Abstract
Introduction
Outcome after traumatic injury has typically been limited to determination at time of discharge or brief follow-up. This study investigates the natural history of long-term survival after trauma.
Methods
All highest level activation patients prospectively enrolled in an on-going cohort study from 2005–2012 were selected. To allow for long-term follow-up, patients had to be enrolled at least 1 year prior to the latest available data from the National Death Index (NDI 2013). Time and cause of mortality was determined based upon death certificates. Survival status was determined by the latest date of either care in our institution or NDI query. Kaplan-Meier curves were created stratified for injury severity (ISS). Survival was compared with estimated actuarial survival based on age, gender, and race.
Results
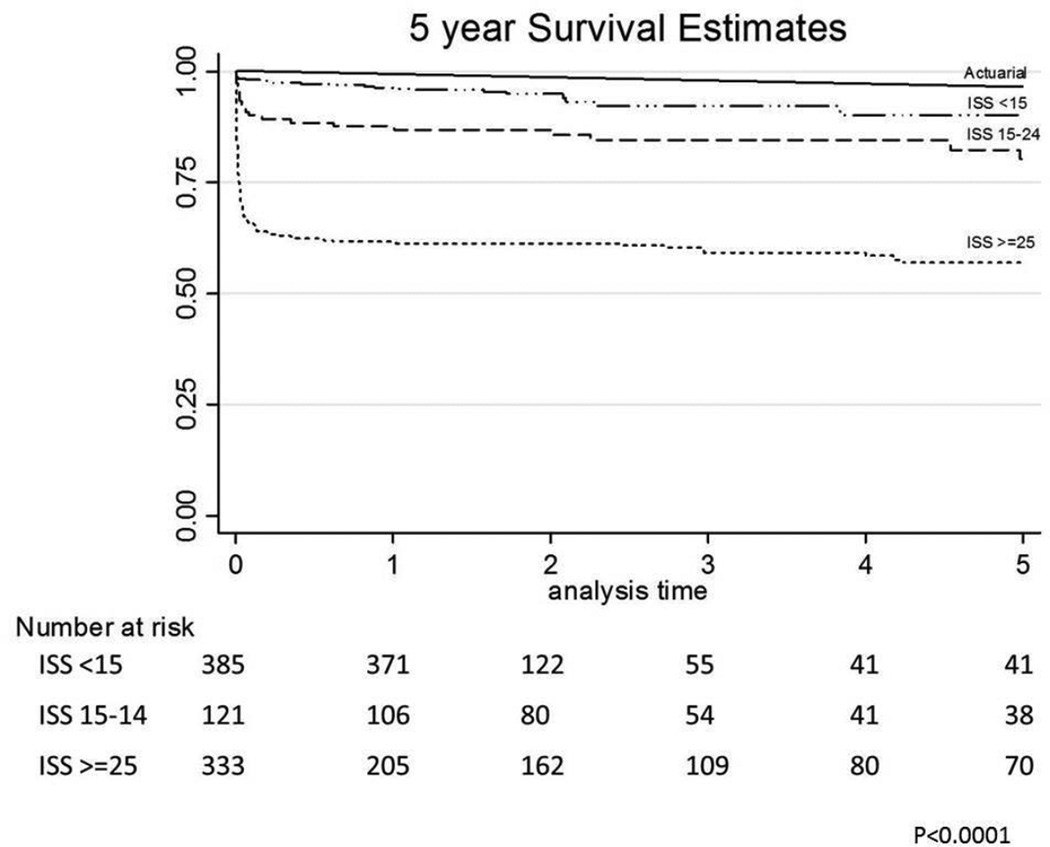
908 highest level activation patients (median ISS 18) were followed for a median 1.7 years (IQR 1.0 – 2.9; maximum 9.8 years). Survival data was available on 99.8%. Overall survival was 73% (663/908). For those with at least 2 year follow-up, survival was only 62% (317/509). Severity of injury predicted long-term survival (p<.0001) with those having ISS>=25 with the poorest outcome (57% survival at 5 years). For all ISS groups, survival was worse than predicted actuarial survival [p<0.001]. Excluding early deaths (<=30 days), observed survival was still significantly lower than estimated actuarial survival [p<0.002]. 18% (44/245 deaths) of all deaths occurred after 30 days. Amongst late deaths, 53% occurred between 31 days to 1 year post trauma. Trauma related mortality was the leading cause of post-discharge death accounting for 43% of the late deaths.
Conclusion
Post-discharge deaths represent a significant percentage of total trauma related mortality. Despite having ‘survived’ to leave the hospital, long term survival was worse than predicted actuarial survival suggesting that the mortality from injury does not end at ‘successful’ hospital discharge.
Keywords: trauma-related mortality, long-term death, post-discharge outcome, trauma
Introduction
According to the 2010 World Health Organization Global Burden of Disease study, injury accounts for over 5 million deaths per year and represents 1 out of every 10 deaths worldwide(1). It is estimated that injury will rise to the 5th leading cause of death by 2030(1). Trauma related morbidity, as measured by Disability Adjusted Life Years (DALYs), ranks second behind only ischemic heart disease when examining the most common causes of disability in the US(2). Additionally, the cost of care for traumatic injury is staggering, with an estimate in excess of $27 Billion per year in the US(3). A large proportion of the cost of trauma is utilized to provide care for those left with significant trauma related disability. Unfortunately, little current data exists regarding the net impact of post-discharge disability on long-term mortality.
Further, our current mortality metrics reported for trauma centers focus on either in-hospital mortality, 28-day, or 30-day mortality. In addition, the currently available mortality prediction algorithms are based upon data from the 1980s and early 1990s that pre-date many modern advances in trauma care(4). Benchmarking performance is a necessity to push hospital systems to continue to improve quality; however, the target for trauma patients has largely focused on short-term results and post-discharge outcomes are rarely reported in trauma outcomes studies. This study is the first to investigate the natural history of long-term survival following traumatic injury. We hypothesized that post-discharge deaths following incident hospitalization account for a significant uncaptured burden of disease.
Methods
Inclusion criteria
Comprehensive demographic, injury, clinical, and outcomes data were prospectively collected on highest-level trauma activation patients at an urban Level 1 trauma center between 2005 and 2013 as part of an on-going cohort study. To allow for long-term follow-up data to be obtainable, we selected all patients that had been enrolled at least 1 year prior to the latest available data from the National Death Index (NDI) as our study group. The most current NDI data available is through December 2013, therefore, all study patients from January 2005 to December 2012 were submitted for determination of death status. This study was approved by the University of California, San Francisco institutional review board.
Death Status
Institutional records were reviewed to verify status at hospital discharge and the most recent date of care at our institution. For all patients who were alive at the time of discharge from our institution, data was submitted for out of hospital vital status determination as alive or dead. Name, last name, middle name (if available), month of birth, day of birth, year of birth, and sex were provided to the National Death Index (NDI) for query. Race was collected but not submitted as our institution utilized differing race categories than the NDI file structure.
Date of death, state of death, cause of death, and contributing factors to death were provided by the NDI as perfect matches based on submitted patient data elements, high probability matches, or possible matches. Exact perfect matches on all submitted data elements were coded as deaths. High probability and possible matches were reviewed by investigators to determine if these patients were likely dead based on the NDI analysis. NDI records with the date of death preceding the date of the incident trauma hospitalization were excluded. Next, for those patients with a social security number, if there was a probable or possible match based on social security number and other major elements correlated, they were coded as deaths. Major elements were considered last name, first initial, date of birth within 1 year of date provided, and death date followed date of discharge from our institution. If patients did not have a social security number and there were matches for the other major elements, they were classified as dead.
For those not matching on major elements but having a NDI possible match, individual cases were reviewed to evaluate whether death status was determinable. First, sex was utilized. If this did not correlate, the possible match was eliminated. Next, date of birth was analyzed. If the date of birth was greater than 10 years from our date of birth, the possible match was eliminated. Next, if the last name matched only on the first initial, the match was eliminated. After this algorithm, only 2 patients with NDI potential matches remained and both were coded as indeterminate death status. Neither patient had follow-up care in our institution after the date of death recorded by the NDI.
Alive patients were classified as those with no NDI matches. The follow-up date for alive patients was determined to be the latter of either the date of the NDI query or the most recent care in our institution. For dead patients, the date of follow-up was the date of death. For all deaths, the institutional medical record was searched to insure no patient classified as dead received care following the NDI date of death reported. No conflicts were identified.
Cause of death
In addition to death status, cause of out of hospital death was provided by death certificates from the NDI and based upon ICD-10 coding structure. Death categories were grouped into trauma and non-trauma causes. Deaths were attributable to trauma if the death certificate listed a traumatic cause as either the primary cause of death or a contributing cause of death. The non-trauma causes found in these patients were grouped as substance abuse/overdose, cardiovascular, sepsis/infectious, cancer, renal, pulmonary, and unknown. Death certificate data was available on all NDI matched deaths except for 2 patients in which only date of death was provided from the reporting state.
Data analysis
Data are presented as mean (standard deviation), median (interquartile range), or percentage; univariate and group comparisons were made using 2 tailed Student’s t test or one-way analysis of variance for normally distributed data, Wilcoxon rank sum or Kruskal Wallis testing for skewed data, and Fisher’s exact test for proportions. Kaplan-Meier survival curves were computed to assess the time to event and compared using log-rank analysis. The curves were created stratified for injury severity (ISS). Reported survival of our cohort was compared with estimated survival based on US Population Vital Statistics(5). Each patient’s predicted yearly survival was calculated using US Life Tables adjusted by age, gender, and ethnicity using the method described previously by Mell et al(6). Mean overall estimated survival of the cohort was then calculated with standard descriptive statistics. Data analysis was conducted using SPSS software version PASW Statistics 18 and SAS version 9.2 (Cary, N.C.). Statistical significance was determined at the level of p < .05.
Results
Study group characteristics
During the study period, 908 highest level activation patients had been enrolled with at least one year lapsing between time of enrollment and the latest available NDI data file. The patients were predominantly male (80.0%),had a median age of 36 (IQR 25–53), and 59.9% suffered blunt injury [Table 1]. Falls (23.1%) were the most common mechanism followed by gunshot wounds (19.5%), stab wounds (19.5%), and pedestrians struck (13.5%). Patients had a median ISS of 18 and 43.4% had an ISS >=25. Significant head injury as classified as a head AIS>=3 was present in 44.7% [Table 1]. Patients were hospitalized for a median of 5 days (IQR 2–17). The majority of patients (76.4%, n=694) were admitted to the ICU with a median ICU length of stay of 2 days (IQR 0–7). The 24 hour mortality was 7.5% (69/908) with an overall in-hospital mortality of 23.0% [Table 2].
Table 1.
Demographic Data
| n | value | |
|---|---|---|
| Male | 726 | 80.0% |
| Age (median) | 908 | 36 (IQR 25–53) |
| Race/Ethnicity | ||
| Caucasian | 436 | 48.0% |
| Black | 214 | 23.6% |
| Hispanic | 209 | 23.0% |
| Other | 49 | 5.4% |
| Blunt | 544 | 59.9% |
| ISS (median) | 908 | 18 (IQR 5–30) |
| ISS <15 | 390 | 43.0% |
| ISS 15–24 | 124 | 13.7% |
| ISS >=25 | 394 | 43.4% |
| Head AIS >=3 | 406 | 44.7% |
| Chest AIS >=3 | 259 | 28.5% |
| Abdomen AIS >=3 | 140 | 15.4% |
n: number of patients; ISS: injury severity score; AIS: abbreviated injury severity score
Table 2.
Outcome data
| ICU days (median, IQR) | 2 | IQR 0–7 |
| Hospital days (median, IQR) | 5 | IQR 2–17 |
| Lost to follow-up | 0.2% | 2 / 908 patients |
| Median follow-up (IQR) | 1.7 years | IQR 1.0 – 2.9 years |
| Maximum follow-up | 9.8 years | |
| Overall survival | 73.0% | 663/908 patients |
| Mortality | ||
| 24-hour | 7.5% | 69/908 patients |
| 30-day | 22.1% | 201/908 patients |
| In-hospital | 23.1% | 210/908 patients |
| Out-of-hospital | 5.0% | 35/698 patients |
| Trauma related cause of death | 90.2% | 221/245 deaths |
| Out of hospital trauma related cause of death | 42.8% | 15/35 deaths |
ICU: intensive care unit; IQR: interquartile range
Vital status determination
392 (56.2%) of the 698 patients surviving to hospital discharge had no National Death Index (NDI) registry files found on query and were classified as alive as of December 31, 2013. Possible registry files were ascertained for the remaining 44.0% (n=307). Of the potential matches, social security numbers had been submitted for 83.7% (257/307). For each patient with a NDI registry file, an average of 3.4 potential death certificates was provided as possible matches. Twenty-six patients had a perfect match on all available variables and were classified as dead. Amongst these were 4 patients in whom the social security was not known at the time of the trauma, but they were an exact match for all other variables. Of the remaining probable NDI match records, 9 additional patients were felt to be likely deceased for a total of 35 confirmed out of hospital deaths.
Possible matches were able to be excluded in 99.3% (270/272) of the remaining patients with a NDI files based upon the death certificate death preceding the incident trauma hospitalization (n=192), social security number not matching (n=49), or age being greater than 10 years off (n=29). Of the two patients who could not be conclusively matched, neither had a social security number provided. One had several exact matches on name, age, sex, but with different dates of death. The other had several matches due to a common last name and only a first initial match. Both were classified as alive for further analysis as death could not be confirmed definitively.
Long-term Mortality Outcome
Patients were followed for a median 1.7 years (IQR 1.0 – 2.9 years) with a maximum follow-up of 9.8 years. Survival data was available on 99.8% of patients [Table 2]. Overall survival was 73.0% (663/908). The 30 day mortality was 22.1% (201/908 patients). 18.0% (44/245 deaths) of deaths occurred after 30 days and 79.5% (35/44) of these occurred post-hospital discharge. For those who died post-discharge, the most common initial mechanism of injury was falls (n=10/35), followed by gunshot wounds (n=6), motor vehicle collisions (n=4), and pedestrians struck (n=4). There was no difference in median AIS head (2 vs 0, p=0.12), chest (0 vs 0, p=.54), or abdomen (0 vs. 0, p=.94) between those dying out of hospital and surviving. Those who died post-discharge had longer initial ICU lengths of stay of compared with those still alive at the latest out of hospital follow-up (median 5 days vs 2 days, p<0.001). An initial ICU stay of >=14 days occurred in 28.5% (10/35) of those who experienced a post-discharge death.
Amongst late deaths, 53.0% occurred between 31 days to 1 year post trauma. For those with at least 2 year follow-up, overall survival was only 62.3% (317/509). Severity of injury predicted long-term survival (p<.0001) with those severely injured (ISS>=25) having the poorest outcome of an overall 57% survival at 5 years (Table 3). For all ISS groups, survival was worse than predicted actuarial survival (p<0.001) [Figure 1]. Excluding early deaths (<=30 days), observed survival was still significantly lower than estimated actuarial survival from day 31 to 5 years across ISS groups [p<0.002]. More specifically, out of hospital mortality was increased across the ISS groups with a 4% mortality in those with minor injury, 7% in moderate injury, and 10% in severely injured patients (p=0.012). Those with an ISS>=25 had an HR (hazard ratio) of out of hospital death of 2.7 (1.4 – 5.3) compared with those having an ISS <15 (p=0.004).
Table 3.
Survival estimates
| Overall Cohort | ||||
|---|---|---|---|---|
| actuarial | ISS <15 | ISS 15–24 | ISS >25 | |
| 1 year | 98.97% | 96.38% | 87.60% | 61.56% |
| 2 year | 98.05% | 94.91% | 86.78% | 61.26% |
| 3 year | 96.80% | 92.29% | 84.50% | 59.20% |
| 4 year | 95.97% | 90.33% | 84.50% | 59.20% |
| 5 year | 94.70% | 90.33% | 80.17% | 56.89% |
ISS: injury severity score
Figure 1.
5 year Survival for Cohort stratified by injury severity score (ISS)
Discharge location was known for 34/35 patients suffering out of hospital deaths. An equal number of patients (n=17) were discharged directly home compared with not home (n=17). Amongst those not discharged directly home, 7 went to rehabilitation centers, 6 went to inpatient or long-term acute care facilities, and 4 went to skilled nursing facilities. Those discharged home who died were slightly younger (median 51 years, IQR 42–56) compared to those who died after discharge to long-term care/rehab facilities (59 years, IQR 46–82; p=0.03). There was no statistical difference between the median ISS of those being discharged directly home (14, IQR 5–22) versus not home (26, IQR 11–33; p=0.07). No patient in our study was discharged to outpatient hospice. Trauma related mortality was the leading cause of post-discharge death accounting for 42.9% of the late deaths [Table 4]. Although those discharged home had a lower absolute incidence of post-discharge trauma related mortality (29%), there was no statistical difference compared with those not initially discharged home (58%; p=0.09). For those who died of a traumatic cause out of hospital (TOHD), the median survival was only 12 months (IQR 5–29 months) compared with 16 months (IQR 5–35) for those dying of non-trauma causes (p=0.80). The median age of patients suffering TOHD was lower (52 years, IQR 26–59), but not statistically different than non-trauma deaths (54 years, IQR 48–65; p=0.21). The TOHD appeared to be more injured then their non-trauma death counterparts having a median ISS of 26 (IQR 17–30) versus 13 (IQR 5–24; p=0.03). One patient who died post-discharge suffered a repeat suicide attempt.
Table 4.
Cause of Death Distribution
| Cause of Death | Overall (n=245) |
Out of Hospital (n=35) |
||
|---|---|---|---|---|
| n | % | N | % | |
| Trauma related | 221 | 90.2% | 15 | 42.9% |
| Substance abuse/Overdose | 7 | 2.9% | 7 | 20.0% |
| Cardiovascular | 7 | 2.9% | 5 | 14.3% |
| Infectious/Sepsis | 4 | 1.6% | 4 | 11.4% |
| Pulmonary | 1 | 0.4% | 1 | 2.9% |
| Cancer | 1 | 0.4% | 1 | 2.9% |
| Unknown | 2 | 0.8% | 2 | 5.7% |
n: total number of patients
Despite falls being the most common initial mechanism suffered by patients who died out of hospital, 80% (n=8/10) ultimately died of non-trauma causes and the median age of these patients was 53 years (IQR 46–81). The most common cause of non-trauma out of hospital deaths were drug overdoses or complications of substance abuse (n=7), followed by cardiovascular events (n=5) [Table 4]. Those dying out of hospital as a result of overdose/substance abuse were younger (median 49 years, IQR 44–52), than those who died of cardiovascular events (60 years, IQR 51–91; p=0.03).
Discussion
This study represents the first investigation in the United States following traumatic injury to compare long-term mortality following traumatic injury to predicted population actuarial survival and confirms the hypothesis that the risk of trauma related mortality continues beyond hospital discharge. As attention has been increased on hospital level performance metrics, there has been a growing concern that in-hospital mortality data may be significantly bias. A recent report in the British Medical Journal noted that “analyses based only on in-hospital deaths are potentially biased by differences in hospitals’ discharge practices(7).”
This is particularly relevant for traumatic injury, especially in those with traumatic brain injury (TBI). As an example, for those suffering severe TBI, there is widespread variation in timing of limitation of further care and rates of placement in long term care facilities have been found to reflect geographic variation and differing practitioner practices. For these patients, little prior data exists as to their outcome once discharged but a recent study suggested that out of hospital TBI deaths account for an additional 6 to 10% mortality(8). If this mortality was not factored into a trauma centers risk adjusted performance metrics, inaccuracy in classification of quality of care could be affected.
The bias introduced by capturing mortality data based upon those who survive only to hospital discharge has been termed discharge bias(7, 9). As more emphasis has shifted toward reduction of length of stay, out of hospital mortality has increased. A 2013 Dutch study of all comer admissions (medical and surgical) found that a shorter length of stay was associated with low in-hospital mortality, but higher post-discharge mortality(7). Davidson et al. in 2011 examined a statewide discharge database and found that despite in-hospital trauma mortality rates nearly cut in half from 1995 to 2008, out of hospital rates rose significantly from 4.7% to 7.4%(10). The rise in out of hospital mortality rates were attributed to both changes in discharge practices and improvements in care for those severely injured who now survive the initial hospitalization to latter succumb to trauma related complications.
Santry et al. recently proposed in their June 2015 publication that the traditional description of death after trauma being trimodal (pre-hospital, early in-hospital, and late in-hospital deaths) should be altered to be “quadrimodal(11).” The introduction of the “quadrimodal” model would include those deaths that occur post-discharge. They identified 1695 trauma patients retrospectively from their trauma registry that required intensive care admission and found similar results to our study. Whereas 53% of our patients died surviving to hospital discharge died within 1 year post-discharge, 47% of their patients were dead at 1 year(11). Both our study and the Santry study differ from the Davidson study by inclusion of a much sicker cohort of patients which explains our increased overall mortality. The Santry studied did not include cause of death as they only utilized the social security death index to determine if patients were alive or dead.
Although the vast majority of trauma related deaths occur in-hospital, a few prior studies have examined out of hospital mortality and all report an additional mortality of between 5 to 15%(9, 12). Our additional overall mortality of 5.0% (35 post-discharge deaths out of 698 patients alive at hospital discharge) for our cohort is consistent with these findings. None of these prior studies detailed cause of death and deaths were assumed to be trauma related. Of the trauma related deaths in our study (n=236 total, 221 in-hospital, 15 out of hospital), 93.6% occurred in the hospital. The out of hospital deaths resulted in an overall trauma specific mortality increase from 24.3% (221/908) to 26.0% (236/908).
The increase in overall trauma mortality appears modest with inclusion of out of hospital deaths, but importantly, 43% of the out of hospital deaths were attributable directly to trauma. The only other two studies to detail specific causes of death following traumatic injury were conducted outside the US in Germany and Norway. The German study was a population based study where 19% of post-discharge deaths were trauma related with an additional 9% suicide related(13). Whereas we have nearly complete death data on our cohort, the German study had a high (17%) rate of missing data, specifically death certificate data missing in 15% of their patients. As a result, they excluded these patients in the death analysis which could contribute to the discrepancy in findings. In contrast, our results are similar to the Norwegian study where 47% of the out of hospital deaths were confirmed to be trauma related(14). Given these findings in conjunction with the prior literature, efforts should be undertaken to standardize methods for ascertainment of longer term mortality data for benchmarking trauma center performance.
Our study is the first to investigate post-traumatic survival using actuarial population predicted survival. We demonstrated that even in less injured patients, post-trauma survival is different compared with actuarial population based survival controlled for age, gender, and ethnicity. Although a large proportion of the deaths are trauma specific, the significant rate of death due to high risk behaviors including substance abuse and mental health reflect the hypothesis that traumatic injury may be marker of poorer life expectancy. Prior authors have hypothesized in the literature that being a victim of trauma for some is a marker of high risk behavior that contributes later in life to earlier death(13). Our data seems to provide further support that secondary prevention effort after trauma to mitigate high risk behavior is warranted.
This study has several limitations. First, probabilistic matching was utilized to determine out of hospital deaths. The National Death Index (NDI) does not require social security numbers for matching which allows trauma centers that have a sizable rate of undocumented persons to still track long-term outcomes. In order to minimize risk for incorrect matching, we utilized a stringent matching algorithm placing emphasis on exact or near exact matches for determination of death status. This has the risk of biasing our results toward underestimating out of hospital deaths. Second, we are limited with regards to cause of death to what is reported on the death certificates to the NDI. Therefore, we can only attribute trauma as a cause of death if it was specifically listed on the death certificates. This may also bias our results toward under-reporting of trauma related deaths. Third, we cannot determine if out of hospital trauma related deaths were a result of the initial traumatic incident or a subsequent traumatic event due to ICD coding limitations. However, given how short the interval was from discharge to median death, we feel it is most likely that these deaths resulted from the incident event. Finally, given the small number of overall out of hospital deaths, the study is underpowered to detect a difference between characteristics of those who died out of hospital from trauma and non-trauma causes including the impact of discharge location on out of hospital death.
Conclusions
Post-discharge deaths represent an important percentage of total trauma related mortality especially for those severely injured. Despite having ‘survived’ to leave the hospital, long term survival was worse than predicted actuarial survival suggesting that the mortality from injury does not end at ‘successful’ hospital discharge. Efforts should be undertaken to track deaths beyond hospital discharge to understand the true outcome following trauma.
Acknowledgments
Funding for Study: Dr. Callcut was supported with salary support from the National Center for Advancing Translational Sciences (NIH grant 8KL2TR000143-09) via the University of California San Francisco Clinical & Translational Science Institute (CTSI) and via a Research Scientist Development Award from the National Institute of Environmental Health Sciences (NIEHS) of the NIH (award K01ES026834).
Footnotes
This work was presented at the American Association for the Surgery of Trauma Annual Meeting September 2015 in Las Vegas, Nevada.
Author contributions:
Callcut - literature search, study design, data collection, data analysis, data interpretation, writing
Wakam – literature search, study design, data collection, critical review
Conroy – data collection, data analysis, critical review
Kornblith – study design, data collection, data interpretation, critical review
Howard – study design, data collection, data interpretation, critical review
Campion – study design, data collection, critical review
Nelson – study design, data collection, critical review
Mell – study design, data analysis, data interpretation, critical review
Cohen – study design, data interpretation, critical review
Contributor Information
Rachael A. Callcut, Email: Rachael.Callcut@ucsf.edu.
Glenn Wakam, Email: Glenn.Wakam@ucsf.edu.
Amanda S. Conroy, Email: Amanda.Conroy@ucsf.edu.
Lucy Z. Kornblith, Email: Lucy.Kornblith@ucsf.edu.
Benjamin M. Howard, Email: Benjamin.Howard@ucsf.edu.
Eric M. Campion, Email: Eric.Campion@dhha.org.
Mary F. Nelson, Email: Mary.Nelson@ucsf.edu.
Matthew W. Mell, Email: mwmell@stanford.edu.
Mitchell J. Cohen, Email: Mitchell.Cohen@ucsf.edu.
References
- 1.Norton R, Kobusingye O. Injuries. N Engl J Med. 2013 May 2;368(18):1723–1730. doi: 10.1056/NEJMra1109343. [DOI] [PubMed] [Google Scholar]
- 2.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon J, Abdalla S, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec 15;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Weir S, Salkever DS, Rivara FP, Jurkovich GJ, Nathens AB, Mackenzie EJ. One-year treatment costs of trauma care in the USA. Expert Rev Pharmacoecon Outcomes Res. 2010 Apr;10(2):187–197. doi: 10.1586/erp.10.8. [DOI] [PubMed] [Google Scholar]
- 4.Rogers FB, Osler T, Krasne M, Rogers A, Bradburn EH, Lee JC, Wu D, McWilliams N, Horst NA. Has TRISS become an anachronism? A comparison of mortality between the National Trauma Data Bank and Major Trauma Outcome Study databases. J Trauma Acute Care Surg. 2012 Aug;73(2):326–331. doi: 10.1097/TA.0b013e31825a7758. discussion 31. [DOI] [PubMed] [Google Scholar]
- 5.Arias E. United States Life Tables. National Vital Statistics Reports 2010. 2010 [PubMed] [Google Scholar]
- 6.Mell M, White JJ, Hill BB, Hastie T, Dalman RL. No increased mortality with early aortic aneurysm disease. J Vasc Surg. 2012 Nov;56(5):1246–1251. doi: 10.1016/j.jvs.2012.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pouw ME, Peelen LM, Moons KG, Kalkman CJ, Lingsma HF. Including post-discharge mortality in calculation of hospital standardised mortality ratios: retrospective analysis of hospital episode statistics. BMJ. 2013;347:f5913. doi: 10.1136/bmj.f5913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raj R, Skrifvars MB, Kivisaari R, Hernesniemi J, Lappalainen J, Siironen J. Acute alcohol intoxication and long-term outcome in patients with traumatic brain injury. J Neurotrauma. 2015 Jan 15;32(2):95–100. doi: 10.1089/neu.2014.3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vasilevskis EE, Kuzniewicz MW, Dean ML, Clay T, Vittinghoff E, Rennie DJ, Dudley RA. Relationship between discharge practices and intensive care unit in-hospital mortality performance: evidence of a discharge bias. Med Care. 2009 Jul;47(7):803–812. doi: 10.1097/MLR.0b013e3181a39454. [DOI] [PubMed] [Google Scholar]
- 10.Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA. 2011 Mar 9;305(10):1001–1007. doi: 10.1001/jama.2011.259. [DOI] [PubMed] [Google Scholar]
- 11.Santry HP, Psoinos CM, Wilbert CJ, Flahive JM, Kroll-Desrosiers AR, Emhoff TA, Kiefe CI. Quadrimodal distribution of death after trauma suggests that critical injury is a potentially terminal disease. J Crit Care. 2015 Jun;30(3):656 e1–656 e7. doi: 10.1016/j.jcrc.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Claridge JA, Leukhardt WH, Golob JF, McCoy AM, Malangoni MA. Moving beyond traditional measurement of mortality after injury: evaluation of risks for late death. J Am Coll Surg. 2010 May;210(5):788–794. 94–96. doi: 10.1016/j.jamcollsurg.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Probst C, Zelle BA, Sittaro NA, Lohse R, Krettek C, Pape HC. Late death after multiple severe trauma: when does it occur and what are the causes? J Trauma. 2009 Apr;66(4):1212–1217. doi: 10.1097/TA.0b013e318197b97c. [DOI] [PubMed] [Google Scholar]
- 14.Skaga NO, Eken T, Jones JM, Steen PA. Different definitions of patient outcome: consequences for performance analysis in trauma. Injury. 2008 May;39(5):612–622. doi: 10.1016/j.injury.2007.11.426. [DOI] [PubMed] [Google Scholar]