Abstract
Acute coronary syndrome (ACS) is a term for a range of clinical signs and symptoms suggestive of myocardial ischemia. It results in functional and structural changes and ultimately releasing protein from injured cardiomyocytes. These cardiac markers play a major role in diagnosis and prognosis of ACS. This study aims to assess the efficacy of heart type fatty acid binding protein (h-FABP) as a marker for ACS along with the routinely used hs-TropT. In our observational study, plasma h-FABP (cut-off 6.32 ng/ml) and routinely done hs-Trop T (cutoff 0.1 and 0.014 ng/ml) were estimated by immunometric laboratory assays in 88 patients with acute chest pain. Based on the clinical and laboratory test findings the patients were grouped into ACS (n = 41) and non-ACS (n = 47). The diagnostic sensitivity, specificity, NPV, PPV and ROC curve at 95 % CI were determined. Sensitivity of hs-TropT (0.1 ng/ml), hs-TropT (0.014 ng/ml) and h-FABP were 53, 86 and 78 % respectively and specificity for the same were 98, 73 and 70 % respectively. Sensitivity, specificity and NPV calculated for a cut-off combination of hs-TropT 0.014 ng/ml and h-FABP was 100, 51 and 100 % respectively. These results were substantiated by ROC analysis. Measurement of plasma h-FABP and hs-TropT together on admission appears to be more precise predictor of ACS rather than either hs-Trop T or h-FABP.
Keywords: Acute coronary syndrome, Heart type fatty acid binding protein (h-FABP), High sensitive Troponin T (hs-TropT), Cardiac markers
Introduction
Acute coronary syndrome (ACS) refers to a constellation of clinical symptoms caused by acute myocardial ischemia. Patients with ACS are subdivided into two major categories based on the 12-lead electrocardiogram (ECG) at presentation, those with ST-elevation myocardial infarction (STEMI) and those who present with ST-segment depression, T-wave changes, or no ECG abnormalities (non-ST elevation ACS, NSTEACS). The latter term NSTEACS includes both unstable angina and non-ST elevation myocardial infarction (NSTEMI) [1], which can be detected through biomarkers for myocardial necrosis.
Myocardial necrosis is accompanied by the release of structural proteins and other intracellular macromolecules into the cardiac interstitium as a result of compromise of the integrity of cellular membranes [1]. Biomarkers of myocardial necrosis include cardiac Troponin I and T (TropI and TropT), creatine phosphokinase and isoenzymes, heart type fatty acid binding protein (h-FABP) [2] and myoglobin [3]. Currently, on the basis of improved sensitivity and superior tissue-specificity compared with the other available biomarkers of necrosis, troponins are the preferred biomarker for the detection of myocardial injury [4]. Troponins typically increase more than 20 times above the upper limit of the reference range in myocardial infarction (MI) as compared to creatine kinase MB (CKMB) which usually increases ten times above the reference range. The troponins begin to elevate 3 h from the onset of chest pain in MI. And because of the continuous release, troponin elevation persists for days. This prolonged course with troponin is advantageous for the late diagnosis of MI; however, it limits the diagnosis of early infarction [2].
Fatty acid binding proteins (FABP) are small (12–15 kDa) cytoplasmic proteins that have diverse tissue distribution and concentration in different organs, diverse isoelectric point (PI), binding capacity and binding specificity [5]. These are abundantly expressed in tissues with an active fatty acid metabolism such as heart and liver. The primary function of FABP is facilitation of intracellular long-chain fatty acid transport [6]. Heart-type fatty acid-binding protein (h-FABP) is a low molecular weight (14.5 kDa) protein, which contains 132 amino acid residues [7]. h-FABP is found in abundance in cardiomyocytes but is also expressed (to a lesser extent) in skeletal muscle, distal tubular cells of the kidney, specific parts of the brain, lactating mammary glands and placenta [8]. h-FABP binds two molecules of fatty acids and is involved in the delivery of fatty acyl coenzyme A, which is actively included in oxidation processes, which generate energy in the mitochondria. The concentration of fatty acids in plasma and in myocardial tissue rise during myocardial ischemia and it is postulated that h-FABP, which is immediately available for the metabolic needs of the cell, protects myocytes against fatty acid oxidation. Following myocardial cell damage, this small protein diffuses much more rapidly than troponins through the interstitial space and appears in the circulation probably through a trans-endothelial pathway [9]. This protein can be detected in the blood as early as 1–3 h after onset of chest pain, with peak values reached at 6–8 h and plasma levels returning to normal within 24–30 h [10]. Thus, h-FABP appears to be a very stable protein for early detection of myocardial necrosis and can be useful for in vitro clinical diagnostic purposes.
Recent studies have shown that h-FABP might have potential as an early cardiac biomarker in latent myocardial injury. It can be used for prognosis in chronic heart failure patients [11], and also to detect myocardial damage within 1 h after onset of ischemia [12]. However, the clinical impact of this on its diagnostic performance remains uncertain [13]. This study aims to validate the immunoturbidimetric quantitative in vitro determination of h-FABP and to compare its levels to routinely measured Troponin T levels in early diagnosis of patient presenting with acute chest pain in emergency department in a tertiary care hospital.
Methods
Study Population
The study was carried out in the Department of Biochemistry, P. D Hinduja National Hospital and Medical Research Centre, Mumbai, India. Patients arriving at the emergency department with chest pain or pain radiating to left arm, epigastric pain, shortness of breath and other symptoms indicative of ACS were recommended to perform biomarker test for Troponin T by the cardiologists. These patients were then also analysed for h-FABP. Symptom onset was recorded for each patient at the time of admission. Demographics, including body mass index (BMI) and clinical data, such as, ECG recordings, Systolic and diastolic blood pressures diagnosis, revascularization, and coronary risk factors were collected from hospital medical records.
Final Diagnosis
Diagnostic outcome was categorized into two groups: (1) ACS [which included Unstable, Angina (UA), STEMI, and non-STEMI]; (2) No ACS [which included cases of non-cardiac chest pain (NCCP), epigastric pain, left leg/arm pain etc.]. The diagnosis of NCCP was based on absence of significant findings indicative of cardiovascular problems, laboratory tests and ECG findings.
Sample Collection and Biochemical Analysis
Blood samples drawn in EDTA vacutainer from the patients admitted to the Emergency department were sent to the biochemistry laboratory for Troponin T (hs-TropT) estimation. Plasma TropT levels were measured quantitatively using the Elecsys high sensitive Troponin T (hs-TropT) immunoassay (Roche Diagnostics, Switzerland) using 912 Roche analyzer. For this study, two different cut-off values of 0.1 ng/ml recommended by WHO and 0.014 ng/ml recommended in kit insert by the manufacturers were used to compare the results. As analysis of h-FABP was not done immediately after hs-TropT estimation, these samples were stored at −80 °C till h-FABP test was performed.
Estimations of h-FABP assay (Randox Laboratories Ltd., Crumlin, UK) was done on VITROS® 5, 1 FS Chemistry System, (Ortho-Clinical Diagnostics, Johnson & Johnson Limited) using bi-level quality control material and calibrators supplied with the assay kit The analytical range for h-FABP is 0.75–120 ng/ml; a cut-off of 6.32 ng/ml was used to define abnormality based on 99th percentile for the 250 healthy controls as per the kit inserts.
Statistical Analysis (Table 2, 3)
Table 2.
Bio-statistical analysis of cardiac markers in ACS patients
| ACS (n = 41) | Non-ACS (n = 47) | Sensitivity (%) (95 % CI) | Specificity (%) (95 % CI) | PPV (%) (95 % CI) | NPV (%) (95 % CI) | |
|---|---|---|---|---|---|---|
| Trop T (cut off 0.1 ng/ml) | ||||||
| >0.1 | TP = 22 | FP = 1 | 53 (37.4–69.3) | 98 (88.7–99.6) | 96 (77.9–99.3) | 71 (58.2–81.4) |
| <0.1 | FN = 19 | TN = 46 | ||||
| Trop T (cut off 0.014 ng/ml) | ||||||
| >0.014 | TP = 35 | FP = 13 | 86 (70.8–94.4) | 73 (57.4–84.4) | 73 (58.2–84.7) | 85 (70.2–94.3) |
| <0.014 | FN = 6 | TN = 34 | ||||
| h-FABP (cut off 6.32 ng/ml) | ||||||
| >6.32 | TP = 32 | FP = 14 | 78 (62.4–89.4) | 70 (55.1–82.6) | 70 (54.2–82.3) | 79 (63.2–89.7) |
| <6.32 | FN = 9 | TN = 33 | ||||
ACS acute coronary syndrome, PPV positive predictive value, NPV negative predictive value CI confidence interval, TP true positive, FP false positive, TN true negative, FN false negative
Table 3.
Bio-statistical analysis of cardiac markers in combination for ACS patients
| ACS (n = 41) | Non-ACS (n = 47) | Sensitivity (%) (95 % CI) | Specificity (%) (95 % CI) | PPV (%) (95 % CI) | NPV (%) (95 % CI) | |
|---|---|---|---|---|---|---|
| Trop T (cut off 0.1 ng/ml) and/or h-FABP (cut off 6.32 ng/ml) | ||||||
| >0.1 | TP = 37 | FP = 15 | 90 (76.9–97.2) | 68 (52.9–80.9) | 71 (56.9–82.9) | 89 (73.9–96.8) |
| <0.1 | FN = 4 | TN = 32 | ||||
| Trop T (cut off 0.014 ng/ml) and/or h-FABP (cut off 6.32 ng/ml) | ||||||
| >0.014 | TP = 41 | FP = 23 | 100 (91.3–100) | 51 (36.1–65.9) | 64 (51.1–75.7) | 100 (91.7–100) |
| <0.014 | FN = 0 | TN = 24 | ||||
ACS acute coronary syndrome, PPV positive predictive value, NPV negative predictive value, CI confidence interval, TP true positive, FP false positive, TN true negative, FN false negative
Categorical variables are presented as numbers and percentages, while continuous variables are presented as mean ± SD (Standard deviation). Variables were compared using z-transformation test, Chi squared test and Mann–Whitney U test. All hypothesis were 2-tailed tests and P < 0.05 was considered statistically significant. Area under the receiver operator characteristic (ROC) curves at 95 % confidence interval (CI) was calculated using MedCalc Statistical Software (MedCalc version 12, Mariakerke, Belgium).
Results
Of the 88 patients, 41 (46.9 %) were diagnosed with ACS at admission. Patients with a final diagnosis of ACS did not differ significantly from those without ACS with respect to mean age, gender, risk factors like hypertension, diabetes, smoking, renal disease, previous interventions (Table 1).
Table 1.
Baseline clinical data of subjects in the study population
| Characteristic | All subjects (n = 88) | Subjects with ACS (n = 41) | Subjects without ACS (n = 47) | P value | Significance |
|---|---|---|---|---|---|
| Age (mean years ± SD) | 58.7 ± 16.2 | 64.6 ± 14.4 | 53.6 ± 15.7 | 0.44 | NS |
| Male, n (%) | 51 (58) | 25 (61) | 26 (55) | 0.85 | NS |
| Female, n (%) | 37 (42) | 16 (39) | 21 (45) | 0.72 | NS |
| Risk factors | |||||
| Hypertension, n (%) | 45 (51) | 22 (54) | 23 (49) | 0.65 | NS |
| Diabetes, n (%) | 22 (25) | 13 (32) | 9 (19) | 0.18 | NS |
| Smoking, n (%) | 11 (13) | 7 (17) | 4 (9) | 0.23 | NS |
| Renal disease, n (%) | 5 (6) | 3 (7) | 2 (4) | 0.54 | NS |
| Previous interventions, n (PCI/CABG) (%) | 14 (16) | 10 (24) | 4 (9) | 0.05 | S |
| Clinical findings | |||||
| Heart rate (beats/min) (mean ± SD) | 91.6 ± 25.3 | 95.3 ± 32.1 | 88 ± 19.18 | _ | _ |
| Blood pressure (mmHg) (mean ± SD) | |||||
| Diastolic | 84.9 ± 5 | 83.9 ± 20.6 | 84.9 ± 20.4 | _ | _ |
| Systolic | 131.1 ± 26.1 | 134.5 ± 23.6 | 136.1 ± 25.9 | _ | _ |
| Creatinine (mg/dl) (mean ± SD) | 1.4 ± 1.3 | 1.3 ± 1.4 | 1.5 ± 1.8 | _ | _ |
ACS acute coronary syndrome, PCI percutaneous coronary interventions, CABG coronary artery bypass graft, SD standard deviation, NS non-significant, S significant
In this study, two different diagnostic cut-offs were used for hs-Trop T, 0.1 and 0.014 ng/ml respectively, to compare the performance of the assay. The specificity of hs-TropT >0.1 ng/ml (98 %) is significantly higher than Troponin T >0.014 ng/ml (73 %) and h-FABP >6.32 ng/ml (70 %). In contrast, h-FABP >6.23 ng/ml and Troponin T >0.014 ng/ml was more sensitive than Troponin T >0.1 ng/ml with sensitivities equal to 78, 86 and 53 % respectively. Table 2 shows that Troponin T > 0.014 ng/ml is superior to Troponin T >0.1 ng/ml and h-FABP in terms of accuracy.
A combination of h-FABP (>6.32 ng/ml) OR Trop T (>0.014 ng/ml) was found to be optimal for early diagnosis of ACS, comparing with the combination of h-FABP (>6.32 ng/ml) OR Trop T (>0.1 ng/ml) as the former gives a sensitivity and NPV of 100 % (Table 3).
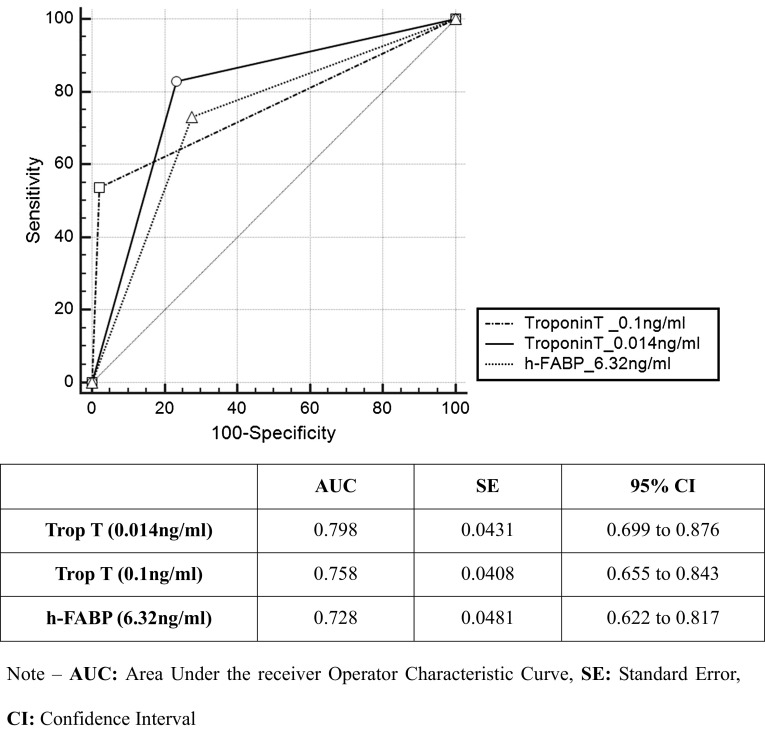
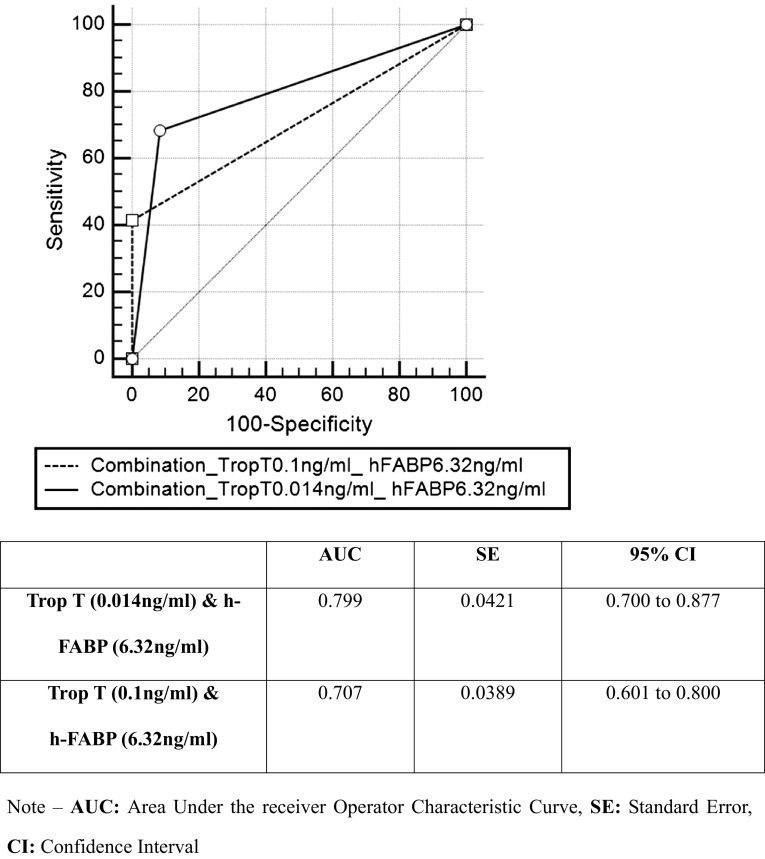
The area under the ROC curve to distinguish ACS from non-ACS after the symptom onset was, 0.758 for TropT (0.1 ng/ml), 0.798 for TropT (0.014 ng/ml) and 0.728 for h-FABP (Fig. 1). And in combination, area under the curve (AUC) for TropT (0.1 ng/ml) and h-FABP was 0.707 whereas for TropT (0.014 ng/ml) and h-FABP was 0.799 (Fig. 2).
Fig. 1.
Comparative receiver operator characteristic (ROC) curve for individual markers, Troponin T and h-FABP
Fig. 2.
Comparative receiver operator characteristic (ROC) curve in combination of markers, Troponin T and h-FABP
Discussion
This observational study demonstrated that measurement of plasma h-FABP in accordance with Troponin T concentrations on admission provides important information for risk stratification of patients presenting with ACS after the onset of chest pain. Importance of biomarkers, both in diagnosis and prognosis of ACS is now well established [2] and proved superior to electrocardiographic guidance alone [8]. Cardiac troponins remain the cornerstone in the risk stratification of patients with suspected ACS [14]. h-FABP has been reported to be particularly sensitive within the first few hours after the onset of coronary occlusion and symptoms. The reason for this sensitivity has been explained by its small molecular weight (15 kDa) and its cytoplasmic unbound abundance, resulting in rapid release from damaged myocardium. Authors [7, 10, 15] have reported sensitivity and specificity as 42–67 % and 95–97 % respectively for troponin whereas for h-FABP, 75–87 % and 89–93 %, in patients admitted with 6 h of chest pain onset. Our study result was in complete agreement with the above studies presenting with 53 and 97 % sensitivity and specificity for Troponin T and 78 and 70 % for h-FABP respectively.
The low h-FABP specificity of 42–70 % in similar settings was also reported by number of other investigators [7, 10, 15–17]. The reasons for the poor specificity of h-FABP for the final diagnosis of AMI have been due its presence in tissues outside the heart or may be because renal insufficiency [18].
In accordance with our study, an increased sensitivity in combination of hs-TropT measurement with h-FABP has been discussed in other reports [3, 15, 18]. Also, ROC curves demonstrated that a combined measurement of plasma h-FABP and Troponin T, has a great potential which allows to discriminate between ACS and non-ACS patients as compared to the conventional measurement of both markers individually.
Conclusion
The present study highlights the importance of estimating both cardiac markers (h-FAPB and hs-Trop T) in early diagnosis of ACS. Furthermore, in cases present at the emergency department after the chest pain onset, combined use of Troponin T and h-FABP is optimal for improving the early diagnosis of ACS. Also, the 100 % NPV at this time point may improve the accuracy of discharge decisions of the patients. The small sample size can be a limitation of the study which prevent generalisation of results. However, further large scale studies would certainly help to access the value of the combined use of these markers in the context of suspected ACS, and to detect myocardial ischemia and injury, such as after PCI or surgical interventions.
Acknowledgments
We acknowledge P. D Hinduja National Hospital & Medical Research Centre for their continued encouragement and Randox laboratories India Pvt. Ltd. for support in terms of reagents for the study.
References
- 1.Morrow D, Cannon C, Jesse R, Newby L, Ravkilde J, Storrow A, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation. 2007;115(13):e356–e375. doi: 10.1161/CIRCULATIONAHA.107.182882. [DOI] [PubMed] [Google Scholar]
- 2.Nagesh C, Roy A. Role of biomarkers in risk stratification of acute coronary syndrome. Indian J Med Res. 2010;132:627. doi: 10.4103/0971-5916.73419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Body R, McDowell G, Carley S, Wibberley C, Ferguson J, Mackway-Jones K. A FABP-ulous ‘rule out’ strategy? Heart fatty acid binding protein and troponin for rapid exclusion of acute myocardial infarction. Resuscitation. 2011;82(8):1041–1046. doi: 10.1016/j.resuscitation.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Nusier M, Ababneh B. Diagnostic efficiency of creatine kinase (CK), CKMB, troponin T and troponin I in patients with suspected acute myocardial infarction. J Health Sci. 2006;52(2):180–185. doi: 10.1248/jhs.52.180. [DOI] [Google Scholar]
- 5.Bass N. The cellular fatty acid binding proteins: aspects of structure, regulation, and function. Int Rev Cytol. 1988;111:143–184. doi: 10.1016/S0074-7696(08)61733-7. [DOI] [PubMed] [Google Scholar]
- 6.Viswanathan K, Hall A, Barth J. An evidence-based approach to the assessment of heart-type fatty acid binding protein in acute coronary syndrome. Clin Biochem Rev. 2012;33:3–11. [PMC free article] [PubMed] [Google Scholar]
- 7.Ruzgar O, Bilge A, Bugra Z, Umman S, Yilmaz E, Ozben B, et al. The use of human heart-type fatty acid-binding protein as an early diagnostic biochemical marker of myocardial necrosis in patients with acute coronary syndrome, and its comparison with troponin-T and creatine kinase–myocardial band. Heart Vessels. 2006;21(5):309–314. doi: 10.1007/s00380-006-0908-2. [DOI] [PubMed] [Google Scholar]
- 8.Ishii J, Ozaki Y, Lu J, Kitagawa F, Kuno T, Nakano T, et al. Prognostic value of serum concentration of heart-type fatty acid-binding protein relative to cardiac troponin T on admission in the early hours of acute coronary syndrome. Clin Chem. 2005;51(8):1397–1404. doi: 10.1373/clinchem.2004.047662. [DOI] [PubMed] [Google Scholar]
- 9.Colli A, Josa M, Pomar J, Mestres C, Gherli T. Heart fatty acid binding protein in the diagnosis of myocardial infarction: where do we stand today? Cardiology. 2007;108(1):4. doi: 10.1159/000095594. [DOI] [PubMed] [Google Scholar]
- 10.Gururajan P, Gurumurthy P, Nayar P, Rao GSN, Babu S, Cherian K. Heart fatty acid binding protein (H-FABP) as a diagnostic biomarker in patients with acute coronary syndrome. Heart Lung Circ. 2010;19(11):660–664. doi: 10.1016/j.hlc.2010.06.665. [DOI] [PubMed] [Google Scholar]
- 11.Niizeki T, Takeishi Y, Takabatake N, Shibata Y, Konta T, Kato T, et al. Circulating levels of heart-type fatty acid-binding protein in a general Japanese population. Circ J. 2007;71(9):1452–1457. doi: 10.1253/circj.71.1452. [DOI] [PubMed] [Google Scholar]
- 12.Slot MB, van der Heijden G, Rutten F, van der Spoel O, Mast E, Bredero A, et al. Heart-type fatty acid-binding protein in acute myocardial infarction evaluation (FAME): background and design of a diagnostic study in primary care. BMC Cardiovasc Disord. 2008;8(1):8. doi: 10.1186/1471-2261-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mad P, Domanovits H, Fazelnia C, Stiassny K, Russmuller G, Cseh A, et al. Human heart-type fatty-acid-binding protein as a point-of-care test in the early diagnosis of acute myocardial infarction. QJM. 2007;100(4):203–210. doi: 10.1093/qjmed/hcm007. [DOI] [PubMed] [Google Scholar]
- 14.Viswanathan K, Kilcullen N, Morrell C, Thistlethwaite S, Sivananthan M, Hassan T, et al. Heart-type fatty acid-binding protein predicts long-term mortality and re-infarction in consecutive patients with suspected acute coronary syndrome who are troponin-negative. J Am Coll Cardiol. 2010;55(23):2590–2598. doi: 10.1016/j.jacc.2009.12.062. [DOI] [PubMed] [Google Scholar]
- 15.McMahon C, Lamont J, Curtin E, McConnell R, Crockard M, Kurth M, et al. Diagnostic accuracy of heart-type fatty acid–binding protein for the early diagnosis of acute myocardial infarction. Ame J Emerg Med. 2012;30(2):267–274. doi: 10.1016/j.ajem.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 16.Haltern G, Peiniger S, Bufe A, Reiss G, Gülker H, Scheffold T. Comparison of usefulness of heart-type fatty acid binding protein versus cardiac troponin T for diagnosis of acute myocardial infarction. Am J Cardiol. 2010;105(1):1–9. doi: 10.1016/j.amjcard.2009.08.645. [DOI] [PubMed] [Google Scholar]
- 17.Nakata T, Hashimoto A, Hase M, Tsuchihashi K, Shimamoto K. Human heart-type fatty acid-binding protein as an early diagnostic and prognostic marker in acute coronary syndrome. Cardiology. 2003;99(2):96–104. doi: 10.1159/000069726. [DOI] [PubMed] [Google Scholar]
- 18.Ramaiah JH, Ramegowda TR, Ashalatha B, Ananthakrishna R, Nanjappa CM. Heart-type fatty acid-binding protein (h-fabp) as a novel biomarker for the early diagnosis of acute myocardial infarction in comparison with cardiac troponin T. J Evol Med Dent Sci. 2013;2(1):8–18. doi: 10.14260/jemds/208. [DOI] [Google Scholar]