Abstract
Objective
The objective of this study was to determine whether the Minimum Data Set (MDS) 3.0 discharge record accurately identifies hospitalizations and deaths of nursing home residents.
Design
We merged date of death from Medicare enrollment data and hospital inpatient claims with MDS discharge records to check whether the same information can be verified from both the sources. We examined the association of 30-day rehospitalization rates from nursing homes calculated only from MDS and only from claims. We also examined how correspondence between these 2 data sources varies across nursing homes.
Settings
All fee-for-service (FFS) Medicare beneficiaries admitted for Medicare-paid (with prospective payment system) skilled nursing facility (SNF) care in 2011.
Results
Some 94% of hospitalization events in Medicare claims can be identified using MDS discharge records and 87% of hospitalization events detected in MDS data can be verified by Medicare hospital claims. Death can be identified almost perfectly from MDS discharge records. More than 99% of the variation in nursing home–level 30-day rehospitalization rate calculated using claims data can be explained by the same rates calculated using MDS. Nursing home structural characteristics explain only 5% of the variation in nursing home–level sensitivity and 3% of the variation in nursing home–level specificity.
Conclusion
The new MDS 3.0 discharge record matches Medicare enrollment and hospitalization claims events with a high degree of accuracy, meaning that hospitalization rates calculated based on MDS offer a good proxy for the “gold standard” Medicare data.
Keywords: Sensitivity, specificity, Minimum Data Set, Medicare, hospitalization
Over the past decade, hospitalizations from skilled nursing facilities (SNFs) received considerable attention of researchers and policy makers. Hospitalizations are widely used in the nursing home (NH) literature1–7 and are known to be frequent,8 costly,9 and often preventable.10,11 In particular, between 2000 and 2006, 30-day re-hospitalization rates of Medicare beneficiaries newly discharged to SNF rose from 16% to 20% and for prior NH residents the increase went from 22% to 27%, at an estimated total cost to Medicare of $4.34 billion in 2006.3 The Medicare Payment Advisory Commission (MedPAC), maintains that rehospitalizations are a symptom of dysfunction in the continuity of care and represent quality problems. As a result, the Affordable Care Act proposed rehospitalization as a quality measure for the health care system in general, one that could be used to compare hospitals. Additionally, after October 1, 2012, section 3025 of the 2010 Affordable Care Act fined hospitals with higher than expected readmission rates.12,13 Because approximately 30% of all Medicare hospitalizations are discharged to SNFs,14 re-hospitalization from SNFs are likely to play a key role in hospitals’ discharge decisions under such payment mechanisms.
There is now increasing pressure to adopt rehospitalization from SNFs as a quality measure for NHs, meaning that timely calculation of this rate has become increasingly important. Currently, hospitalizations of Medicare beneficiaries are calculated from Medicare claims, which are regularly updated but can lag by as much as a year before they are complete and adjudicated. Besides the time lag, Medicare claims data are not available for the Medicare Advantage (MA) patients, a growing percentage of all Medicare beneficiaries. As a result of the Medicare Modernization Act in 2003 that raised payments to MA plans for serving more medically complex and frail beneficiaries, the MA population in NH has doubled over the past 10 years and has been projected to continue to rise even further.15 Thus, there is a growing need for an alternative data source to identify hospitalizations of NH patients.
The MDS, first implemented in 1990 in response to the Nursing Home Reform Act of 1987, has been actively used in creating quality measures since its inception.16–20 In October 2010, the Centers for Medicare and Medicaid Services implemented version 3.0 of the Minimum Data Set (MDS 3.0) in all certified NHs in the United States. The MDS was updated from the 2.0 version primarily because of concerns about the reliability, validity, and clinical relevance of its content.21 Nursing facilities submit the MDS data nightly or weekly and these are then used to update NH quality measures quarterly for public reporting.
With the introduction of MDS 3.0, complete resident assessments have been required on discharge (not only filing a tracking form). This feature has the potential to significantly improve the ability of the MDS to accurately measure quality at the NH level, as patients’ change in function and other clinical areas can be calculated. This article investigates the accuracy of the MDS discharge record in identifying a hospitalization event among newly admitted fee-for-service patients as compared to Medicare claims. The rationale for undertaking these analyses is as follows: (1) identification of hospitalizations using MDS permits the calculation of hospitalization rates in a timely manner based on MDS data only, and (2) assuming that such accuracy holds for discharge records for all types of patients, an MDS-based hospitalization rate allows calculation of hospitalization rates for all NH residents, including MA and young Medicaid (non-Medicare) patients for whom these rates cannot be calculated using Medicare claims.
Methods
We merged individual-level data for 2011 from 3 sources: (1) Medicare enrollment files, (2) Minimum Data Set (MDS), and (3) Medicare hospital inpatient and outpatient claims. We used the Online Survey, Certification, and Reporting system and LTCfocus.org data for NH characteristics. The research protocol was approved by the Brown University institutional review board.
Approximately 3.7 million individuals had at least one MDS assessment in 2011. We identified a cohort of patients who were admitted as Medicare-paid SNF patients after an acute hospitalization event who had had no previous MDS record within the past 3 months to ensure that they were not permanent NH residents. To ensure that all the patients in our cohort were Medicare-paid SNF patients, we dropped all individuals whose first or second assessment was not part of a prospective payment system (PPS) 5-day assessment. We also dropped all the MA patients because claims data are not available for these individuals. We excluded 1,009,164 individuals who were either managed care beneficiaries or individuals without PPS 5-day assessment. We also excluded 174,564 individuals who first entered an NH in December 2011, because we could not track them for 30 days following admission using 2011 data. Our final cohort consisted of 1,056,330 Medicare beneficiaries who were admitted from a hospital to an SNF, and who had at least one MDS assessment first initialized between January 1, 2011, and November 30, 2011 (see Appendix Table 1). This patient sample is associated with 6.3 million MDS assessments of which 1.4 million were discharge assessments. We further identified 862,555 hospital inpatient and 68,445 outpatient claim records that occurred after the first MDS assessment claims for the individuals in this study.
Appendix Table 1.
Reasons for Excluding Individuals From the Study Cohort
| Reasons for Exclusion | No. of Individuals Excluded | No. Remaining in Sample |
|---|---|---|
| Individuals with an MDS assessment during 2011 | 3,725,433 | |
| Baseline assessment year of entry is before 2011 | 1,377,770 | 2,347,663 |
| Age <65 y | 50,234 | 2,297,429 |
| Baseline assessment month is December 2011 | 174,564 | 2,122,865 |
| First assessment identified as reentry | 57,371 | 2,065,494 |
| 1st or 2nd assessment is not PPS 5-day assessment | 652,558 | 1,412,936 |
| Did not match the enrollment data or we could not find qualifying hospitalization claim | 317,727 | 1,095,209 |
| Any sign of HMO involvement | 38,879 | 1,056,330 |
HMO, health maintenance organization; MDS, Minimum Data Set; PPS, prospective payment system.
We focused on 3 types of MDS discharge records: acute (if acute hospital), nonacute (if psychiatric hospital or Mental Retardation/Developmental Disabilities facility), and death (if deceased). We categorized claims records into 2 groups: inpatient and outpatient (in case of emergency room visit or observation unit stay without a corresponding inpatient admission). We also identified death from enrollment records. We compared the information on patients’ discharge disposition from MDS and Medicare data in 2 ways. First, we identified all MDS discharge records within 30 days following SNF admission and compared them with the Medicare data. Re-hospitalization events from the MDS discharge code were verified using Medicare claims if there was a hospitalization claim within 3 days of the date of the discharge assessment. Deaths noted on the discharge record were verified using vital status on the enrollment record. Second, we identified all Medicare claim records within 30 days following SNF admission and “verified” these records using the MDS discharge records. Rehospitalization events were verified using MDS records if there was an MDS discharge code within 3 days of the discharge assessment date.
The remainder of our analysis is based on 2 separate resident-level binary indicators of 30-day rehospitalization for the study cohort based on MDS acute hospitalization discharge records and Medicare claims. We aggregated these data to calculate nursing facility–level 30-day rehospitalization rates based on MDS and based on claims and showed the statistical association between these 2 rates. We estimated linear regression models between NH-level Medicare inpatient claims–based 30-day rehospitalization rates and NH-level MDS-based 30-day rehospitalization rates without a constant term and used number of individuals in corresponding facility as a weighting factor.
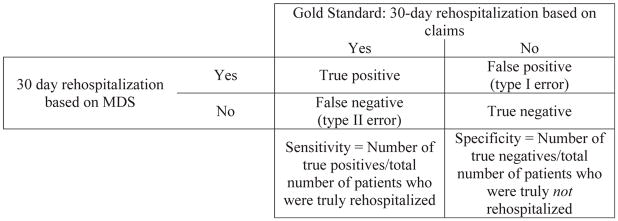
We computed the sensitivity and specificity of the MDS-based 30-day rehospitalization measure using the hospital claims–based measure as the gold standard. Figure 1 shows how sensitivity and specificity have been defined. Sensitivity is defined as the ratio of the number of individuals with 30-day rehospitalizations correctly identified by MDS and the true number of individuals with 30-day hospitalization (indicated by claims). Specificity is defined as the ratio of the number of individuals without any 30-day re-hospitalization correctly identified by MDS and the true number of individuals without any 30-day rehospitalization. Thus, if MDS-based rehospitalization coincides with claims-based rehospitalization perfectly, both specificity and sensitivity will be 100%.
Fig. 1.
Defining sensitivity and specificity of 30 day rehospitalization based on MDS 3.0.
Finally, we calculated the sensitivity and specificity of the MDS-based rehospitalization from NH for each nursing facility and examined whether these varied with NH characteristics by using linear regression with NH characteristics as the independent variables. Our null hypothesis was that variations in sensitivity and specificity across NHs are random and are not associated with structural NH characteristics.
Results
Table 1 shows how MDS discharge records can be verified by Medicare claims and enrollment records; 86.7% of MDS discharges indicating acute rehospitalization were verified with Medicare claims data based on the presence of a claim within 3 days. Among the relatively small number of MDS discharges that indicated re-hospitalization events in a nonacute setting, 80.7% could be verified with a Medicare claim, but most claims (60%) were for inpatient hospitalizations, whereas only 20.7% were verified by outpatient claims. MDS discharge records indicating death were extremely accurate, with 99.8% of such discharge records corresponding to the date of death on the Medicare enrollment files.
Table 1.
Verification of MDS Discharge Records and Medicare Claims Records Within 30 Days of SNF Admission Using Alternative Source
| Verifying MDS Discharge Records Using Medicare Claims and Enrollment Records
| ||||
|---|---|---|---|---|
| Discharge Code From MDS | Total No. of Discharge Records | % of Discharge Codes Verified by Medicare Claim Type
|
||
| Inpatient Claims | Outpatient Claims | Any Medicare Claims/Enrollment | ||
| Acute | 216,674 | 86.2 | 0.5 | 86.7 |
| Nonacute | 4,760 | 60.0 | 20.7 | 80.7 |
| Dead | 33,803 | — | — | 99.8 |
| Verifying Medicare Rehospitalization Claims Using MDS Discharge Records
| ||||
|---|---|---|---|---|
| Type of Medicare Claims | No. of Claims Originated From SNF (% of All Claims) | % of Claims Identified as From SNF That Can Be Verified by MDS Records
|
||
| Acute | Nonacute | All | ||
| Inpatient | 202166 (78.7) | 92.9 | 1.5 | 94.3 |
| Outpatient | 2,597 (36.2) | 47.7 | 38.2 | 85.9 |
MDS, Minimum Data Set; SNF, skilled nursing facility.
The lower panel of Table 2 presents the results of our examination of the extent to which Medicare claims correspond to MDS discharge records. We focused on the hospitalizations having Medicare claims that originated from the NH (ie, patients for whom there is no evidence from MDS that they were discharged to home or any other care settings before that claim). Of all these Medicare inpatient claims within 30 days of SNF admission, 94.4% had a corresponding MDS discharge record, all but 1.5% were MDS discharge records indicating rehospitalization in an acute hospital. Finally, for outpatient Medicare claims that are indicative of an observation stay in hospital, 85% could be verified with MDS discharge records. For these claims, 47.7% corresponded to an MDS discharge record, indicating acute re-hospitalizations, with an additional 38.2% verified by MDS discharge records indicating nonacute rehospitalizations.
Table 2.
Sensitivity and Specificity of 30-Day Rehospitalization Indicator Based on MDS 3.0
| All | Gold Standard 1: 30-Day Rehospitalization Based on Inpatient Claims
|
Gold Standard 2: 30-Day Rehospitalization Based on Inpatient and Outpatient Claims
|
||||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||
| All | 1,056,330 | 199,215 | 857,115 | 209,159 | 847,171 | |
| 30-day rehospitalization based on MDS | Yes | 194,034 | 167,478 | 26,556 | 173,964 | 20,070 |
| No | 862,296 | 31,737 | 830,559 | 35,195 | 827,101 | |
| Sensitivity = 84.1 | Specificity = 96.9 | Sensitivity = 83.2 | Specificity = 97.6 | |||
MDS, Minimum Data Set.
As can be calculated from the numbers in Table 2, 30-day rehospitalization rate is 18.4% if calculated from the MDS, 18.9% if calculated based on inpatient claims, and 19.8% if calculated based on both inpatient and outpatient claims.
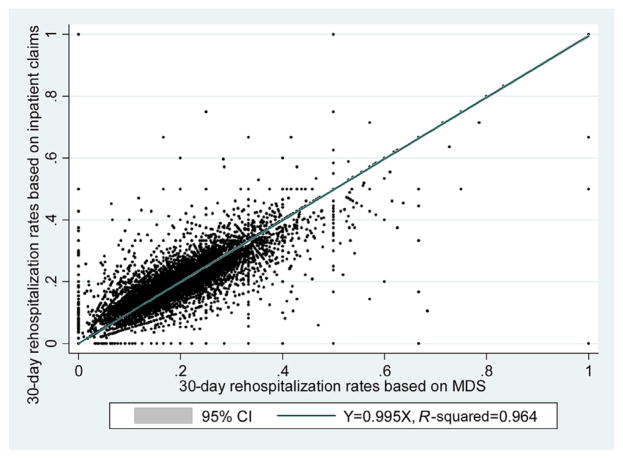
Figure 2 plots NH-level 30-day rehospitalization rates calculated using inpatient claims data relative to 30-day rehospitalization rates calculated using acute hospitalization discharge records from MDS. If we fit a line without a constant term, approximately 96% of the variation in NH-level claims-based 30-day rehospitalization rates can be explained by the MDS rate. The estimated correlation coefficient is 0.995. The 95% confidence interval is 0.992 to 1.000, which implies that we cannot reject the null hypothesis of one-to-one correspondence between claims and MDS-based 30-day rehospitalization rates at the 5% level of significance.
Fig. 2.
Scatter plot of NH–level 30-day rehospitalization rates calculated from inpatient claims data onto rates calculated from MDS data. The 95% confidence interval (CI) of this coefficient using robust SE is 0.992–1.000. Estimated coefficient is 0.962 and R2 is 0.93 if we do not use number of patients in the NH as weighing factor.
Table 2 presents the sensitivity and specificity of the MDS-based 30-day rehospitalization indicator using 2 alternative definitions of the gold standard: the 30-day rehospitalization measure based only on inpatient claims and that based on both inpatient and outpatient claims (adding in the observation stays). As can be calculated from Table 2, the 30-day rehospitalization rate is 0.184 if calculated from MDS, 0.189 if calculated based on inpatient claims, and 0.198 if calculated based on both inpatient and outpatient claims. When this gold standard is defined based only on inpatient claims, sensitivity is 84% and specificity is 97%. When the gold standard includes outpatient observation stays, sensitivity decreases by approximately 1 percentage point and specificity increases by approximately 1 percentage point.
Table 3 presents the association of NH-level sensitivity/specificity and NH facility characteristics estimated using linear regression model. Under both definitions of gold standard, the SD of NH sensitivity rate is approximately 18% and that of specificity rate is 5%. As expected, both these rates are largely unrelated to NH characteristics. Only approximately 5% of the variation in sensitivity and 3% variation in specificity can be explained by NH characteristics. Sensitivity is found to be associated with hospital affiliation, occupancy rate, and number of admissions per bed. Specificity is found to be associated with hospital affiliation, nursing care hours per patient per day, and the proportion of admissions for African American patients. There is no statistical association between specificity/sensitivity and key NH structural characteristics, such as size, payer composition, availability of nursing staff, ownership status, and patient acuity. As a robustness check, we found similar results restricting the analysis to NHs with more than 30 patients in our sample (see Appendix Table 2).
Table 3.
Regression of Sensitivity and Specificity Rates of 30-Day Rehospitalization Indicator Based on MDS Onto Nursing Home Characteristics
| Gold Standard 1: 30-Day Rehospitalization Based on Inpatient Claims
|
Gold Standard 2: 30-Day Rehospitalization Based on Inpatient and Outpatient Claims
|
|||
|---|---|---|---|---|
| (1)
|
(2)
|
(3)
|
(4)
|
|
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Current health deficiency | 0.00602 (.908) | −0.0166* (.0391) | 0.0132 (.785) | −0.0193* (.0381) |
| Total no. of beds | 0.00272 (.381) | 0.000355 (.763) | 0.00562 (.0615) | 0.000673 (.369) |
| Percentage of Medicaid patients | −0.0104 (.511) | −0.00530 (.179) | −0.0140 (.318) | −0.00603 (.0847) |
| Facility is part of chain | 0.244 (.557) | −0.0692 (.587) | 0.435 (.272) | −0.00894 (.947) |
| Facility is run for profit | −0.399 (.455) | −0.153 (.236) | −0.261 (.651) | −0.133 (.287) |
| Facility is hospital based | −7.396*** (6.39e–07) | 1.285*** (9.61e–07) | −8.128*** (3.75e–08) | 1.023*** (3.59e–06) |
| Resident acuity index | 0.293 (.153) | −0.0570 (.194) | 0.334 (.122) | −0.0594 (.165) |
| Ratio of registered nurses to total nurses | 4.461** (.00626) | 0.943* (.0334) | 4.277* (.0120) | 0.609 (.0973) |
| Total direct care hours per patient per day | −0.212 (.216) | 0.108*** (6.76e–05) | −0.173 (.335) | 0.0650** (.00731) |
| Occupancy rate | 0.113*** (3.90e–07) | 0.0110* (.0269) | 0.117*** (5.80e–07) | 0.00393 (.378) |
| % of admissions classified as low care | 0.0150 (.826) | −0.0112 (.560) | −0.00491 (.937) | 0.00250 (.908) |
| % of admissions female | 0.0220 (.347) | 0.00863 (.185) | 0.0187 (.403) | 0.0123* (.0213) |
| % of admissions black | 0.00387 (.806) | −0.0272*** (2.99e–09) | 0.0112 (.481) | −0.0275*** (4.06e–10) |
| % of admissions Hispanic | −0.0387 (.411) | −0.00663 (.0872) | −0.0337 (.416) | −0.00706 (.103) |
| No. of annual admissions per bed | −0.770*** (9.56e–11) | −0.0321 (.0576) | −0.727*** (1.37e–10) | −0.0323* (.0458) |
| Mean age | −0.0153 (.736) | 0.0285 (.0927) | −0.0291 (.510) | 0.0229 (.122) |
| Constant | 71.42*** (0) | 93.80*** (0) | 70.74*** (0) | 95.63*** (0) |
| n | 13,554 | 14,422 | 13,610 | 14,421 |
| R2 | 0.051 | 0.027 | 0.051 | 0.026 |
P values are in parentheses.
P < .01,
P < .05,
P < .1.
Appendix Table 2.
Regression of Sensitivity and Specificity Rates of 30-Day Rehospitalization Indicator Based on MDS Onto Nursing Home Characteristics (Using Nursing Homes With at Least 30 Patients)
| Variables | Gold Standard 1: 30-Day Rehospitalization Based on Inpatient Claims
|
Gold Standard 2: 30-Day Rehospitalization Based on Inpatient and Outpatient Claims
|
||
|---|---|---|---|---|
| (1)
|
(2)
|
(3)
|
(4)
|
|
| Sensitivity | Specificity | Sensitivity | Specificity | |
| Current health deficiency | 0.00821 (.860) | −0.0145* (.0419) | 0.00486 (.915) | −0.0158* (.0241) |
| Total no. of beds | 0.0104*** (.000383) | 0.000940 (.196) | 0.0117*** (7.53e–05) | 0.000207 (.658) |
| Percentage of Medicaid patients | −0.0148 (.321) | −0.000352 (.898) | −0.0180 (.225) | −0.000975 (.712) |
| Facility is part of chain | 0.458 (.189) | −0.0141 (.859) | 0.519 (.135) | −0.0296 (.706) |
| Facility is run for profit | 0.507 (.305) | −0.328** (.00414) | 0.803 (.103) | −0.229* (.0185) |
| Facility is hospital based | −8.385*** (0) | 0.803** (.00153) | −8.809*** (0) | 0.556* (.0122) |
| Resident acuity index | 0.212 (.140) | −0.0403 (.232) | 0.227 (.117) | −0.0410 (.183) |
| Ratio of registered nurses to total nurses | 2.671 (.142) | 0.616 (.120) | 2.471 (.165) | 0.558 (.0636) |
| Total direct care hours per patient per day | −0.368* (.0241) | 0.0874*** (.000182) | −0.372* (.0201) | 0.0382 (.0758) |
| Occupancy rate | 0.0810*** (.000265) | 0.00906* (.0264) | 0.0805*** (.000186) | 0.000893 (.794) |
| % of admissions classified as low care | −0.0575 (.351) | −0.0195 (.299) | −0.0719 (.256) | −0.00122 (.942) |
| % of admissions female | 0.00824 (.691) | 0.0181*** (.000985) | 0.00219 (.920) | 0.0175*** (.000310) |
| % of admissions black | −0.000714 (.957) | −0.0268*** (1.16e–08) | 0.00622 (.647) | −0.0261*** (6.31e–10) |
| % of admissions Hispanic | −0.0353 (.286) | −0.0240*** (3.67e–06) | −0.0247 (.432) | −0.0220*** (2.80e–07) |
| No. of annual admissions per bed | −0.629*** (1.33e–09) | 0.0248* (.0360) | −0.608*** (8.56e–10) | 0.0157 (.112) |
| Mean age | −0.0296 (.510) | 0.0396*** (.000272) | −0.0312 (.482) | 0.0363*** (8.40e–05) |
| Constant | 76.96*** (0) | 92.33*** (0) | 76.28*** (0) | 94.36*** (0) |
| n | 8983 | 8987 | 8986 | 8987 |
| R2 | 0.120 | 0.068 | 0.125 | 0.065 |
P values are in parentheses.
P < .01,
P < .05,
P < .1.
Discussion
This article compares MDS discharge records and Medicare claims records to ascertain the accuracy of MDS records and our ability to reliably calculate hospitalization rates, using only MDS data, occurring from nursing facilities. We found that approximately 94% of the hospitalization events in Medicare claims can be identified using MDS discharge records. We also found that 87% of hospitalization events detected in MDS data can be verified by claims data. Death can be identified almost perfectly from MDS discharge records. The 30-day rehospitalization rate is 18.4% if calculated from MDS and 18.9% if calculated from inpatient claims. Using Medicare acute inpatient hospitalizations originating from NH as the “gold standard,” the sensitivity of the MDS discharge record indicating a 30-day re-hospitalization is 84% and the specificity is 97%. When we create and compare NH-level, aggregated versions of 30-day rehospitalization rates derived from MDS and from the claims, we observe that 96% of the variation in the NH-level rehospitalization rates calculated from the Medicare claims can be explained by that calculated from MDS. We found that NH-level specificity and sensitivity are not directly related to key NH characteristics, such as size, payer composition, availability of nursing staff, ownership status, or patient acuity.
The MDS 3.0 has more complete discharge records and we see a clear improvement, particularly in ascertaining vital status on discharge. Mor et al22 found that 90% of the hospitalization events in Medicare claims were identified from MDS 2.0 in 2006 and a comparable figure based on MDS 3.0 is 94%. They also found that 80% of hospitalization events detected in MDS 2.0 for 2006 could be verified by claims data; the comparable figure from our analysis is 87%. This is a substantial improvement over the performance of the MDS 2.0 discharge record, based on published analysis from the past decade.
The correspondence between the types of hospital to which patients are discharged on the MDS with which type of provider submitted the corresponding Medicare claim is less than perfect, particularly because 98% of all hospital discharges are labeled acute. We calculated MDS-based 30-day rehospitalization rate using only acute hospital discharges, which increases by 0.2% points if we include nonacute hospital discharges. Interestingly, most current claims-based rehospitalization models ignore outpatient claims indicating an observation stay; however, 0.5% of the MDS hospital discharges correspond to outpatient observation day claims. Given the ongoing growth of observation stays and the possibility that hospitals use these in lieu of readmissions, consideration will have to be given to incorporating these types of claims into future claims-based measures of rehospitalization.23
Although MDS acute discharges overestimate the rates of re-hospitalization by 0.5 percentage points, 30-day rehospitalization rates at the nursing facility level from 2 different sources are highly correlated and the frequency of error is barely associated with NH characteristics. These findings imply that hospitalization rates calculated from MDS could be used as a provisional quality measure that could be used to rank the relative performance of nursing facilities with respect to rehospitalization. Because a growing number of Medicare beneficiaries are enrolled in MA plans, which do not submit claims, having a more comprehensive measure based on all admissions is particularly important. Indeed, in some heavily concentrated MA markets, some SNFs might specialize in caring for these patients and might not, therefore, have the requisite number of regular Medicare admissions for a claims-based rehospitalization rate to be calculated. However, it should be noted that an important deficit is that MDS-based hospitalization measures cannot identify 30-day rehospitalizations that occurred after discharge from the NH to any setting other than the hospital. That is, these measures are relevant only for rehospitalizations that are directly from the NH.
Our study has an important limitation in that we could not verify 13% of MDS hospital discharge records using inpatient and outpatient claims. Among the outpatient visits, we looked only at observation stays and ignored emergency room visits. It may be that facilities will complete the MDS even though they are not sure that patients will be sent back after a stay in the emergency room. These could also potentially be explained by internal rehabilitation admissions or other types of hospital visits. Nevertheless, magnitude of error is much smaller when pertaining to indicators of hospitalization. Another limitation of this study is that we focus only on newly admitted SNF patients and ignore the long-stay patients. We did this because among dual-eligible long-stay NH residents, as many as 20% to 30% of those hospitalized do not return on the Medicare SNF benefit, so that testing the correspondence between the 2 measure sources would be less complete. However, because NHs can be assumed to have better knowledge of their long-term patients, the incidence of error in reporting hospitalization of these patients might be lower.
Conclusion
The new MDS 3.0 discharge record matches Medicare enrollment and hospitalization claims events with a high degree of accuracy, meaning that individual-level indicators of hospitalization and NH-level hospitalization rates calculated based on the MDS offer a good proxy for the “gold standard” Medicare data.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Rahman M, Zinn JS, Mor V. The impact of hospital-based skilled nursing facility closures on rehospitalizations. Health Serv Res. 2013;48:499518. doi: 10.1111/1475-6773.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood) 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grabowski DC, Feng Z, Hirth R, et al. Effect of nursing home ownership on the quality of post-acute care: An instrumental variables approach. J Health Econ. 2013;32:12–21. doi: 10.1016/j.jhealeco.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirth RA, Grabowski DC, Feng Z, et al. Effect of nursing home ownership on hospitalization of long-stay residents: An instrumental variables approach. Int J Health Care Finance Econ. 2014;14:1–18. doi: 10.1007/s10754-013-9136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rahman M, Foster AD, Grabowski DC, et al. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013;48:1898–1919. doi: 10.1111/1475-6773.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahman M, Grabowski DC, Intrator O, et al. Serious mental illness and nursing home quality of care. Health Serv Res. 2013;48:1279–1298. doi: 10.1111/1475-6773.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Intrator O, Grabowski DC, Zinn J, et al. Hospitalization of nursing home residents: The effects of states’ Medicaid payment and bed-hold policies. Health Serv Res. 2007;42:1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grabowski DC, O’Malley AJ, Barhydt NR. The costs and potential savings associated with nursing home hospitalizations. Health Aff (Millwood) 2007;26:1753–1761. doi: 10.1377/hlthaff.26.6.1753. [DOI] [PubMed] [Google Scholar]
- 10.Intrator O, Zinn J, Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J Am Geriatr Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 11.Saliba D, Kington R, Buchanan J, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48:154–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- 12.Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act. JAMA. 2011;306:1794–1795. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- 13.Fontanarosa PB, McNutt RA. Revisiting hospital readmissions. JAMA. 2013;309:398–400. doi: 10.1001/jama.2013.42. [DOI] [PubMed] [Google Scholar]
- 14.MEDPac MPAC. A Data Book: Health Care Spending and the Medicare Program. Washington, DC: Medicare Payment Advisory Commission; 2009. [Google Scholar]
- 15.Gold MR, Jacobson G, Damico A, Neuman T. Medicare Advantage 2012 Data Spotlight: Enrollment Market Update. Washington, DC: Kaiser Family Fund; 2013. [Google Scholar]
- 16.Morris JN, Hawes C, Fries BE, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30:293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- 17.Mor V. A comprehensive clinical assessment tool to inform policy and practice: Applications of the minimum data set. Med Care. 2004;42:III50–III59. doi: 10.1097/01.mlr.0000120104.01232.5e. [DOI] [PubMed] [Google Scholar]
- 18.Zimmerman DR, Karon SL, Arling G, et al. Development and testing of nursing home quality indicators. Health Care Financ Rev. 1995;16:107–127. [PMC free article] [PubMed] [Google Scholar]
- 19.Werner RM, Konetzka RT, Kruse GB. Impact of public reporting on unreported quality of care. Health Serv Res. 2009;44:379–398. doi: 10.1111/j.1475-6773.2008.00915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Campaign O. Achieving improvement through nursing home quality measurement. Health Care Financ Rev. 2002;23:5. [PMC free article] [PubMed] [Google Scholar]
- 21.Rahman AN, Applebaum RA. The nursing home Minimum Data Set assessment instrument: Manifest functions and unintended consequences—past, present, and future. Gerontologist. 2009;49:727–735. doi: 10.1093/geront/gnp066. [DOI] [PubMed] [Google Scholar]
- 22.Mor V, Intrator O, Unruh MA, Cai S. Temporal and geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2. 0. BMC Health Serv Res. 2011;11:78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood) 2012;31:1251–1259. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]