Abstract
Anorexia nervosa (AN) is perhaps the most lethal mental disorder, in part due to starvation-related health problems, but especially because of high suicide rates. One potential reason for high suicide rates in AN may be that those affected face pain and provocation on many fronts, which may in turn reduce their fear of pain and thereby increase risk for death by suicide. The purpose of the following studies was to explore whether repetitive exposure to painful and destructive behaviors such as vomiting, laxative use, and non-suicidal self-injury (NSSI) was a mechanism that linked AN-binge-purging (ANBP) subtype, as opposed to AN-restricting subtype (ANR), to extreme suicidal behavior. Study 1 utilized a sample of 787 individuals diagnosed with one or the other subtype of AN, and structural equation modeling results supported provocative behaviors as a mechanism linking ANBP to suicidal behavior. A second, unexpected mechanism emerged linking ANR to suicidal behavior via restricting. Study 2, which used a sample of 249 AN patients, replicated these findings, including the second mechanism linking ANR to suicide attempts. Two potential routes to suicidal behavior in AN appear to have been identified: one route through repetitive experience with provocative behaviors for ANBP, and a second for exposure to pain through the starvation of restricting in ANR.
Keywords: anorexia, suicide, restricting, purging, self-injury
Anorexia nervosa (AN), a disorder characterized by an incessant pursuit of thinness even after reaching an extremely low body weight, is a deadly disease (Sullivan, 2002), with a standardized mortality ratio (SMR; the ratio of number of actual deaths to expected deaths in the population) ranging from 6.2 in recent studies (Papadopoulos, Ekbom, Brandt, & Ekselius, 2009), to as high as 17.8. (Norring & Sohlberg, 1993). Contrary to popular belief, the majority of deaths from AN are by suicide, not from medical complications that result from prolonged starvation (e.g., Crisp, Callender, Halek, & Hsu, 1992; Fedorowicz, Falissard, Foulon, Dardennes, Guelfi, et al., 2007; Harris, E. C., & Barraclough, 1997). Keel and colleagues found that people with AN were almost 57 times more likely to die by suicide than those in the general population (SMR=56.90; 2003). Remarkably, these rates of death by suicide are high even as compared to rates for other lethal mental disorders, such as schizophrenia and major depressive disorder (Harris & Barraclough, 1997).
The elevated suicide rate evidenced in people with AN begs a question: What are the mechanisms through which AN confers such a high risk for suicide? One explanation is that the suicide rates reported in published studies are inflated due to their reliance on inpatient samples (which arguably represent more serious cases). Yet studies have found that not only does a history of hospitalization for eating disorders appear to have no effect on risk for suicide, but that eating disordered patients who had been hospitalized actually appear to have a lower risk for death by suicide than those who have not been hospitalized (Keel et al., 2003; Papadopoulos, Ekbom, Brandt, & Ekselius, 2009).
Another explanation is what some have called the “fragility hypothesis” (Joiner, Van Orden, Witte, & Rudd, 2009). According to this hypothesis people with AN die by suicide at an elevated rate due to the starvation-induced frailty of their bodies. Attempts that would not be lethal for a normal weight individual might result in death in people with AN, due to their weakened condition. However, results from studies that report the methods of suicide used suggest that the attempts made by people with AN are lethal enough to kill even the healthiest individuals (Bulik et al., 2008; Holm-Denoma et al., 2007).
Anorexia Nervosa and the Acquired Capability for Suicidal Behavior
The Interpersonal-Psychological theory of suicidal behavior (IPTS; Joiner, 2005) poses that there are three proximal, jointly necessary, and jointly sufficient causes which must be present before a person will die by suicide; these are: 1) feelings of perceived burdensomeness, 2) a sense of thwarted belongingness, and 3) an acquired capability to enact lethal self-injury. Although AN has been found to influence belongingness and burdensomeness (e.g., de la Rie, Noordenbos, Donker, Furth, 2007; de la Rie, van Furth, De Koning, Noordenbos & Donker, 2005; Hillege, Beale, & McMaster, 2006; Simon, Schmidt, & Pilling, 2005; Tiller et al., 1997), the primary focus of this study is on the third factor, fearlessness about pain and death (subsequently referred to as the acquired capability for suicide).
Death by suicide is inherently fearsome, and often involves substantial pain. The IPTS suggests that the acquired capability is developed over time through repeated experience with painful and/or provocative events, ultimately decreasing fear of pain and death, through habituation. Studies supporting this hypothesis have found that painful experiences such as car accidents, non-suicidal self-injury, previous suicide attempts, childhood abuse, and exposure to combat during wartime have been all linked to later suicidal behavior (Joiner et al., 2007; Van Orden et al., 2008; Selby et al., in press). Other impulsive behaviors, for example skydiving, intravenous drug use, physical fights, and jumping from high places have also been linked to suicidal behavior (Van Orden et al., 2008). Importantly, provocative behaviors have also been found to be correlated with one’s perceived ability to enact lethal self-injury (r=.29, p<.01; Van Orden et al., 2008). For more detail about the various ways that painful and provocative experiences can influence acquired capability and subsequently death by suicide please see a review of the IPTS conducted by Van Orden and colleagues (in press).
Based on the IPTS, then, people with AN should possess high levels of acquired capability for suicide due to painful and provocative experiences such as damaging weight control methods, other associated behaviors such as self-injury, and habitual starvation. Weight control methods damage tissues, exert pain, and have adverse health consequences (Sidiropoulos, 2007; Baker & Sandle, 1996; Hellstrom, 2007). Thus, the repetition of the types of painful behaviors necessary to keep one’s weight drastically low, accompanied by enduring the painful sequelae of these behaviors, is likely to inure one to the painful effects of these behaviors, potentially resulting in a fearlessness and stoicism towards the experience of pain. There is no doubt that the effects of starvation are also painful; moreover, starvation has deleterious effects on every organ of the body. Although the acquired capability has not been directly tested in individuals with AN there is a large body of research which shows that people with AN have higher pain tolerance, an analogue of acquired capability, as compared to healthy controls (e.g., Claes, Vandereycken, Vertommen, 2006; Lautenbacher, Pauls, Strian, Pirke, & Krieg, 1991; Raymond et al., 1995).
The idea of fearlessness in the face of pain and death in AN may seem paradoxical, as previous research has found that AN is associated with high levels of harm avoidance (Klump et al., 2004), a trait that manifests as increased worry, shyness, fearfulness, and increased behavioral inhibition in order to avoid punishment. Low harm avoidance, on the other hand, may result in more bold, confident behavior – and would seem more in line with acquired capability. Yet harm avoidance and a lack of fear of death may not be mutually exclusive. For example, some individuals may have no fear of one thing (e.g. spiders) and be terrified of another (e.g. giving a speech). Many with AN may avoid situations that are interpersonally problematic or that may interfere with personal goals, but they may also be more tolerant of the discomfort and pain involved in compensatory behaviors. This same reasoning may extend to self-injurious and suicidal behaviors.
Differential risk for death by suicide across AN-subtypes?
Importantly, the acquired capability aspect of the IPTS may explain the high rate of suicide in AN, but it also makes predictions about which subtype of AN one would expect to be most lethal. Specifically, the theory would predict that the binge-purge subtype of AN (ANBP) should confer greater suicide risk because people with this subtype are likely to engage in even more painful and provocative behaviors than people with the restricting subtype of AN (ANR). Although people with ANR and ANBP both restrict, those with ANBP will additionally employ painful purging behaviors. Furthermore, individuals with ANBP are more likely to engage in impulsive behaviors, such as delinquency and substance use (e.g., Wonderlich, Connolly, & Stice, 2004), which may result in the experience of pain.
Although relatively few studies have been conducted which closely examine suicidal behavior by AN subtype, those that have been conducted seem to support this prediction. Some studies have found that individuals with ANBP had more suicide attempts than individuals with ANR (Bulik et al., 2008; Favaro & Santonastaso, 1997), diagnostic migration from ANR to ANBP increases the likelihood of a suicide attempt (Foulon et al., 2007), and purging behaviors are highly associated with suicide attempts (Franko & Keel, 2006; Tozzi et al., 2006). Furthermore, researchers have found that individuals with ANBP have higher pain tolerance than individuals with ANR (Papežova, Yamamotova, & Uher, 2005). Despite the findings that ANBP individuals have higher rates of suicidality, ANR individuals still appear to have elevated levels of suicide attempts compared to the general population (Franko & Keel, 2006).
Current Studies
The purpose of the current studies was to determine whether the acquired capability component of the IPTS provides a useful mechanism for understanding suicidal behavior in people with AN. Specifically, we theorized that higher levels of acquired capability would be the mechanism that links those with ANBP to higher levels of suicidal behavior than those with ANR. Although the other components of IPTS theory may be relevant to suicide in AN, they were not examined in these studies. It was hypothesized that the relation between ANBP and extreme suicidal behavior (i.e. more frequent and lethal) would be fully mediated by a “Provocative Behaviors” latent variable, comprised of both eating disordered and non-eating disordered behaviors. This hypothesis was tested using structural equation modeling in two large samples of individuals diagnosed with either ANBP or ANR. As will be seen in both Study 1 and Study 2, support was found for the hypothesized mechanism, and furthermore a second mechanism linking ANR to suicidal behavior also emerged, namely, restricting.
Study 1
Methods
Participants
Participants consisted of 787 primarily European ancestry, primarily female (96%) individuals enrolled in a NIH funded Genetics of Anorexia Nervosa (GAN) Collaborative Study. This was a multi-site study that took place in various research and clinical settings across North America and Europe. The full methods for this investigation can be found in Kaye et al. (2008). Although the number of male participants in the sample was somewhat small (N = 33), we thought that it was important to conduct the study with male participants included because studies indicate that males account for approximately 10% of all bulimic and anorexic patients (Carlat, Carmargo, & Herzog, 1997), and this rate may be increasing (Braun, 1999). Including males in the study may also increase the generalizability of the findings.
To be included in this study, all participants had to be over age 16 and have had a lifetime diagnosis of AN according to DSM-IV criteria (with or without amenorrhea) by age 45. The amenorrhea criterion was waived due to the lack of reliability of retrospective assessment in women, complications in assessment posed by frequent hormonal treatment, and that its presence/absence may not characterize AN individuals in a meaningful way (Gendall et al., 2006; Pinheiro et al., 2007). The standardized threshold for low weight was defined as a Body Mass Index (BMI) at or below 18 kg/m2 for females and 19.6 kg/m2 for males.1 Specific criteria for probands included having a diagnosis of AN at least 3 years before entry into the study and that they did not engage in regular binge eating as defined by the frequency and duration set forth by DSM-IV for bulimia nervosa. There were some probands who reported a history of binging, as well as some who engaged in current occasional binge-eating, however, only not at DSM-IV threshold for frequent binge-eating.
Lastly, to participate in the study all probands were required to have at least one first through third degree relative with AN who was willing to participate in the study. The exceptions to this were parents and MZ twins, who were not eligible because these relationships are not genetically informative for linkage analysis. Thus, all participants in the study had at least one affected relative who also participated. Exclusion criteria for potential participants included: a history of severe CNS trauma, psychotic disorders, developmental disability, or any other medical, neurological, or substance use disorder that could confound a diagnosis of AN or interfere with responding during assessment. Those who did not speak either English or German were also excluded from the study.
Assessment of ED Pathology
To assess for a diagnosis of AN, the Extended Screening Instrument, an expanded modified version of Module H of the Structured Clinical Interview for Axis I Disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1997), was used. Participants were diagnosed with AN and specified with subtypes of restricting (ANR), purging (ANP), binging and purging (ANBP), and AN with a history of bulimia nervosa (ANBN). A total of 357 individuals (45.4% of the sample) met criteria for ANR, 220 participants (25% of the sample) were diagnosed with ANP, 116 participants (14.7% of the sample) met criteria for ANBP, and 94 participants (11.9% of the sample) met criteria for ANBN. Inter-rater reliability for the eating disorder diagnoses in this study ranged from .93 to 1.0 (Kaye et al., 2008). Approximately 68.5% of the sample was indicated as currently experiencing symptoms of AN (Kaye et al., 2008).
Provocative Behaviors Variables
Painful and provocative events in this study were defined as events or behaviors that would elicit physical pain and/or fear in most people, such as self-induced vomiting, severe restriction, or non-suicidal self-injury. Although many of these behaviors are traditionally thought of as “impulsive behaviors,” recent research indicates that the relation between impulsivity and suicide is a function of the pain and fear that can arise from these impulsive behaviors (Smith et al., 2008; Witte et al., 2008). Thus, these behaviors may serve as good indicators of one’s potential habituation to pain and fear. The following variables were created for use as indicators of a Provocative Behaviors latent variable created to tap the construct of acquired capability:
Non-Eating Disordered Provocative Behaviors (NonEDPB)
The Eatatelife Phenotype (EATATE), Version 2.1, January 19, 2001 (Project EHE, 2001) The EATATE is a retrospective assessment of childhood perfectionism and rigidity as well as other personality traits which often predate the onset of an eating disorder. Of particular relevance to this study, information was also collected on behaviors that could be considered painful and/or provocative: excessive alcohol consumption, shoplifting or stealing, gambling, hitting someone or breaking things, provoking fights or arguments, fire setting, non-suicidal self-injury, overdosing, using street drugs, excessive spending, and disinhibited or reckless sexual activities. These behaviors were coded as the patient either engaged (1), or did not engage (0) in each behavior. The scores for all of these behaviors were then summed to create a continuous score where higher scores indicated more experience with these dysregulated behaviors. This variable demonstrated somewhat low internal consistency, ranging from α = .57 when either drug use or overdosing was included, and a potentially inflated α = .63 when both are included, due to the nested nature of the two questions.
Eating Disordered Provocative Behaviors (EDPB)
The Structured Interview for Anorexia Nervosa and Bulimic Syndromes (SIAB; Fichter et al., 1998) was used to assess many common behaviors found in individuals with eating disorder psychopathology. The following behaviors were assessed: appetite suppressant misuse, enema misuse, excessive exercise, fasting, Ipecac misuse, laxative misuse, self-induced vomiting, and diuretic misuse. Each of these eating behaviors was coded as to whether the patient ever (1) engaged in the behavior or never (0) engaged in the behavior. The scores for all behaviors were summed to create a continuous variable where higher scores indicated more use of these behaviors as compensatory mechanisms. This variable demonstrated adequate internal consistency (α = .63).
Suicidal Behavior Variables
Previous suicidal behavior was assessed with Section O of the Diagnostic Interview for Genetics Studies (DIGS; Nurnberger, et al., 1994). This portion of the DIGS contains in-depth questions about suicidal ideation and behaviors. Each of these variables was used to create a latent variable of Extreme Suicidal Behavior. Information obtained included:
Number of previous suicide attempts.
Lethality of most serious attempt, rated by the interviewer as: 0 = no previous suicide attempts, 1 = No danger (e.g., held pills in hand), 2 = minimal (e.g., scratch on wrist), 3 = Mild (e.g., 10 aspirin, mild gastritis), 4 = moderate (e.g., 10 Seconals, briefly unconscious), 5 = severe (e.g., cut throat), 6 = extreme (e.g., respiratory arrest or prolonged coma).
Intent to Die during most serious attempt, rated by the interviewer as: 0 = no previous suicide attempts, 1 = no or minimal intent, manipulative gesture; 2 = definite intent, but ambivalent; 3 = serious intent, expected to die.
Premeditation prior to most serious attempt, rated by the interviewer as: 0 = no previous suicide attempts, 1 = impulsive (less than 1 hour or forethought, used materials immediately at hand), 2 = somewhat premeditated (had suicidal ideation over hours or days, or intermittently throughout an episode, prior to making an attempt), 3 = thoroughly premeditated (persistent suicidal ideation over weeks, months, or longer prior to the attempt).
Classification of most serious attempt as a violent attempt: All individuals were rated on the severity of their attempt method for their most severe suicide attempt. The attempt was rated (1) for a violent attempt, as defined as gunshot, stabbing, hanging, or jumping from a high place. All other suicide attempts or no attempts were coded as (0). Approximately 2.8% of the sample was coded as having made a violent attempt.
Assessment of Co-Occurring Psychopathology
Axis I disorders were diagnosed using the Diagnostic Interview for Genetics Studies (DIGS; Nurnberger, et al., 1994). This diagnostic interview has been demonstrated to have strong inter-rater and test-retest reliability (Preisig et al., 1999; Roca et al., 2007). The inter-rater reliability of Axis I and II diagnoses in the GAN study ranged from .80 to 1.0 (Kaye et al., 2008). Although the full sample characteristics of the GAN collaborative study can be found in Kaye et al. (2008), we have provided information on the most frequent co-occurring disorders for each AN subtype. For the ANR group the most common co-occurring lifetime disorders were: major depressive disorder (64%), obsessive-compulsive disorder (38%), social phobia (17%), and alcohol abuse/dependence (14%). For the ANBP combined group the most common co-occurring lifetime disorders were: major depressive disorder (85%), obsessive-compulsive disorder (54%), alcohol abuse/dependence (34%), social phobia (25%), any drug abuse/dependence (24%), and post-traumatic stress disorder (15%). Below we provide more detail on assessments of specific disorders used as covariates in the study.
Lifetime Depression
Lifetime depression was used in the analyses for Study 1 as a covariate in order to demonstrate that the suicidal behavior of AN individuals was not primarily a function of depression. In this sample, 538 individuals (68% of the sample) met diagnostic criteria for a past episode of depression.
Borderline Personality Disorder (BPD)
All Axis II disorders were assessed using the Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II; First et al., 1997). Only borderline personality disorder (BPD) was used as a covariate in the analyses for Study 1, as it is a disorder that also has elevated suicide rates (Duberstein & Conwell, 1997) and high co-occurrence with eating disorders (Wonderlich, Swift, & Goodman, 1990). In this sample, 40 individuals (6% of the sample) met diagnostic criteria for BPD.
Data Analytic Strategy
The data for this study were analyzed using structural equation modeling (SEM), with analyses conducted using AMOS 6.0 (Arbuckle & Wothke, 1999). The model that was tested is displayed in Figure 1. This model explores the mediational effects of Provocative Behaviors (both eating disorder2 and non-eating disorder related) in the relation between AN status (ANR versus ANBP) and Extreme Suicidal Behavior. There were two latent variables in the model that were created to parse out potential error in measurement and capture the various facets of each construct better than observed variables alone can. The first latent variable in the model was Provocative Behaviors, which consisted of the eating disorder related painful behaviors variable (EDPB), and the non-eating disorder related painful behavior variable (NonEDPB). The second latent variable was Extreme Suicidal Behavior, which consisted of the following indicators: number of suicide attempts, lethality of the most serious attempt, length of premeditation prior to the most serious attempt, intent to die during the most serious attempt, and whether the most serious attempt was classified as violent or not.
Figure 1.
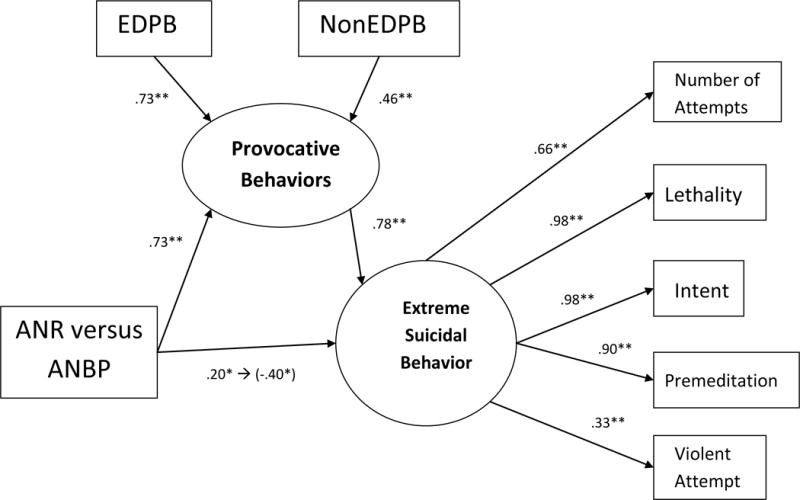
Study 1 model with Anorexia Nervosa (AN) status predicting Provocative Behaviors and Extreme Suicidal Behavior. N=787. AN Status was coded as ANR (restricting) = 1, ANBP (binging/purging) = 2; *=p<.05; **=p<.01; ➔ indicates the path before and after including Provocative Behaviors in the model. EDPB = Eating Disordered Provocative Behaviors; NonEDPB=Non-Eating Disordered Provocative Behaviors. Lifetime depression, borderline personality disorder, age, and sex were used as covariates in the analysis, but are not displayed for clarity of presentation.
Residual variables were placed on the latent variables to measure error in predicting the latent variables with the indicators. The following variables were used as covariates in the structural model, but are not shown in Figure 1 for ease of presentation: age, sex, lifetime depression, and diagnosis of BPD. Sex and age were used as covariates because women tend to have more suicide attempts (McIntosh, 2002), and age is generally correlated with number of suicide attempts (McIntosh, 2002). All exogenous variables (AN status and covariates) had direct paths to both latent variables and correlations with each other. A causal path was indicated between Provocative Behaviors and Extreme Suicidal Behavior.
In order to evaluate the overall model, the maximum likelihood chi-square statistic (χ2) was used (with non-significance indicating that the model fit the data perfectly). Due to the chi-square’s sensitivity to large sample sizes, other fit indices were also used including the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the Tucker-Lewis index (TLI). Multiple cutoff criteria were used to determine if the model adequately fit the data, and consisted of CFI values greater than .95, RMSEA values of less than .08, and TLI values of .90 or higher (Hu & Bentler, 1999). To test individual parameter estimates, a cutoff criterion value for significance was set at p = .05. Due to missing data for some of the variables (30 participants were missing data at random; less than 4% of data was missing for the whole sample), full information maximum likelihood estimation (FIML; Anderson, 1957) was used. FIML provides less biased information than ad-hoc procedures such as listwise deletion, pairwise deletion, or imputation of means (Little & Rubin, 1987; Schafer, 1997).
Results
Preliminary Analyses
The age of participants ranged from 16 to 76 (mean = 29.7, SD = 11.2). The current BMIs of participants in this study ranged from 10.78 to 32.85 kg/m2, with an average BMI of 19.39 kg/m2 (SD = 2.57). Approximately 17% of the sample reported a previous suicide attempt, and of those 3% were classified as having made a recent, violent suicide attempt. Initial ANOVA analyses on the other variables used in the study indicated that there were significant group differences on most variables between the ANR group and the other subtypes, but there were no significant differences between ANP, ANBP, and ANBN groups. With this in mind, in subsequent analyses individuals with AN were separated into two groups: AN restricting (ANR) and AN binge eating-purging (ANBP), the latter of which consisted of ANP, ANBP, and ANBN participants3. For all analyses individuals with ANR were coded (1), and individuals with ANBP were coded (2).
Measurement Model
Before examining a structural equation model, Kline (2005) recommends that the measurement model be examined in order to detect potential problems with the latent variables to be used in the structural model. Accordingly, a confirmatory factor analysis was conducted with the two latent variables and consisted only of the two latent variables displayed in Figure 1. The measurement model met criteria for adequate fit (χ2 = 83.33, df = 13, p<.001, CFI = .98, TLI = .96, RMSEA = .08). All factor loadings of the manifest indicators were significant (p<.001) and were between .33 and .98. The correlation between Provocative Behaviors and Extreme Suicidal Behavior was significant (r = .58, p<.001) – a result, incidentally, consistent with the IPTS. Thus, an exploration of the measurement model indicated that the latent variables provided adequate fit to the data as two correlated factors, and all indicators significantly contributed to their corresponding latent variable.
Structural Model
The hypothesized model met criteria for adequate fit (χ2 = 209.00, df = 38, p<.001, CFI = .96, TLI = .92, RMSEA = .076)4. All indicators significantly loaded onto their latent variables (p<.05). When interpreting the results, it is important to note that ANR was coded as (1), and ANBP was coded as (2), which means that a positive path from AN status to another variable indicates a stronger relation to ANBP while a negative path from AN status indicates a stronger relation to ANR.
The model results indicated that our hypothesized mediational relation between ANBP and Extreme Suicidal Behavior through Provocative Behaviors was supported, with a significant, positive path from AN status to Pain Behaviors (p<.001, β=.73), and a significant, positive path from Pain Behaviors to Extreme Suicidal Behavior (p<.001, β=.78)5. These findings suggest that there was a positive association between ANBP and Provocative Behaviors, and that Provocative Behaviors had a positive association with Extreme Suicidal Behavior.
The path from AN status to Extreme Suicidal Behavior remained significant even after accounting for Provocative Behaviors (β = −.40, p<.05), indicating that a partial mediation effect was supported, rather than the predicted fully mediational effect. To confirm the original valence and magnitude of the relation between AN and Extreme Suicidal Behavior the analysis was rerun without the Provocative Behaviors variable included as a mediator. In this analysis the path was both significant and positive (β=.20, p<.05); the positive relation indicates that ANBP and suicidality are related, such that ANBP individuals reported more Extreme Suicidal Behavior than their ANR counterparts.
Interestingly, as noted above, when the Provocative Behaviors latent variable was introduced into the model, the relation between AN and Extreme Suicidal Behavior flipped from being significant and positive (β=.20; indicating a stronger relation between ANBP and suicidality) to being significant and negative (β = −.40; indicating a stronger association between ANR and suicidality). Given the finding that ANBP individuals tend to engage in more serious suicidal behavior than ANR individuals (Bulik et al., 2008), this finding was unexpected. This reverse in signs indicates that individuals with ANBP may have a stronger relation with suicidality through painful and provocative behaviors, but when these behaviors are accounted for, a unique relation between ANR and suicidality emerges such that individuals with ANR endorse more Extreme Suicidal Behavior than those with ANBP.
In the original model, the standardized indirect effect of AN status on Extreme Suicidal Behavior was β=.57, indicating a significant indirect effect of ANBP on suicidality. In order to test the meditational impact of Provocative Behaviors on the relations between AN status and Extreme Suicidal behavior, the PRODCLIN program was used. This program was developed by MacKinnon and colleagues (2007), and tests meditational effects without some of the problems inherent in other methods of testing for mediation (e.g. inflated rates of Type I error, see MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In addition, the logic for this method is well suited to testing for mediation in structural equation modeling (Bollen, 1987). PRODCLIN examines the product of the unstandardized path coefficients divided by the pooled standard error of the path coefficients (αβ/σαβ) and a confidence interval is generated, with a statistically significant mediation effect indicated by the absence of zero in the confidence interval. The unstandardized path coefficients and standard errors of the path coefficients for the indirect effect of AN status on Extreme Suicidal Behavior were entered into PRODCLIN, and produced a 95% confidence interval of .72 to 2.54. Because zero was not included in the confidence interval, we concluded that the relation between ANBP and Extreme Suicidal Behavior was significantly mediated by Provocative Behaviors.
Additional information regarding the model that was of interest, though not central to our main aims, was obtained. Both lifetime depression (β = .20, p<.001) and BPD (β = .19, p<.001) had significant paths to Provocative Behaviors. The direct paths from both depression and BPD to Extreme Suicidal Behavior were not significant, which suggests that there may be a full mediation effect of painful behaviors on the relation between these disorders and suicidal behavior (a result that is corroborative of the IPTS and of interest in its own right but is beyond the current scope and thus not expanded upon further). The other covariates (sex and age) did not significantly predict either Provocative Behaviors or Extreme Suicidal Behavior. There were significant correlations between the following: AN status and depression (r = .18, p<.001) such that individuals with ANBP had a higher prevalence of depression; AN status and BPD (r = .10, p<.01) such that individuals with ANBP had a higher prevalence of BPD; depression and BPD (r = .15, p<.001) such that individuals diagnosed with BPD had higher rates of lifetime depression than those without BPD diagnoses; AN status and sex (r = .13, p<.001) such that men in the sample tended to have ANBP slightly more than ANR; and AN status and age (r = .08, p<.05) such that the ANBP group was somewhat older.
Due to the unexpected switch of the relation between AN status and Extreme Suicidal Behavior after controlling for Provocative Behaviors, we generated a post-hoc hypothesis that restricting itself could cause a great deal of pain and increase risk for Extreme Suicidal Behavior, and we re-analyzed our model without fasting included in the EDPB variable. Removing fasting from the EDPB indicator would allow for more variance to be allocated from the Provocative Behaviors mediator to the direct path from AN to Extreme Suicidal Behavior. Thus, if fasting was driving the association between ANR and Extreme Suicidal Behavior, removing fasting from the mediator should have increased the strength of the direct path from AN to Extreme Suicidal Behavior. After rerunning the original model with fasting removed from the EDPB variable, the path from AN to Extreme Suicidal Behavior changed from β = −.40 to β = −.55, indicating that the strength of the relation between ANR and Extreme Suicidal Behavior increased, providing some support for our post-hoc hypothesis that fasting may be a second mechanism linking AN to suicidal behavior.
Study 1 Discussion
The results of Study 1 support our hypothesis that the relation between ANBP and Extreme Suicidal Behavior is mediated in part by behaviors such as laxative use and NSSI. This supports the IPTS notion that the ability to engage in suicidal behavior may develop through repetitive experience with these behaviors, causing habituation to pain and fear. A novel finding of Study 1 was that when controlling for Provocative Behaviors, the association between ANR and Extreme Suicidal Behavior became significant, suggesting that there may be a specific relation between ANR and Extreme Suicidal Behavior separate from that of the mechanism linking ANBP to Extreme Suicidal Behavior.
What might explain this unpredicted effect? Because most painful and fear inducing behaviors employed by individuals with AN were accounted for by the Provocative Behaviors latent variable, there was only one apparent difference between the two diagnostic subtypes that might be involved in the association between ANR and Extreme Suicidal Behavior: the degree of restricting engaged in, which for ANR individuals involves extremely limited food intake or complete refusal of food (APA, 1994). Extensive restriction is more characteristic of people with ANR and is perhaps qualitatively different from the restriction seen in people with ANBP, as people with ANBP may occasionally alleviate their hunger through binge eating episodes. Accordingly, we believe that extreme restricting may be a second route to development of acquired capability in AN.
Removing the fasting item from the EDPB indicator of the Provocative Behaviors mediator increased the magnitude of the relation between ANR and Extreme Suicidal Behaviors. Allowing the fasting item to contribute to the path between ANR and Extreme Suicidal Behavior, rather than to the Provocative Behaviors mediator, may explain this increase in relation strength. This finding suggests that fasting/restriction may be a painful behavior influencing the relation between ANR and suicidal behavior. It may be that extensive experience with the pain induced by restriction increases the acquired capability for suicide in individuals with ANR, and that this represents a second mechanism through which AN is linked to suicidal behavior.
There was an important limitation of note with Study 1. The Provocative Behaviors variables were created from Likert scale questions regarding how much one engaged in a particular behavior (e.g. for vomiting the response options were: never, rarely (less than twice a week), sometimes (at least twice a week), frequently (up to once a day), very frequently (several times a day). For this study, these responses were then dichotomized so that the participant was scored a 0 if they never engaged in the behavior and 1 one for all other responses. This method of assessment gauges whether one has used a behavior, which is relevant to our hypothesized mechanism linking ANBP to suicidality, but it does not account for frequency of engagement in a behavior. For example, one might use only one of the behaviors list (e.g., vomiting), but engage in that behavior frequently, which may have a similar influence on suicidal behavior as using a broad array of these behaviors.
Study 2
Despite finding two possibly different routes to suicidal behavior in AN, the detection of the relation between ANR and suicidal behavior was not originally predicted. Furthermore, Study 1 assessed the number of types of painful behaviors that might be used in AN, but it did not account for the frequency of those behaviors. In order to explore both mechanisms a second time, and to include frequency of provocative behaviors in the model, we analyzed a similar model in a second sample of ANR and ANBP participants. We again predicted a positive, indirect effect between ANBP and suicidal behavior, which flowed through a Provocative Behaviors mediational variable. We also made a riskier prediction: in the presence of the Provocative Behaviors mediator the relation between AN and suicidal behavior would be negative, indicating that ANR also has a distinct relation with suicidal behavior, through persistent restriction. Study 2 also aimed to test the hypotheses, without the limitation noted from Study, 1 by including the frequency of engaging in painful behaviors in the model.
Methods
Participants
Participants were 249 current patients drawn from an outpatient and day hospital eating disorders treatment setting at Toronto General Hospital in Toronto, Canada6. All patients were assessed at intake, and all provided full, informed, and written consent for research participation. All patients in this study were diagnosed with current AN, with 106 (43%) specified with ANR and 143 specified with ANBP. The age of patients ranged from 16 to 68, with an average age of 26.30 (SD = 8.50). The sample was 98% female and consisted of almost entirely Caucasian individuals. The intake BMIs of patients ranged from 11.8 to 18.5 kg/m2, with an average BMI of 16.75 kg/m2 (SD = 1.33). Patients were not given full Axis I diagnostic interviews, given the eating disorder specialty of the treatment center, so information on diagnostic co-occurrence for this sample was not available.
Measures
Anorexia Diagnoses
All patients were assessed with a modified version of the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993) to diagnose AN as well as other eating disorders. Only patients with AN were included in this study, and all met criteria for AN according to DSM-IV-TR criteria (except for the amenorrhea criterion, which was waived). Diagnoses of AN were further specified according to specific subtypes, ANR and ANBP. The ANBP group consisted of individuals who purge only as well as those who binge and purge.
Provocative Behaviors
A latent variable similar to that in Study 1 was created using three indicators: vomiting frequency, laxative abuse, and NSSI. Information on vomiting frequency was assessed by asking each participant to indicate how many times he or she engaged in vomiting behavior each month. Information on general frequency of laxative abuse was obtained by having each participant rate his or her frequency of laxative abuse with a four-point Likert scale (1 = never, 4 = often). Frequency of NSSI was assessed by asking all patients how many times they had engaged in self-injury, without suicidal intent, in their lives.
Lifetime Suicide Attempts
All patients were asked how many times in their lives they had attempted suicide. Information on the severity of the attempt, the preparation for the attempt, or the amount of desire to die during the attempt was not collected in this study. The number of lifetime suicide attempts was used as the outcome variable in the structural model.
Substance Use
A Substance Use latent variable was created as a covariate in the structural model. All patients were asked to rate how frequently they used each of the following substances during their periods of most heavy use: barbiturates, amphetamines, cocaine, and hallucinogens. Each drug category was rated on a six-point Likert scale (0=never, 5=very frequently). Information on alcohol use was also collected. For use as an indicator in the Substance Use latent variable, the number of drinks per day during their heaviest period of alcohol use was included in order to represent problematic alcohol use.
Data Analytic Strategy
Structural equation modeling, using AMOS 6.0, was again employed in an attempt to replicate the results from Study 1. For the Study 2 model, a similar Provocative Behaviors latent variable was created using the following indicators: frequency of vomiting in the last month, general frequency of laxative abuse, and frequency of NSSI. Although this model did not provide an extensive list of painful/provocative behaviors as in Study 1, it nonetheless contained important behaviors that may contribute to acquired capability and, importantly, the frequency of those behaviors.
A latent variable of Substance Use was also created to use as a covariate in the Study 2 model. Although Study 1 tested a number of important covariates in the relation between AN and suicidal behavior, substance use was not included. Given the strong relation between substance abuse and suicidal behavior (Maser et al., 2002), substance abuse was another important covariate to rule out in the suicidal behavior of individuals with AN. The Substance Use latent variable was created using the following indicators: period of heaviest hallucinogen use, heaviest cocaine use, heaviest barbiturate use, heaviest amphetamine use, and number of drinks per day during heaviest period of drinking. A causal path was drawn between AN status and Substance Use because we hypothesized that an AN diagnosis, particularly ANBP, would likely influence substance use behavior. We also predicted Substance Use would contribute to Provocative Behaviors as these behaviors may result in habituation to pain as well (i.e., intravenous use).
In a similar manner as Study 1, AN individuals for Study 2 were coded with (1) if specified with ANR and (2) if specified with ANBP. We hypothesized that ANBP would have a positive relation with number of suicide attempts through the mechanism of the Provocative Behaviors latent variable. Thus, we expected to find a significant, positive indirect effect of the AN status variable on suicidal behavior. Furthermore, we had the a-priori hypothesis for Study 2 that ANR would have a relation with number of suicide attempts after controlling for pain behaviors because severe restricting is another way that one might develop the acquired capability for suicidal behavior. Thus, we expected to see the positive relation between AN status and increased suicidality change to a significant negative relation between the AN variable and suicide attempts when controlling for Provocative Behaviors. Age and sex were included as covariates in the model, and residual predictors were included on the latent variables to model error.
Establishing excellent model fit was not the goal of Study 2; instead the purpose was to replicate the two mechanisms for suicidal behavior in AN that were identified in Study 1. Thus, less stringent model fit criteria were used to evaluate model fit, with a CFI > .90 and an RMSEA < .10 indicating adequate fit. Mediational effects were again explored using the PRODCLIN program. Due to data missing at random for 22 people in the sample (9% of total sample), FIML was again used to estimate those missing data points for the model.
Results
Approximately 30% of this sample reported at least one lifetime suicide attempt. The average number of suicide attempts in this sample was .81 (SD = 1.63). No significant difference between the two groups was found regarding number of suicide attempts (F (1, 248) = 1.22, β = .07, p = .27). Both groups appeared to have similar statistics on suicide attempts, although the ANBP group (M = .91, SD = 1.66) trended toward more suicide attempts than the ANR group (M = .68, SD = 1.60).
The results of the Study 2 model are displayed in Figure 2. This model provided adequate fit to the data (χ2 = 87.12, df = 44, p<.001, CFI = .91, RMSEA = .06)7. All latent variable indicators significantly loaded onto their respective latent variables. The path from AN status to Provocative Behaviors was positive and significant (β = .82, p<.001), indicating an association between ANBP and Provocative Behaviors. The path from Provocative Behaviors to number of suicide attempts was also significant and positive (β = 2.1, p<.001), suggesting that the more patients engaged in purging, laxative abuse, and self-injury the more suicide attempts they were likely to have. Yet, also as predicted based on the results of Study 1, the direct path from AN type to suicide attempts was negative and significant (β = −1.70, p<.001), after controlling for Provocative Behaviors.
Figure 2.
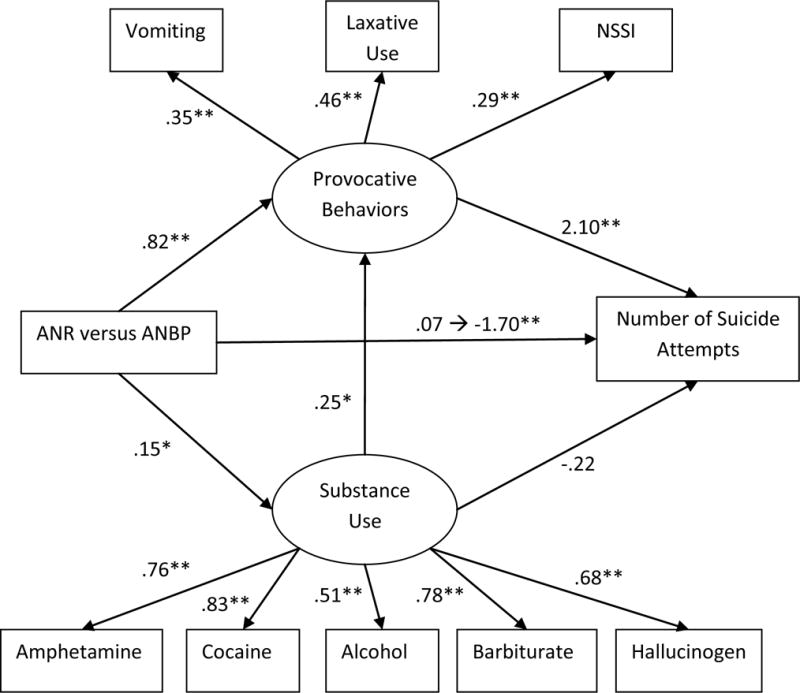
Study 2 Model. N = 249 (Anorexia – Restricting [ANR] = 106, Anorexia-Binge-Purging [ANBP] = 143). ANR is coded as 1, while ANBP is coded as 2; * = p<.05; ** = p<.01; ➔ indicates the path before and after including Provocative Behaviors in the model. Model includes sex and age as covariates, which are not displayed for clarified presentation. ANR = anorexia nervosa restricting; ANPB = anorexia nervosa binging and purging; NSSI = non-suicidal self-injury.
There was a positive indirect effect from AN type to number of suicide attempts (β = 1.77), as was hypothesized. This positive indirect effect indicated that the relation between ANBP and number of suicide attempts flowed through the Provocative Behaviors latent variable. The mediational effects of Provocative Behaviors on the relation between ANBP and suicide attempts was explored with PRODCLIN, described in more detail in Study 1. A confidence interval of 2.82 to 8.99 was obtained, and because the range did not include zero, a significant mediation effect was indicated.
Although not central to our aims, there was additional information of importance regarding the model. The significant positive path from AN status to Substance Abuse (β = .15, p<.001) indicated that the ANBP group tended to engage in more substance use than the ANR group. There was a significant positive relation between the Substance Use latent variable and the Provocative Behaviors latent variable (β = .25, p<.01), supporting the hypothesis that substance use also contributes to increasing acquired capability. The path from Substance Use to suicide attempts was not significant. Age and sex did not significantly predict either Provocative Behaviors or Substance Abuse, nor did they predict suicide attempts. The correlations of both age and sex with AN status were not significant.
General Discussion
Although various studies have documented the relation between AN and suicidal behavior, few studies have explored potential mechanisms in this relation. Inspired by the IPTS (Joiner, 2005), we tested the hypothesis that employment of behaviors that result in provocation and/or pain would mediate the relation between ANBP and extreme suicidal behavior. The results of both Study 1 and Study 2 support the mediational effects of painful/fear-inducing behaviors on the association between ANBP and extreme suicidal behavior.
The second major finding of these studies was that, only after accounting for paininducing behaviors, there appears to be a substantive association between ANR and extreme suicidal behavior. Individuals with ANBP tend to endorse more suicidal behaviors than their ANR counterparts, perhaps due to the painful and provocative behaviors they engage in. But, after accounting for these painful behaviors, ANR appears to have a stronger association with suicidal behaviors. In Study 1 we hypothesized that the relation between ANR and suicidal behavior emerges because the act of starving oneself is extremely painful, and restriction is the only other painful behavior diagnostically specific to ANR that remains after accounting for the other painful behaviors found in AN. Furthermore, those with ANR engage in a type of restriction that is different in severity from those with ANBP, which may independently increase acquired capability.
This hypothesis was supported in Study 1, as the magnitude of the path between ANR and Extreme Suicidal Behavior increased when the fasting item was removed from the Provocative Behaviors mediation latent variable, allowing for the variance accounted for by fasting to be allocated to the path between ANR and suicidal behavior. Although our interpretation of this finding in Study 1 was post-hoc, the a-priori hypothesis of this effect and replication of this finding in Study 2 suggest that severe and unrelenting restriction may be another important behavior that influences suicide risk in AN. It is also important to note that the suicidal behavior latent variable in Study 1 consisted of indicators concerning number of attempts, the use of a violent attempt method, lethality, intent to die, and premeditation for the most serious attempt. This suggests that many individuals with AN reported experience with extreme forms of suicidality, as opposed to a solitary, tentative attempt. Thus, the suicidal behaviors of many with AN are extremely dangerous, and not simply a “cry for help,” as some families or clinicians may mistakenly think. Importantly, both studies included key covariates such as depression, BPD diagnosis, and substance abuse, suggesting that these findings are unlikely a result of co-occurring psychopathology.
Two Routes to Suicidal Behavior in AN
Support was found for two independent routes to increased suicidal behavior in AN: one through provocative behaviors, such as vomiting and laxative abuse, the second route through unwavering restriction. The connection between both subtypes of AN, a diminished fear of death, and serious suicidality can be seen in a recent series of case studies on death by suicide and AN (Holm-Denoma et al., 2008). Among these cases, the authors identified individuals with ANR and ANBP who died by suicide and these individuals used particularly lethal methods that would have killed healthy individuals, rather than less lethal methods that might have only killed someone in a weakened state. Individuals with ANR jumped in front of trains (two cases), ingested a household cleaning product containing hydrochloric acid, severely overdosed, and died by hanging. On the other hand, individuals with ANBP died by jumping in front of a train, hanging, severe overdosing, and fire-induced carbon monoxide poisoning. The take away point from the Holm-Denoma et al. (2008) study, interpreted in context of the findings of this study, is that most of the individuals with both ANR and ANBP who died by suicide did so through violent methods with a high probability of death. The ability to enact lethal self-injury in these cases may have developed by overcoming a fear of death through familiarity with the pain of restricting and compensatory methods.
Strengths and Limitations
These studies have a number of important strengths that speak to the robustness and generalizability of our findings and conclusions. Importantly, we found the same pattern of results across two large, clinically-impaired, yet distinct, groups of individuals with AN – one treatment seeking and the other not. This includes the replication of the positive indirect effect between ANBP and suicidal behavior, through painful behaviors, as well as the replication of the association between ANR and suicidal behavior when including provocative behaviors as a mediator/covariate in the model. A second strength was that both studies used different indices of provocative behaviors and suicidality, yet the results remained essentially the same. Finally, both studies included rigorous covariates, all of which were important because stronger conclusions can be made for the specificity of the relation between AN and suicidal behaviors, with evidence that suicidality in AN was not an artifact of depression, BPD, or substance abuse.
Although this study makes important contributions to the literature on AN and suicidal behavior, there are a few limitations that should be considered when interpreting the findings. The most important limitation of this study was that both samples were cross-sectional, a problem that can lead to difficulty identifying the flow of a meditational model. Yet, given the preliminary stages of understanding suicidal behavior in AN, there is still much that can be learned from this study. Another important limitation is that this study was about suicide attempts, rather than death by suicide. Even though the findings of this study suggest that engaging in painful behaviors (both related and unrelated to eating disorders) is associated with increased severity of suicidal behavior, these findings may not necessarily generalize to AN individuals who eventually die by suicide. Yet, given the use of a latent variable of severity of suicidal behavior (more attempts, longer premeditation, greater intent, and greater lethality) in Study 1, it is a reasonable possibility that individuals expressing extreme suicidal behavior at the time of this study may have higher risk for death by suicide in the future.
Another limitation is that the ANR group and ANBP group in Study 2 did not significantly differ on number of suicide attempts (though the means were in the expected direction). Although inconsistent with our results from Study 1, other studies have also found similar rates of suicidal behavior between ANR and ANBP individuals (e.g., Eddy, Keel, Dorer, Delinsky, Franko, et al., 2001). In general suicidality appears to be higher in individuals with ANBP, but it is clearly high in both ANBP and ANR; and thus, it is not surprising that occasionally the groups are found not to differ on this behavior. Furthermore, because the sample used in Study 2 was a treatment seeking sample, patients may have had more severe impairment, including suicidal behaviors, and thus the ANR group in Study 2 may have had more severe suicidality than the population based subsample in Study 1. Final limitations include the crosssectional design, and both samples consisted of primarily female, Caucasian participants. Although this is an important group to study with regard to eating disorders and suicidal behavior, the findings may not generalize to other ethnic groups or males with these disorders.
It is also important to note that there may be alternative factors influencing the link between AN and suicidal behavior, making the mechanisms proposed in this study somewhat speculative. For example, the link between unrelenting restriction and suicidality may be influenced through impaired serotonin function, which is known to increase depression and suicidality (e.g., Owens & Nemeroff, 1994). If this were the case, we would expect to find more impairment in serotonin function in people with ANR versus ANBP. Though some differences in serotonin function have been found in recovered ANR versus ANBP individuals, it is unclear if these differences exist during the active phase of the illness (Kaye, 2008). Moreover, Favaro and colleagues (2004) found similarly low levels of cholesterol in both ANR and ANBP patients as compared to controls. It is believed that low cholesterol levels may decrease the activity of serotonin receptors and the serotonin transporter (Engelberg, 1992). Thus, these findings imply that differences in suicidality between ANR and ANBP are unlikely due solely to impaired serotonin functioning.
Yet, other alternative mechanisms may account for the relation between AN and suicide. For example, intense psychological pain, termed psychache by Schneidman (1996), could be more prevalent in individuals with AN, and psychache could then be further aggravated by painful and provocative behaviors such that the pain of living is worse than that of dying. The IPTS theory of suicide would suggest that this psychache is a result of feelings of burdensomeness and belongingness, however, and that acquired capability is still needed to actually make a serious suicide attempt. More research on psychache and burdensomeness/belongingness is needed to address this alternative explanation. Similarly, research on behaviors such as NSSI and purging suggests they may be used to cope with negative affect due to physical distractions such as pain (Selby, Anestis, & Joiner, 2008), yet many patients who engage in seemingly painful behaviors report an analgesic state during these behaviors, suggesting that these behaviors might not actually instill pain (Lieb et al., 2004). This could be evidence against the development of acquired capability through these behaviors. Yet, along the lines of the IPTS framework, not feeling pain during these behaviors could be the result of opponent-processes where, through repetition, habituation to pain occurs and feelings of relief from emotional distress take its place. Essentially, the analgesia reported during these behaviors could be evidence of habituation and increased acquired capability. More research is needed to fully address this point, however. Future research on the relation between AN and suicide may benefit from more strict assessment of feelings of fearlessness about pain and death, perhaps with the use of the Acquired Capability for Suicide Scale (ACSS; see Van Orden et al., 2008). Replication of the findings from the current studies with a more precise measurement of acquired capability may provide more support for the speculative theoretical underpinnings of the current study. Future studies should also attempt to test all three components of the IPTS in AN to determine if all components of this theory are relevant to those with AN, and future studies should examine if the behaviors examined in this study actually contribute to the development of acquired capability.
Conclusion
The results of this study provide two potential routes to increased suicidal behavior in AN. The first route, applying primarily to individuals with ANBP, may be through the use of painful compensatory behaviors as well as other self-damaging behaviors, such as NSSI. The second route, which may be somewhat more relevant to the ANR group (but relevant to some degree for both groups), may be through the constant pain associated with obstinate dietary restriction. Future research should continue to explore the proposed mechanisms as well as identify other mechanisms that may increase suicide risk in AN. AN is undoubtedly a painful disorder to live with—so painful, in fact, that for these afflicted individuals the pain involved with death may no longer serve to deter suicidal desire.
Table 1.
Study 1 Means and Standard Deviations for, and Intercorrelations Between, All Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. AN Status | – | |||||||||||
| 2. EDPB | .62** | – | ||||||||||
| 3. NonEDPB | .23** | .34** | – | |||||||||
| 4. Suicide Attempts | .20** | .27** | .35** | – | ||||||||
| 5. Lethality | .21** | .27** | .38** | .64** | – | |||||||
| 6. Intent | .22** | .28** | .39** | .64** | .96** | – | ||||||
| 7. Premeditation | .22** | .28** | .34** | .63** | .88** | .88** | – | |||||
| 8. Violent Attempt | .09** | .07* | .09* | .36** | .30** | .34** | 33** | – | ||||
| 9. Depression | .18** | .23** | .27** | .19** | .25** | .25** | .24** | .08* | – | |||
| 10. BPD Diagnosis | .10** | .15** | .32** | .18** | .17** | .18** | .19** | .03 | .15** | – | ||
| 11. Sex | .14** | .09* | .08* | .05 | .05 | .06 | .06 | .03 | .04 | .05 | – | |
| 12. Age | .08* | .001 | −.03 | −.02 | .02 | .02 | .02 | −.04 | −.02 | −.03 | −.02 | – |
|
| ||||||||||||
| MEAN | 45.4% | 1.93 | 1.13 | .40 | .60 | .37 | .30 | 2.8% | 69% | 6% | 96% | 29.71 |
| SD | – | 1.70 | 1.50 | 1.26 | 1.41 | .87 | .74 | – | – | – | – | 11.24 |
| Range | – | 0–8 | 0–8 | 0–15 | 0–6 | 0–3 | 0–3 | – | – | – | – | 16–76 |
Note. N = 787,
= p<.05,
= p<.001. AN Status = Anorexia Nervosa (Restricting = 1, Binging/Purging = 2); AN Mean = % with ANR; EDPB = Eating Disordered Painful Behaviors; NonEDPB = Non-Eating Disordered Painful Behaviors; Violent Attempt Mean = % with a violent attempt; Lifetime depression Mean= % with depression; BPD Diagnosis= Borderline Personality Disorder, Mean = % with BPD; Sex Mean = % female.
Table 2.
Study 2 Means and Standard Deviations for, and Intercorrelations Between, All Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. AN Status | – | |||||||||||
| 2. Vomiting | .65** | – | ||||||||||
| 3. Laxative Use | .32** | .16** | – | |||||||||
| 4. NSSI | .12 | .07 | .04 | – | ||||||||
| 5. Suicide Attempts | .07 | .18* | .13 | .40** | – | |||||||
| 6. Hallucinogen Use | .21** | .19* | .20** | .08 | .29** | – | ||||||
| 7. Cocaine Use | .09 | .07 | .13 | .13 | .22** | .52** | – | |||||
| 8. Barbiturate Use | .05 | .18* | .18* | .13 | .36** | .57** | .64** | – | ||||
| 9. Alcohol Use | .28** | .20* | .19* | .08 | .20** | .42** | .50** | .43** | – | |||
| 10. Amphetam. Use | .12 | .08 | .17* | .05 | .22** | .48** | .68** | .56** | .34** | – | ||
| 11. Sex | −.01 | −.05 | −.004 | −.03 | −.05 | −.03 | −.02 | −.02 | .03 | −.03 | – | |
| 12. Age | −.06 | −.10 | .08 | −.01 | −.03 | −.07 | .001 | .001 | −.05 | −.07 | −.07 | – |
|
| ||||||||||||
| MEAN | 43%ˆ | 29.60 | 1.53 | 6.46 | .81 | 1.19 | 1.18 | 1.07 | 3.51 | 1.28 | 98%+ | 26.32 |
| SD | – | 46.90 | .98 | 20.95 | 1.63 | .67 | .77 | .44 | 3.48 | .96 | – | 8.53 |
| Range | – | 0–200 | 1–4 | 0–99 | 0–10 | 0–5 | 0–5 | 0–5 | 0–20 | 0–5 | – | 16–68 |
Note: N=249.
=p<.05;
=p<.01;
= percent of sample diagnosed with ANR;
= percent of sample that is female; AN Status = anorexia nervosa restricting subtype coded as 1 and anorexia nervosa binge-purging subtype coded as 2; NSSI = non-suicidal self-injury; Amphetam. Use = Amphetamine Use.
Acknowledgments
This study was funded, in part, by National Institute of Mental Health grant F31MH081396 to E. A. Selby (under the sponsorship of T.E. Joiner) and by an NIMH grant F31MH083382 to A. R. Smith (under the sponsorship of T. E. Joiner), as well as the following National Institutes of Health Grants (MH066122, MH066117, MH066145, MH066296, MH066147, MH066289, MH066193, MH066287, MH066288, MH066146). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health. The authors thank the study managers and clinical interviewers of the Genetics of Anorexia Nervosa Collaboration for their efforts in participant screening and clinical assessments. Genotyping services for the Genetics of Anorexia Nervosa Collaboration were provided by the Center for Inherited Disease Research (CIDR). CIDR is fully funded through a federal contract from the National Institutes of Health to The Johns Hopkins University, Contract Number HHSN268200782096C. Michael Strober receives support from the Franklin Mint Chair in Eating Disorders. The authors are indebted to the participating families for their contribution of time and effort in support of this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
These standardized BMI values correspond to the 5th percentile BMI values of the National Health and Nutrition Examination Survey epidemiological sample of females and males, for the average age range (27–29 years) of participants from previous studies (Hebebrand et al., 1996).
Because using eating-disordered provocative behaviors as a mediator results in overlap with the ANBP subtype, which is defined by these behaviors, the overall model was evaluated without a provocative behaviors latent variable and the non-eating disordered provocative behaviors variable alone was used as a mediator. This model resulted in essentially the same fit, path directions and magnitudes as the model presented in the results. This finding indicates that the overlap of the eating disorder provocative behaviors and ANBP does not account for the significant findings of the model.
The same analyses presented in the results section were analyzed comparing the ANR group to those formally diagnosed ANBP instead of the combined ANBP group, and the results were essentially the same as the analyses presented, which combine the ANP, ANBP, and ANBN groups into one group (ANBP).
Because these data were intended to study the genetics of AN, all participants were related to one or more other participants in the study. This resulted in a potential problem with non-independence of observations. In order to ensure that this issue of non-independence was not influencing the results of this study, all analyses were run a second time using a modified dataset that included only one, randomly-selected member from each family. This ensured that all participants in this second dataset were independent from each other. The model fit and results remained essentially the same (N = 382; χ2 = 145.32, df = 38, p<.001, CFI = .96, TLI = .91, RMSEA = .086); there were no changes in significant findings for either regression paths or factor loadings, indicating that the pattern of findings is unlikely to be influenced by data non-independence.
It is possible that the indicators for the painful and provocative behaviors latent variable served primarily as markers of disorder severity of AN, rather than as indicators of level of acquired capability. If this were true, then severity of disorder may play a larger role in suicidal behavior than our hypothesis of acquired capability. In order to test this potential alternative, we evaluated the exact same model tested in Study 1 with the exception that the mediator latent variable had different indicators. Instead of indicators of painful and provocative behaviors, we used lowest lifetime BMI as one indicator, and highest lifetime BMI as second indicator. Research has found these indices to be reliable markers of illness severity; specifically, the lower an individual’s BMI the less likely that individual is to recover from anorexia and the greater the probability of death due to the condition (Hebebrand et al., 1997; Howard et al., 1999). Similarly, those with more severe conditions are also likely to have a lower overall highest lifetime BMI, potentially indicating longer experience with the condition and less likelihood of full recovery. This alternative model fit the data well (χ2 = 4475.53, df = 56, CFI = .98, RMSEA = .046) and both indicators significantly loaded onto the latent mediator variable. Importantly, however, this severity latent variable did not have a significant path to the extreme suicidal behavior latent variable (β=.02, p=.72), and the direct path from AN status to suicidal behavior remained significant with a positive magnitude. The failure of the severity variable to mediate the relationship between AN status and suicidal behavior suggests that the findings of Study 1 are not due to overall severity of AN. A similar alternative analysis was conducted for Study 2, with similar, consistent results.
There was some concern about patient overlap between the samples of Study 1 and Study 2, as both involve AN individuals from the Toronto area. Unfortunately records linking participants’ identification to the sample for Study 2 were destroyed at the end of the study, making identification impossible. In order to control for any participants potentially included in both samples, the analyses from Study 1 were reanalyzed without any of the participants (N=82) from the Toronto site included. The results were essentially unchanged, and the model maintained similar fit statistics (χ2 = 207.31, df = 38, p<.001, CFI = .96, TLI = .94, RMSEA = .079). Thus, even if there is some overlap between the two samples, the results remain consistent even without those participants included.
When this model was analyzed a negative error variance was obtained for the residual indicator for suicide attempts. This was likely a function of the residual being near zero, a problem which is minor enough that AMOS was still able to conduct the analysis. The recommended way to remedy a negative error variance is to remove the residual indicator and reanalyze the model (Dillon, Kumar, & Mulani, 1987). After running a second analysis where the residual predictor for suicide attempts was removed, the model was empirically identified (i.e. there were no negative error variances) and model fit was the same. Following this second analysis, the empirical identification of the model remains intact and the fit indices generated by the model remain valid.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. fourth. Washington, D.C.: Author; 1994. [Google Scholar]
- Anderson TW. Maximum likelihood estimates for a multivariate normal distributions when some observations are missing. Journal of American Statistical Association. 1957;52:200–203. [Google Scholar]
- Baker EH, Sandle GI. Complications of laxative abuse. Annual Review of Medicine. 1996;47:127–134. doi: 10.1146/annurev.med.47.1.127. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Scale for Suicide Ideation. San Antonio: The Psychological Corporation; 1993. [Google Scholar]
- Beck AT, Steer RA, Ranieri WF. Scale for Suicide Ideation: Psychometric properties of a self-report version. Journal of Clinical Psychology. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Black C, Wilson GT, Labouvie E, Heffernan K. Selective processing of eating disorder relevant stimuli: Does the Stroop Test provide an objective measure of bulimia nervosa? International Journal of Eating Disorders. 1997;22:329–333. doi: 10.1002/(sici)1098-108x(199711)22:3<329::aid-eat13>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Total, direct, and indirect effects in structural equation models. Sociological Methodology. 1987;17:37–69. [Google Scholar]
- Braun DL. More males seek treatment for eating disorders. International Journal of Eating Disorders. 1999;25:415–424. doi: 10.1002/(sici)1098-108x(199905)25:4<415::aid-eat6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Thornton L, Pinheiro AP, Plotnicov K, KIump KL, Brandt H, et al. Suicide attempts in anorexia nervosa. Psychosomatic Medicine. 2008;70:378–383. doi: 10.1097/PSY.0b013e3181646765. [DOI] [PubMed] [Google Scholar]
- Carlat DJ, Carmargo CA, Herzog DB. Eating disorders in males: A report of 135 patients. American Journal of Psychiatry. 1997;15:1127–1132. doi: 10.1176/ajp.154.8.1127. [DOI] [PubMed] [Google Scholar]
- Claes L, Vandereycken W, Vertommen H. Pain experience related to self-injury in eating disorder patients. Eating Behaviors. 2006;7:204–213. doi: 10.1016/j.eatbeh.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. 12th. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Crisp AH, Callender JS, Halek C, Hus LK. Long-term mortality in anorexia nervosa. A 20-year follow-up of the St George’s and Aberdeen cohorts. The British Journal of Psychiatry. 1992;161:104–107. doi: 10.1192/bjp.161.1.104. [DOI] [PubMed] [Google Scholar]
- De la Rie SM, Noordenbos G, Donker M, van Furth EF. The patient’s view on quality of life and eating disorders. International Journal of Eating Disorders. 2007;40:13–20. doi: 10.1002/eat.20338. [DOI] [PubMed] [Google Scholar]
- De la Rie SM, van Furth EF, De Koning A, Noordenbos G, Donker MC. The quality of life of family caregivers of eating disorder patients. Eating Disorders. 2005;13:345–351. doi: 10.1080/10640260591005236. [DOI] [PubMed] [Google Scholar]
- Dillon WR, Kumar A, Mulani N. Offending estimates in covariance structure analysis: Comments on the causes of and solutions to Heywood cases. Psychological Bulletin. 1987;101(1):126–135. [Google Scholar]
- Dobson KS, Dozois DJ. Attentional biases in eating disorders: A meta-analytic review of Stroop performance. Clinical Psychology Review. 1995;23:1001–1022. doi: 10.1016/j.cpr.2003.09.004. [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Conwell Y. Personality disorders and completed suicide: A methodological and conceptual review. Clinical Psychology: Science and Practice. 1997;4:359–376. [Google Scholar]
- Engelberg H. Low serum cholesterol and suicide. Lancet. 1992;339:727–9. doi: 10.1016/0140-6736(92)90609-7. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Keel PK, Dorer DJ, Delinsky SS, Franko DL, Herzog DB. Longitudinal Comparison of Anorexia Nervosa Subtypes. International Journal of Eating Disorders. 2001;31:191–201. doi: 10.1002/eat.10016. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Favaro A, Caregaro L, Di Pascoli L, Brambilla F, Santonastaso P. Total Serum Cholesterol and Suicidality in Anorexia Nervosa. Psychosomatic Medicine. 2004;66:549–522. doi: 10.1097/01.psy.0000127873.31062.80. [DOI] [PubMed] [Google Scholar]
- Favaro A, Santonastaso P. Suicidality in eating disorders: Clinical and psychological correlates. Acta Psychiatrica Scandinavica. 1997;95:508–514. doi: 10.1111/j.1600-0447.1997.tb10139.x. [DOI] [PubMed] [Google Scholar]
- Fedorowicz VJ, Falissard B, Foulon C, Dardennes R, Snezana DM, Guelfi JD, et al. Factors associated with suicidal behaviors in a large French sample of inpatients with eating disorders. International Journal of Eating Disorders. 2007;40:589–595. doi: 10.1002/eat.20415. [DOI] [PubMed] [Google Scholar]
- Fichter M, Herpetz S, Quadflieg N, Herpetz-Dahlmann B. Structured interview for anorexic and bulimic disorders for DSM-IV and ICD-10: Updated (third) revision. International Journal of Eating Disorders. 1998;24:227–49. doi: 10.1002/(sici)1098-108x(199811)24:3<227::aid-eat1>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) Biometrics Research Department, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) Washington, DC: American Psychiatric Publishing; 1997. [Google Scholar]
- Foulon C, Guelfi JD, Kimpan A, Ades J, Romo L, Houdeyer K, et al. Switching to the bingeing/purging subtype of anorexia nervosa is frequently associated with suicidal attempts. European Psychiatry. 2007;22:513–519. doi: 10.1016/j.eurpsy.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Franko DL, Keel PK. Suicidality in eating disorders: Occurrence, correlates, and clinical implications. Clinical Psychology Review. 2006;26:769–782. doi: 10.1016/j.cpr.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Friedman J, et al. Diagnostic Interview for Genetic Studies: Rationale, unique features, and training. Archives of General Psychiatry. 1994;51:849–59. doi: 10.1001/archpsyc.1994.03950110009002. [DOI] [PubMed] [Google Scholar]
- Gendall K, Joyce P, Carter F, McIntosh V, Jordan J, Bulik C. The psychobiology and diagnostic significance of amenorrhea in patients with anorexia nervosa. Fertility and Sterility. 2006;85:1531–1535. doi: 10.1016/j.fertnstert.2005.10.048. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders: A meta-analysis. The British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hebebrand J, Mimmelmann GW, Herzog W, Herpertz-Dahlmann BM, Steinhausen HC, Amstein M, Seidel R, et al. Prediction of low body weight at long-term followup in acute anorexia nervosa by low body weight at referral. American Journal of Psychiatry. 1997;154:566–569. doi: 10.1176/ajp.154.4.566. [DOI] [PubMed] [Google Scholar]
- Hebebrand J, Himmelmann GW, Heseker H, Schafer H, Remschmidt H. Use of percentiles for the body mass index in anorexia nervosa: Diagnostic, epidemiological, and therapeutic considerations. International Journal of Eating Disorders. 1996;19:359–369. doi: 10.1002/(SICI)1098-108X(199605)19:4<359::AID-EAT4>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Hellstrom I. Oral complications in anorexia nervosa. European Journal of Oral Sciences. 2007;85:71–86. doi: 10.1111/j.1600-0722.1977.tb00535.x. [DOI] [PubMed] [Google Scholar]
- Hillege S, Beale B, McMaster R. Impact of eating disorders on family life: Individual parents’ stories. Journal of Clinical Nursing. 2005;15:1016–1022. doi: 10.1111/j.1365-2702.2006.01367.x. [DOI] [PubMed] [Google Scholar]
- Holm-Denoma JM, Witte TK, Gordon KH, Herzog DB, Franko DL, et al. Deaths by suicide among individuals with anorexia as arbiters between competing explanations of the anorexia–suicide link. Journal of Affective Disorders. 2008;107:231–236. doi: 10.1016/j.jad.2007.07.029. [DOI] [PubMed] [Google Scholar]
- Howard WT, Evans KK, Quintero-Howard CV, Bowers WA, Andersen AE. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. American Journal of Psychiatry. 1999;156:1697–1702. doi: 10.1176/ajp.156.11.1697. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Joiner TE, Jr, Van Orden KA, Witte TK, Rudd MD. The Interpersonal Theory of Suicide: Guidance for Working with Suicidal Clients. Washington, D.C: American Psychological Association; in press. [Google Scholar]
- Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiology and Behavior. 2008;94:121–135. doi: 10.1016/j.physbeh.2007.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye WH, Plotnicov K, Thornton L, Devlin B, Fichter M, Treasure J, et al. The Genetics of Anorexia Nervosa (GAN) Collaborative Study: Methods and sample description. International Journal of Eating Disorders. 2008;41:289–300. doi: 10.1002/eat.20509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DA, et al. Predictors of mortality in eating disorders. Archives of General Psychiatry. 2003;60:179–183. doi: 10.1001/archpsyc.60.2.179. [DOI] [PubMed] [Google Scholar]
- Klump KL, Strober M, Bulik CM, Thornton L, Johnson C, Devlin B, Fichter MM, Halmi KA, Kaplan AS, Woodside DB, Crow S, Mitchell J, Rotondo A, Keel PK, Berrettini WH, Plotnicov K, Pollice C, Lilenfeld LR, Kaye WH. Personality characteristics of women before and after recovery from an eating disorder. Psychological Medicine. 2004;34:1407–1418. doi: 10.1017/s0033291704002442. [DOI] [PubMed] [Google Scholar]
- Lautenbacher S, Barth K, Friess E, Strian F, Pirke KM, Krieg JC. Dieting and pain sensitivity: A validation of clinical findings. Physiology & Behavior. 1991;50:629–631. doi: 10.1016/0031-9384(91)90557-5. [DOI] [PubMed] [Google Scholar]
- Lieb K, Zanarini MC, Schmahl C, Linehan M, Bohus M. Borderline personality disorder. Lancet. 2004;364:453–461. doi: 10.1016/S0140-6736(04)16770-6. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- Luce KH, Crowther JH. The reliability of the Eating Disorder Examination–Self-Report Questionnaire Version (EDE-Q) International Journal of Eating Disorders. 25:349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39(3):384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maser JD, Akiskal HS, Schettler P, Scheftner W, Mueller T, Endicott J, Solomon D, Clayton P. Can temperament identify affectively ill patients who engage in lethal or near-lethal suicidal behavior? A 14-year prospective study. Suicide & Life-Threatening Behavior. 2002;32:10–32. doi: 10.1521/suli.32.1.10.22183. [DOI] [PubMed] [Google Scholar]
- McIntosh JL. USA Suicide Statistics for the Year 1999: Overheads and a Presentation Guide. Washington, D.C.: American Association of Suicidology; 2002. [Google Scholar]
- Nock MK, Banaji MR. Assessment of self-injurious thoughts using a behavioral test. American Journal of Psychiatry. 2007;164:820–823. doi: 10.1176/ajp.2007.164.5.820. [DOI] [PubMed] [Google Scholar]
- Norring CE, Sohlberg SS. Outcome, recovery, relapse and mortality across six years in patients with clinical eating disorders. Acta Psychiatrica Scandinavica. 1993;87:437–444. doi: 10.1111/j.1600-0447.1993.tb03401.x. [DOI] [PubMed] [Google Scholar]
- Nurnberger JI, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Karakavy-Owens MJ, Nemeroff CB. Role of serotonininthe pathophysiology of depression: Focus on the serotonin transporter. Clinical Chemestriy. 1994;40:288–295. [PubMed] [Google Scholar]
- Papadopoulos FC, Ekbom A, Brandt L, Ekselius L. Excess mortality, causes of death and prognostic factors in anorexia nervosa. British Journal of Psychiatry. 2009;194(1):7–10. doi: 10.1192/bjp.bp.108.054742. [DOI] [PubMed] [Google Scholar]
- Papežova H, Yamamotova A, Uher R. Elevated pain threshold in eating disorders: Physiological and psychological factors. Journal of Psychiatric Research. 2005;39:431–438. doi: 10.1016/j.jpsychires.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Pinheiro A, Thornton L, Plotnicov K, Tozzi T, Klump K, Berrettini W, et al. Patterns of menstrual disturbance in eating disorders. International Journal of Eating Disorders. 2007;40(5):424–434. doi: 10.1002/eat.20388. [DOI] [PubMed] [Google Scholar]
- Pompili M, Girardi P, Tatarelli G, Ruberto A, Tatarelli R. Suicide and attempted suicide in eating disorders, obesity and weight–image concern. Eating Behaviors. 2006;7:384–394. doi: 10.1016/j.eatbeh.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Pompili M, Mancinelli I, Girardi P, Ruberto A, Tatarelli R. Suicide in Anorexia Nervosa: A Meta-Analysis. International Journal of Eating Disorders. 2004;36:99–103. doi: 10.1002/eat.20011. [DOI] [PubMed] [Google Scholar]
- Preisig M, Fenton BT, Matthey ML, Berney A, Ferrero F. Diagnostic Interview for Genetic Studies (DIGS): Inter-rater and test-retest reliability of the French version. European Archives of Psychiatry and Clinical Neuroscience. 1999;249:174–179. doi: 10.1007/s004060050084. [DOI] [PubMed] [Google Scholar]
- Project EHE. Eatatelife Phenotype Interview, Version. 2001;2:1. [Google Scholar]
- Raymond NC, de Zwaan M, Faris PL, Nugent SM, Ackard DM, Crosby RD, et al. Pain thresholds in obese binge-eating disorder subjects. Biological Psychiatry. 1995;37:202–204. doi: 10.1016/0006-3223(94)00244-w. [DOI] [PubMed] [Google Scholar]
- Roca M, Martin-Santos R, Raiz J, Obiols J, Serrano MJ, Torrens M, Subira S, Gili M, Navines R, Ibanez A, Nadal M, Barrantes N, Canellas F. Diagnostic Interview for Genetic Studies (DIGS): Inter-rater and test-retest reliability and validity in a Spanish population. European Psychiatry. 2007;22:44–48. doi: 10.1016/j.eurpsy.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Bender TW, Ribeiro JD, Nock MK, Rudd MD, Bryan C, et al. Overcoming the fear of lethal injury: Evaluating suicidal behavior in the military through the lens of the Interpersonal-Psychological Theory of Suicide. Clinical Psychology Review. doi: 10.1016/j.cpr.2009.12.004. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Anestis MD, Joiner TE., Jr Understanding the relationship between emotional and behavioral dysregulation: Emotional Cascades. Behaviour Research and Therapy. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Sidiropoulos M. Anorexia Nervosa: The physiological consequences of starvation and the need for primary prevention efforts. McGill Journal of Medicine. 2007;10:20–25. [PMC free article] [PubMed] [Google Scholar]
- Simon J, Schmidt U, Pilling S. The health service use and cost of eating disorders. Psychological Medicine. 2005;35:1543–1551. doi: 10.1017/S0033291705004708. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. The suicidal mind. Oxford: Oxford University Press; 1996. [Google Scholar]
- Smith AR, Witte TK, Teale NE, King SL, Bender TW, Joiner TE. Revisiting impulsivity in suicide: Implications for civil liability of third parties. Behavioral Sciences and the Law. 2008;26(6):779–797. doi: 10.1002/bsl.848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PF. Course and outcome of anorexia nervosa and bulimia nervosa. In: Fairburn CG, Brownell KD, editors. Eating disorders and obesity: A comprehensive handbook. 2nd. New York: The Guilford Press; 2002. pp. 226–232. [Google Scholar]
- Tiller JM, Gaynor S, Schmidt U, Troop N, Power M, et al. Social support in patients with anorexia nervosa and bulimia nervosa. International Journal of Eating Disorders. 1997;21:31–38. doi: 10.1002/(sici)1098-108x(199701)21:1<31::aid-eat4>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Tozzi F, Thornton LM, Mitchell J, Fichter MM, Klump KL, Lilenfeld LR, Reba L, Strober M, Kaye WH, Bulik CM, The Price Foundation Collaborative Group Features associated with laxative abuse in individuals with eating disorders. Psychosomatic Medicine. 2006;68:470–477. doi: 10.1097/01.psy.0000221359.35034.e7. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, Joiner TE., Jr The interpersonal theory of suicide. Psychological Review. doi: 10.1037/a0018697. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE., Jr Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- Witte TK, Merrill KA, Stellrect NE, Bernert RA, Hollar DL, Schatschneider C, Joiner TE., Jr “Impulsive” youth suicide attempters are not necessarily all that impulsive. Journal of Affective Disorders. 2008;107:107–116. doi: 10.1016/j.jad.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Connolly KM, Stice E. Impulsivity as a risk factor for eating disorder behavior: Assessment implications with adolescents. International Journal of Eating Disorders. 2004;36:172–182. doi: 10.1002/eat.20033. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Swift WJ, Slomik HB, Goodman S. DSM-III-R personality disorders in eating disorder subtypes. International Journal of Eating Disorders. 1990;9:607–616. [Google Scholar]


