients with compromised renal function.11,12 Recently, novel nonsteroidal mineralocorticoid receptor antagonists (MRAs) such as BR-4628 have been described. BR-4628 is a dihydropyridine derivate and displays high selectivity and potency for MR.13 Furthermore, the risk of hyperkalemia may be less with this class of agents, at least in the chronic setting.14
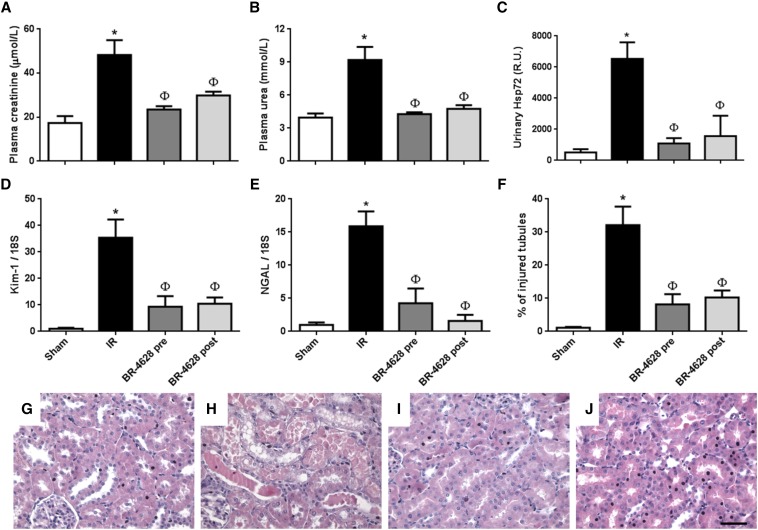
In this study we tested the efficiency of the nonsteroidal MRA BR-4628 to protect against renal injury induced by IR and provided insights into the mechanism of kidney protection conferred by MRA. First, we evaluated whether BR-4628 can prevent or treat renal injury induced by IR. AKI induced by bilateral renal IR was assessed by the increase in the plasma levels of creatinine (Figure 1A) and urea (Figure 1B). These alterations were prevented by BR-4628 when administered before or up to 3 hours after the ischemic insult. We determined the effects on the sensitive biomarkers of tubular injury such as Hsp72, Kim-1, and neutrophil gelatinase-associated lipocalin (NGAL). The increased urinary Hsp72 induced by IR was significantly reduced in rats treated with BR-4628 (Figure 1C). A similar pattern was observed for renal Kim-1 (Figure 1D) and NGAL (Figure 1E) mRNA levels. The tubular lesions induced by IR were documented by histologic analysis and the percentage of injured tubules was determined (Figure 1F). Kidneys from rats subjected to IR displayed tubular casts, tubular dilation, and cell detachment (Figure 1H). These structural alterations were also prevented by BR-4628 administration before (Figure 1I) or after (Figure 1J) the induction of the renal ischemia. As an indicator of apoptosis in the kidneys with IR, we analyzed the protein levels of cleaved caspase-3. Renal IR was characterized by an increase in cleaved caspase-3 levels, which was prevented by MR antagonism (Supplemental Figure 1). To evaluate if the treatment with BR-4628 reduced inflammation induced by renal IR, we performed immunohistochemistry for CD68 positive cells to evaluate macrophage infiltration in renal sections. Renal IR was associated with a marked increase in macrophage infiltration, an effect that was efficiently blunted by the administration of BR-4628 either before or after the induction of the renal injury (Supplemental Figure 2). The plasma levels of potassium remained unchanged either by IR or by MR antagonism with BR-4628 (Supplemental Figure 3). Therefore, the antagonism of MR by BR-4628 prevented or treated the renal dysfunction and tubular lesions induced by IR. These functional and histologic benefits were associated with the prevention of renal oxidant stress. Indeed, the production of reactive oxygen species (ROS) is a hallmark of IR and may induce damage to biomolecules such as proteins and alter their function.15 In addition to the ROS released upon renal reperfusion, it has been shown that MR activation contributes to increased ROS production by activation of NADPH oxidase in both endothelial and smooth muscle cells.16,17 Moreover, in endothelial cells aldosterone reduced the expression of glucose-6–phosphate dehydrogenase, a key regulator of the redox balance, therefore increasing oxidative stress.18 Renal IR increased the amount of oxidized proteins in the kidney, an effect that is blunted by MR antagonism before or after renal IR (Supplemental Figure 4A). BR-4628 administration also prevented the IR-induced increase in the urinary levels of hydrogen peroxide, a marker of oxidant stress (Supplemental Figure 4B).
Figure 1.
Benefit of BR-4628 (10 mg/kg) administration against renal injury induced by IR. Renal function was assessed by quantification of the plasma levels of (A) creatinine and (B) urea. As indicators of tubular injury: (C) the urinary levels of heat shock protein 72 were determined by western blot and the bands scanned for densitometric analysis and the mRNA levels in the kidney of kidney injury molecule-1 (D) and neutrophil gelatinase–associated lipocalin (E) were determined by RT-PCR. (F) The percentage of injured tubules was blindly quantified in ten fields per rat. Representative images from the hematoxylin-and-eosin staining are shown for sham (G), IR (H), BR-4628 pre (I), and BR-4628 post (J). Scale bar, 100 μm. n=5 per group. *P<0.05 versus sham and Φ P<0.05 versus IR.
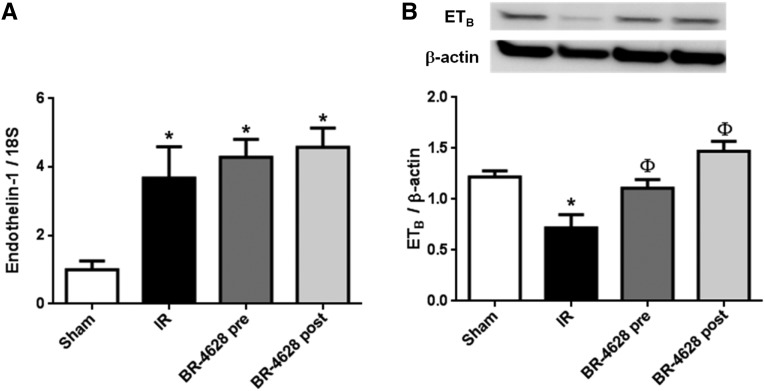
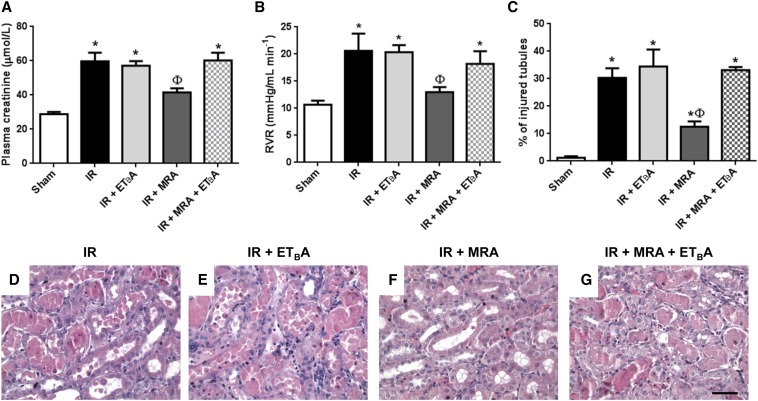
The underlying mechanisms of the benefit of MRA in renal IR are unclear; we hypothesized that the improvement in renal blood flow may be related to the effects of ET-1 on renal hemodynamics. ET-1 is one of the vasoactive substances that are altered during renal IR and may contribute to the enhanced vasoconstriction.19 ET-1 induces constriction when it binds on the ETA receptor in the smooth muscle cells. In contrast, when it binds the ETB receptor in endothelial cells, it exerts vasodilator actions through increased NO production by endothelial nitric oxide synthase (eNOS).20,21 As expected, renal IR induced an increase in mRNA levels of pre-pro-endothelin-1 (Figure 2A). This was not prevented by MR antagonism, suggesting that the effect of MRA is downstream of ET-1 production (Figure 2A). The mRNA levels of ETA receptor were not altered (data not shown). However, ETB receptor expression was reduced in IR (Figure 2B). This effect was prevented by BR-4628 administration before or after IR. To analyze whether the mechanism of kidney protection from IR by MR antagonism is dependent on the ETB receptor, we included another group of rats in which a selective ETB receptor antagonist (BQ-788)22 was coadministered with BR-4628. Renal IR was accompanied by increased plasma creatinine (Figure 3A) and renal vascular resistance (Figure 3B), reduced renal blood flow (Supplemental Figure 5A), and tubular injury (Figure 3C). No changes were observed for the mean arterial pressure among the groups (Supplemental Figure 5B). As previously reported,23 ETB antagonism had no effect on renal IR severity (similar levels of creatinine, renal blood flow, and renal injury in the IR+ BQ-788 group when compared with untreated IR rats) (Figure 3, A–C). Again, MR antagonism with BR-4628 was associated with protection against IR (Figure 3, A–C). Importantly, ETB receptor antagonism fully blunted the protective effect of BR-4628: creatinine levels remained elevated, renal vascular resistance was augmented, and histology analysis indicated a similar degree of renal injury compared to those in the nontreated IR group, showing that the protective effect of MRA is lost when an ETB antagonist is coadministered.
Figure 2.
Effect of renal IR on ET-1 and ETB receptor. (A) mRNA levels of endothelin-1. (B) The upper inset shows a representative western blot analysis for the levels of ETB receptor in the kidney cortex and the lower inset the densitometric analysis. n=5 per group. *P<0.05 versus sham and Φ P<0.05 versus IR.
Figure 3.
The benefit of BR-4628 is prevented by ETB receptor antagonism. (A) Plasma creatinine levels as an indicator of renal function. (B) The renal vascular resistance. (C) The percentage of injured tubules was quantified in hematoxylin-and-eosin–stained slides. Representative images from the hematoxylin-and-eosin staining are shown for IR (D), IR+ETBA (E), IR+MRA (F), and IR+ETBA+MRA (G). ETBA=ETB receptor antagonist. MRA = Mineralocorticoid receptor antagonist. Scale bar, 100 μm. n=5 per group. *P<0.05 versus sham and Φ P<0.05 versus IR.
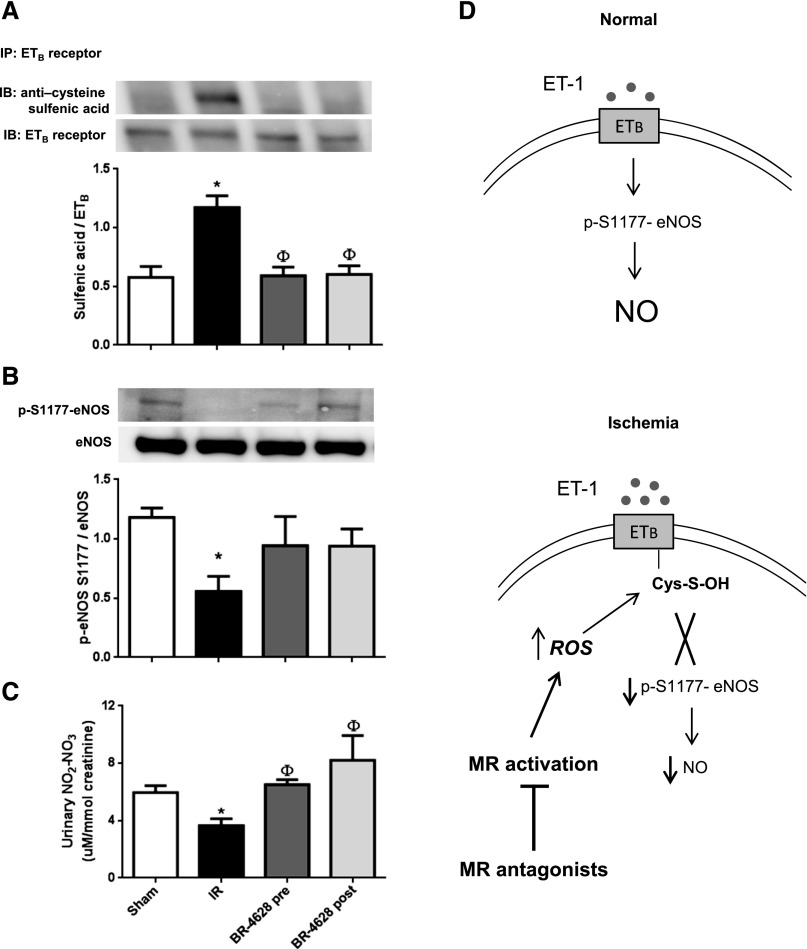
To understand the underlying mechanisms linking the ETB receptor and the benefit of MR antagonism in IR-induced renal injury, we evaluated the presence of a cysteine sulfenic acid modification, a post-translational modification of ETB. It has been previously reported that Cysteine 405 (Cys405) of ETB can be modified, preventing its activation and, therefore, preventing increased eNOS activity mediated by the ETB receptor when stimulated by ET-1.24 In cultured pulmonary artery endothelial cells, aldosterone induces inactivation of the ETB receptor through a mechanism involving MR activation, increased oxidant stress, and sulfenic acid modification in Cys405, thus leading to reduced NO production.25 We hypothesized that this mechanism could be translated in vivo and underlies the benefit of the BR-4628 MRA in IR. ETB sulfenic acid modification was analyzed in kidneys following IR, with or without treatment with the BR-4628 MRA. Renal IR induced ETB receptor sulfonilation in vivo (Figure 4A). These data suggest that NO bioavailability may be reduced during renal IR due to ETB inactivation by a cysteine sulfenic acid modification. To support this idea we analyzed the phosphorylation of eNOS on Serine residue 1177 (S1177), which is known to activate the production of NO by eNOS,26 as well as urinary nitrite and nitrate excretion as an indirect measurement of NO production.27,28 During renal IR, phosphorylation of the S1177 residue was decreased (Figure 4B), and this effect was associated with a reduction in urinary nitrite and nitrate excretion (Figure 4C). MR antagonism with BR-4628 prevented the sulfenic acid modification of the ETB receptor (Figure 4A), and prevented the decrease of S1177 eNOS phosphorylation (Figure 4B). Moreover, the reduction of urinary nitrites and nitrates was prevented by MRA given before or after the induction of renal IR (Figure 4C).
Figure 4.
Effect of renal IR on ETB receptor sulfenic acid modification and eNOS phosphorylation. (A) ETB receptor was immunoprecipitated from kidney proteins extracted in dimedone lysis buffer and immunoblotting was performed to detect the protein sulfenic acid levels (R-SOH). (B) The activation of eNOS was determined by the levels of phosphorylation in the S1177 residue of eNOS determined by western blot analysis. (C) The urinary levels of nitrites and nitrates were quantified and normalized by urinary creatinine. (D) Schematic representation of ET-1 signaling through ETB receptor in the endothelial cells on normal conditions or schematic representation of altered ETB signaling during renal ischemia leading to reduced NO production in the endothelial cell. n=5 per group. *P<0.05 versus sham and Φ P<0.05 versus IR. IP, immunoprecipitation; IB, immunoblotting.
Therefore, during renal IR there is an increased production of ROS, which in turn induces a sulfenic acid modification in the ETB receptor, preventing its ability to stimulate eNOS and NO production. This results in renal vasoconstriction and decreased blood flow (Figure 4D). On the other hand, when MR is antagonized with BR-4628 the oxidant injury and the sulfenic acid modification on the ETB receptor are prevented, thus maintaining normal eNOS activation and NO balance, which appear to blunt the deleterious effects of IR (Figure 4D).
In summary, we report that BR-4628, a novel nonsteroidal MR antagonist, is a novel pharmacological agent for prevention or treatment of AKI in a rat model of renal IR injury. Moreover, we provide evidence that, during renal IR, the ETB receptor undergoes sulfenic acid modification of a critical cysteine residue that decreases the activation of eNOS and hence NO production. Finally, we demonstrated that the benefit of the nonsteroidal MR antagonist BR-4628 against renal IR is dependent on ETB receptor activation and increased NO bioavailability. Altogether, these data support the use of nonsteroidal MR antagonists in the clinical practice for the prevention and/or treatment of ischemic AKI.
CONCISE METHODS
Experimental Protocols
All the experiments involving animal manipulation were performed according to the ethical guidelines of the Institut National de la Santé et de la Recherche Médicale for the care and use of laboratory animals. Male Wistar rats (Janvier Labs, France) weighing 270–300 g were included in the study. The BR-4628 was administered at a dose of 10 mg/kg by oral gavage in vehicle (40% kolliphor, 10% ethanol, and 50% water); the dose was selected according to previous studies performed in rats.29 In the first set of experiments, 20 rats were divided into four groups: sham-operated rats, rats that underwent 25 min of bilateral ischemia (IR), rats that received doses of BR-4628 at 48, 24 and 1 hour before the induction of IR (BR-4628 pre), and rats receiving BR-4628 (10 mg/kg) 3 hours after the IR (BR-4628 post). For the second set of experiments, 30 rats were divided into five groups: sham-operated rats, rats that underwent 25 min of bilateral ischemia (IR), rats receiving the ETB antagonist BQ-788 for 2 days before IR (ETBA), rats receiving BR-4628 for 2 days before the induction of IR (MRA), and rats receiving BR-4628 and BQ-788 for 2 days before renal ischemia (ETBA + MRA). Rats were euthanized 24 hours after IR.
Kidney IR Injury Model
The rats were anesthetized by an intraperitoneal injection of sodium pentobarbital (30 mg/kg) and placed on a heating pad with a rectal probe to maintain a constant body temperature of around 37°C. An abdominal incision was performed and both renal pedicles were exposed and dissected. Renal ischemia was induced by placing nontraumatic vascular clamps over the pedicles and was visually verified by the change in kidney color. After 25 min the clamps were released and the reperfusion was corroborated by the return of oxygenated blood to the kidney. The abdominal incision was closed in two layers with 5–0 sutures and the reperfusion was allowed for 24 hours.
Evaluation of Functional Parameters
After 24 hours of reperfusion the rats were anesthetized with an intraperitoneal injection of sodium pentobarbital (30 mg/kg) and placed on a heating pad. The right femoral artery was catheterized with polyethylene tubing (PE-50) in order to monitor and register the mean arterial pressure with the help of an IWX/214 unit. The left renal artery was dissected and the renal blood flow was recorded by placing an ultrasound flow probe (Transonic) filled with ultrasonic coupling gel around the artery. A blood sample was taken and the plasma creatinine and urea concentrations were determined by an automatic analyzer (Konelab 20i, Thermo Fisher Scientific). The plasma levels of potassium were analyzed by flame photometer. At the end of the experiment the right kidney was removed and fixed in Bouin Fixative solution and the left kidney was quickly frozen for molecular studies.
Histologic Analysis
After fixation of the tissue, the kidney slices were dehydrated and embedded in paraffin. Sections of 4 μm were made and stained by hematoxilin and eosin. For each rat, 10 subcortical fields were visualized and analyzed on a Leica DM4000 microscope at a magnification of ×200. The percentage of injured tubules was blindly analyzed. Tubular injury was assessed in hematoxylin-and-eosin–stained sections in at least 10 cortical fields per rat. The number of tubules displaying epithelial cell necrosis and detachment, cast formation, or tubular dilation was determined. The percentage of injured tubules was referred to the total number of tubules per field. For CD68 immunohistochemistry studies, 4 μm sections from paraffin-embedded tissues were dewaxed and probed against CD68 (ED1) (ab31630 antibody; Abcam, Inc.). Ten cortical fields (magnification ×400) were randomly recorded from each kidney slide. The number of cells that were positive for CD68 were counted and reported as CD68 positive cells per high power field.
RNA Extraction and Real-Time PCR
Total RNA extraction was carried out from the kidney cortex by using the TRIZOL reagent (Life Technologies, Carlsbad, CA) according to the manufacturer’s instructions. The reverse transcription was performed with 1 μg of RNA and the Superscript II Reverse Transcription Kit (Life Technologies). Transcript levels of genes were analyzed by real-time PCR (fluorescence detection of SYBR green) in an iCycler iQ apparatus (Bio-Rad). The mRNA levels were normalized by the amount of 18S as an endogenous control. The primer sequences of the analyzed genes are listed in Supplemental Table 1.
Oxyblot
The protein carbonylation levels were assessed with the Oxyblot protein oxidation detection kit, following the manufacturer’s instructions (Chemicon, EMD Millipore). For each assay, 10 μg of protein were used. To quantify protein oxidation, we defined an oxidation index as the ratio of the densitometric value of the Oxyblot bands to the β-actin levels (Las3000 DarkBox; Fuji Photo Film (Europe) GmbH, Dusseldorf, Germany).
Western Blot Analysis
Total renal proteins were isolated from cortexes from each group and homogenized in 1% SDS homogenization buffer with protease inhibitor (Roche Diagnostics). Protein samples containing 20 μg of total protein were diluted in Laemmli buffer and heated at 95°C. The proteins were resolved in 4%–15% Mini-PROTEAN TGX precast polyacrylamide gels (Bio-rad) and transferred onto polyvinylidinedifluoride membranes (Bio-Rad). Membranes were then blocked with 5% blotting-grade nonfat dry milk. Membranes were then incubated in 0.1% blotting-grade nonfat dry milk with their respective antibodies. Specific antibodies against ETB (1:500; Santa Cruz Biotechnology), Caspase-3 (1:200; Santa Cruz Biotechnology), or pS1177-eNOS (1:5000; Abcam, Inc.) were used. After incubation with primary antibody, membranes were washed and incubated with their respective secondary antibody. As a loading control, membranes were incubated) overnight at 4°C with goat anti-actin antibody (1:5000 dilution; Santa Cruz Biotechnology). Proteins were detected with an enhanced chemiluminescence kit (Bio-Rad). For urinary Hsp72 detection by western blot, urine was diluted 1:100 in 0.9% saline solution, and 10 µl of each dilution was loaded and resolved by 8.5% SDS-PAGE electrophoresis and electroblotted, as previously described. Membranes were then blocked with 5% blotting‐grade nonfat dry milk and incubated in 0.1% blotting‐grade nonfat dry milk with anti-Hsp72 antibody (1:10,000; Santa Cruz Biotechnology).
Immunoprecipitation
For immunoprecipitation analysis the tissues from each group were pooled and the proteins were extracted in dimedone lysis buffer. ETB receptor was immune-precipitated using protein A agarose beads (Thermo Fisher Scientific) and 4 μg of anti-ETB antibody (Santa Cruz Biotechnology). The immune-precipitated proteins were eluted by boiling in Laemmli buffer, and blotted and probed for anticysteine sulfenic acid (EMD Millipore) and ETB.
Urinary Hydrogen Peroxide and Nitrate and Nitrite Excretion
The urinary levels of hydrogen peroxide were detected with the Amplex® Red kit (Life Technologies) according to the manufacturer’s instructions. For the detection of urinary nitrates and nitrites the colorimetric nitric oxide assay kit (Oxford Biomedical Research) was used. The data were normalized by the urinary creatinine.
Statistical Analyses
The results are represented as mean±SEM. The statistical differences among the groups were determined by Kruskal–Wallis test using the Dunn’s post hoc test for multiple comparisons in the GraphPad Prism 6 software. The P value < 0.05 was defined as statistically significant.
Disclosures
Peter Kolkhof is an employee at Bayer HealthCare Pharmaceuticals.
Supplementary Material
Acknowledgments
This work was supported by grants from the Institut National de la Santé et de la Recherche Médicale, the “Centre de Recherche Industrielle et Technique,” the Fondation de France, the Agence de la Biomédecine (Appel d’offre recherche “greffe” 2014), and a research grant from Bayer (12127a10). J.B.-C. was supported by a postdoctoral fellowship from the French Society of Nephrology (SPF2012FDR_SN) and the French Foundation for Medical Research (SPF20130526725).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Mineralocorticoid Receptor Antagonism in AKI: A New Hope?,” on pages 335–337.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2014121216/-/DCSupplemental.
REFERENCES
- 1.Lewington AJ, Cerdá J, Mehta RL: Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int 84: 457–467, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta RL, Pascual MT, Soroko S, Savage BR, Himmelfarb J, Ikizler TA, Paganini EP, Chertow GM, Program to Improve Care in Acute Renal Disease : Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int 66: 1613–1621, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Kinsey GR, Okusa MD: Pathogenesis of acute kidney injury: foundation for clinical practice. Am J Kidney Dis 58: 291–301, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jo SK, Rosner MH, Okusa MD: Pharmacologic treatment of acute kidney injury: why drugs haven’t worked and what is on the horizon. Clin J Am Soc Nephrol 2: 356–365, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Bonventre JV, Yang L: Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 121: 4210–4221, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharfuddin AA, Molitoris BA: Pathophysiology of ischemic acute kidney injury. Nat Rev Nephrol 7: 189–200, 2011 [DOI] [PubMed] [Google Scholar]
- 7.Sutton TA, Fisher CJ, Molitoris BA: Microvascular endothelial injury and dysfunction during ischemic acute renal failure. Kidney Int 62: 1539–1549, 2002 [DOI] [PubMed] [Google Scholar]
- 8.Phillips L, Toledo AH, Lopez-Neblina F, Anaya-Prado R, Toledo-Pereyra LH: Nitric oxide mechanism of protection in ischemia and reperfusion injury. J Invest Surg 22: 46–55, 2009 [DOI] [PubMed] [Google Scholar]
- 9.Mejía-Vilet JM, Ramírez V, Cruz C, Uribe N, Gamba G, Bobadilla NA: Renal ischemia-reperfusion injury is prevented by the mineralocorticoid receptor blocker spironolactone. Am J Physiol Renal Physiol 293: F78–F86, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Sánchez-Pozos K, Barrera-Chimal J, Garzón-Muvdi J, Pérez-Villalva R, Rodríguez-Romo R, Cruz C, Gamba G, Bobadilla NA: Recovery from ischemic acute kidney injury by spironolactone administration. Nephrol Dial Transplant 27: 3160–3169, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Weir MR, Rolfe M: Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin J Am Soc Nephrol 5: 531–548, 2010 [DOI] [PubMed] [Google Scholar]
- 12.Palmer BF: Managing hyperkalemia caused by inhibitors of the renin-angiotensin-aldosterone system. N Engl J Med 351: 585–592, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Fagart J, Hillisch A, Huyet J, Bärfacker L, Fay M, Pleiss U, Pook E, Schäfer S, Rafestin-Oblin ME, Kolkhof P: A new mode of mineralocorticoid receptor antagonism by a potent and selective nonsteroidal molecule. J Biol Chem 285: 29932–29940, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pitt B, Kober L, Ponikowski P, Gheorghiade M, Filippatos G, Krum H, Nowack C, Kolkhof P, Kim SY, Zannad F: Safety and tolerability of the novel non-steroidal mineralocorticoid receptor antagonist BAY 94-8862 in patients with chronic heart failure and mild or moderate chronic kidney disease: a randomized, double-blind trial. Eur Heart J 34: 2453–2463, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Himmelfarb J, McMonagle E, Freedman S, Klenzak J, McMenamin E, Le P, Pupim LB, Ikizler TA, The PICARD Group : Oxidative stress is increased in critically ill patients with acute renal failure. J Am Soc Nephrol 15: 2449–2456, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Caprio M, Newfell BG, la Sala A, Baur W, Fabbri A, Rosano G, Mendelsohn ME, Jaffe IZ: Functional mineralocorticoid receptors in human vascular endothelial cells regulate intercellular adhesion molecule-1 expression and promote leukocyte adhesion. Circ Res 102: 1359–1367, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Callera GE, Touyz RM, Tostes RC, Yogi A, He Y, Malkinson S, Schiffrin EL: Aldosterone activates vascular p38MAP kinase and NADPH oxidase via c-Src. Hypertension 45: 773–779, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Leopold JA, Dam A, Maron BA, Scribner AW, Liao R, Handy DE, Stanton RC, Pitt B, Loscalzo J: Aldosterone impairs vascular reactivity by decreasing glucose-6-phosphate dehydrogenase activity. Nat Med 13: 189–197, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilhelm SM, Simonson MS, Robinson AV, Stowe NT, Schulak JA: Endothelin up-regulation and localization following renal ischemia and reperfusion. Kidney Int 55: 1011–1018, 1999 [DOI] [PubMed] [Google Scholar]
- 20.Liu S, Premont RT, Kontos CD, Huang J, Rockey DC: Endothelin-1 activates endothelial cell nitric-oxide synthase via heterotrimeric G-protein betagamma subunit signaling to protein jinase B/Akt. J Biol Chem 278: 49929–49935, 2003 [DOI] [PubMed] [Google Scholar]
- 21.Mazzuca MQ, Khalil RA: Vascular endothelin receptor type B: structure, function and dysregulation in vascular disease. Biochem Pharmacol 84: 147–162, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishikawa K, Ihara M, Noguchi K, Mase T, Mino N, Saeki T, Fukuroda T, Fukami T, Ozaki S, Nagase T, Nishikibe M, Yano M: Biochemical and pharmacological profile of a potent and selective endothelin B-receptor antagonist, BQ-788. Proc Natl Acad Sci U S A 91: 4892–4896, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuro T, Kohnou K, Kobayashi Y, Takaoka M, Opgenorth TJ, Wessale JL, Matsumura Y: Selective antagonism of the ETA receptor, but not the ETB receptor, is protective against ischemic acute renal failure in rats. Jpn J Pharmacol 82: 307–316, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Okamoto Y, Ninomiya H, Tanioka M, Sakamoto A, Miwa S, Masaki T: Palmitoylation of human endothelinB. Its critical role in G protein coupling and a differential requirement for the cytoplasmic tail by G protein subtypes. J Biol Chem 272: 21589–21596, 1997 [DOI] [PubMed] [Google Scholar]
- 25.Maron BA, Zhang YY, White K, Chan SY, Handy DE, Mahoney CE, Loscalzo J, Leopold JA: Aldosterone inactivates the endothelin-B receptor via a cysteinyl thiol redox switch to decrease pulmonary endothelial nitric oxide levels and modulate pulmonary arterial hypertension. Circulation 126: 963–974, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rafikov R, Fonseca FV, Kumar S, Pardo D, Darragh C, Elms S, Fulton D, Black SM: eNOS activation and NO function: structural motifs responsible for the posttranslational control of endothelial nitric oxide synthase activity. J Endocrinol 210: 271–284, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barrera-Chimal J, Pérez-Villalva R, Ortega JA, Uribe N, Gamba G, Cortés-González C, Bobadilla NA: Intra-renal transfection of heat shock protein 90 alpha or beta (Hsp90α or Hsp90β) protects against ischemia/reperfusion injury. Nephrol Dial Transplant 29: 301–312, 2014 [DOI] [PubMed] [Google Scholar]
- 28.Kwon O, Hong SM, Ramesh G: Diminished NO generation by injured endothelium and loss of macula densa nNOS may contribute to sustained acute kidney injury after ischemia-reperfusion. Am J Physiol Renal Physiol 296: F25–F33, 2009 [DOI] [PubMed] [Google Scholar]
- 29.Schupp N, Kolkhof P, Queisser N, Gärtner S, Schmid U, Kretschmer A, Hartmann E, Oli RG, Schäfer S, Stopper H: Mineralocorticoid receptor-mediated DNA damage in kidneys of DOCA-salt hypertensive rats. FASEB J 25: 968–978, 2011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.