Abstract
Background
Esophageal cancer is the most common cancer in less developed countries. It is necessary to understand epidemiology of the cancer for planning. The aim of this study was to evaluate the incidence and mortality of esophageal cancer, and its relationship with Human Development Index (HDI) and its components in Asia in 2012.
Methods
This study was an Ecological study, which conducted based on GLOBOCAN project of WHO for Asian counters. We assess the correlation between standardized incidence rates (SIR) and standardized mortality rates (SMR) of esophageal cancer with HDI and its components with using of SPSS18.
Results
A total of 337,698 incidence (70.33% were males and 29.87% females. Sex ratio was 2.37) and 296,734 death (69.45% in men and 30.54% in women. The sex ratio was 2.27) esophageal cancer was recorded in Asian countries in 2012. Five countries with the highest SIR and SMR of esophageal cancer were Turkmenistan, Mongolia and Tajikistan, Bangladesh and China respectively. Correlation between HDI and SIR was −0.211 (P=0.159), in men −0.175 (P=0.244) and in women −0.231 (P=0.123). Also between HDI and SMR −0.250 (P=0.094) in men −0.226 (P=0.131) and in women −0.251 (P=0.037).
Conclusions
The incidence of esophageal cancer is more in less developed and developing countries. Statistically significant correlation was not found between standardized incidence and mortality rates of esophageal cancer, and HDI and its dimensions, except for life expectancy at birth.
Keywords: Asia, epidemiology, esophageal cancer, inequality, incidence, mortality
Introduction
Esophageal cancer is the eighth most common cancer in the world. It is also the sixth leading cause of death from cancer worldwide (1,2). In 2001, over 300,000 cases of esophageal cancer were reported in the world (3). In 2012, approximately 450,000 people (3.2% of all cancers) suffered from the cancer, and 400,000 patients (4.9% of the total) lost their lives due to cancer worldwide. It highlighted an increase in incidence in the last decade, and it is expected to quickly increase its incidence (4,5). Low survival rate and rapid progression of this cancer are main features of this cancer (6,7). Despite medical advances in recent decades for the treatment of cancer, 5-year survival rate for patients is less than 20% (8). More than 80% of cases and deaths from the cancer occur in developing and less developed countries (9,10). Geographically dispersed distribution is the distinguishing feature of esophageal cancer (9). The highest incidence of esophageal cancer in the world was observed in China, Northeastern of Iran, southeast of United States, and South of Africa (1,11). Asian belt of the cancer begins from East of Turkey and Northeastern of Iran, and continues to the East Asian countries, including North and center of China. The incidence of the cancer in these areas is more than 100 per 100,000 (1,11). Esophagus cancer more occurs in men. Sex ratio (male to female) varies from 2 to 4 times. However, in some areas it occurs equally in men and women, which represents the same exposure to causal factors of the disease (3,12). The incidence of esophagus cancer is different in both men and women in various regions of the world about 20 times, in men from 0.8 per 100,000 in West Africa to 17 per 100,000 in East Asia and in women from 0.02 per 100,000 in Micronesia/Polynesia (central and southern Pacific) to 7.8 per 100,000 in East Africa (4,5). Two types of morphologies known for the cancer are squamous cell carcinoma (SCC) and adenocarcinoma (ADC). Different epidemiological features and risk factors are also considered for the cancer. Alcohol, smoking, malnutrition, a history of head and neck cancer, frequent consumption of beer, and other factors are the main causes of SCC, while the ADC is more associated with gastro esophageal reflux and Barrett’s esophagus, obesity, age, and male sex (8,12-14). Exposure to X-rays also increases both the type of cancer (15). Most cases of esophagus cancer are SCC (16), but the incidence is decreasing for unknown reasons. In contrast, the incidence of ADC is rising (17). Esophagus cancer has not a good screening, but it can be detected at an early stage using endoscopy every three to 5 years in people at high risk, such as Barrett’s esophagus, heavy smokers, and heavy alcohol consumers (17,18). Life style is one of the effective factors on the distribution of the cancer, and it is strongly influenced by individuals’ socio-economic level. Studies found that people with low socio-economic level due to poor nutrition, excessive alcohol consumption, and smoking are more likely to SCC. The incidence is higher in patients with a lower income level than those who have a high income level (19). People with low education and low socio-economic level are also more likely to die from the cancer due to lack of access to proper medical services (20-22).
HDI is one of the indicators related to the position of a country in three basic aspects of development, and a composite of longevity, knowledge, and standard of living. Longevity is measured with life expectancy at birth, knowledge with potential years of education, and standard of living with GPD per capita or income. HDI is a number between zero and one. According to HDI, countries in the world are divided into four categories, as follows: Countries with very high HDI (HDI ≥0.9), countries with a high HDI (HDI ≥0.8), middle HDI countries (0.8> HDI >0.5), and countries with a low HDI (HDI ≤0.5). The index was proposed by UNDP in 1990 as an indicator comparing countries in three human dimensions. On average, HDI was reported from the Arabic countries about 0.682, East Asia and Pacific 0.703, and South Asia 0.588. The mean the index in some Asian countries is lower than the global mean (0.702) in 2013 (23).
The importance of HDI in incidence and mortality from esophageal cancer has been confirmed in a number of studies (21,24). It is necessary to know information on incidence and mortality for health planning and research activities. Considering the possible role, the aim of this study was to evaluate the incidence and mortality of esophageal cancer, and its relationship with Human Development Index (HDI) and its components in Asia in 2012.
Methods
This study was an ecologic study in Asia for assessment the correlation between age-specific incidence and mortality rate (ASR) of esophageal cancer with HDI and its details that include: Life expectancy at birth, Mean years of schooling and gross national income (GNI) per capita. Data about the ASR for every Asian counter for year 2012 get from global cancer project that available in (http://globocan.iarc.fr/Default.aspx) and HDI from Human Development Report 2013 (23) that includes information about HDI and its details for every country in the word for year 2012.
Method of estimate the age-specific incidence and mortality rates in global cancer project by international agency for research on cancer
Age-specific incidence rate estimate
The methods of estimation are country specific and the quality of the estimation depends upon the quality and on the amount of the information available for each country. In theory, there are as many methods as countries, and because of the variety and the complexity of these methods, an overall quality score for the incidence and mortality estimates combined is almost impossible to establish. However, an alphanumeric scoring system, which independently describes the availability of incidence and mortality data, has been established at the country level. The combined score is presented together with the estimates for each country with an aim of providing a broad indication of the robustness of the estimation.
The methods to estimate the sex- and age-specific incidence rates of cancer for a specific country fall into one of the following broad categories, in priority order: (I) rates projected to 2012 (38 countries); (II) most recent rates applied to 2012 population (20 countries); (III) estimated from national mortality by modelling, using incidence mortality ratios derived from recorded data in country-specific cancer registries (13 countries); (IV) estimated from national mortality estimates by modeling, using incidence mortality ratios derived from recorded data in local cancer registries in neighboring countries (9 European countries); (V) estimated from national mortality estimates using modeled survival (32 countries); (VI) estimated as the weighted average of the local rates (16 countries); (VII) one cancer registry covering part of a country is used as representative of the country profile (11 countries); (VIII) age/sex specific rates for “all cancers” were partitioned using data on relative frequency of different cancers (by age and sex) (12 countries); (IX) the rates are those of neighboring countries or registries in the same area (33 countries) (4,5,10).
Age-specific mortality rate estimate
Depending of the degree of detail and accuracy of the national mortality data, six methods have been utilized in the following order of priority: (I) rates projected to 2012 (69 countries); (II) most recent rates applied to 2012 population (26 countries); (III) estimated as the weighted average of regional rates (1 country); (IV) estimated from national incidence estimates by modeling, using country-specific survival (2 countries); (V) estimated from national incidence estimates using modeled survival (83 countries); (VI) the rates are those of neighboring countries or registries in the same area (3 countries) (4,5,10).
Human Development Index (HDI)
HDI is a composite measure of indicators along three dimensions: life expectancy, educational attainment and command over the resources needed for a decent living. All groups and regions have seen notable improvement in all HDI components, with faster progress in low and medium HDI countries. On this basis, the world is becoming less unequal. Nevertheless, national averages hide large variations in human experience. Wide disparities remaining within countries of both the North and the South, and income inequality within and between many countries have been rising (23).
Statistical analysis
In this study, we use of correlation bivariate method for assessment the correlation between ASR with HDI and its details that include life expectancy at birth and mean years of schooling and GNI per capita. Statistical significance was assumed if P<0.05. All reported P values are two-sided. Statistical analyses were performed using SPSS (Version 15.0, SPSS Inc. USA).
Results
A total of 337,698 esophageal cancer cases were recorded in Asian countries in 2012. Overall, 237,510 cases (70.33%) were males and 100,188 cases (29.87%) females. Sex ratio in Asia was 2.37. The five countries with the highest number of new patients were china (223,306 cases), India (41,774 cases), Japan (19,683 cases), Bangladesh (13,909 cases), and Iran (5,343,489 cases), respectively.
Among Asian countries, five countries with the highest standardized incidence rates (SIR) of the cancer were Turkmenistan with 19.7 per 100,000, Mongolia with 17.6 per 100,000, Tajikistan with 14.7 per 100,000, Bangladesh with 12.7 per 100,000, and China with 12.5 per 100,000, respectively. Five countries with the lowest SIR of the cancer were Georgia with 0.6 per 100,000, Lao PDR with 0.6 per 100,000, Lebanon with 0.7 per 100,000, Brunei with 0.7 per 100,000, and Kuwait with 0.8 per 100,000, respectively. The number, crude and SIR of the cancer in Asian countries based on sex are presented in Table 1. Countries in the table are sorted from high to low based on the SIR. The countries with the highest and lowest SIR in both sexes are observable in Table 1 and Figure 1.
Table 1. Number, crude, and standardized incidence rate of esophageal cancer in Asian countries in 2012 (sorted by age standardized rates of both sexes from highest to lowest).
| Population | Esophagus: estimated incidence |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| All ages: both sexes |
All ages: male |
All ages: female |
|||||||||
| Numbers | Crude rate | ASR (W) | Numbers | Crude rate | ASR (W) | Numbers | Crude rate | ASR (W) | |||
| Turkmenistan | 719 | 13.9 | 19.7 | 384 | 15.1 | 24.0 | 335 | 12.8 | 16.4 | ||
| Mongolia | 316 | 11.1 | 17.6 | 166 | 11.8 | 21.2 | 150 | 10.4 | 14.9 | ||
| Tajikistan | 570 | 8.1 | 14.7 | 342 | 9.8 | 19.8 | 228 | 6.3 | 10.7 | ||
| China | 223,306 | 16.4 | 12.5 | 160,436 | 22.7 | 18.6 | 62,870 | 9.6 | 6.7 | ||
| Bangladesh | 13,909 | 9.1 | 12.7 | 8,567 | 11.1 | 15.9 | 5,342 | 7.1 | 9.5 | ||
| Kazakhstan | 1,684 | 10.3 | 10.1 | 965 | 12.3 | 15.8 | 719 | 8.4 | 6.6 | ||
| Afghanistan | 1,326 | 4.0 | 9.6 | 801 | 4.6 | 11.8 | 525 | 3.3 | 7.5 | ||
| Islamic Republic of Iran | 5,343 | 7.1 | 8.6 | 2,898 | 7.6 | 9.0 | 2,445 | 6.6 | 8.0 | ||
| Myanmar | 3,437 | 7.1 | 7.6 | 2,441 | 10.2 | 11.4 | 996 | 4.0 | 4.2 | ||
| Japan | 19,683 | 15.6 | 6.1 | 16,530 | 26.9 | 11.1 | 3,153 | 4.9 | 1.7 | ||
| Uzbekistan | 1,180 | 4.2 | 6.0 | 627 | 4.5 | 7.2 | 553 | 3.9 | 5.0 | ||
| Bhutan | 32 | 4.3 | 5.7 | 19 | 4.8 | 6.5 | 13 | 3.7 | 4.8 | ||
| Sri Lanka | 1,407 | 6.6 | 5.6 | 667 | 6.4 | 5.7 | 740 | 6.9 | 5.4 | ||
| Democratic Republic of Korea | 1,618 | 6.6 | 5.2 | 1,226 | 10.2 | 9.5 | 392 | 3.1 | 1.9 | ||
| Kyrgyzstan | 187 | 3.4 | 4.9 | 108 | 4.0 | 6.9 | 79 | 2.9 | 3.4 | ||
| Azerbaijan | 440 | 4.7 | 4.6 | 253 | 5.4 | 6.3 | 187 | 3.9 | 3.3 | ||
| Maldives | 10 | 3.1 | 4.3 | 7 | 4.3 | 6.0 | 3 | 1.9 | 2.6 | ||
| Yemen | 462 | 1.8 | 4.3 | 203 | 1.6 | 4.4 | 259 | 2.0 | 4.4 | ||
| Pakistan | 5,168 | 2.9 | 4.1 | 2,450 | 2.7 | 3.9 | 2,718 | 3.1 | 4.4 | ||
| India | 41,774 | 3.3 | 4.1 | 27,152 | 4.2 | 5.4 | 14,622 | 2.4 | 2.8 | ||
| Turkey | 2,536 | 3.4 | 3.6 | 1,395 | 3.8 | 4.3 | 1,141 | 3.1 | 3.0 | ||
| Viet Nam | 2,763 | 3.1 | 3.1 | 2,428 | 5.5 | 5.8 | 335 | 0.7 | 0.7 | ||
| Republic of Korea | 2,223 | 4.6 | 2.9 | 2,034 | 8.4 | 6.0 | 189 | 0.8 | 0.4 | ||
| Thailand | 2,308 | 3.3 | 2.5 | 1,873 | 5.5 | 4.4 | 435 | 1.2 | 0.8 | ||
| Nepal | 504 | 1.6 | 2.5 | 328 | 2.1 | 3.6 | 176 | 1.1 | 1.6 | ||
| Cambodia | 237 | 1.6 | 2.4 | 161 | 2.3 | 4.2 | 76 | 1.0 | 1.3 | ||
| Qatar | 13 | 0.7 | 2.2 | 9 | 0.6 | 1.8 | 4 | 0.9 | 3.0 | ||
| United Arab Emirates | 40 | 0.5 | 2.0 | 24 | 0.4 | 1.8 | 16 | 0.6 | 2.5 | ||
| Malaysia | 483 | 1.6 | 2.0 | 298 | 2.0 | 2.5 | 185 | 1.3 | 1.5 | ||
| Singapore | 137 | 2.6 | 1.7 | 107 | 4.0 | 2.9 | 30 | 1.2 | 0.6 | ||
| Bahrain | 10 | 0.7 | 1.7 | 7 | 0.8 | 2.2 | 3 | 0.6 | 1.3 | ||
| Timor-Leste | 10 | 0.8 | 1.7 | 8 | 1.3 | 2.6 | 2 | 0.3 | 0.8 | ||
| State of Palestine | 30 | 0.7 | 1.6 | 22 | 1.0 | 2.3 | 8 | 0.4 | 0.8 | ||
| Oman | 21 | 0.7 | 1.5 | 14 | 0.8 | 1.8 | 7 | 0.6 | 1.2 | ||
| Saudi Arabia | 225 | 0.8 | 1.4 | 121 | 0.8 | 1.4 | 104 | 0.8 | 1.4 | ||
| Armenia | 60 | 1.9 | 1.3 | 39 | 2.7 | 2.2 | 21 | 1.3 | 0.6 | ||
| Israel | 140 | 1.8 | 1.2 | 85 | 2.2 | 1.7 | 55 | 1.4 | 0.8 | ||
| Iraq | 190 | 0.6 | 1.2 | 99 | 0.6 | 1.4 | 91 | 0.5 | 1.0 | ||
| Philippines | 715 | 0.7 | 1.1 | 519 | 1.1 | 1.8 | 196 | 0.4 | 0.6 | ||
| Syrian Arab Republic | 138 | 0.7 | 1.0 | 85 | 0.8 | 1.3 | 53 | 0.5 | 0.8 | ||
| Indonesia | 2,191 | 0.9 | 1.0 | 1,513 | 1.2 | 1.5 | 678 | 0.6 | 0.6 | ||
| Jordan | 33 | 0.5 | 0.9 | 22 | 0.7 | 1.2 | 11 | 0.4 | 0.6 | ||
| Kuwait | 11 | 0.4 | 0.8 | 7 | 0.4 | 0.7 | 4 | 0.3 | 0.9 | ||
| Brunei | 2 | 0.5 | 0.7 | 1 | 0.5 | 0.5 | 1 | 0.5 | 1.2 | ||
| Lebanon | 34 | 0.8 | 0.7 | 19 | 0.9 | 0.9 | 15 | 0.7 | 0.6 | ||
| Lao PDR | 25 | 0.4 | 0.6 | 17 | 0.5 | 0.9 | 8 | 0.3 | 0.4 | ||
| Georgia | 48 | 1.1 | 0.6 | 33 | 1.6 | 1.0 | 15 | 0.7 | 0.3 | ||
Figure 1.
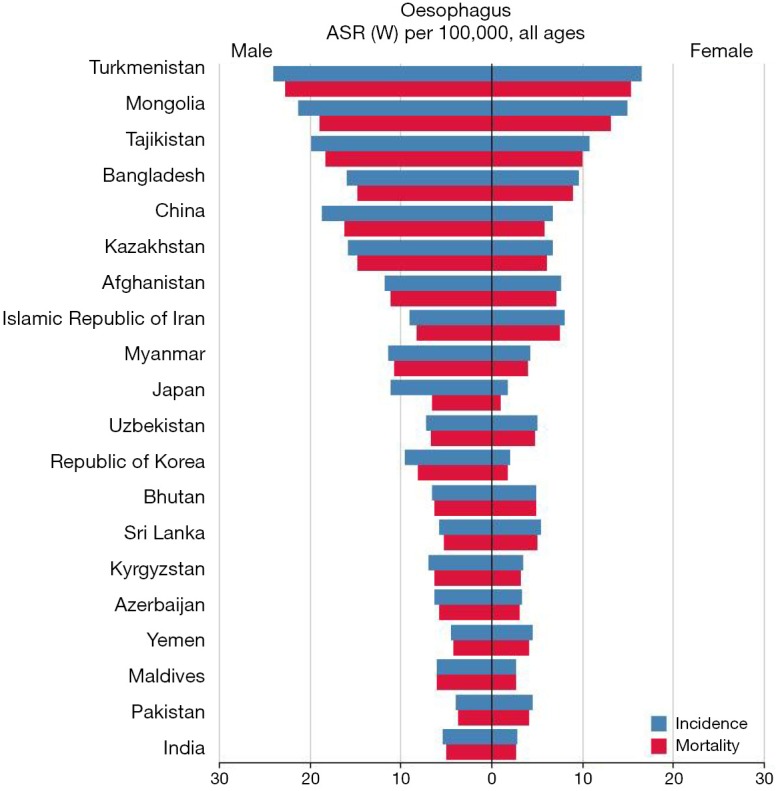
Standardized incidence and mortality rates from esophageal cancer in Asia in 2012 (extracted from GLOBALCAN 2012, http://globocan.iarc.fr) (5).
However, in 2012, in Asia, the number of deaths due to lung cancer was 296,734 cases, 206,096 cases (69.45%) in men and 90, 638 cases (30.54%) in women. The sex ratio (male to female) of mortality was equal to 2.27. The five countries with the highest number of deaths were china (197,472 cases), India (38,683 cases), Bangladesh (12,909 cases), Japan (12,440 cases), and Iran (4,915 cases), respectively. The countries included a total of 266,419 cases (89.78%) of the total mortality in Asia.
In Asian countries, five countries with the highest standardized mortality rates (SMR) from the cancer were Turkmenistan with 18.5 per 100,000, Mongolia with 15.5 per 100,000, Tajikistan with 13.6 per 100,000, Bangladesh with 11.7 per 100,000, and China with 10.9 per 100,000, respectively. Five countries with the lowest SMR from the cancer were Georgia with 15.5 per 100,000, Lao PDR with 0.6 per 100,000, Lebanon with 0.7 per 100,000, Brunei with 0.7 per 100,000, and Bahrain with 0.8 per 100,000, respectively. The number, crude, and SIR of the cancer in Asian countries based on sex are presented in Table 2. Countries in the table are sorted from high to low based on the SIR. The countries with the highest and lowest SIR are observable in both sexes in Table 2 and Figure 2.
Table 2. Number, crude, and standardized mortality rate of esophageal cancer in Asian countries in 2012 (sorted by age standardized rates of both sexes from highest to lowest).
| Population | Esophagus: estimated mortality |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| All ages: both sexes |
All ages: female |
All ages: male |
|||||||||
| Numbers | Crude rate | ASR (W) | Numbers | Crude rate | ASR (W) | Numbers | Crude rate | ASR (W) | |||
| Turkmenistan | 663 | 12.8 | 18.5 | 356 | 14.0 | 22.7 | 307 | 11.7 | 15.2 | ||
| Mongolia | 278 | 9.8 | 15.5 | 148 | 10.5 | 18.9 | 130 | 9.0 | 13.0 | ||
| Tajikistan | 527 | 7.4 | 13.6 | 313 | 9.0 | 18.3 | 214 | 5.9 | 9.9 | ||
| Bangladesh | 12,909 | 8.5 | 11.7 | 7,925 | 10.3 | 14.7 | 4,984 | 6.6 | 8.9 | ||
| China | 197,472 | 14.5 | 10.9 | 140,329 | 19.9 | 16.2 | 57,143 | 8.7 | 5.8 | ||
| Kazakhstan | 1,555 | 9.5 | 9.3 | 891 | 11.3 | 14.7 | 664 | 7.8 | 6.0 | ||
| Afghanistan | 1,217 | 3.6 | 9.0 | 738 | 4.3 | 11.1 | 479 | 3.0 | 7.0 | ||
| Islamic Republic of Iran | 4,915 | 6.5 | 7.8 | 2,662 | 6.9 | 8.2 | 2,253 | 6.0 | 7.4 | ||
| Myanmar | 3,207 | 6.6 | 7.1 | 2,273 | 9.5 | 10.7 | 934 | 3.8 | 3.9 | ||
| Uzbekistan | 1,094 | 3.9 | 5.6 | 582 | 4.2 | 6.7 | 512 | 3.6 | 4.7 | ||
| Bhutan | 31 | 4.1 | 5.5 | 18 | 4.5 | 6.2 | 13 | 3.7 | 4.8 | ||
| Sri Lanka | 1,302 | 6.1 | 5.1 | 618 | 5.9 | 5.2 | 684 | 6.4 | 5.0 | ||
| Kyrgyzstan | 172 | 3.2 | 4.5 | 98 | 3.6 | 6.3 | 74 | 2.7 | 3.1 | ||
| Democratic Republic of Korea | 1,396 | 5.7 | 4.4 | 1,039 | 8.6 | 8.1 | 357 | 2.9 | 1.7 | ||
| Maldives | 10 | 3.1 | 4.3 | 7 | 4.3 | 6.0 | 3 | 1.9 | 2.6 | ||
| Azerbaijan | 404 | 4.3 | 4.2 | 233 | 5.0 | 5.8 | 171 | 3.6 | 3.0 | ||
| Yemen | 431 | 1.7 | 4.1 | 192 | 1.5 | 4.2 | 239 | 1.9 | 4.1 | ||
| Pakistan | 4,748 | 2.6 | 3.8 | 2,241 | 2.5 | 3.6 | 2,507 | 2.8 | 4.0 | ||
| India | 38,683 | 3.1 | 3.8 | 25,170 | 3.9 | 5.0 | 13,513 | 2.2 | 2.6 | ||
| Japan | 12,440 | 9.8 | 3.5 | 10,443 | 17.0 | 6.5 | 1,997 | 3.1 | 0.9 | ||
| Turkey | 2,340 | 3.1 | 3.3 | 1,288 | 3.5 | 4.0 | 1,052 | 2.8 | 2.7 | ||
| Viet Nam | 2,577 | 2.9 | 2.9 | 2,269 | 5.1 | 5.5 | 308 | 0.7 | 0.6 | ||
| Nepal | 466 | 1.5 | 2.3 | 303 | 2.0 | 3.4 | 163 | 1.0 | 1.5 | ||
| Cambodia | 222 | 1.5 | 2.3 | 150 | 2.1 | 4.0 | 72 | 1.0 | 1.3 | ||
| Thailand | 2,061 | 2.9 | 2.2 | 1,675 | 4.9 | 4.0 | 386 | 1.1 | 0.8 | ||
| Qatar | 13 | 0.7 | 2.2 | 9 | 0.6 | 1.8 | 4 | 0.9 | 3.0 | ||
| United Arab Emirates | 39 | 0.5 | 2.0 | 23 | 0.4 | 1.7 | 16 | 0.6 | 2.5 | ||
| Republic of Korea | 1,551 | 3.2 | 1.9 | 1,415 | 5.8 | 4.1 | 136 | 0.6 | 0.2 | ||
| Timor-Leste | 10 | 0.8 | 1.7 | 8 | 1.3 | 2.6 | 2 | 0.3 | 0.8 | ||
| State of Palestine | 29 | 0.7 | 1.6 | 21 | 1.0 | 2.3 | 8 | 0.4 | 0.8 | ||
| Singapore | 126 | 2.4 | 1.6 | 99 | 3.7 | 2.6 | 27 | 1.0 | 0.6 | ||
| Oman | 21 | 0.7 | 1.5 | 14 | 0.8 | 1.8 | 7 | 0.6 | 1.2 | ||
| Malaysia | 328 | 1.1 | 1.3 | 210 | 1.4 | 1.7 | 118 | 0.8 | 1.0 | ||
| Saudi Arabia | 210 | 0.7 | 1.3 | 113 | 0.7 | 1.4 | 97 | 0.8 | 1.3 | ||
| Armenia | 58 | 1.9 | 1.2 | 37 | 2.6 | 2.0 | 21 | 1.3 | 0.6 | ||
| Iraq | 176 | 0.5 | 1.1 | 92 | 0.5 | 1.3 | 84 | 0.5 | 0.9 | ||
| Philippines | 623 | 0.6 | 1.0 | 449 | 0.9 | 1.6 | 174 | 0.4 | 0.5 | ||
| Kuwait | 15 | 0.5 | 1.0 | 9 | 0.5 | 0.9 | 6 | 0.5 | 1.2 | ||
| Syrian Arab Republic | 130 | 0.6 | 1.0 | 79 | 0.7 | 1.2 | 51 | 0.5 | 0.7 | ||
| Israel | 118 | 1.5 | 1.0 | 69 | 1.8 | 1.4 | 49 | 1.3 | 0.6 | ||
| Indonesia | 2,023 | 0.8 | 0.9 | 1,394 | 1.1 | 1.4 | 629 | 0.5 | 0.5 | ||
| Jordan | 32 | 0.5 | 0.9 | 21 | 0.6 | 1.1 | 11 | 0.4 | 0.6 | ||
| Bahrain | 6 | 0.4 | 0.8 | 5 | 0.6 | 1.4 | 1 | 0.2 | 0.2 | ||
| Brunei | 2 | 0.5 | 0.7 | 1 | 0.5 | 0.5 | 1 | 0.5 | 1.2 | ||
| Lebanon | 34 | 0.8 | 0.7 | 19 | 0.9 | 0.9 | 15 | 0.7 | 0.6 | ||
| Lao PDR | 25 | 0.4 | 0.6 | 17 | 0.5 | 0.9 | 8 | 0.3 | 0.4 | ||
| Georgia | 45 | 1.0 | 0.6 | 31 | 1.5 | 0.9 | 14 | 0.6 | 0.3 | ||
Figure 2.
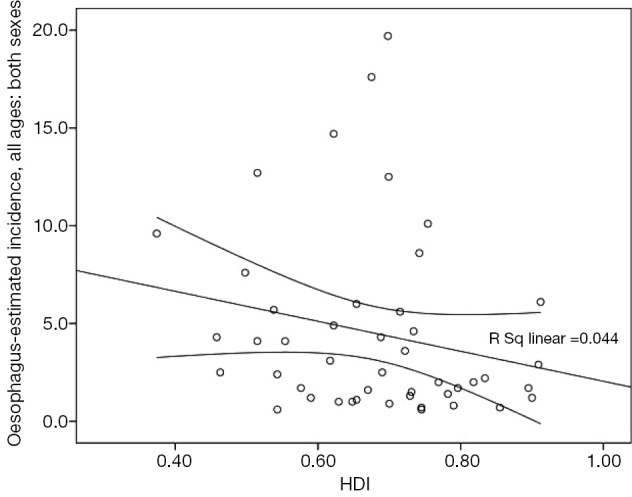
Correlation between HDI and standardized incidence of esophagus cancer in Asia in 2012 (mean ± 95% confidence interval). HDI, Human Development Index.
In Table 3, amounts related to HDI and its components for each of the Asian countries (sorted based on HDI) is shown. Accordingly, Asian countries are classified according to HDI as follows: three countries in the very high category, four countries in high, 35 countries in the middle category, three countries in low, and one in the unknown category.
Table 3. Human Development Index in Asian countries in 2012.
| Population | Human Development Index (HDI) | Life expectancy at birth | Mean year of schooling | Gross national income (GNI) per capita |
|---|---|---|---|---|
| Very high human development | ||||
| Japan | 0.912 | 83.6 | 11.6 | 32,545 |
| Republic of Korea | 0.909 | 80.7 | 11.6 | 28,231 |
| Israel | 0.900 | 81.9 | 11.9 | 26,224 |
| Singapore | 0.895 | 81.2 | 10.1 | 52,613 |
| Brunei | 0.855 | 78.1 | 8.6 | 45,690 |
| Qatar | 0.834 | 78.5 | 7.3 | 87,478 |
| United Arab Emirates | 0.818 | 76.7 | 8.9 | 42,716 |
| High human development | ||||
| Bahrain | 0.796 | 75.2 | 9.4 | 19,154 |
| Kuwait | 0.790 | 74.7 | 6.1 | 52,793 |
| Saudi Arabia | 0.782 | 74.1 | 7.8 | 22,616 |
| Malaysia | 0.769 | 74.5 | 9.5 | 13,676 |
| Kazakhstan | 0.754 | 67.4 | 10.4 | 10,451 |
| Georgia | 0.745 | 73.9 | 12.1 | 5,005 |
| Lebanon | 0.745 | 72.8 | 7.9 | 12,364 |
| Islamic Republic of Iran | 0.742 | 73.2 | 7.8 | 10,695 |
| Azerbaijan | 0.734 | 70.9 | 11.2 | 8,153 |
| Oman | 0.731 | 73.2 | 5.5 | 24,092 |
| Armenia | 0.729 | 74.4 | 10.8 | 5,540 |
| Turkey | 0.722 | 74.2 | 6.5 | 13,710 |
| Sri Lanka | 0.715 | 75.1 | 9.3 | 5,170 |
| Medium human development | ||||
| Jordan | 0.700 | 73.5 | 8.6 | 5,272 |
| China | 0.699 | 73.7 | 7.5 | 7,945 |
| Turkmenistan | 0.698 | 65.2 | 9.9 | 7,782 |
| Thailand | 0.690 | 74.3 | 6.6 | 7,722 |
| Maldives | 0.688 | 77.1 | 5.8 | 7,478 |
| Mongolia | 0.675 | 68.8 | 8.3 | 4,245 |
| State of Palestine | 0.670 | 73.0 | 8.0 | 3,359 |
| Philippines | 0.654 | 69.0 | 8.9 | 3,752 |
| Uzbekistan | 0.654 | 68.6 | 10.0 | 3,201 |
| Syrian Arab Republic | 0.648 | 76.0 | 5.7 | 4,674 |
| Indonesia | 0.629 | 69.8 | 5.8 | 4,154 |
| Kyrgyzstan | 0.622 | 68.0 | 9.3 | 2,009 |
| Tajikistan | 0.622 | 67.8 | 9.8 | 2,119 |
| Viet Nam | 0.617 | 75.4 | 5.5 | 2,970 |
| Iraq | 0.590 | 69.6 | 5.6 | 3,557 |
| Timor-Leste | 0.576 | 62.9 | 4.4 | 5,446 |
| India | 0.554 | 65.8 | 4.4 | 3,285 |
| Cambodia | 0.543 | 63.6 | 5.8 | 2,095 |
| Lao PDR | 0.543 | 67.8 | 4.6 | 2,435 |
| Bhutan | 0.538 | 67.6 | 2.3 | 5,246 |
| Low human development | ||||
| Bangladesh | 0.515 | 69.2 | 4.8 | 1,785 |
| Pakistan | 0.515 | 65.7 | 4.9 | 2,566 |
| Myanmar | 0.498 | 65.7 | 3.9 | 1,817 |
| Nepal | 0.463 | 69.1 | 3.2 | 1,137 |
| Yemen | 0.458 | 65.9 | 5.3 | 928 |
| Afghanistan | 0.374 | 49.1 | 3.1 | 1,000 |
| Other countries or territories | ||||
| Democratic Republic of Korea | – | – | – | – |
Standardized incidence rate (SIR) and Human Development Index (HDI)
A negative correlation was seen between the SIR of esophagus cancer and HDI about 0.211. This association was not statistically significant (P=0.159). There was a negative correlation between the SIR and life expectancy at birth about 0.363 (P=0.013), positive correlation between the SIR and mean years of schooling about 0.042 (P=0.783), and positive correlation between the level of income per each person of the population and the SIR equal to −0.175 (P=0.244).
In men, a negative correlation of −0.175 was observed between the SIR of esophagus cancer and HDI. It was not statistically significant (P=0.244). There was a negative correlation between the SIR and life expectancy at birth about −0.321 (P=0.03), positive correlation between mean years of schooling and the SIR about 0.082 (P=0.588), and negative correlation between the level of income per each person of the population and the SIR equal to −0.266 (P=0.074).
In women, a negative correlation of −0.231 was observed between the SIR of esophagus cancer and HDI. It was not statistically significant (P=0.123). There was a positive correlation between the SIR and life expectancy at birth about 0.402 (P=0.006), positive correlation between mean years of schooling and the SIR about 0.01 (P=0.950), and negative correlation between the level of income per each person of the population and the SIR equal to −0.217 (P=0.147).
The standardized mortality rate (SMR) and Human Development Index (HDI)
There was between the SMR for esophagus cancer and HDI a negative correlation of 0.250 (P=0.094) (Figure 3), expectancy at birth a negative correlation of −0.402 (P=0.006), mean years of schooling a negative correlation equal to −0.005 (P=0.975), and the level of income per each person of population a negative correlation of −0.271 (P=0.068).
Figure 3.
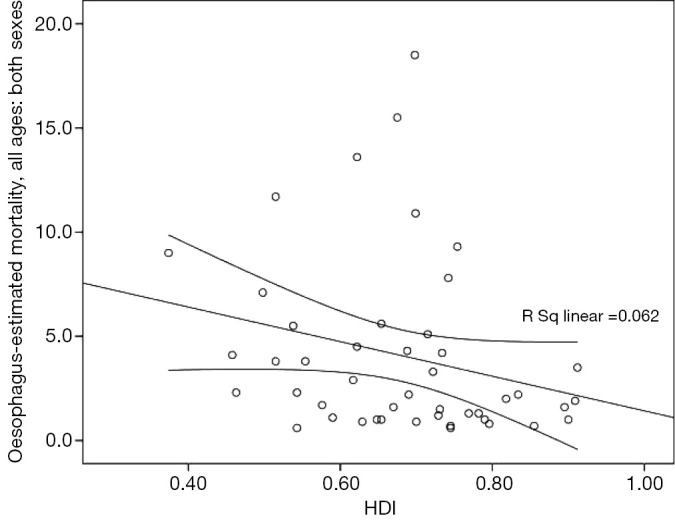
Correlation between HDI and standardized mortality rates for esophagus cancer in Asia in 2012 (mean ± 95% confidence interval). HDI, Human Development Index.
In men, there was between the SMR for esophagus cancer and HDI a negative correlation of 0.226 (P=0.131), expectancy at birth a negative correlation of 0.374 (P=0.010), mean years of schooling a positive correlation equal to 0.037 (P=0.808), and the level of income per each person of population a negative correlation of 0.212 (P=0.158).
In women, there was between the SMR for esophagus cancer and HDI a negative correlation of 0.251 (P=0.037), expectancy at birth a negative correlation of 0.419 (P=0.004), mean years of schooling a negative correlation equal to 0.017 (P=0.912), and the level of income per each person of population a negative correlation of 0.212 (P=0.158).
Discussion
More than 75% of esophageal cancers in the world occur in Asia, because of Asian belt of esophageal cancer. The disease is affecting many countries (4,10,25). Given that more than 60% of people and most developing countries in the world are in Asia. It is expected to dramatically increase the cancer in the continent. Therefore, health macro policies to deal with this cancer in the future are an important requirement (4,5).
The findings of this study showed that there was a negative correlation between esophageal cancer and HDI, but this relationship was not significant. The highest incidence of esophageal cancer in Asian countries was related to Turkmenistan, Mongolia, Tajikistan, Bangladesh, and China. All these countries are a part of the Asian belt of the cancer. Cancer incidence was in the region more than 100 per 100,000 (1,11). HDI was in all these countries middle. Studies have shown that in countries with middle HDI, esophageal cancer is the most common cancer (24). Many cases of esophageal cancer occur in less developed and developing countries, due to changing lifestyles, smoking, alcohol, and nutrition (8-10).
Another dimension of HDI was the level of education or awareness. However, no significant relationship was found between the SMR for the cancer and education, but other studies have shown that increasing the level of awareness reduced high-risk behaviors including smoking, alcohol consumption, physical inactivity, and poor lifestyle, that cause the cancer. It has been shown that educated people more tend to pay attention to health messages and checkup themselves for early detection of cancer (26).
One of the dimensions of HDI is the level of income, characterized by gross domestic product. In our study, there was no relationship between income, and mortality and incidence rates of esophageal cancer. Brown revealed that people with low income more consume smoking and alcohol, and consume fruits and vegetables less than those with higher incomes (19). Multiple regression analysis showed that black men are more likely to suffer from this cancer (27). Lifestyle changes, avoiding the risk of esophageal cancer in these individuals, and periodic examinations in the patients at high risk (Barrett’s esophagus, heavy smoker, and heavy alcohol consumer) are a priority in these people (17-19).
In our study, a significant relationship was not found between the incidence and mortality rates, and HDI and its dimensions, except for life expectancy at birth. Other studies have shown that death rates from the cancer are more in low and middle HDI countries (21,24). The incidence and mortality of esophageal cancer are higher in developing countries compared to developed countries. The incidence and prevalence of esophageal cancer is less when HDI increases (4,10). It seems to reduce incidence and prevalence of esophageal cancer in developed countries because of better treatment, screening using endoscopy, appropriate lifestyle, better access to health services, and reduction of infectious diseases. In contrast, in developing and least developed countries, incidence and dying from the cancer is likely more because of poor lifestyle, smoking, alcohol, and lack of adequate infrastructure for the implementation of comprehensive cancer control programs (8-10).
Limitations
This was an ecological study. The ecological fallacy will occur if results are inferred and concluded at the individual level. The results of this study are attributable only at the population level.
Conclusions
The incidence of esophageal cancer is more in less developed and developing countries. Statistically significant correlation was not found between standardized incidence and mortality rates of esophageal cancer, and HDI and its dimensions, except for life expectancy at birth.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Pennathur A, Gibson MK, Jobe BA, et al. Oesophageal carcinoma. Lancet 2013;381:400-12. [DOI] [PubMed] [Google Scholar]
- 2.Esophageal cancer: epidemiology, pathogenesis and prevention. Nat Clin Pract Gastroenterol Hepatol 2008;5:517-26. [DOI] [PubMed] [Google Scholar]
- 3.Pera M, Pera M. Recent changes in the epidemiology of esophageal cancer. Surg Oncol 2001;10:81-90. [DOI] [PubMed] [Google Scholar]
- 4.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available online: http://globocan.iarc.fr
- 5.Bekmukhambetov Y, Imangazina Z, Jarkenov T, et al. Cancer incidence and mortality data in Aktobe, west Kazakhstan, 2000-2010. Asian Pac J Cancer Prev 2015;16:2379-83. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol 2013;19:5598-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mao WM, Zheng WH, Ling ZQ. Epidemiologic risk factors for esophageal cancer development. Asian Pac J Cancer Prev 2011;12:2461-6. [PubMed] [Google Scholar]
- 8.Cheng ML, Zhang L, Borok M, et al. The incidence of oesophageal cancer in Eastern Africa: identification of a new geographic hot spot? Cancer Epidemiol 2015;39:143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [DOI] [PubMed] [Google Scholar]
- 10.Nikfarjam Z, Massoudi T, Salehi M, et al. Demographic survey of four thousand patients with 10 common cancers in North Eastern Iran over the past three decades. Asian Pac J Cancer Prev 2014;15:10193-8. [DOI] [PubMed] [Google Scholar]
- 11.Chong VH, Telisinghe PU, Chong CF. Esophageal Cancer in Brunei Darussalam over a three Decade Period: an Epidemiologic Study of Trends and Differences between Genders and Racial Groups. Asian Pac J Cancer Prev 2015;16:4123-6. [DOI] [PubMed] [Google Scholar]
- 12.Gatenby PA, Preston SR. Oesophageal cancer. Surgery (United Kingdom) 2014;32:588-93. [Google Scholar]
- 13.Koca T, Arslan D, Basaran H, et al. Dietary and demographical risk factors for oesophageal squamous cell carcinoma in the Eastern Anatolian region of Turkey where upper gastrointestinal cancers are endemic. Asian Pac J Cancer Prev 2015;16:1913-7. [DOI] [PubMed] [Google Scholar]
- 14.Wang FR, Fang QQ, Tang WM, et al. Nested Case-control Study of Occupational Radiation Exposure and Breast and Esophagus Cancer Risk among Medical Diagnostic X Ray Workers in Jiangsu of China. Asian Pac J Cancer Prev 2015;16:4699-704. [DOI] [PubMed] [Google Scholar]
- 15.Nun-Anan P, Vilaichone RK. Late stage and grave prognosis of esophageal cancer in Thailand. Asian Pac J Cancer Prev 2015;16:1747-9. [DOI] [PubMed] [Google Scholar]
- 16.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med 2003;349:2241-52. [DOI] [PubMed] [Google Scholar]
- 17.Morimoto M, Nishiyama K, Nakamura S, et al. Significance of endoscopic screening and endoscopic resection for esophageal cancer in patients with hypopharyngeal cancer. Jpn J Clin Oncol 2010;40:938-43. [DOI] [PubMed] [Google Scholar]
- 18.Brown LM, Hoover R, Silverman D, et al. Excess incidence of squamous cell esophageal cancer among US Black men: role of social class and other risk factors. Am J Epidemiol 2001;153:114-22. [DOI] [PubMed] [Google Scholar]
- 19.Menvielle G, Luce D, Geoffroy-Perez B, et al. Social inequalities and cancer mortality in France, 1975-1990. Cancer Causes Control 2005;16:501-13. [DOI] [PubMed] [Google Scholar]
- 20.Kiadaliri AA. Gender and social disparities in esophagus cancer incidence in Iran, 2003-2009: a time trend province-level study. Asian Pac J Cancer Prev 2014;15:623-7. [DOI] [PubMed] [Google Scholar]
- 21.Ghoncheh M, Mohammadian-Hafshejani A, Salehiniya H. Incidence and Mortality of Breast Cancer and their Relationship to Development in Asia. Asian Pac J Cancer Prev 2015;16:6081-7. [DOI] [PubMed] [Google Scholar]
- 22.Ghoncheh M, Mirzaei M, Salehiniya H. Incidence and Mortality of Breast Cancer and their Relationship with the Human Development Index (HDI) in the World in 2012. Asian Pac J Cancer Prev 2015;16:8439-43. [DOI] [PubMed] [Google Scholar]
- 23.Human development report 2013: the rise of the South. Human Progress in a Diverse World. Available online: http://hdr.undp.org/en/2013-report
- 24.Bray F, Jemal A, Grey N, et al. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol 2012;13:790-801. [DOI] [PubMed] [Google Scholar]
- 25.Keyghobadi N, Rafiemanesh H, Mohammadian-Hafshejani A, et al. Epidemiology and trend of cancers in the province of Kerman: southeast of Iran. Asian Pac J Cancer Prev 2015;16:1409-13. [DOI] [PubMed] [Google Scholar]
- 26.Mazor KM, Roblin DW, Williams AE, et al. Health literacy and cancer prevention: two new instruments to assess comprehension. Patient Educ Couns 2012;88:54-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.DeLancey JO, Thun MJ, Jemal A, et al. Recent trends in Black-White disparities in cancer mortality. Cancer Epidemiol Biomarkers Prev 2008;17:2908-12. [DOI] [PubMed] [Google Scholar]


