Abstract
A ketogenic diet (KD) is a dietary approach to treat intractable epilepsy. The KD begins with hospitalization and the child and their parents can adapt to the KD for 1-2 weeks. Recently, various type of dietary intervention such as the modified Atkins diet (MAD) and the low glycemic index treatment (LGIT) have been performed. Since 2010, we carried out the KD, MAD, and LGIT for total of 802 patients; 489 patients (61%) for the KD, 147 patients (18.3%) with the MAD, and 166 patients (20.7%) for the LGIT. In this report, application of these dietary practices in Severance Hospital is shared.
Keywords: Intractable epilepsy, Ketogenic diet, Modified Atkins diet, Low glycemic index treatment
Introduction
Medical treatment for epilepsy includes antiepileptic medi-cation, epilepsy surgery and vagal nerve stimulation. But 30% of children remains with uncontrolled seizure. A ketogenic diet (KD) can be an alternative medical treatment for these children. In general, approximately 50-60% of children show 50% or more reduction in seizure, 15% of whom become seizure free after 6 months of diet treatment [1].
The KD can be traced back to the texts of Hippocrates at the 5th century BC. Wilder (1921) reported significant seizure control effect of the KD at first [2]. The KD is composed of high fat, moderate protein and restricted carbohydrate and it results in a state of ketosis. The most frequently used ratios of fat to non-fat (carbohydrate+protein) in the KD diet 4:1 and 3:1. To maintain strong ketosis state, 4:1 ratio is used and 3:1 ratio is used for under 1 year or older children to improve compliance with the KD. In order to maintain the 4:1 ratio of fat and non-fat (carbohydrate + protein), large amount of fat is needed from oils not only from the fat partially contained in a certain food.
The staple food of Asian countries is rice and fat contributes to 20% of total calories in regular rice-oriented diet. But in the KD, fat contributes to 90% of total calories. Incorporating high amount of fat into the diet is the main challenge to proceeding the KD.
Case
KD initiation
A child suffering with epilepsy is usually to initiate the KD. In our hospital, a KD team is composed of a physician, a registered nurse, and a registered dietitian. During the diet, the physician evaluates and manages complications of KD. Right after the physician, the head of the team, decides to start the KD program, the dietitian provides nutritional management to maintain the KD, and the nurse examines child for tolerance toward the KD diet and educate caregivers how to care child with the KD at home. Frequent communications between caregivers and the KD team are necessary to continue the KD program.
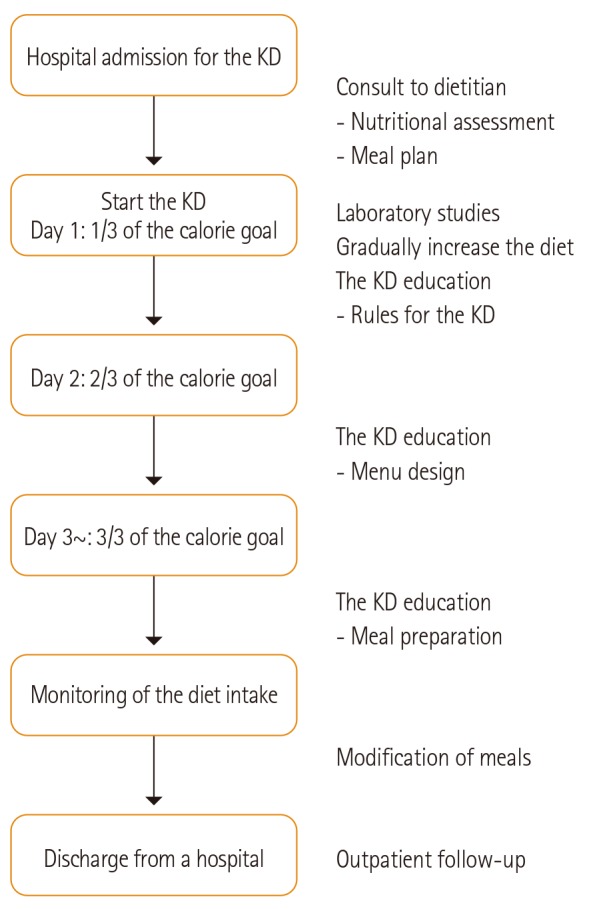
Our KD program starts without initial fasting. Total fat contents in a patient's meal is gradually increased within 3 days. On the first day the meals provide an 1/3 of energy of daily requirement with a desired ratio of major nutrients. On the second day, content of energy in the meals is increased to 2/3 of daily requirement and achieved to full energy requirements on the third day (Figure 1).
Figure 1. Protocol of the ketogenic diet (KD).
Meal plan
Before starting the KD, the dietitian evaluates the nutritional status of the child at the initial day and evaluates his or her ability to take food, activity level and growth pattern such as current height, weight and weight change.
For the meal planning, the dietitian has to decide nutritional requirement of energy and nutrient distribution. In general case, calories for the KD are allowed up to 85~95% of daily requirement. Total 90% of calories are from fat, 6~8% of calories are from protein and remaining calories are from carbohydrate. Protein can be adjusted by child's current weight.
For general case example, a meal plan for a five-year-old child, with 108 cm, 18 kg, PIBW 99.4%, has an energy goal of 1,200 kcal with 4:1 of fat and non-fat ratio. This goal is achieved by meals composed of 120 g of fat, 18 g of protein and 12 g of carbohydrate per, which makes the ratio of fat (120 g) to nonfat (30 g) is 4:1. Then these amounts from each nutrient is divided by the numbers of meal supply.
Menu design
The carbohydrate-rich foods such as rice, bread, grain and simple sugars are eliminated. One food is selected from each food group which is categorized to either meat, fish, vegetables, milk or fat sources. The amounts of each food are calculated in grams and the content of nutrients are analyzed to achieve a desired ratio based on the individual nutrient requirement. It is not easy for caregivers to calculate the amounts of each food in grams by themselves. For their convenience, the KD team provides them a computer program to calculate accurate amounts of foods and nutrients contents to minimize human errors. After calculation, the proportions of carbohydrate, protein, fat in calories, the desired ratio, and nutrient requirement of a patients are confirmed (Table 1). The meals are provided in accurate amounts by weighing food with digital precision scale.
Table 1. Example of the KD with the 4:1 ratio of fat and not-fat (For a five-year-old child).
| Food group | Amount, g | Carbohydrate, g | Protein, g | Fat, g | Calorie, kcal |
|---|---|---|---|---|---|
| Beef | 9 | 0.018 | 1.800 | 1.080 | 17.8 |
| Cheese | 8 | 0.440 | 1.464 | 1.936 | 25.6 |
| Broccoli | 15 | 0.750 | 0.750 | 0.045 | 5.0 |
| Milk | 31 | 1.550 | 0.868 | 1.023 | 18.9 |
| Almond | 6 | 1.182 | 1.116 | 3.252 | 35.9 |
| Olive oil | 14 | 0.000 | 0.000 | 14.000 | 128.9 |
| Sesame oil | 19 | 0.076 | 0.019 | 18.886 | 173.9 |
| Sum | 102 | 4.016 | 6.017 | 40.22 | 406.0 |
| Ratio | 1 | 4.009 | |||
KD: Ketogenic diet, Total calories: 400 kcal from 4g of carbohydrate, 6g of protein and 40g of fat.
Source: 8th revision Standard food composition table, Rural development administration (ROK) [7].
Fat sources
In order to achieve the ideal ratio, more fat from vegetable oils is needed not only from foods but also from others. In our hospital, we usually supply olive oil as a main fat source. In order to improve the composition of fatty acids, we combine olive oil with sesame oil, perilla seed oil, canola oil and others. We also provide nuts in order to improve flavor of meal and reduce the amount of vegetable oils.
Meal preparation
In our hospital there are three basic types of formulation; all-in-one, separated and semi-separated types. All-in-one type is a blended or pureed form for the children at initial stage of the KD, and also for children who have difficulties in chewing and swallowing. All-in-one type has an advantage of maintaining the desired ratio of the meal and does not affect feeding time which can be extended by meal tolerance of a child. However users often complain about the small volume of the meal.
Separated type is for children who have enough abilities to chew and swallow. It is generally recommended to finish the meal completely within 30 minutes. But when the child has difficulties in eating oils, it can be mixed with nuts and milk. This is classified as a semi-separated type.
Liquid type formula is used for bottle-feeding infants and tube-feeding children who are fed by using a nasogastric tube or a gastrostomy tube.
The dietitian monitors children's tolerance and preference of the KD in order to modify consistency, palatability and formulation of the diet.
Rules for the KD
Maintaining the desired ratio of fat and non-fat is the most important thing in the KD. Eating all foods in each meal should be completed within 30 minutes. Meals are planned based on individual nutrient requirement which is divided by number of meal supply. If the child wants snacks, meal and snacks are planned based on the required calories and ratio. Multivitamins and minerals including calcium and vitamin D supplements are needed every day during the KD.
Education of the KD
The dietitian provides education to parents of the child during the period of the KD. The education is very important because the child generally stays in the hospital for 1-2 weeks and should continue the KD at home.
Discharge plan
After returning home, follow-up monitoring for the KD is needed at 1, 3, 6, 12, 18, and 24 month intervals to control seizure and metabolic complications [3]. The most common complications in the KD are gastrointestinal discomforts including nausea, vomiting, constipation and diarrhea. High fat diet can affect on serum levels of lipid profile and can results in dyslipidemia such as hypertriglyceridemia and hypercholesterolemia. Late onset complications of the KD are infectious disease, osteopenia and renal stones [4].
The dietary treatment continues 2-3 years in order to achieve seizure control. The ratio of fat and non-fat decreases slowly from 4:1, 3:1, 2:1 to normal diet over 2-3 months. The dietitian needs to keep in touch with the parents of the child to adjust dietary therapy.
Dietary practices for the KD
We have carried out the KD, modified Atkins diet (MAD), and low glycemic index treatment (LGIT) since 2003, 2009, and 2010, respectively. Since 2010, we have carried out diet for seizure control for a total of 802 patients; 489 patients (61%) for the KD, 147 patients (18.3%) for the MAD, and 166 patients (20.7%) for the LGIT.
Discussion
Recently, other dietary therapy such as MAD and LGIT are suggested for refusers of the traditional KD to improve tolerance of the KD.
Percentage of calories from fat in the MAD is lower than that of the KD, but the MAD still contains high fat and low carbohydrate. But it contains sufficient protein unlike the KD. The percentages of calories are 75-80% from fat, 17% from protein, and remains from carbohydrate. The ratio of fat and non-fat in the MAD is almost 1.5-2:1 [5]. In our cases, the MAD provides sufficient amount of protein so this diet is beneficial for children who complain about starvation during the period of the KD therapy.
For the LGIT, food items which have glycemic index (GI) of 50 or lower are selected. GI indicates how quickly blood sugar levels rise after eating a particular type of foods. For the LGIT, carbohydrates need to be limited to 40-60 g per day and percentages of calories are 60% from fat, 30% from protein, and 10% from carbohydrate and the ratio of fat and non-fat in the diet is almost 0.66:1 [6] (Table 2). In our cases, the ratio of fat and non-fat of the LGIT is close to that of general diet so that a child and parents feel more comfortable with practicing the diet.
Table 2. Comparison of macronutrient composition of dietary therapy (KD, MAD, LGIT) Example of 1200 kcal.
| Ratio | Macronutrient composition | ||||||
|---|---|---|---|---|---|---|---|
| g/day | % of total kcal | ||||||
| Carbohydrate | Protein | Fat | Carbohydrate | Protein | Fat | ||
| KD | 4:1 | 12 | 18 | 120 | 4.0 | 6.0 | 90.0 |
| MAD | 1.7:1 | 10.0 | 51.5 | 106.2 | 3.3 | 17.1 | 79.6 |
| LGIT | 0.66:1 | 30 | 90 | 80 | 10.0 | 30.0 | 60.0 |
KD:Ketogenic diet, MAD: modified Atkins diet, LGIT: low glycemic index treatment.
In our hospital, 61% of diet treatment for intractable epilepsy is the KD, 18.3% is the MAD and 20.7% is the LGIT since 2010.
The KD is suggested for inducing strong ketosis, the MAD is provided for older children who complain about starvation with the KD and the LGIT is suggested as more comfortable diet treatment for intractable epilepsy.
Footnotes
Conflict of interest: The authors have declared no conflict of interest.
References
- 1.Kossoff EH. Efficacy of ketogenic dietary therapy: what is the evidence? In: Neal E, editor. Dietary treatment of epilepsy: practical implementation of ketogenic therapy. Chichester: Wiley-Blackwell; 2012. pp. 24–33. [Google Scholar]
- 2.Neal E. Introduction to the ketogenic diet and other dietary treatments. In: Neal E, editor. Dietary treatment of epilepsy: practical implementation of ketogenic therapy. Chichester: Wiley-Blackwell; 2012. pp. 3–10. [Google Scholar]
- 3.Kang HC, Kim HD. Diet therapy in refractory pediatric epilepsy: increased efficacy and tolerability. Epileptic Disord. 2006;8:309–316. [PubMed] [Google Scholar]
- 4.Kang HC, Chung DE, Kim DW, Kim HD. Early- and late-onset complications of the ketogenic diet for intractable epilepsy. Epilepsia. 2004;45:1116–1123. doi: 10.1111/j.0013-9580.2004.10004.x. [DOI] [PubMed] [Google Scholar]
- 5.Kossoff EH, Krauss GL, McGrogan JR, McGrogan JM. Efficacy of the Atkins diet as therapy for intractable epilepsy. Neurology. 2003;61:1789–1791. doi: 10.1212/01.wnl.0000098889.35155.72. [DOI] [PubMed] [Google Scholar]
- 6.Pfeifer HH, Lyczkowski DA, Thiele EA. Low glycemic index treatment: implementation and new insights into efficacy. Epilepsia. 2008;49(Suppl 8):42–45. doi: 10.1111/j.1528-1167.2008.01832.x. [DOI] [PubMed] [Google Scholar]
- 7.Rural Development Administration (KR) Standard food composition table. 8th rev. ed. Suwon: Rural Development Administration; 2011. [Google Scholar]


