Abstract
Magnetic resonance elastography (MRE) is an innovative imaging technique for the non-invasive quantification of the biomechanical properties of soft tissues via the direct visualization of propagating shear waves in vivo using a modified phase-contrast magnetic resonance imaging (MRI) sequence. Fundamentally, MRE employs the same physical property that physicians utilize when performing manual palpation - that healthy and diseased tissues can be differentiated on the basis of widely differing mechanical stiffness. By performing “virtual palpation”, MRE is able to provide information that is beyond the capabilities of conventional morphologic imaging modalities. In an era of increasing adoption of multi-parametric imaging approaches for solving complex problems, MRE can be seamlessly incorporated into a standard MRI examination to provide a rapid, reliable and comprehensive imaging evaluation at a single patient appointment. Originally described by the Mayo Clinic in 1995, the technique represents the most accurate non-invasive method for the detection and staging of liver fibrosis and is currently performed in more than 100 centers worldwide. In this general review, the mechanical properties of soft tissues, principles of MRE, clinical applications of MRE in the liver and beyond, and limitations and future directions of this discipline -are discussed. Selected diagrams and images are provided for illustration.
Keywords: Magnetic resonance elastography, Elasticity imaging techniques, Liver disease, Fibrosis, Emerging applications
Core tip: Magnetic resonance elastography (MRE) is a non-invasive technique for probing the mechanical properties of biologic tissues. The three main steps involved in the MRE technique include the production of mechanical waves in soft tissues, the adoption of a modified phase-contrast MR sequence to image wave motion, and the application of an inversion algorithm to convert the wave image into an elastogram. MRE has received validation for the non-invasive assessment and grading of fibrosis in chronic liver disease patients. MRE also has potential diagnostic applications in other organ systems and may help further the understanding of disease processes.
INTRODUCTION
Magnetic resonance elastography (MRE) is a rapidly emerging non-invasive diagnostic technique for the detection and characterization of a wide range of disease processes. By interrogating the biomechanical properties of tissues, which range widely in physiologic and pathologic states, MRE renders information that is beyond the capabilities of conventional imaging modalities that rely almost exclusively on morphological changes for detecting disease. In an era of increasing adoption of multi-modality techniques for evaluating complex disease processes, MRE may be incorporated into a standard magnetic resonance imaging (MRI) examination to provide a rapid, reliable and comprehensive imaging assessment at a single patient appointment. The largest amount of clinical experience in MRE is in the evaluation of chronic parenchymal liver diseases although MRE has applicability in other organs systems as well. In this general review - the mechanical properties of soft tissues, principles of MRE, clinical applications of MRE in the liver and beyond, and limitations and future directions of this discipline - are discussed.
MECHANICAL PROPERTIES OF SOFT TISSUES
Elasticity imaging is a field of medical science that involves the profiling of the mechanical properties of biologic tissues for the detection and characterization of disease. This discipline derives its motivation from palpation, a clinical assessment technique that has stood the test of time, having been passed down to successive generations of physicians for centuries. When tissues become pathologic, biomechanical changes occur which alter the rigidity of these tissues, a phenomenon perceived on palpation as increased stiffness. The term “stiffness”, a biomechanical property of tissue, represents its ability to resist deformation when subjected to a force. The mechanical properties of biologic tissues, including between physiologic and pathologic states, vary widely by more than 4 orders of magnitude[1,2]. In comparison, conventional modalities such as ultrasound (US), computed tomography and MRI vary over a much narrower diagnostic range. Since its clinical introduction 2 decades earlier, many elasticity imaging techniques have been explored. These applications vary in several ways including[1-6]; (1) the origin of the stress (external/internal); (2) the temporal characteristics of the stress (static/quasi-static/dynamic); and (3) the imaging platform (optical imaging/ultrasound elastography/MRE) used. Irrespective of the particular technique in question, all applications share the same foundational concept. This involves (1) generating a stress in a target tissue; (2) examining the tissue’s strain response; and (3) characterizing the stress-strain dynamics of the tissue. In material science, stress is defined as “force applied per unit area” while strain is defined as “tissue displacement per unit sample length”. The slope of the stress-strain curve is the “elastic modulus” - a physical parameter that reflects the intrinsic stiffness of the tissue (Figure 1).
Figure 1.
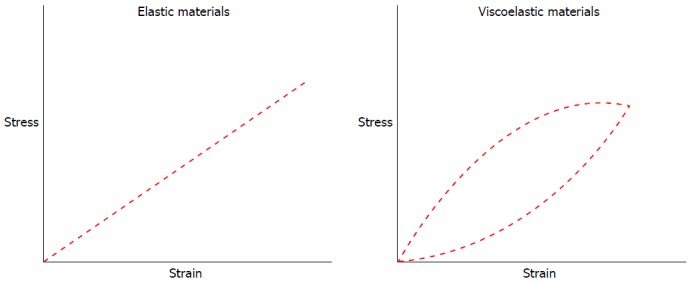
Schematic diagram illustrates the stress-strain relationship of elastic materials and viscoelastic materials.
Purely elastic materials demonstrate “spring-like” behavior, where stress and strain are linearly related according to Hooke’s Law. However, most biologic tissues are viscoelastic and show both elastic and viscous properties. In these tissues, the elastic modulus is a complex entity that comprises a storage modulus (representing elasticity) and a loss modulus (representing viscosity). The viscosity component exhibits a “dashpot like” behavior (damping), where the strain rate varies with time and is characterized by a hysteresis loop due energy losses from loading and unloading of stresses. Mathematical models such as described by Maxwell, Volgt, and Kelvin (using different combinations of springs and dashpots) have been developed to predict the stress-strain dynamics of viscoelastic materials[3]. Depending on the type of stress encountered, the elastic modulus is reported as Young’s modulus, E {[longitudinal (compressive or tensile) stress]/longitudinal strain}, shear modulus, μ {[shear (transverse) stress]/shear strain} or bulk modulus, K (volumetric stress/volumetric strain). The SI unit for elastic modulus is expressed in kilopascals (kPa) where 1 kPa = 1 kN/m2. The relationship between E, μ and K is defined mathematically as:
μ = E/[2(1 + v)] and K = E/[3(1 - 2v)]
Since the Poisson’s ratio, v (tranverse contraction per unit breath/longitudinal extension per unit length) for most soft tissues is very close to an incompressible liquid (v = 0.5), E approximately equal 3μ. K does not vary significantly in biologic tissues[7]. MRE utilizes shear wave propagation within target tissues to calculate the shear modulus[8]. Assuming that biologic tissues are homogeneous, isotropic and linearly elastic, μ is calculated as follows[2]:
μ = ρvs2 or ρλ2ƒ2 and vs = λƒ
where vs is the speed of the shear wave (m/s), λ is the wavelength of the shear wave (m), ƒ is the frequency of the shear wave (Hz) and ρ is the soft tissue density (assumed to be 1000 kg/m3)[2]. Given that these assumptions may be inaccurate as biologic tissues have viscoelastic properties, the term “shear stiffness” is used in MRE as an approximation for the effective shear modulus estimated at a specified frequency. Given the contribution of viscoelasticity on tissue stiffness, using the same excitation frequency is a key issue in maintaining consistency between MRE examinations. MRE may be performed using either a quasi-static or dynamic excitation - while the former offers a qualitative estimation of tissue stiffness, the latter is preferred as it allows a precise quantitative assessment of this parameter[8-11].
PRINCIPLES OF MRE
Dynamic MRE is a diagnostic technique that was originally described at the Mayo Clinic by Muthupillai and colleagues in 1995[8,12,13]. MRE can be performed on most standard MRI platforms, be this 1.5T or 3T, with the introduction of additional hardware and software[2,12] (Figures 2-4). The three main steps involved in the MRE technique include the production of mechanical waves in soft tissues, the adoption of a modified phase-contrast MR sequence to image wave motion, and the application of an inversion algorithm to convert the wave image into an elastogram[8,12].
Figure 2.
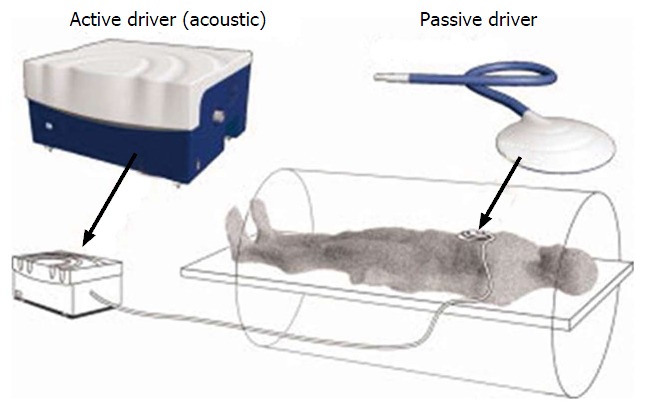
Schematic diagram demonstrates the set up for an magnetic resonance elastography examination using a pneumatic actuator system. Reproduced with permission from “John Wiley and Sons”, Venkatesh et al[12].
Figure 4.
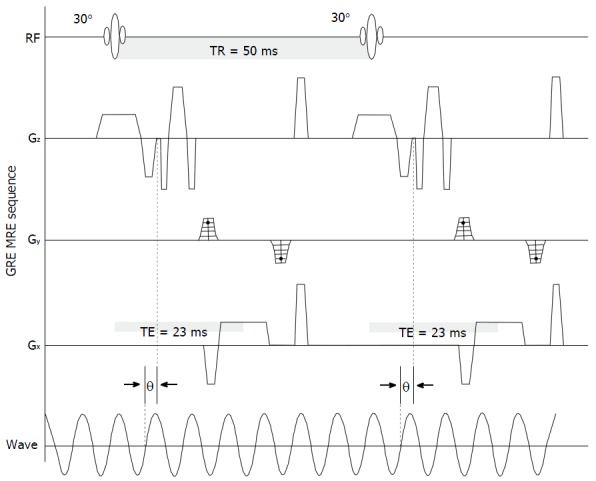
Gradient-echo magnetic resonance imaging sequence with motion sensitizing gradient applied along the slice selection direction (GZ) to detect cyclic motion in that direction. A phase offset (θ) between the MSG and the acoustic driver was adjusted to acquire wave images at different time intervals during a single period of wave motion. Reproduced with permission from “Elsevier”, Yin et al[13]. MSG: Motion sensitizing gradient.
Figure 3.
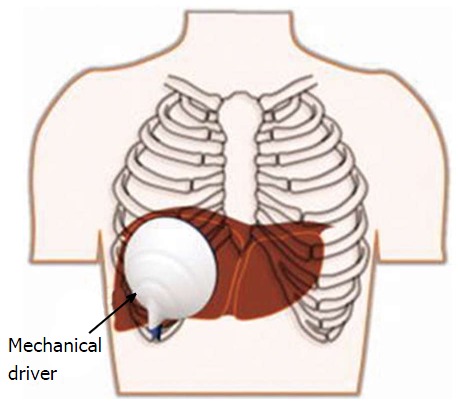
Typical transcostal position of the passive driver for magnetic resonance elastography assessment of the liver. Reproduced with permission from “John Wiley and Sons”, Venkatesh et al[12].
Mechanical excitations are produced by actuator devices such as pneumatic, electromechanical and piezoelectric systems, which are positioned against the body surface close to the target organ. These devices generate longitudinal compression waves at skin surfaces, which are then mode converted at internal tissue interfaces into transverse shear waves. A pneumatic system incorporates a non-MRI compatible active driver (placed outside the scan room) for producing continuous acoustic wave motion, an MRI compatible passive driver placed against the body surface, and an air-filled plastic tube for transmitting the pneumatic excitations from the active to the passive driver. The active driver generally consists of a signal generator connected to an audio amplifier and a loudspeaker. The passive driver for most abdominal applications has a drum or disc-shaped design to maximize surface area contact, and this may be applied to the body in any orientation. It is often secured to the patient by an elastic strap. A transcostal position is favored over a subcostal position when imaging the liver, as trans costal excitation improves penetration as the ribs act as a secondary wave source[14]. Limitations of pneumatic actuators include susceptibility to phase delays that may affect synchronization with the MRI sequence, and reduced effectiveness at frequencies > 300 Hz[15,16]. Electromechanical actuators have the advantage of good synchronization with the MRI sequence and can produce high amplitude mechanical excitations at low power requirements[15]. However, these systems can cause electromagnetic interference with eddy current induction leading to MRI artifacts and heat build-up. As such, electromechanical actuators have to be positioned remote from the imaging region and have to conform to a fixed orientation with respect to the static magnetic field[15]. Piezoelectric actuators provide stable and precise mechanical excitation up to frequencies of 500 Hz but are relatively expensive[15].
The propagating shear waves are imaged using a phase contrast MRI technique that includes oscillating motion sensitizing gradients (MSGs). This may be achieved with a wide range of sequences such as gradient-echo, spin-echo, balanced steady-state free precession or echo-planar imaging. The MSGs measure tissue motion along a specified direction, and can be applied along all 3 orthogonal planes of motion to capture the entire 3-dimensional (3D) wave vector. Trigger pulses are used to synchronize the mechanical excitations with the MRI sequence, and the actuator and MSGs are typically set to the same frequency (e.g., 40-200 Hz)[17]. Shear wave motion in tissues induces cyclic spin displacement of protons, which in the presence of synchronized MSGs are encoded as phase shifts within the MRI signal. The phase shifts are calculated as follows[8]:
Math 1
Math 1.
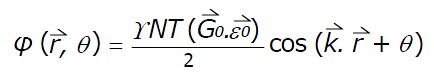
Math(A1).
Where φ is the phase shift, vector r is the spin position vector, Θ is the relative phase of mechanical and magnetic oscillations, ϒ is the gyromagnetic ratio, N is the number of gradient cycles, T is the period of the gradient waveform, G0 is the MSG vector, vector Ε0 is the displacement amplitude vector, and vector k is the wave vector[8]. The phase shift is proportional to the dot product of the MSG and the displacement vectors[8]. This information is used by the MRI signal to create phase and magnitude images. A curl filter is then applied to separate the shear wave data from the longitudinal wave data. The resultant MRI image, called a wave image, is a spin displacement map - a snapshot of the shear wave motion in the tissues (with sensitivity to displacements as small as 100 nm)[8]. Several wave images at different time points are acquired by varying the phase offset between the actuator and the MSGs. Typically, 4 to 8 phase offsets are applied.
Post-processing inversion algorithms, such as local frequency estimation and algebraic inversion of the differential equation, are used to transform the wave images into elastograms. The elastograms are quantitative maps of tissue stiffness and are displayed as both greyscale and color images. Tissue stiffness is assessed by performing region of interest tracings of the target organ, in areas that have adequate wave amplitude, and which do not extend closer than half a wavelength to the organ boundary[12]. Tracings should avoid large vessels and areas affected by motion artifact[12].
CLINICAL APPLICATIONS IN THE LIVER
The largest volume of collective experience on MRE is in the investigation of chronic liver diseases (CLD) (Figure 5). Multiple studies have confirmed the value of MRE for the non-invasive evaluation of liver fibrosis[13,14,18-23]. A systemic review and meta-analysis by Singh et al[22] of 12 studies involving 697 patients with a less than one year interval between MRE and liver biopsy reported that MRE had high accuracy for the diagnosis of significant (F2) or advanced fibrosis (F3) and cirrhosis (F4) independent of etiology of CLD or body mass index (BMI). On receiver operating characteristic (ROC) analysis, the area under the ROC curve and 95%CI for MRE were 0.84 (0.76-0.92) for ≥ F1, 0.88 (0.84-0.91) for ≥ F2, 0.93 (0.9-0.95) for ≥ F3 and 0.92 (0.9-0.94) for F4. The study also reported a low failure rate of 4.3% for MRE. A meta-analysis by Su et al[23] of 13 studies involving 989 patients also showed a high diagnostic performance for MRE in the detection and staging of liver fibrosis. The authors found pooled sensitivities and specificities for MRE of 87% (95%CI: 84%-89%) and 92% (95%CI: 87%-96%) for F ≥ 1, 87% (95%CI: 84%-90%) and 92% (95%CI: 89%-95%) for F ≥ 2, 88% (95%CI: 85%-91%) and 91% (95%CI: 88%-93%) for F ≥ 3, and 91% (95%CI: 87%-94%) and 92% (95%CI: 89%-94%) for F4. The pooled area under the ROC curve was 0.95 for F ≥ 1, 0.97 for F ≥ 2, 0.97 for F ≥ 3, and 0.98 for F4. In a study of 50 patients with CLD and 35 healthy volunteers, Yin et al[13] demonstrated that liver stiffness on MRE exhibited a consistent and systematic increase with increasing fibrosis scores (Figure 6). Using a threshold of 2.93 kPa at 60 Hz, Yin et al[13] found that MRE had 98% sensitivity, 99% specificity and 97% negative predictive value for liver fibrosis. MRE also performs well in direct comparisons with other tests such as serum fibrotic markers (APRI - aspartate aminotransferase to platelet ratio index, FIBROSpectII), ultrasound elastography and contemporary MRI techniques (e.g., dynamic contrast-enhanced MRI including gadoxetic acid enhanced MRI, diffusion-weighted imaging, etc.)[19,20,24-27]. In a retrospective study of 58 patients with non-alcoholic fatty liver disease (NAFLD), Chen et al[28] found elevated liver stiffness in patients with non-alcoholic steatohepatitis (NASH), where chronic inflammation was present without fibrosis. MRE was able to stratify NALFD cases into 3 categories - simple steatosis, NASH or fibrosis[28] based on the liver stiffness. Using a threshold of 2.74 kPa, MRE showed high accuracy for differentiating patients with NASH from those with simple steatosis with an area under the ROC curve of 0.93, sensitivity of 94% and specificity of 73%. The authors concluded that MRE had the potential to identify patients with steatohepatitis prior to the onset of fibrosis. Loomba et al[29] evaluated the diagnostic accuracy of MRE for the detection of advanced fibrosis (F3-4) in a prospective study of 117 consecutive patients with biopsy-proven NAFLD. The mean BMI was 32.4 ± 5 kg/m2 and the median time from biopsy to MRE was 45 d. Using a threshold of ≥ 3.63 kPa, MRE had an area under the ROC curve of 0.92 for differentiating F3-4 from F0-2 with 86% sensitivity (95%CI: 65%-97%), 91% specificity (95%CI: 83%-96%), 68% positive predictive value (95%CI: 48%-84%) and 97% negative predictive value (95%CI: 91%-99%). In a randomized double-blind trial by Loomba et al[30] of 50 patients with biopsy-proven NASH, ezetimibe (a drug that inhibits intestinal fat absorption) was compared with placebo - treatment efficacy was assessed using a combination of MRE, MRI derived proton density fat fraction (PDFF) and liver biopsy. Although the study found that ezetimibe did not significantly reduce hepatic steatosis, the authors deemed that the trial was successful in demonstrating that MRE combined with PDFF was a feasible non-invasive method for evaluating treatment response in NASH.
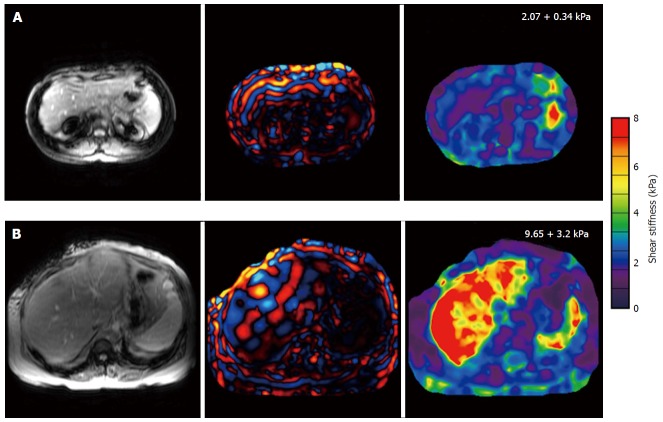
Figure 5.
Largest volume of collective experience on magnetic resonance elastography is in the investigation of chronic liver disease. A: A 32-year-old female with PSC disease stage 1 with normal liver stiffness; B: A 53-year-old female with hepatitis C and presumed cirrhosis, which was determined by MRE results. PSC: Primary sclerosing cholangitis; MRE: Magnetic resonance elastography.
Figure 6.
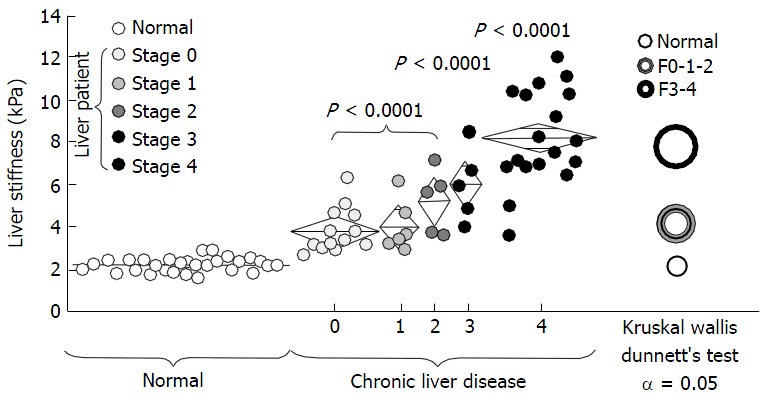
Liver stiffness on magnetic resonance elastography increases systematically with greater fibrosis extent as determined by liver biopsy. Reproduced with permission from “Elsevier” Yin et al[13].
Studies have confirmed that liver MRE is a reliable test with good repeatability and inter-rater agreement[31-34]. While most investigations were performed on a 1.5T MR system, Shi et al[35] showed in 22 healthy volunteers that liver MRE performed on a 3T MR system had good short and mid-term (within 6 mo) repeatability. In a study of 41 healthy Asian volunteers, Venkatesh et al[36] demonstrated that liver stiffness measurements on MRE were not significantly influenced by age, gender, BMI or hepatic steatosis. For liver MRE examinations performed 4 to 6 wk apart, the study found an intraclass correlation coefficient (ICC) of 0.9 (95%CI: 0.78-0.96) and a within-subject coefficient of variation of 2.2%-11.4%. Serai et al[37] found consistent liver stiffness measurements (ICC = 0.994, P < 0.01) in 13 participants (8 healthy volunteers and 5 patients) examined on the same day using 2 separate 1.5-T MR vendor platforms (Phillips and General Electric). On Bland-Altman analysis, the mean stiffness difference between vendor platforms was 0.09 kPa and the 95% limits of agreement were 0.34 kPa and -0.16 kPa. Hallinan et al[38] performed liver MRE twice (before and 5 min after intravenous gadolinium administration) in 210 patients with CLD on the same 1.5T MR system. The study found that gadolinium did not significantly affect the diagnostic performance of MRE for detecting significant liver fibrosis. With the advent of multi-parametric liver imaging, the flexibility of being able to perform MRE either before or after gadolinium administration is an advantage. To determine if participants require to be fasted for liver MRE, a few studies have evaluated whether liver stiffness measurements differ when performed before a meal vs after a meal[33,39,40]. In 12 healthy volunteers, Hines et al[33] found that liver MRE had a within-subject standard deviation of 8.5% and 9% for fasted and fed states, respectively. Yin et al[39] performed liver MRE before and after a meal in 25 patients with biopsy-proven fibrosis and 20 healthy volunteers. Patients with fibrosis showed a significant post-prandial liver stiffness increase of 0.89 ± 0.96 kPa or 21.24% ± 14.98%. Healthy volunteers showed a smaller but significant post-prandial stiffness increase of 0.16 ± 0.20 kPa or 8.08% ± 10.33%. In a study of 19 CLD patients and 11 healthy volunteers, Jajamovich et al[40] showed that liver stiffness measurements on a 3T MR system were significantly higher for the post-prandial state compared with the pre-prandial state. The liver stiffness measurements were also significantly higher in patients compared with healthy volunteers. The mean liver stiffness for CLD patients was 4.9 ± 1.4 kPa for a fasted state vs 5 ± 1.2 kPa for a fed state (P < 0.001) while in healthy volunteers it was 1.8 ± 0.2 kPa for a fasted state and 2 ± 0.2 kPa for a fed state (P < 0.001). The authors concluded that liver MRE should be performed in a fasted state.
MRE may have a role as an alternative to liver biopsy for well-selected patients[12,27]. Biopsy is invasive and is associated with poor patient acceptability and risk of complications. It is also prone to sampling errors and may be non-diagnostic if the sample volume is insufficient or of poor quality. Given its non-invasiveness, MRE is an attractive option for longitudinal patient monitoring, including evaluating treatment efficacy. If a liver biopsy is necessary, MRE could be used to target biopsy to areas where the fibrosis is most severe[41]. A preliminary study involving 44 liver tumors found that MRE was able to differentiate tumors as malignant or benign with 100% accuracy, using a stiffness threshold of 5 kPa at 60 Hz[42]. A recent study of 79 patients with 80 malignant and 44 benign focal liver lesions found that MRE was superior to diffusion weighted imaging (DWI) for differentiating between malignant and benign etiologies[43]. Malignant lesions exhibited a significantly higher mean stiffness (7.9 kPa vs 3.1 kPa, P < 0.001) and lower mean apparent diffusion coefficient value (129 vs 200 × 10-3 mm2/s, P < 0.001) compared with benign lesions[43]. ROC analysis found a significantly higher accuracy for MRE than DWI (0.986 vs 0.82, P = 0.0016)[43]. The study also showed higher stiffness in cholangiocarcinomas compared with hepatocellular carcinomas and focal nodular hyperplasias compared with adenomas.
US elastography methods such as transient elastography (TE) and shear wave elastography (SWE) are alternative techniques to MRE. Each modality has its own merits and limitations. MRE offers wide field imaging coverage and can also be performed as a 3D technique. In contrast, TE is a 1D technique and is limited to narrow field imaging to a maximum depth of 8 cm. As such, MRE has superior diagnostic accuracy compared to TE and provides a more representative delineation of tissue stiffness[20,44]. This is particularly relevant in liver fibrosis which may affect the liver heterogeneously. In a study of 113 patients with CLD, Ichikawa et al[44] found an area under the ROC curve of 0.97 (MRE) vs 0.93 (TE) for F4 (P = 0.03), 0.98 (MRE) vs 0.87 (TE) for ≥ F2 (P = 0.0003) and 0.97 (MRE) vs 0.87 (TE) for ≥ F1 (P = 0.01). In a study of 129 patients, Yoon et al[45] showed that liver stiffness measurements were more reliable on MRE compared with SWE although both techniques showed moderate correlation (r = 0.724) and comparable diagnostic performance for ≥ F2. In a study of 141 patients with CLD, Huwart et al[20] found that MRE had a greater technical success rate than TE (94% vs 84%) - unlike the latter, MRE may be performed in obese subjects and in those with ascites. The merits of US elastography compared with MRE include (1) lower equipment costs; (2) more established technique; (3) shorter examination length; (4) portability (e.g., can be performed at the bedside in unstable patients); and (5) may be performed in claustrophobic patients and those with MRI contraindications. In practice, both modalities are often viewed as complementary, where one technique may be preferred over the other depending on specific circumstances.
CLINICAL APPLICATIONS BEYOND THE LIVER
Several preliminary studies have assessed the utility of MRE in other organs. However, more evidence is needed before definitive recommendations can be made.
Spleen
A couple of studies have evaluated MRE in the spleen (Figure 7). A study of 16 healthy volunteers by Mannelli et al[46] found that splenic stiffness (mean of 3.57 ± 0.59 kPa at 60 Hz) was not influenced by BMI, mean arterial pressure, age, splenic volume or liver stiffness. Talwalkar et al[47] found that splenic stiffness was significantly higher in patients (n = 38) with CLD compared with controls (n = 12), with a splenic stiffness ≥ 10.5 kPa at 60 Hz reported in patients with esophageal varices. In a study of 139 patients, Shin et al[48] found a significant positive linear correlation between splenic and hepatic stiffness measurements and the grade of esophageal varices. Furthermore, the authors found that splenic and hepatic stiffness measurements showed superior performance compared to splenic length in predicting high-risk varices. In 10 patients, Guo et al[49] found a linear correlation between splenic viscoelasticity on multi-frequency MRE and hepatic venous pressure gradient (HVPG) measurements (reflecting portal pressure) before and after transjugular intrahepatic portosystemic shunt placement. On multi-frequency MRE in 36 patients, Ronot et al[50] showed that the splenic loss modulus (representing viscosity) was the best parameter for the non-invasive evaluation of HVPG -this showed potential for detecting high-risk esophageal varices and severe portal hypertension.
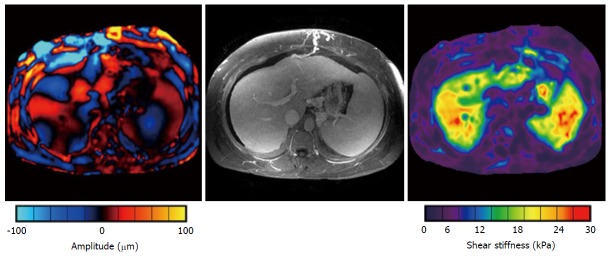
Figure 7.
A patient with non-alcoholic steatohepatitis has a cirrhotic liver with stigmata of portal hypertension including splenomegaly, ascites, esophageal varices, splenorenal shunts and other collaterals. The left image shows mechanical waves throughout the liver and the spleen. In the resulting elastogram (right), both the liver and the spleen show very high shear stiffness values of over 20 kPa.
Kidneys
A few studies have explored the utility of MRE in the kidneys (Figure 7). A study involving 16 healthy volunteers found that renal MRE was a reliable technique as assessed by test-retest repeatability and inter-rater agreement with ICC values > 0.9. The study also found a within-subject coefficient of variation of 7.7% at 60 Hz and 13.6% at 90 Hz[51]. Rouvière et al[52] also reported that renal MRE was a reliable technique with a mean variation of 6% (2%-16%) at 45 Hz and 6% (1%-14%) at 76 Hz in 10 healthy volunteers. Correlating MRE findings with renal transplant biopsy, Lee et al[53] found a non-significant trend towards higher stiffness in moderate fibrosis (n = 2) compared with mild fibrosis (n = 6)[53]. Interestingly, the renal stiffness was slightly higher in a single case of no fibrosis at 120 and 150 Hz, and slightly lower at 90 Hz, compared with 2 cases of moderate fibrosis. The findings should be interpreted with caution given the small sample size. A study of 21 patients with cirrhosis and ascites found that renal MRE has potential for the evaluation of hepatorenal syndrome (HRS)[54]. The study found that renal stiffness in patients with HRS (median stiffness of 3.30 kPa and 2.62 kPa at 90 Hz and 60 Hz, respectively) was significantly lower compared with patients with normal renal function (median stiffness of 5.08 kPa and 3.41 kPa at 90 Hz and 60 Hz, respectively)[54]. On ROC analysis, renal MRE had an area under the ROC curve of 0.94 at 90 Hz and 0.89 at 60 Hz for the detection of HRS. Renal MRE also had an excellent inter-rater agreement with ICC values > 0.9. These early studies provide motivation for new lines of research in the kidneys.
Breast
Preliminary clinical studies involving small numbers of patients suggest that MRE has the potential to distinguish between malignant and benign breast tumors, based on the higher stiffness of malignancies[55-65]. In a breast MRE study involving 20 patients and 15 healthy volunteers, Lorenzen et al[55] found a median stiffness of 15.9 kPa for malignant breast tumors, 7 kPa for benign breast tumors and 2.5 kPa for normal breast parenchyma at 60 Hz. In a study of 57 patients with breast lesions, Siegmann et al[65] found that the addition of breast MRE to conventional contrast-enhanced MRI improved diagnostic yield for lesion characterization.
Brain
Imaging the mechanical properties of the brain may open up new possibilities for the study of brain function and neurologic disease (Figure 7). The MRE measured stiffness varies between different regions in the brain and between healthy and diseased states. In healthy volunteers, stiffness varies between the cerebrum and the cerebellum and between grey and white matter[66-69]. By probing the mechanical properties of brain tissue, MRE may contribute to the understanding of diseases such as multiple sclerosis, Alzheimer’s disease, traumatic brain injury and normal pressure hydrocephalus[70-76]. Preliminary investigations on brain tumors are encouraging and suggest that MRE offers fresh information beyond that of conventional modalities[77,78]. A study by Reiss-Zimmermann et al[79] in 27 patients found that MRE showed potential for characterizing intracranial neoplasms (e.g., glioblastomas, anaplastic astrocytomas, meningiomas and cerebral metastases) based on their mechanical properties including differentiating meningiomas from intra-axial neoplasms. Future work would include assessing if MRE can be used to guide surgical planning including evaluating the adequacy of resection (Figure 8).
Figure 8.
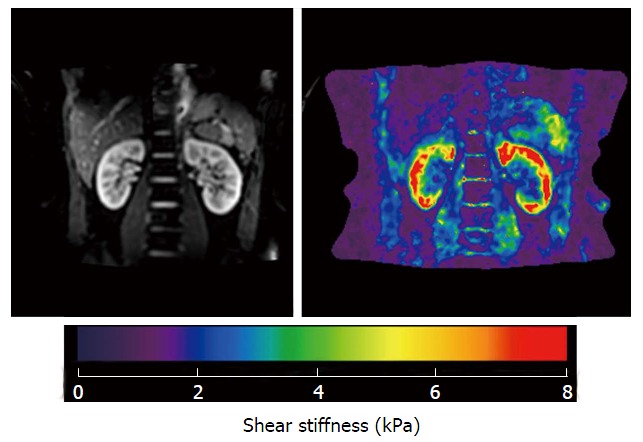
A 2-dimensional multislice magnetic resonance elastography sequence was used to collect 3-dimensional vector wave images in a healthy volunteer at 90 Hz. The elastogram from the 3D direct inversion is shown. The mean shear stiffness of the right kidney is 5.8 + 0.34 kPa and the left kidney is 6.1 + 0.42 kPa. 3D: 3-dimensional.
Musculoskeletal
MRE shows promise for the biomechanical analysis of diseased and healthy skeletal muscle[80-89]. It has the potential to characterize neuromuscular diseases and to evaluate treatment efficacy[83,84]. In the assessment of muscle function, MRE shows good correlation with electromyography and is sensitive to age-related changes in muscle mechanical properties[85-87]. Both shear wavelength and tissue stiffness increase with greater muscle loading, while elevated muscle stiffness has been found in patients with neuromuscular disorders[88]. In a study involving 9 patients with active myositis, a significant reduction in muscle stiffness was observed during the relaxation phase in diseased muscles compared with controls[89]. The MRE technique for musculoskeletal assessment can be further extended to a 3T MR system (benefits include shorter examination lengths and superior signal to noise ratio). A study of 16 healthy volunteers by Hong et al[90] showed that MRE at 3T was a feasible technique for assessing shoulder muscle stiffness with good to excellent levels of inter-observer agreement (Figure 9).
Figure 9.
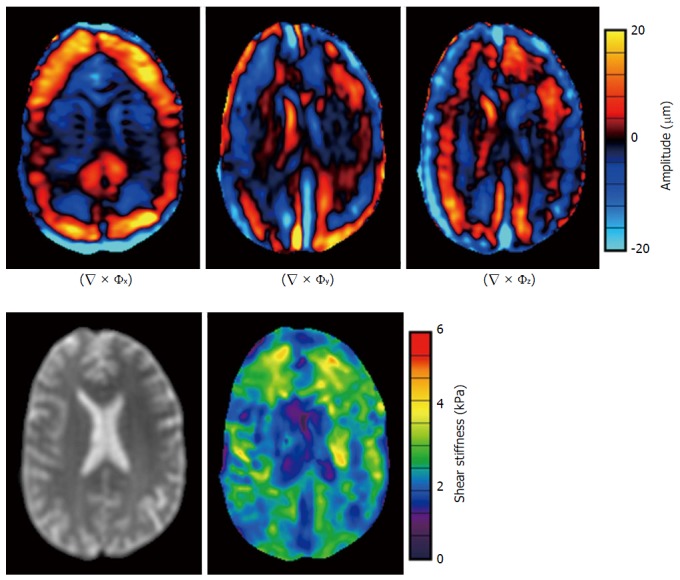
A 39-year-old healthy male volunteer. Axial images of the brain including 60 Hz curl images and the 3D direct inversion elastogram. 3D: 3-dimensional.
Miscellaneous
Early studies suggest that MRE may have a role in evaluating cardiac function (e.g., left ventricular contractility), estimating chamber pressures (e.g., end-diastolic left ventricular pressure) and detecting abnormal ventricular relaxation[91-96]. A few investigators have performed MRE in the pancreas[97], uterus and cervix[98], prostate[99-106], the abdominal aorta[107-110], the lungs[111-115] and the head and neck[116,117]. These early studies should act as a stimulus for further research activity.
LIMITATIONS AND FUTURE DIRECTIONS
Hepatic MRE has limited utility in iron-overload states. On a gradient-echo MRE sequence, parenchymal iron-overload may result in the MRI signal being too low for shear wave detection. This problem can be mitigated by utilizing spin-echo or echo-planar imaging as these sequences are less susceptible to T2* effects. As in conventional MRI, MRE cannot be performed in patients with recognized MRI contraindications (e.g., cardiac pacemakers, cerebral aneurysm clips, cochlear implants, etc.) and may be impractical in patients with claustrophobia. There are also challenges involved in performing MRE in unstable patients given the longer examination times involved and in morbidly obese patients who may have problems fitting into the MRI scanner. It should be noted that the evaluation of parenchymal organ fibrosis may be limited by confounders of increased tissue stiffness. In the liver, alternative causes of elevated stiffness include acute inflammation (e.g., alcohol and viral hepatitis), biliary obstruction, passive hepatic congestion from cardiac failure, and hepatic venous obstruction. In the kidneys, alternative causes of elevated stiffness include renal vein thrombosis, hydronephrosis, renal compression from adjacent peri-renal collections, and possibly hypertension. While early studies suggest that MRE shows promise in differentiating benign from malignant tumors in a variety of organ systems, an overlap in stiffness is a limiting factor and prospective studies involving larger numbers of patients are required for validation.
Future directions involving MRE include (1) improving image quality and reducing acquisition time (e.g., use of echo-planar imaging, parallel imaging, reduced k-space acquisitions, imaging at ≥ 3 T, adoption of sophisticated inversion algorithms, 3D- and multi-frequency techniques, etc.)[118-124]; (2) expanding research into topics beyond fibrosis (e.g., inflammation, necrosis, edema, perfusion, tumor characterization, evaluation of treatment response, etc.)[12,28,125-128]; (3) better defining the pitfalls of MRE and developing novel solutions for overcoming these limitations; and (4) better defining the clinical indications for MRE beyond the research setting. Unquestionably, MRE is an emerging technology with genuine promise but the technique has yet to be fully mapped out and new frontiers exist for exploration.
Footnotes
Supported by National Institutes of Health, No. R01 EB001981; and National Institute of Health Research Cambridge Biomedical Research Centre.
Conflict-of-interest statement: The authors declare no conflict-of-interests for this article.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 1, 2015
First decision: November 6, 2015
Article in press: December 4, 2015
P- Reviewer: Cerwenka HR, Lassandro F
S- Editor: Qi Y L- Editor: A E- Editor: Li D
References
- 1.Sarvazyan A, Hall TJ, Urban MW, Fatemi M, Aglyamov SR, Garra BS. An overview of elastography - an emerging branch of medical imaging. Curr Med Imaging Rev. 2011;7:255–282. doi: 10.2174/157340511798038684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manduca A, Oliphant TE, Dresner MA, Mahowald JL, Kruse SA, Amromin E, Felmlee JP, Greenleaf JF, Ehman RL. Magnetic resonance elastography: non-invasive mapping of tissue elasticity. Med Image Anal. 2001;5:237–254. doi: 10.1016/s1361-8415(00)00039-6. [DOI] [PubMed] [Google Scholar]
- 3.Gao L, Parker KJ, Lerner RM, Levinson SF. Imaging of the elastic properties of tissue--a review. Ultrasound Med Biol. 1996;22:959–977. doi: 10.1016/s0301-5629(96)00120-2. [DOI] [PubMed] [Google Scholar]
- 4.Parker KJ, Doyley MM, Rubens DJ. Imaging the elastic properties of tissue: the 20 year perspective. Phys Med Biol. 2011;56:R1–R29. doi: 10.1088/0031-9155/56/1/R01. [DOI] [PubMed] [Google Scholar]
- 5.Vappou J. Magnetic resonance- and ultrasound imaging-based elasticity imaging methods: a review. Crit Rev Biomed Eng. 2012;40:121–134. doi: 10.1615/critrevbiomedeng.v40.i2.30. [DOI] [PubMed] [Google Scholar]
- 6.Wells PN, Liang HD. Medical ultrasound: imaging of soft tissue strain and elasticity. J R Soc Interface. 2011;8:1521–1549. doi: 10.1098/rsif.2011.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goss SA, Johnston RL, Dunn F. Comprehensive compilation of empirical ultrasonic properties of mammalian tissues. J Acoust Soc Am. 1978;64:423–457. doi: 10.1121/1.382016. [DOI] [PubMed] [Google Scholar]
- 8.Muthupillai R, Lomas DJ, Rossman PJ, Greenleaf JF, Manduca A, Ehman RL. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science. 1995;269:1854–1857. doi: 10.1126/science.7569924. [DOI] [PubMed] [Google Scholar]
- 9.Chenevert TL, Skovoroda AR, O’Donnell M, Emelianov SY. Elasticity reconstructive imaging by means of stimulated echo MRI. Magn Reson Med. 1998;39:482–490. doi: 10.1002/mrm.1910390319. [DOI] [PubMed] [Google Scholar]
- 10.Plewes DB, Betty I, Urchuk SN, Soutar I. Visualizing tissue compliance with MR imaging. J Magn Reson Imaging. 1995;5:733–738. doi: 10.1002/jmri.1880050620. [DOI] [PubMed] [Google Scholar]
- 11.Osman NF. Detecting stiff masses using strain-encoded (SENC) imaging. Magn Reson Med. 2003;49:605–608. doi: 10.1002/mrm.10376. [DOI] [PubMed] [Google Scholar]
- 12.Venkatesh SK, Yin M, Ehman RL. Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging. 2013;37:544–555. doi: 10.1002/jmri.23731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm RC, Rossman PJ, Fidler JL, Ehman RL. Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol. 2007;5:1207–1213.e2. doi: 10.1016/j.cgh.2007.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rouvière O, Yin M, Dresner MA, Rossman PJ, Burgart LJ, Fidler JL, Ehman RL. MR elastography of the liver: preliminary results. Radiology. 2006;240:440–448. doi: 10.1148/radiol.2402050606. [DOI] [PubMed] [Google Scholar]
- 15.Uffmann K, Ladd ME. Actuation systems for MR elastography: design and applications. IEEE Eng Med Biol Mag. 2008;27:28–34. doi: 10.1109/EMB.2007.910268. [DOI] [PubMed] [Google Scholar]
- 16.Di Ieva A, Grizzi F, Rognone E, Tse ZT, Parittotokkaporn T, Rodriguez Y Baena F, Tschabitscher M, Matula C, Trattnig S, Rodriguez Y Baena R. Magnetic resonance elastography: a general overview of its current and future applications in brain imaging. Neurosurg Rev. 2010;33:137–145; discussion 145. doi: 10.1007/s10143-010-0249-6. [DOI] [PubMed] [Google Scholar]
- 17.Yin M, Chen J, Glaser KJ, Talwalkar JA, Ehman RL. Abdominal magnetic resonance elastography. Top Magn Reson Imaging. 2009;20:79–87. doi: 10.1097/RMR.0b013e3181c4737e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huwart L, Peeters F, Sinkus R, Annet L, Salameh N, ter Beek LC, Horsmans Y, Van Beers BE. Liver fibrosis: non-invasive assessment with MR elastography. NMR Biomed. 2006;19:173–179. doi: 10.1002/nbm.1030. [DOI] [PubMed] [Google Scholar]
- 19.Huwart L, Sempoux C, Salameh N, Jamart J, Annet L, Sinkus R, Peeters F, ter Beek LC, Horsmans Y, Van Beers BE. Liver fibrosis: noninvasive assessment with MR elastography versus aspartate aminotransferase-to-platelet ratio index. Radiology. 2007;245:458–466. doi: 10.1148/radiol.2452061673. [DOI] [PubMed] [Google Scholar]
- 20.Huwart L, Sempoux C, Vicaut E, Salameh N, Annet L, Danse E, Peeters F, ter Beek LC, Rahier J, Sinkus R, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology. 2008;135:32–40. doi: 10.1053/j.gastro.2008.03.076. [DOI] [PubMed] [Google Scholar]
- 21.Godfrey EM, Patterson AJ, Priest AN, Davies SE, Joubert I, Krishnan AS, Griffin N, Shaw AS, Alexander GJ, Allison ME, et al. A comparison of MR elastography and 31P MR spectroscopy with histological staging of liver fibrosis. Eur Radiol. 2012;22:2790–2797. doi: 10.1007/s00330-012-2527-x. [DOI] [PubMed] [Google Scholar]
- 22.Singh S, Venkatesh SK, Wang Z, Miller FH, Motosugi U, Low RN, Hassanein T, Asbach P, Godfrey EM, Yin M, et al. Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol. 2015;13:440–451.e6. doi: 10.1016/j.cgh.2014.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su LN, Guo SL, Li BX, Yang P. Diagnostic value of magnetic resonance elastography for detecting and staging of hepatic fibrosis: a meta-analysis. Clin Radiol. 2014;69:e545–e552. doi: 10.1016/j.crad.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Lee VS, Miller FH, Omary RA, Wang Y, Ganger DR, Wang E, Rao S, Levitsky J. Magnetic resonance elastography and biomarkers to assess fibrosis from recurrent hepatitis C in liver transplant recipients. Transplantation. 2011;92:581–586. doi: 10.1097/TP.0b013e31822805fa. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Ganger DR, Levitsky J, Sternick LA, McCarthy RJ, Chen ZE, Fasanati CW, Bolster B, Shah S, Zuehlsdorff S, et al. Assessment of chronic hepatitis and fibrosis: comparison of MR elastography and diffusion-weighted imaging. AJR Am J Roentgenol. 2011;196:553–561. doi: 10.2214/AJR.10.4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rustogi R, Horowitz J, Harmath C, Wang Y, Chalian H, Ganger DR, Chen ZE, Bolster BD, Shah S, Miller FH. Accuracy of MR elastography and anatomic MR imaging features in the diagnosis of severe hepatic fibrosis and cirrhosis. J Magn Reson Imaging. 2012;35:1356–1364. doi: 10.1002/jmri.23585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park HS, Kim YJ, Yu MH, Choe WH, Jung SI, Jeon HJ. Three-Tesla magnetic resonance elastography for hepatic fibrosis: comparison with diffusion-weighted imaging and gadoxetic acid-enhanced magnetic resonance imaging. World J Gastroenterol. 2014;20:17558–17567. doi: 10.3748/wjg.v20.i46.17558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J, Talwalkar JA, Yin M, Glaser KJ, Sanderson SO, Ehman RL. Early detection of nonalcoholic steatohepatitis in patients with nonalcoholic fatty liver disease by using MR elastography. Radiology. 2011;259:749–756. doi: 10.1148/radiol.11101942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Loomba R, Wolfson T, Ang B, Hooker J, Behling C, Peterson M, Valasek M, Lin G, Brenner D, Gamst A, et al. Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: a prospective study. Hepatology. 2014;60:1920–1928. doi: 10.1002/hep.27362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loomba R, Sirlin CB, Ang B, Bettencourt R, Jain R, Salotti J, Soaft L, Hooker J, Kono Y, Bhatt A, et al. Ezetimibe for the treatment of nonalcoholic steatohepatitis: assessment by novel magnetic resonance imaging and magnetic resonance elastography in a randomized trial (MOZART trial) Hepatology. 2015;61:1239–1250. doi: 10.1002/hep.27647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hines CD, Bley TA, Lindstrom MJ, Reeder SB. Repeatability of magnetic resonance elastography for quantification of hepatic stiffness. J Magn Reson Imaging. 2010;31:725–731. doi: 10.1002/jmri.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shire NJ, Yin M, Chen J, Railkar RA, Fox-Bosetti S, Johnson SM, Beals CR, Dardzinski BJ, Sanderson SO, Talwalkar JA, et al. Test-retest repeatability of MR elastography for noninvasive liver fibrosis assessment in hepatitis C. J Magn Reson Imaging. 2011;34:947–955. doi: 10.1002/jmri.22716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hines CD, Lindstrom MJ, Varma AK, Reeder SB. Effects of postprandial state and mesenteric blood flow on the repeatability of MR elastography in asymptomatic subjects. J Magn Reson Imaging. 2011;33:239–244. doi: 10.1002/jmri.22354. [DOI] [PubMed] [Google Scholar]
- 34.Motosugi U, Ichikawa T, Sano K, Sou H, Muhi A, Koshiishi T, Ehman RL, Araki T. Magnetic resonance elastography of the liver: preliminary results and estimation of inter-rater reliability. Jpn J Radiol. 2010;28:623–627. doi: 10.1007/s11604-010-0478-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi Y, Guo Q, Xia F, Sun J, Gao Y. Short- and midterm repeatability of magnetic resonance elastography in healthy volunteers at 3.0 T. Magn Reson Imaging. 2014;32:665–670. doi: 10.1016/j.mri.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 36.Venkatesh SK, Wang G, Teo LL, Ang BW. Magnetic resonance elastography of liver in healthy Asians: normal liver stiffness quantification and reproducibility assessment. J Magn Reson Imaging. 2014;39:1–8. doi: 10.1002/jmri.24084. [DOI] [PubMed] [Google Scholar]
- 37.Serai SD, Yin M, Wang H, Ehman RL, Podberesky DJ. Cross-vendor validation of liver magnetic resonance elastography. Abdom Imaging. 2015;40:789–794. doi: 10.1007/s00261-014-0282-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hallinan JT, Alsaif HS, Wee A, Venkatesh SK. Magnetic resonance elastography of liver: influence of intravenous gadolinium administration on measured liver stiffness. Abdom Imaging. 2015;40:783–788. doi: 10.1007/s00261-014-0275-x. [DOI] [PubMed] [Google Scholar]
- 39.Yin M, Talwalkar JA, Glaser KJ, Venkatesh SK, Chen J, Manduca A, Ehman RL. Dynamic postprandial hepatic stiffness augmentation assessed with MR elastography in patients with chronic liver disease. AJR Am J Roentgenol. 2011;197:64–70. doi: 10.2214/AJR.10.5989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B. Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One. 2014;9:e97355. doi: 10.1371/journal.pone.0097355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perumpail RB, Levitsky J, Wang Y, Lee VS, Karp J, Jin N, Yang GY, Bolster BD, Shah S, Zuehlsdorff S, et al. MRI-guided biopsy to correlate tissue specimens with MR elastography stiffness readings in liver transplants. Acad Radiol. 2012;19:1121–1126. doi: 10.1016/j.acra.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Venkatesh SK, Yin M, Glockner JF, Takahashi N, Araoz PA, Talwalkar JA, Ehman RL. MR elastography of liver tumors: preliminary results. AJR Am J Roentgenol. 2008;190:1534–1540. doi: 10.2214/AJR.07.3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hennedige TP, Hallinan JT, Leung FP, Teo LL, Iyer S, Wang G, Chang S, Madhavan KK, Wee A, Venkatesh SK. Comparison of magnetic resonance elastography and diffusion-weighted imaging for differentiating benign and malignant liver lesions. Eur Radiol. 2015:Epub ahead of print. doi: 10.1007/s00330-015-3835-8. [DOI] [PubMed] [Google Scholar]
- 44.Ichikawa S, Motosugi U, Morisaka H, Sano K, Ichikawa T, Tatsumi A, Enomoto N, Matsuda M, Fujii H, Onishi H. Comparison of the diagnostic accuracies of magnetic resonance elastography and transient elastography for hepatic fibrosis. Magn Reson Imaging. 2015;33:26–30. doi: 10.1016/j.mri.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 45.Yoon JH, Lee JM, Joo I, Lee ES, Sohn JY, Jang SK, Lee KB, Han JK, Choi BI. Hepatic fibrosis: prospective comparison of MR elastography and US shear-wave elastography for evaluation. Radiology. 2014;273:772–782. doi: 10.1148/radiol.14132000. [DOI] [PubMed] [Google Scholar]
- 46.Mannelli L, Godfrey E, Joubert I, Patterson AJ, Graves MJ, Gallagher FA, Lomas DJ. MR elastography: Spleen stiffness measurements in healthy volunteers--preliminary experience. AJR Am J Roentgenol. 2010;195:387–392. doi: 10.2214/AJR.09.3390. [DOI] [PubMed] [Google Scholar]
- 47.Talwalkar JA, Yin M, Venkatesh S, Rossman PJ, Grimm RC, Manduca A, Romano A, Kamath PS, Ehman RL. Feasibility of in vivo MR elastographic splenic stiffness measurements in the assessment of portal hypertension. AJR Am J Roentgenol. 2009;193:122–127. doi: 10.2214/AJR.07.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shin SU, Lee JM, Yu MH, Yoon JH, Han JK, Choi BI, Glaser KJ, Ehman RL. Prediction of esophageal varices in patients with cirrhosis: usefulness of three-dimensional MR elastography with echo-planar imaging technique. Radiology. 2014;272:143–153. doi: 10.1148/radiol.14130916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guo J, Büning C, Schott E, Kröncke T, Braun J, Sack I, Althoff C. In vivo abdominal magnetic resonance elastography for the assessment of portal hypertension before and after transjugular intrahepatic portosystemic shunt implantation. Invest Radiol. 2015;50:347–351. doi: 10.1097/RLI.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 50.Ronot M, Lambert S, Elkrief L, Doblas S, Rautou PE, Castera L, Vilgrain V, Sinkus R, Van Beers BE, Garteiser P. Assessment of portal hypertension and high-risk oesophageal varices with liver and spleen three-dimensional multifrequency MR elastography in liver cirrhosis. Eur Radiol. 2014;24:1394–1402. doi: 10.1007/s00330-014-3124-y. [DOI] [PubMed] [Google Scholar]
- 51.Low G, Owen NE, Joubert I, Patterson AJ, Graves MJ, Glaser KJ, Alexander GJ, Lomas DJ. Reliability of magnetic resonance elastography using multislice two-dimensional spin-echo echo-planar imaging (SE-EPI) and three-dimensional inversion reconstruction for assessing renal stiffness. J Magn Reson Imaging. 2015;42:844–850. doi: 10.1002/jmri.24826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rouvière O, Souchon R, Pagnoux G, Ménager JM, Chapelon JY. Magnetic resonance elastography of the kidneys: feasibility and reproducibility in young healthy adults. J Magn Reson Imaging. 2011;34:880–886. doi: 10.1002/jmri.22670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee CU, Glockner JF, Glaser KJ, Yin M, Chen J, Kawashima A, Kim B, Kremers WK, Ehman RL, Gloor JM. MR elastography in renal transplant patients and correlation with renal allograft biopsy: a feasibility study. Acad Radiol. 2012;19:834–841. doi: 10.1016/j.acra.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Low G, Owen NE, Joubert I, Patterson AJ, Graves MJ, Alexander GJ, Lomas DJ. Magnetic resonance elastography in the detection of hepatorenal syndrome in patients with cirrhosis and ascites. Eur Radiol. 2015;25:2851–2858. doi: 10.1007/s00330-015-3723-2. [DOI] [PubMed] [Google Scholar]
- 55.Lorenzen J, Sinkus R, Lorenzen M, Dargatz M, Leussler C, Röschmann P, Adam G. MR elastography of the breast: preliminary clinical results. Rofo. 2002;174:830–834. doi: 10.1055/s-2002-32690. [DOI] [PubMed] [Google Scholar]
- 56.Sinkus R, Siegmann K, Xydeas T, Tanter M, Claussen C, Fink M. MR elastography of breast lesions: understanding the solid/liquid duality can improve the specificity of contrast-enhanced MR mammography. Magn Reson Med. 2007;58:1135–1144. doi: 10.1002/mrm.21404. [DOI] [PubMed] [Google Scholar]
- 57.Xydeas T, Siegmann K, Sinkus R, Krainick-Strobel U, Miller S, Claussen CD. Magnetic resonance elastography of the breast: correlation of signal intensity data with viscoelastic properties. Invest Radiol. 2005;40:412–420. doi: 10.1097/01.rli.0000166940.72971.4a. [DOI] [PubMed] [Google Scholar]
- 58.Sinkus R, Tanter M, Xydeas T, Catheline S, Bercoff J, Fink M. Viscoelastic shear properties of in vivo breast lesions measured by MR elastography. Magn Reson Imaging. 2005;23:159–165. doi: 10.1016/j.mri.2004.11.060. [DOI] [PubMed] [Google Scholar]
- 59.Sinkus R, Tanter M, Catheline S, Lorenzen J, Kuhl C, Sondermann E, Fink M. Imaging anisotropic and viscous properties of breast tissue by magnetic resonance-elastography. Magn Reson Med. 2005;53:372–387. doi: 10.1002/mrm.20355. [DOI] [PubMed] [Google Scholar]
- 60.Lorenzen J, Sinkus R, Biesterfeldt M, Adam G. Menstrual-cycle dependence of breast parenchyma elasticity: estimation with magnetic resonance elastography of breast tissue during the menstrual cycle. Invest Radiol. 2003;38:236–240. doi: 10.1097/01.RLI.0000059544.18910.BD. [DOI] [PubMed] [Google Scholar]
- 61.McKnight AL, Kugel JL, Rossman PJ, Manduca A, Hartmann LC, Ehman RL. MR elastography of breast cancer: preliminary results. AJR Am J Roentgenol. 2002;178:1411–1417. doi: 10.2214/ajr.178.6.1781411. [DOI] [PubMed] [Google Scholar]
- 62.Lorenzen J, Sinkus R, Schrader D, Lorenzen M, Leussler C, Dargatz M, Röschmann P. [Imaging of breast tumors using MR elastography] Rofo. 2001;173:12–17. doi: 10.1055/s-2001-10233. [DOI] [PubMed] [Google Scholar]
- 63.Sinkus R, Lorenzen J, Schrader D, Lorenzen M, Dargatz M, Holz D. High-resolution tensor MR elastography for breast tumour detection. Phys Med Biol. 2000;45:1649–1664. doi: 10.1088/0031-9155/45/6/317. [DOI] [PubMed] [Google Scholar]
- 64.Plewes DB, Bishop J, Samani A, Sciarretta J. Visualization and quantification of breast cancer biomechanical properties with magnetic resonance elastography. Phys Med Biol. 2000;45:1591–1610. doi: 10.1088/0031-9155/45/6/314. [DOI] [PubMed] [Google Scholar]
- 65.Siegmann KC, Xydeas T, Sinkus R, Kraemer B, Vogel U, Claussen CD. Diagnostic value of MR elastography in addition to contrast-enhanced MR imaging of the breast-initial clinical results. Eur Radiol. 2010;20:318–325. doi: 10.1007/s00330-009-1566-4. [DOI] [PubMed] [Google Scholar]
- 66.Zhang J, Green MA, Sinkus R, Bilston LE. Viscoelastic properties of human cerebellum using magnetic resonance elastography. J Biomech. 2011;44:1909–1913. doi: 10.1016/j.jbiomech.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 67.Green MA, Bilston LE, Sinkus R. In vivo brain viscoelastic properties measured by magnetic resonance elastography. NMR Biomed. 2008;21:755–764. doi: 10.1002/nbm.1254. [DOI] [PubMed] [Google Scholar]
- 68.Kruse SA, Rose GH, Glaser KJ, Manduca A, Felmlee JP, Jack CR, Ehman RL. Magnetic resonance elastography of the brain. Neuroimage. 2008;39:231–237. doi: 10.1016/j.neuroimage.2007.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xu L, Lin Y, Xi ZN, Shen H, Gao PY. Magnetic resonance elastography of the human brain: a preliminary study. Acta Radiol. 2007;48:112–115. doi: 10.1080/02841850601026401. [DOI] [PubMed] [Google Scholar]
- 70.Wuerfel J, Paul F, Beierbach B, Hamhaber U, Klatt D, Papazoglou S, Zipp F, Martus P, Braun J, Sack I. MR-elastography reveals degradation of tissue integrity in multiple sclerosis. Neuroimage. 2010;49:2520–2525. doi: 10.1016/j.neuroimage.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 71.Streitberger KJ, Sack I, Krefting D, Pfüller C, Braun J, Paul F, Wuerfel J. Brain viscoelasticity alteration in chronic-progressive multiple sclerosis. PLoS One. 2012;7:e29888. doi: 10.1371/journal.pone.0029888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schregel K, Wuerfel E, Garteiser P, Gemeinhardt I, Prozorovski T, Aktas O, Merz H, Petersen D, Wuerfel J, Sinkus R. Demyelination reduces brain parenchymal stiffness quantified in vivo by magnetic resonance elastography. Proc Natl Acad Sci USA. 2012;109:6650–6655. doi: 10.1073/pnas.1200151109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Murphy MC, Huston J, Jack CR, Glaser KJ, Manduca A, Felmlee JP, Ehman RL. Decreased brain stiffness in Alzheimer’s disease determined by magnetic resonance elastography. J Magn Reson Imaging. 2011;34:494–498. doi: 10.1002/jmri.22707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sack I, Streitberger KJ, Krefting D, Paul F, Braun J. The influence of physiological aging and atrophy on brain viscoelastic properties in humans. PLoS One. 2011;6:e23451. doi: 10.1371/journal.pone.0023451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boulet T, Kelso ML, Othman SF. Microscopic magnetic resonance elastography of traumatic brain injury model. J Neurosci Methods. 2011;201:296–306. doi: 10.1016/j.jneumeth.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 76.Freimann FB, Streitberger KJ, Klatt D, Lin K, McLaughlin J, Braun J, Sprung C, Sack I. Alteration of brain viscoelasticity after shunt treatment in normal pressure hydrocephalus. Neuroradiology. 2012;54:189–196. doi: 10.1007/s00234-011-0871-1. [DOI] [PubMed] [Google Scholar]
- 77.Murphy MC, Huston J, Glaser KJ, Manduca A, Meyer FB, Lanzino G, Morris JM, Felmlee JP, Ehman RL. Preoperative assessment of meningioma stiffness using magnetic resonance elastography. J Neurosurg. 2013;118:643–648. doi: 10.3171/2012.9.JNS12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xu L, Lin Y, Han JC, Xi ZN, Shen H, Gao PY. Magnetic resonance elastography of brain tumors: preliminary results. Acta Radiol. 2007;48:327–330. doi: 10.1080/02841850701199967. [DOI] [PubMed] [Google Scholar]
- 79.Reiss-Zimmermann M, Streitberger KJ, Sack I, Braun J, Arlt F, Fritzsch D, Hoffmann KT. High Resolution Imaging of Viscoelastic Properties of Intracranial Tumours by Multi-Frequency Magnetic Resonance Elastography. Clin Neuroradiol. 2014:Epub ahead of print. doi: 10.1007/s00062-014-0311-9. [DOI] [PubMed] [Google Scholar]
- 80.Jenkyn TR, Ehman RL, An KN. Noninvasive muscle tension measurement using the novel technique of magnetic resonance elastography (MRE) J Biomech. 2003;36:1917–1921. doi: 10.1016/s0021-9290(03)00005-8. [DOI] [PubMed] [Google Scholar]
- 81.Ringleb SI, Bensamoun SF, Chen Q, Manduca A, An KN, Ehman RL. Applications of magnetic resonance elastography to healthy and pathologic skeletal muscle. J Magn Reson Imaging. 2007;25:301–309. doi: 10.1002/jmri.20817. [DOI] [PubMed] [Google Scholar]
- 82.Debernard L, Robert L, Charleux F, Bensamoun SF. A possible clinical tool to depict muscle elasticity mapping using magnetic resonance elastography. Muscle Nerve. 2013;47:903–908. doi: 10.1002/mus.23678. [DOI] [PubMed] [Google Scholar]
- 83.Bensamoun SF, Ringleb SI, Chen Q, Ehman RL, An KN, Brennan M. Thigh muscle stiffness assessed with magnetic resonance elastography in hyperthyroid patients before and after medical treatment. J Magn Reson Imaging. 2007;26:708–713. doi: 10.1002/jmri.21073. [DOI] [PubMed] [Google Scholar]
- 84.Brauck K, Galbán CJ, Maderwald S, Herrmann BL, Ladd ME. Changes in calf muscle elasticity in hypogonadal males before and after testosterone substitution as monitored by magnetic resonance elastography. Eur J Endocrinol. 2007;156:673–678. doi: 10.1530/EJE-06-0694. [DOI] [PubMed] [Google Scholar]
- 85.Heers G, Jenkyn T, Dresner MA, Klein MO, Basford JR, Kaufman KR, Ehman RL, An KN. Measurement of muscle activity with magnetic resonance elastography. Clin Biomech (Bristol, Avon) 2003;18:537–542. doi: 10.1016/s0268-0033(03)00070-6. [DOI] [PubMed] [Google Scholar]
- 86.Debernard L, Robert L, Charleux F, Bensamoun SF. Analysis of thigh muscle stiffness from childhood to adulthood using magnetic resonance elastography (MRE) technique. Clin Biomech (Bristol, Avon) 2011;26:836–840. doi: 10.1016/j.clinbiomech.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 87.Domire ZJ, McCullough MB, Chen Q, An KN. Feasibility of using magnetic resonance elastography to study the effect of aging on shear modulus of skeletal muscle. J Appl Biomech. 2009;25:93–97. doi: 10.1123/jab.25.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Basford JR, Jenkyn TR, An KN, Ehman RL, Heers G, Kaufman KR. Evaluation of healthy and diseased muscle with magnetic resonance elastography. Arch Phys Med Rehabil. 2002;83:1530–1536. doi: 10.1053/apmr.2002.35472. [DOI] [PubMed] [Google Scholar]
- 89.McCullough MB, Domire ZJ, Reed AM, Amin S, Ytterberg SR, Chen Q, An KN. Evaluation of muscles affected by myositis using magnetic resonance elastography. Muscle Nerve. 2011;43:585–590. doi: 10.1002/mus.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hong SH, Hong SJ, Yoon JS, Oh CH, Cha JG, Kim HK, Bolster B Jr. Magnetic resonance elastography (MRE) for measurement of muscle stiffness of the shoulder: feasibility with a 3 T MRI system. Acta Radiol. 2015:Epub ahead of print. doi: 10.1177/0284185115571987. [DOI] [PubMed] [Google Scholar]
- 91.Kolipaka A, Aggarwal SR, McGee KP, Anavekar N, Manduca A, Ehman RL, Araoz PA. Magnetic resonance elastography as a method to estimate myocardial contractility. J Magn Reson Imaging. 2012;36:120–127. doi: 10.1002/jmri.23616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kolipaka A, McGee KP, Manduca A, Anavekar N, Ehman RL, Araoz PA. In vivo assessment of MR elastography-derived effective end-diastolic myocardial stiffness under different loading conditions. J Magn Reson Imaging. 2011;33:1224–1228. doi: 10.1002/jmri.22531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Elgeti T, Beling M, Hamm B, Braun J, Sack I. Cardiac magnetic resonance elastography: toward the diagnosis of abnormal myocardial relaxation. Invest Radiol. 2010;45:782–787. doi: 10.1097/RLI.0b013e3181ec4b63. [DOI] [PubMed] [Google Scholar]
- 94.Elgeti T, Laule M, Kaufels N, Schnorr J, Hamm B, Samani A, Braun J, Sack I. Cardiac MR elastography: comparison with left ventricular pressure measurement. J Cardiovasc Magn Reson. 2009;11:44. doi: 10.1186/1532-429X-11-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Elgeti T, Rump J, Hamhaber U, Papazoglou S, Hamm B, Braun J, Sack I. Cardiac magnetic resonance elastography. Initial results. Invest Radiol. 2008;43:762–772. doi: 10.1097/RLI.0b013e3181822085. [DOI] [PubMed] [Google Scholar]
- 96.Sack I, Rump J, Elgeti T, Samani A, Braun J. MR elastography of the human heart: noninvasive assessment of myocardial elasticity changes by shear wave amplitude variations. Magn Reson Med. 2009;61:668–677. doi: 10.1002/mrm.21878. [DOI] [PubMed] [Google Scholar]
- 97.Shi Y, Glaser KJ, Venkatesh SK, Ben-Abraham EI, Ehman RL. Feasibility of using 3D MR elastography to determine pancreatic stiffness in healthy volunteers. J Magn Reson Imaging. 2015;41:369–375. doi: 10.1002/jmri.24572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jiang X, Asbach P, Streitberger KJ, Thomas A, Hamm B, Braun J, Sack I, Guo J. In vivo high-resolution magnetic resonance elastography of the uterine corpus and cervix. Eur Radiol. 2014;24:3025–3033. doi: 10.1007/s00330-014-3305-8. [DOI] [PubMed] [Google Scholar]
- 99.Arani A, Plewes D, Krieger A, Chopra R. The feasibility of endorectal MR elastography for prostate cancer localization. Magn Reson Med. 2011;66:1649–1657. doi: 10.1002/mrm.22967. [DOI] [PubMed] [Google Scholar]
- 100.Thörmer G, Reiss-Zimmermann M, Otto J, Hoffmann KT, Moche M, Garnov N, Kahn T, Busse H. Novel technique for MR elastography of the prostate using a modified standard endorectal coil as actuator. J Magn Reson Imaging. 2013;37:1480–1485. doi: 10.1002/jmri.23850. [DOI] [PubMed] [Google Scholar]
- 101.Sahebjavaher RS, Baghani A, Honarvar M, Sinkus R, Salcudean SE. Transperineal prostate MR elastography: initial in vivo results. Magn Reson Med. 2013;69:411–420. doi: 10.1002/mrm.24268. [DOI] [PubMed] [Google Scholar]
- 102.Arani A, Da Rosa M, Ramsay E, Plewes DB, Haider MA, Chopra R. Incorporating endorectal MR elastography into multi-parametric MRI for prostate cancer imaging: Initial feasibility in volunteers. J Magn Reson Imaging. 2013;38:1251–1260. doi: 10.1002/jmri.24028. [DOI] [PubMed] [Google Scholar]
- 103.Li S, Chen M, Wang W, Zhao W, Wang J, Zhao X, Zhou C. A feasibility study of MR elastography in the diagnosis of prostate cancer at 3.0T. Acta Radiol. 2011;52:354–358. doi: 10.1258/ar.2010.100276. [DOI] [PubMed] [Google Scholar]
- 104.Arani A, Plewes D, Chopra R. Transurethral prostate magnetic resonance elastography: prospective imaging requirements. Magn Reson Med. 2011;65:340–349. doi: 10.1002/mrm.22633. [DOI] [PubMed] [Google Scholar]
- 105.Chopra R, Arani A, Huang Y, Musquera M, Wachsmuth J, Bronskill M, Plewes D. In vivo MR elastography of the prostate gland using a transurethral actuator. Magn Reson Med. 2009;62:665–671. doi: 10.1002/mrm.22038. [DOI] [PubMed] [Google Scholar]
- 106.Kemper J, Sinkus R, Lorenzen J, Nolte-Ernsting C, Stork A, Adam G. MR elastography of the prostate: initial in-vivo application. Rofo. 2004;176:1094–1099. doi: 10.1055/s-2004-813279. [DOI] [PubMed] [Google Scholar]
- 107.Kolipaka A, Woodrum D, Araoz PA, Ehman RL. MR elastography of the in vivo abdominal aorta: a feasibility study for comparing aortic stiffness between hypertensives and normotensives. J Magn Reson Imaging. 2012;35:582–586. doi: 10.1002/jmri.22866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Woodrum DA, Herrmann J, Lerman A, Romano AJ, Lerman LO, Ehman RL. Phase-contrast MRI-based elastography technique detects early hypertensive changes in ex vivo porcine aortic wall. J Magn Reson Imaging. 2009;29:583–587. doi: 10.1002/jmri.21702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu L, Chen J, Glaser KJ, Yin M, Rossman PJ, Ehman RL. MR elastography of the human abdominal aorta: a preliminary study. J Magn Reson Imaging. 2013;38:1549–1553. doi: 10.1002/jmri.24056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Damughatla AR, Raterman B, Sharkey-Toppen T, Jin N, Simonetti OP, White RD, Kolipaka A. Quantification of aortic stiffness using MR elastography and its comparison to MRI-based pulse wave velocity. J Magn Reson Imaging. 2015;41:44–51. doi: 10.1002/jmri.24506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mariappan YK, Kolipaka A, Manduca A, Hubmayr RD, Ehman RL, Araoz P, McGee KP. Magnetic resonance elastography of the lung parenchyma in an in situ porcine model with a noninvasive mechanical driver: correlation of shear stiffness with trans-respiratory system pressures. Magn Reson Med. 2012;67:210–217. doi: 10.1002/mrm.22976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mariappan YK, Glaser KJ, Hubmayr RD, Manduca A, Ehman RL, McGee KP. MR elastography of human lung parenchyma: technical development, theoretical modeling and in vivo validation. J Magn Reson Imaging. 2011;33:1351–1361. doi: 10.1002/jmri.22550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.McGee KP, Hubmayr RD, Levin D, Ehman RL. Feasibility of quantifying the mechanical properties of lung parenchyma in a small-animal model using (1)H magnetic resonance elastography (MRE) J Magn Reson Imaging. 2009;29:838–845. doi: 10.1002/jmri.21720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.McGee KP, Hubmayr RD, Ehman RL. MR elastography of the lung with hyperpolarized 3He. Magn Reson Med. 2008;59:14–18. doi: 10.1002/mrm.21465. [DOI] [PubMed] [Google Scholar]
- 115.Goss BC, McGee KP, Ehman EC, Manduca A, Ehman RL. Magnetic resonance elastography of the lung: technical feasibility. Magn Reson Med. 2006;56:1060–1066. doi: 10.1002/mrm.21053. [DOI] [PubMed] [Google Scholar]
- 116.Yeung DK, Bhatia KS, Lee YY, King AD, Garteiser P, Sinkus R, Ahuja AT. MR elastography of the head and neck: driver design and initial results. Magn Reson Imaging. 2013;31:624–629. doi: 10.1016/j.mri.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 117.Bahn MM, Brennan MD, Bahn RS, Dean DS, Kugel JL, Ehman RL. Development and application of magnetic resonance elastography of the normal and pathological thyroid gland in vivo. J Magn Reson Imaging. 2009;30:1151–1154. doi: 10.1002/jmri.21963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Huwart L, Salameh N, ter Beek L, Vicaut E, Peeters F, Sinkus R, Van Beers BE. MR elastography of liver fibrosis: preliminary results comparing spin-echo and echo-planar imaging. Eur Radiol. 2008;18:2535–2541. doi: 10.1007/s00330-008-1051-5. [DOI] [PubMed] [Google Scholar]
- 119.Herzka DA, Kotys MS, Sinkus R, Pettigrew RI, Gharib AM. Magnetic resonance elastography in the liver at 3 Tesla using a second harmonic approach. Magn Reson Med. 2009;62:284–291. doi: 10.1002/mrm.21956. [DOI] [PubMed] [Google Scholar]
- 120.Hamhaber U, Klatt D, Papazoglou S, Hollmann M, Stadler J, Sack I, Bernarding J, Braun J. In vivo magnetic resonance elastography of human brain at 7 T and 1.5 T. J Magn Reson Imaging. 2010;32:577–583. doi: 10.1002/jmri.22294. [DOI] [PubMed] [Google Scholar]
- 121.Papazoglou S, Hirsch S, Braun J, Sack I. Multifrequency inversion in magnetic resonance elastography. Phys Med Biol. 2012;57:2329–2346. doi: 10.1088/0031-9155/57/8/2329. [DOI] [PubMed] [Google Scholar]
- 122.Asbach P, Klatt D, Hamhaber U, Braun J, Somasundaram R, Hamm B, Sack I. Assessment of liver viscoelasticity using multifrequency MR elastography. Magn Reson Med. 2008;60:373–379. doi: 10.1002/mrm.21636. [DOI] [PubMed] [Google Scholar]
- 123.Asbach P, Klatt D, Schlosser B, Biermer M, Muche M, Rieger A, Loddenkemper C, Somasundaram R, Berg T, Hamm B, et al. Viscoelasticity-based staging of hepatic fibrosis with multifrequency MR elastography. Radiology. 2010;257:80–86. doi: 10.1148/radiol.10092489. [DOI] [PubMed] [Google Scholar]
- 124.Van Houten EE, Miga MI, Weaver JB, Kennedy FE, Paulsen KD. Three-dimensional subzone-based reconstruction algorithm for MR elastography. Magn Reson Med. 2001;45:827–837. doi: 10.1002/mrm.1111. [DOI] [PubMed] [Google Scholar]
- 125.Millonig G, Friedrich S, Adolf S, Fonouni H, Golriz M, Mehrabi A, Stiefel P, Pöschl G, Büchler MW, Seitz HK, et al. Liver stiffness is directly influenced by central venous pressure. J Hepatol. 2010;52:206–210. doi: 10.1016/j.jhep.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 126.Sagir A, Erhardt A, Schmitt M, Häussinger D. Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology. 2008;47:592–595. doi: 10.1002/hep.22056. [DOI] [PubMed] [Google Scholar]
- 127.Lebray P, Varnous S, Charlotte F, Varaut A, Poynard T, Ratziu V. Liver stiffness is an unreliable marker of liver fibrosis in patients with cardiac insufficiency. Hepatology. 2008;48:2089. doi: 10.1002/hep.22594. [DOI] [PubMed] [Google Scholar]
- 128.Warner L, Yin M, Glaser KJ, Woollard JA, Carrascal CA, Korsmo MJ, Crane JA, Ehman RL, Lerman LO. Noninvasive In vivo assessment of renal tissue elasticity during graded renal ischemia using MR elastography. Invest Radiol. 2011;46:509–514. doi: 10.1097/RLI.0b013e3182183a95. [DOI] [PMC free article] [PubMed] [Google Scholar]