Abstract
Hospital readmissions can negatively impact cost and patient outcomes. Predictors of 30-day readmissions have been primarily identified using medical claims data. Reported here are results of a patient survey developed as part of regular hospital quality assurance activities. Two-thirds of patients reported good discharge experiences but were still readmitted. One-third of patients discharged had a post-discharge doctor appointment scheduled; half were readmitted before that scheduled appointment. Results suggest post-discharge experiences could be improved, especially the timing of follow up doctor appointments. Identified weaknesses in the survey process highlight need for engagement of survey methodologists in efforts to understand patient experiences.
Keywords: Hospital readmissions, Patients discharge, Survey research
Introduction
In the mid-1980s, hospital 30-day readmission rates were >20% (Anderson & Steinberg, 1984), and similar rates continue today (Jencks, Williams, & Coleman, 2009; (MEDPAC, 2007). These readmissions are of concern because of their impact on cost and patient outcomes. The circumstances surrounding hospital readmissions are not fully known; poor care coordination after discharge (MEDPAC, 2007) and poor follow-up care (Hernandez et al., 2010; Jencks, Williams, & Coleman, 2009)(Jencks, Williams, & Coleman, 2009) are considered two primary factors.
Other patient and clinical factors that predict readmission have been identified by research (Bohannon & Maljanian, 2003; Jasti, Mortensen, Obrosky, Kapoor, & Fine, 2008; Krumholz et al., 2000). For example, older adults compared to younger adults (Robinson, Howie-Esquivel, & Vlahov, 2012; Wier, Barrett, Steiner, & Jiang, 2011); females compared to males (Robinson et al., 2012), patients of lower socio-economic status (SES) compared to those with higher SES (Jasti et al., 2008; Wier et al., 2011), and those who have shorter hospital stays compared to longer stays (Carey & Lin, 2014) have all been shown through research to elevate risk for a readmission soon after a hospital discharge.
Although a large body of research has developed and tested a variety of interventions targeting “root causes” of 30-day hospital readmissions (Boutwell & Hwu, 2009; Coleman, Parry, Chalmers, & Min, 2006; Jack et al., 2009; Naylor et al., 1999), national rates averaged 18.4% (Gerhardt et al., 2013) in 2012, with Arkansas hospitals experiencing higher 30-day readmission rates than the nation as a whole (Rau, 2012). These readmissions result in an excess healthcare expenditure of $12 billion to $17 billion annually (MEDPAC, 2007), and put patients at risk for hospital-acquired infections, medical errors, and overall deconditioning (Jahnigen, Hannon, Laxson, & LaForce, 1982). The federal government has implemented several programs (public reporting of 30-day hospital readmission rates and penalties for higher than average 30-day readmission rates for certain conditions) to help incentivize hospitals to reduce their readmissions rates. Additionally, federal resources have been allocated to support Community-based Care Transitions Programs, through which community-based organizations and hospitals collaborate to smooth transitions of patients back to their home (or other community settings) to minimize the risk of readmission (CMS, no date). However, in 2012, more than 1400 hospitals failed to reduce their readmission rates to prescribed levels, resulting in more than $280 million in penalties (Rau, 2013).
The persistently high 30-day readmission rates among many US hospitals, and the societal and patient impacts, highlight the need for continued study to better understand factors which affect rapid patient readmissions. Much of the previous research in this area has relied on analysis of medical claims data. In contrast, this study obtained and analyzed existing readmitted patient survey data collected for administrative purposes, with survey responses reported herein.
Methods
This observational study made use of existing administrative data [hereafter referred to as the survey dataset] to describe the experience of readmitted patients between the initial hospitalization and the re-hospitalization within 30 days and to explore the associations between patient demographic and clinical characteristics and patient post-discharge experience.
Data Source
After authors obtained study approval from the [Institution Name] Institutional Review Board in 2013 (described below), they obtained the survey dataset from the [Institution Name] University Medical Center Quality Assurance (QA) staff. The limited dataset excluded direct patient identifiers but contained patient characteristics [e.g., age, gender] and some protected health information [e.g., admission dates] on completers and non-completers, and survey responses of completers) in order to complete the analysis described herein.
Setting and Routine Quality Assurance Activities
The [Institution Name] University Medical Center is a teaching hospital and a Level 1 trauma center based in [Name of City, State], a moderately-sized capital city of a rural Southern state. The University Medical Center has 437 patient beds, and, according to federal Hospital Compare website (www.medicare.hospitalcompare.gov) from 2009 to 2012, had a 30-day hospital readmission rate of 18.3% for patients with acute myocardial infractions, 23.0% for patients with congestive heart failure, and 17.6% for patients with pneumonia.
As part of its on-going QA activities and internal efforts to address high readmission rate rates, University Medical Center QA staff developed a survey to obtain information from patients who had returned to the hospital within 30 days of a discharge. The survey instrument they developed consisted of three sections. Sections 1 and 2 sought detail on the patient, the index admission and the readmission extracted from the existing medical record by QA or discharge planning staff. Section 3 contained questions which sought detail on patients’ discharge and post-discharge experience, including questions asking about specific factors that have been shown to be associated with readmissions (e.g., poor care coordination after discharge (MEDPAC, 2007) and poor follow up care (Hernandez et al., 2010; Jencks et al., 2009)). Questions were asked by and patient responses were recorded by the staff administering the surveys.
From July to December 2012, QA staff identified 1061 patients who had been readmitted to the University Medical Center within 30 days of a previous hospitalization using daily automated searches of electronic medical records. Staff extracted existing data from the medical records on the identified patients, and then attempted, in-person, to invite all identified patients to complete the survey. If patients were reached, invited, and agreed to participate, staff asked patients the questions and recorded the answers on the survey form. Staff made several attempts to reach patients who on initial tries were not in their rooms or available to discuss the survey.
Study Sample
The analysis of the survey dataset was restricted to adult (age ≥ 18 years) patients readmitted between July and December 2012 to the University Medical Center within 30 days of a discharge. Non-adults (age < 18 years) were excluded as factors associated with their readmission are likely to be different than those of adults. Those whose ages were missing eliminated ability to verify adult status were and also excluded from the analysis. Readmission was defined as readmissions within 30 days of a hospital discharge as federal initiatives are defining readmissions in this way (CMS, no date). Patients with more than 30 days between the two admissions and those patients for whom data were not available to calculate the days between their admissions were excluded from the analysis.
Measures
The study used many patient and clinical characteristics from Sections 1 and 2 of the survey (data obtained by staff from the medical record) and patient responses to survey questions from Section 3 on discharge and post-discharge experience. These are listed in Tables 2.
Table 2.
Patient Discharge and Post Discharge Experience
| n | % | |
|---|---|---|
| Before last discharge, patient … | ||
| Agreed on clear discharge goals | 401 | 75.7 |
| Got readable discharge care plans | 412 | 77.7 |
| After last discharge, patient… | ||
| Understood self-care | 418 | 78.9 |
| Understood Rx | 422 | 79.6 |
| Able to get Rx filled | 393 | 74.2 |
| Knew when to contact DR | 423 | 79.8 |
| Able to discuss concerns with DR/Hospital | 352 | 66.4 |
| Had transport for follow up appointment | 425 | 80.2 |
| Saw DR between index and readmit | 167 | 31.3 |
| Had change in Rx | 41 | 7.7 |
Notes:
Rx= Prescription Medications
DR=Doctor
n=number
Several variables (length of stay, days between admissions, high/low length of stay, high/low SES, and elderly/non-elderly) were calculated from data available in the survey dataset. Length of stay of the initial hospitalization was calculated by counting the days between the date of the initial admission and the date of the initial discharge. Those with lengths of stay greater than the average length of stay (6.4 days) were considered to have a high length of stay. Days between admissions was calculated by counting the days between the date of initial discharge and date of the readmission. The SES variable was constructed using insurance status, with low SES defined as having Medicaid only, being dually eligible for Medicaid and Medicare, or having no insurance (self-pay) (Wier et al., 2011). Elderly was defined as age ≥ 65 years old. This age was used as a cut point as federal initiatives targeting hospital readmissions are focusing on Medicare beneficiaries, who become eligible for Medicare primarily at age 65 (CMS, no date).
Analysis
Descriptive statistics (e.g., frequency, mean, and standard deviation) were used to characterize the readmitted patients and summarize their experience at discharge and between the initial hospitalization and their readmission.
Bivariate analysis using logistic regression was used to compare each patient demographic and clinical characteristic with each patient discharge and post-discharge experience (note: all discharge / post-discharge experience survey questions were dichotomous – presence or absence of the experience). Multivariate logistic regression was used to explore the association between each patient demographic and clinical characteristics and patient discharge and post-discharge experience, after controlling for the other characteristics (e.g. all four variables were entered into a single model for each discharge and post-discharge experience).
Patient characteristics considered in the bivariate and multivariate models included elderly, male, and low SES. The clinical characteristic included in the models was long-stay during the index hospitalization. These were selected for inclusion as previous research (discussed in the introduction section) has shown that these characteristics are associated with hospital readmissions.
The alpha level for significance was set at 0.05. All statistical analysis was conducted using Stata v12 (StataCorp LP, College Station, TX).
Narrative responses made to the one open-ended question were coded and analyzed with content analysis. Common themes were then identified.
Study Review
The original readmitted patient survey data collection effort was part of regular hospital QA activities, and, as such, did not require review as research involving human subjects. Hospital staff were not required to obtain consent from patients invited to complete the readmitted patient survey. However, the study reported on in this paper aimed to generate and share new knowledge about patients’ discharge and post-discharge experiences which could affect 30-day hospital readmissions. As such, the study was considered research, and a protocol for the analysis of that existing survey dataset was submitted to the Institutional Review Board of the [NAME OF INSTITUTE], which approved it under expedited procedures. A waiver of HIPAA authorization was also granted.
Results
From July to December 2012, hospital staff attempted to invite all identified readmitted patients (n=1061) to complete the survey. There were 587 patients who completed the survey, for an overall response rate of 55.3%. Of the remaining 474 patients who did not complete the survey, 468 (44.1% of 1061) patients were unavailable at the time staff attempted to invite their participation in the survey (e.g. out of room for a medical procedure) and 6 (0.1% of 1061) refused to complete the survey. Therefore, the cooperation rate – the proportion of those invited who completed the survey – was 98.9%.
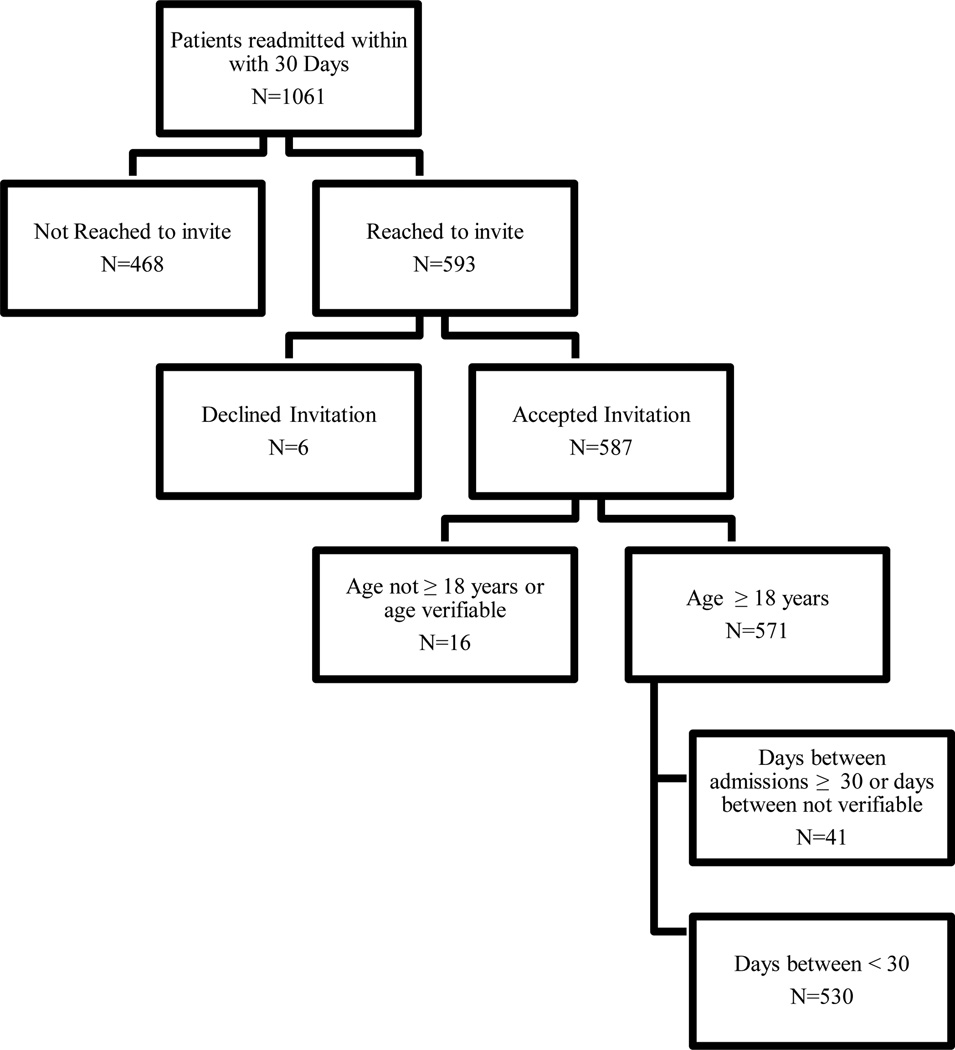
Fifty-seven participants were excluded from the analysis as they did not meet the study eligibility criteria or eligibility could not be determined (e.g., due to missing data). The final study cohort included 530 patients. Figure 1 shows the flow of patients from identification through inclusion in the analysis reported herein.
Figure 1.
Study Participant Selection Flow
Significant differences in demographic characteristics of survey completers and survey non-completers were observed. Completers were significantly younger and of lower SES status. There were no differences observed between the length of stay during their index admission, the number of days between the admissions, or gender (data not shown). Although differences were observed on some characteristics, the survey sample analyzed and reported on herein is considered a convenient one, and the respondents are not representative of all readmitted patients.
Respondents Characteristics
Table 1 provides descriptive information regarding survey respondents. Respondents were on average 52.9±17.0 years of age, with 25.3% of respondents being 65 years or older. Gender and low SES were nearly evenly distributed among respondents (48.5% male, 49.6% low SES).
Table 1.
Readmitted Patient Survey Respondent Characteristics
| Mean | SD | |
| Age, in years | 52.9 | 17.0 |
| Index length of stay, in days | 6.4 | 7.3 |
| Days between index admission and readmission | 12.2 | 8.0 |
| Number | % | |
| Male | 257 | 48.5 |
| 65 years or older | 134 | 25.3 |
| Index admission length of stay > 6.4 days | 173 | 32.6 |
| Low SES | 193 | 36.4 |
| Patient discharged from Index admission to… | ||
| Home without HHS | 341 | 64.3 |
| Home with HHS | 154 | 29.1 |
| Facility | 25 | 4.7 |
| Street / Unknown Place | 10 | 1.9 |
| Patient readmitted from… | ||
| Home | 457 | 86.2 |
| Facility | 36 | 6.8 |
| Street / unknown Place | 23 | 4.3 |
| Clinic | 14 | 2.6 |
Notes:
SES=socio-economic status
SD= Standard Deviation
HHS = Home Health Services
Low SES defined as having Medicaid only, being dually eligible for Medicaid and Medicare, or having no insurance (self-pay)
The average length of stay during the index admission among survey respondents was 6.4 ±7.3 days, with 32.6% of respondents having a long-stay (stay longer than average length of stay of 6.4 days). Nearly all of the responding patients were discharged from their index admission to home, with 64.3% of all discharges being home without home health services and 29.2% of all discharges being home with home health services. Most respondents (86.2%) were also readmitted from home.
Patients’ discharge and post-discharge experiences
Overall, most readmitted patients surveyed reported a relatively positive discharge process, with approximately three-quarters indicating they had agreed on discharge goals (75.7%) and received a readable care plan at discharge (77.7%). Nearly four out of every five responding patients indicated they understood how to care for themselves once discharged, understood how to take prescribed medications, were able to get their prescriptions filled, knew when to contact a health care provider if their condition declined, and had transportation to get to a follow-up doctor’s appointment. Two-thirds of patients reported that they had been able to discuss concerns with their doctor’s office or the hospital. Few (7.7%) reported they had any changes in their prescriptions after the first hospitalization. See Table 2.
The survey database included data extracted from the medical record, which indicated that 38.0% of patients had had a follow up doctor’s appointment scheduled prior to their discharge from the index hospitalization. When directly asked on the survey if they had seen a doctor between the two hospitalizations, nearly one-third (31.1%) reported that they had. Survey data extracted from the medical record also provided the actual date of the follow up doctor appointment for 188 of the 530 responding patients. For those patients with recorded follow-up appointment dates, there was on average 14.5 days between the date of discharge and the follow-up doctor’s appointment date. The average number of days between the discharge from the index admission and the readmission was 12.2 ±7.9 days. The readmission date came before the follow-up doctor’s appointment date in nearly half of the cases (48.4%).
Associations with discharge and post-discharge experiences
A series of bivariate and multivariate logistics regression models were run to explore associations between selected patient (age group, gender, SES) and clinical (length of stay during index admission) characteristics, individual and then as a group, and each of the seven discharge and post-discharge experiences. See Table 3. The bivariate models revealed that three characteristics were associated with only two of the discharge and post-discharge experiences. Males were significantly less likely to understand their self-care compared to females (p=0.04). Both those with low SES compared to those with high SES and elderly patients compared to non-elderly patients were significantly less likely to be able to get their prescriptions filled (p=0.002 and p=0.05, respectively).
Table 3.
Associations between Discharge and Post-Discharge Experience and Select Patient and Clinical Characteristics
| Individual Models | Full Models | Individual Models | Full Models | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | SE | P | OR | SE | P | OR | SE | P | OR | SE | P | ||
| Understood self-care | Was able to discuss concerns with doctors | ||||||||||||
| Low SES | 0.74 | 0.16 | 0.17 | 0.68 | 0.17 | 0.12 | Low SES | 0.83 | 0.16 | 0.32 | 0.78 | 0.16 | 0.24 |
| Male | 0.64 | 0.14 | 0.04 | 0.63 | 0.14 | 0.03 | Male | 0.77 | 0.14 | 0.16 | 0.76 | 0.14 | 0.14 |
| Elder | 1.02 | 0.25 | 0.94 | 0.82 | 0.23 | 0.47 | Elder | 1.00 | 0.21 | 1.00 | 0.87 | 0.20 | 0.56 |
| Long LOS | 1.03 | 0.23 | 0.90 | 1.04 | 0.24 | 0.85 | Long LOS | 1.13 | 0.22 | 0.54 | 1.14 | 0.23 | 0.51 |
| Understood medication requirements | Had transportation | ||||||||||||
| Low SES | 0.76 | 0.17 | 0.20 | 0.67 | 0.17 | 0.10 | Low SES | 0.75 | 0.17 | 0.19 | 0.71 | 0.18 | 0.16 |
| Male | 0.84 | 0.18 | 0.43 | 0.83 | 0.18 | 0.38 | Male | 0.68 | 0.15 | 0.08 | 0.67 | 0.15 | 0.07 |
| Elder | 0.90 | 0.22 | 0.67 | 0.73 | 0.20 | 0.26 | Elder | 1.04 | 0.26 | 0.89 | 0.85 | 0.24 | 0.56 |
| Long LOS | 1.07 | 0.25 | 0.77 | 0.09 | 0.25 | 0.72 | Long LOS | 0.86 | 0.20 | 0.53 | 0.88 | 0.20 | 0.56 |
| Was able to fill prescriptions | Saw doctor between hospitalizations | ||||||||||||
| Low SES | 0.54 | 0.11 | 0.002 | 0.57 | 0.13 | 0.01 | Low SES | 0.97 | 0.19 | 0.87 | 1.09 | 0.24 | 0.68 |
| Male | 0.71 | 0.14 | 0.09 | 0.71 | 0.14 | 0.10 | Male | 0.76 | 0.14 | 0.14 | 0.77 | 0.15 | 0.17 |
| Elder | 1.62 | 0.40 | 0.05 | 1.21 | 0.33 | 0.49 | Elder | 1.36 | 0.29 | 0.15 | 1.38 | 0.32 | 0.16 |
| Long LOS | 0.86 | 0.18 | 0.49 | 0.89 | 0.19 | 0.57 | Long LOS | 1.06 | 0.21 | 0.77 | 1.06 | 0.21 | 0.78 |
| Knew when to contact doctor about condition | Had a change in medications | ||||||||||||
| Low SES | 0.86 | 0.19 | 0.50 | 0.78 | 0.19 | 0.33 | Low SES | 0.80 | 0.28 | 0.52 | 0.89 | 0.34 | 0.77 |
| Male | 0.86 | 0.19 | 0.50 | 0.85 | 0.18 | 0.45 | Male | 0.59 | 0.20 | 0.12 | 0.60 | 0.20 | 0.13 |
| Elder | 0.89 | 0.22 | 0.63 | 0.78 | 0.21 | 0.37 | Elder | 1.41 | 0.50 | 0.33 | 1.28 | 0.50 | 0.52 |
| Long LOS | 0.94 | 0.22 | 0.80 | 0.95 | 0.22 | 0.84 | Long LOS | 0.74 | 0.27 | 0.41 | 0.74 | 0.27 | 0.42 |
Notes: Analysis completed with logistic regression. Individual models assessed association of single characteristics with the outcome. Full models assessed the association of single characteristics with the outcome, after controlling for other variables in the other characteristics in the models. SES=socio-economic status. Low SES status defined as being on Medicaid (with or without Medicaid) or having no insurance. Elder defined as age ≥ 65 years. LOS= Length of stay. Long LOS defined as hospitalizations of 6.4 days or more.
Two of the three characteristics (male and low SES) each remained significant in one multivariate model. Specifically, males remained significantly less likely to not understand their self-care, even after controlling for SES status, age group, and length of stay group (p=0.03). Those with low SES remained significantly less likely to be able to get their prescriptions filled, compared to those with high SES, after control for gender, age group, and length of stay group (p=0.01). After controlling for other characteristics, males were significantly less likely to understand how to care for themselves after discharge and were significantly more likely to be readmitted before their scheduled follow up doctor appointment. Respondents with lower SES status were significantly less likely to report ability to get their prescriptions filled or discuss concerns with their doctor or with the hospital and significantly less likely to have a follow up doctor appointment scheduled before they discharged from the index hospitalization, after controlling for age group, gender and length of stay.
Patients’ perceptions of why they were readmitted
Patients were asked how they thought they became sick enough to be readmitted to the hospital. Ninety-one percent of the survey participants (n=482) responded to this question, providing 617 perceived reasons for their readmission. Those perceived reasons were categorized into 55 groups, indicating the diversity of reasons. The vast majority of the perceived reasons (76.5% of all comments) were reports of symptoms, such as shortness of breath (9.4% of comments), nausea/vomiting (10.5% of comments), and abdominal pain (5.05% of comments). However some patients did report non-symptom related reasons for their readmissions: 1.3% reported they felt they had been discharged too early from their previous hospitalization, 3.2% reported having complications from a previous treatment, and 1.8% reported missing outpatient or home treatment. Just under 2% (n=10) reported non-medical reasons. For example, one patient with colon cancer said he was unable to speak to anyone at the clinic in a timely manner to get questions answered.
Conclusion/Discussion
Most studies on hospital readmissions appearing in the literature relied on medical chart review or analysis of large medical claims datasets, such as the seminal work in this area by Jencks et al that used Medicare claims data (Jencks et al., 2009). Few studies describing patient perceptions of their discharge and post-discharge experience appear in the literature (Kangovi et al., 2012). For example, less than a quarter of the 35 studies included in a systematic review of research identifying patient predictors of acute myocardial infarction relied on patient interviews (along with existing patient data) (Desai, Stauffer, Feringa, & Schreiner, 2009). This study fills this gap by presenting findings of a survey of patients readmitted to a university hospital located in the Southern US.
In general, readmitted patients reported reasonably good post-discharge experiences, as indicated by the high percentage (≥74%) of patients who reported understanding self-care, their medications, when to contact the doctor, being able to get prescriptions filled, and having transportation. More than three-fourths of patients reported that they believed they were prepared for their initial discharge. In a similar survey study of patients readmitted to two large Pennsylvania hospitals, conducted in 2012 by Kangovi et al, responses were also high and similar to these – in that survey, 86.4% of patients reported feeling they were prepared for self-care (Kangovi et al., 2012).
Two possibilities can help explain the high marks on discharge knowledge and experience found among readmitted patients in this study. First, it is possible that these survey responses suffer from courtesy or acquiescence response bias, where surveyed patients gave positive or pleasant responses they thought the surveyors want to hear (Felix, White, McCullough, Morgan, & Stewart, 2004; Hall, 1995). At least theoretically, had these patients (and/or their caregivers) been as prepared at discharge for home care as indicated by the survey responses, they may not have needed to be readmitted. However, this hypothesis could not be tested given the availability of data and the lack of a matched group of patients who were not readmitted within 30 days. Future research to tease this out is warranted.
Second, it is possible that weaknesses in question construction affected the responses of patients. Patients were only given the opportunity to select “yes” or “no” in response to the questions. However, several of the readmitted patient survey questions addressed concepts that go beyond an “all or nothing” response. For example, one question asked patients, “Do you understand what you were supposed to do to care for yourself at home?” Patients may have some, but not comprehensive, knowledge and understanding of self-care; yet the survey allowed them to select only “yes” or “no” in response. The use of a Likert Scale for this question would have allowed patients to indicate the degree of understanding, thus allowing for the identification of patients with some limited knowledge but not lack of complete knowledge (Bethlehem & Biffignandim, 2007; Streiner & Norman, 2008).
Another key finding of this study was low rates of reported post-discharge doctor visits. In other research into hospital readmissions, about half of patients saw their doctor between hospitalizations (Jencks et al., 2009; Kangovi et al., 2012). In the present study, only about one-third (31.3%) of readmitted patients reported seeing doctors between hospitalizations. Theoretically having hospital staff arrange follow-up doctor appointments for patients prior to their discharge may improve this rate. However, as shown in the results, of the 201 patients discharged with a post-hospitalization doctor appointment in hand, only 73 (36.3%) actually showed up for the appointment. Greater attention may need to be given to understanding why patients do not show up for follow up doctor appointments in order to develop strategies to improvement the show up rate.
For 188 of the patients who completed the survey, the actual date of the follow-up appointment was included in the survey data. For these patients, the average number of days from discharge to the actual appointment date was 14.5 days (SD 12.9 days). However, for these same patients, the average number of days between their discharge from the initial hospitalization and their readmission was 12.2 days (SD 7.9 days). In other words, they were readmitted to the hospital before their follow up doctor appointment could have even occurred. This suggests that follow up doctor appointments scheduled even relatively close to discharge (within two weeks of discharge) may be too far out. Discharge staff may want to strive for follow up doctor appointments closer to the date of discharge.
Only two patient characteristics – male gender and lower SES -- were associated with a poorer post-discharge experience. Both males and those with lower SES were significantly less likely to report that they had a follow up doctor appointment scheduled before they discharged from the hospital. If post discharge doctor appointments are important for reducing the odds of readmission, discharge staff may need to specifically target these two patient subgroups for follow up doctor appointment scheduling.
Males were less likely to understand self-care, and those with lower SES were less likely to discuss concerns with their doctor’s office or the hospital. These patients may need to be targeted for increased pre-discharge patient education to improve self-care and self-advocacy. Interestingly, a high percentage of all responses to the open-ended question about what led to the readmission were symptoms (e.g. came back to the hospital because of vomiting, fever or pain). This may indicate that patients understood their condition and warning signs of decline in their condition, and sought treatment. However, the relationship of reported symptoms to actual diagnoses and the relationship of reported symptoms to patient characteristics diagnoses were not tested given the available data.
Finally, patients with lower SES were less likely to be able to get their prescriptions filled after discharge. To help reduce the risk of hospital readmissions, patients with limited resources may need help from hospital discharge staff with getting their prescriptions filled prior to discharge. However, it is possible that in the future limited prescription drug access will be less of an issue as insurance plans in the Health Insurance Marketplace established under the Affordable Care Act are required to include prescription drug coverage.
The study results have several implications for health care delivery and quality improvement practice. However, limitations to these findings must be acknowledged. This study was limited by its reliance on administrative data. The data were collected as part of regular hospital QA activities and not through a controlled study with a rigorous survey research design method or use of a comparison group of patients who were not readmitted. As such, bias may have been introduced through questionnaire design, patient selection, the data collection process, and data entry errors. For example, we recognize that the study may suffer from courtesy bias or acquiescence response bias, which may distort the picture of actual post-discharge experience of patients. In the future, academics and/or hospital administrators conducting such surveys could employ strategies to minimize courtesy bias, such as ensuring a comfortable interview setting, establishing good rapport between the patient and surveyor, and having non-clinical staff administer the survey.
Despite the limitations, this study does expand the hospital readmission literature by providing direct patient responses to questions related to their post-discharge experience rather than additional predictors of 30-day hospital readmission derived for medical claims data. Although patients reported a relatively positive post-discharge experience, results suggest that there is room for improving the discharge and post-discharge process. Of particular note, follow up doctor appointments likely need to be schedule closer to the discharge date to help reduce hospital readmissions (although this suggestion should be tested in an intervention trial). In addition, this study highlights issues around the use of survey research in administrative operations. Survey research methods are complex and involve, at a minimum, sample selection, question/instrument design, standardized data collection processes, and specialized analysis methods (Fowler, 2013). Although many may believe they can administer a survey, poorly designed surveys do occur (Babbie, 1973; Fowler, 2013; Morrel-Samuels, 2002). A number of survey design and data collection issues were identified as the data from the readmitted patient survey were analyzed and reported on herein. Engagement of researchers or consultants with expertise in survey research with routine QA and administrative activities could help address those issues and improve reliability and validity of results.
Acknowledgments
The study was supported by a pilot research award from the UAMS Translational Research Institute (UL1TR000039).
Footnotes
The authors have no conflict of interest in the execution of this study or publication of its results.
Contributor Information
Holly C. Felix, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham Street, Slot 820-12, Little Rock, AR 72205, felixholly@uams.edu / 501-526-6626 / 501-526-6620 fax.
Beverly Seaberg, University Hospital, University of Arkansas for Medical Sciences, 4301 West Markham Street, Slot 572, Little Rock, AR 72205, baseaberg@uams.edu / 501-686-6703.
Zoran Bursac, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham Street, Slot 820, Little Rock, AR 72205, bursaczoran@uams.edu 501-526-6723.
Jeff Thostenson, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham Street, Slot 820, Little Rock, AR 72205, jdthostenson@uams.edu / 501-526-6727.
M. Kathryn Stewart, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 West Markham Street, Slot 820-12, Little Rock, AR 72205, stewartmaryk@uams.edu / 501-526-6625.
References
- Anderson G, Steinberg E. Hospital readmissions in the Medicare population. The New England Journal of Medicine. 1984;311(21):1349–1353. doi: 10.1056/NEJM198411223112105. [DOI] [PubMed] [Google Scholar]
- Babbie E. Survey Research Methods. Belmont, CA: Wadsworth Publishing Company, Inc; 1973. [Google Scholar]
- Bethlehem J, Biffignandim A. Handbook of web surveys. Hoboken, NJ: John Wiley & Sons; 2007. [Google Scholar]
- Bohannon R, Maljanian R. Hospital readmissions of elderly patients hospitalized with pneumonia. Connecticut Medicine. 2003;67(10):599–603. [PubMed] [Google Scholar]
- Boutwell A, Hwu S. Effective interventions to reduce rehospitalizations: A survey of the published evidence. Cambridge, MA: Institute for Healthcare Improvement; 2009. [Google Scholar]
- Carey K, Lin M-Y. Hospital length of stay and readmission: An early investigation. Medical Care Research & Review71. 2014;71(1):99–111. doi: 10.1177/1077558713504998. [DOI] [PubMed] [Google Scholar]
- CMS. Community-Based Care Transition Program. [Retrieved 09/02/2014]; (no date). from http://innovation.cms.gov/initiatives/CCTP/
- Coleman E, Parry C, Chalmers S, Min S. The care transitions intervention: results of a randomized controlled trail. Archives of Internal Medicine. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- Desai M, Stauffer B, Feringa H, Schreiner G. Statistical models and patient predictors of readmission for acute myocardial infarction: A systematic reiew. Circulation: Cardiovascular Quality and Outcomes. 2009;2:500–507. doi: 10.1161/CIRCOUTCOMES.108.832949. [DOI] [PubMed] [Google Scholar]
- Felix H, White M, McCullough H, Morgan J, Stewart M. Issues in assessing satisfaction: Findings of the Arkansas Medicaid Family Planning Demonstration Waiver Evaluation. Journal of Public Health Practice and Management. 2004;10(6):533–538. doi: 10.1097/00124784-200411000-00010. [DOI] [PubMed] [Google Scholar]
- Fowler F. Survey Research Methods. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- Gerhardt G, Yemane A, Hickman P, Oelschlaeger A, Rollins E, Brennan N. Medicare readmissions rates showed meaningful decline in 2012. Medicare & Medicaid Research Review. 2013;3(2):e1–e12. doi: 10.5600/mmrr.003.02.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MF. When methodology compromises anonymity, fear of retaliation can mar hospital survey results. Journal of Health Care Marketing. 1995;15(1):54–61. [PubMed] [Google Scholar]
- Hernandez A, Greiner M, Fonarow G, Hammill B, Heidenreich P, Yancy C, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. Journal of the American Medical Association. 2010;303(17):1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- Jack B, Chetty V, Anthony D, Greenwald J, Burniske G, Johnson A, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Annals of Internal Medicine. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahnigen D, Hannon C, Laxson L, LaForce F. Iatrogenic disease in hospitalized elderly veteran. Journal of the American Geriatrics Society. 1982;60(6):387–390. doi: 10.1111/j.1532-5415.1982.tb02837.x. [DOI] [PubMed] [Google Scholar]
- Jasti H, Mortensen E, Obrosky D, Kapoor W, Fine M. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clinincal Infectious Diseases. 2008;46(4):550–556. doi: 10.1086/526526. [DOI] [PubMed] [Google Scholar]
- Jencks S, Williams M, Coleman E. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kangovi S, Grande D, Meehan P, Mitra N, Shannon R, Long J. Perceptions of readmitted patients on the transition from hospital to home. Journal of Hospital Medicine. 2012;7(9):709–712. doi: 10.1002/jhm.1966. [DOI] [PubMed] [Google Scholar]
- Krumholz H, Chen Y, Wang Y, Vaccarino V, Radford M, Horwitz R. Predictors of readmission among elderly survivors of admission with heart failure. American Heart Journal. 2000;139(1(part 1)):72–77. doi: 10.1016/s0002-8703(00)90311-9. [DOI] [PubMed] [Google Scholar]
- MEDPAC. Report to Congress: Promoting Greater Efficiency in Medicare. Washington, DC: Medicare Payment Advisory Commission; 2007. [Google Scholar]
- Morrel-Samuels P. Getting the truth into workplace surveys. Harvard Business Review. 2002:5–12. [PubMed] [Google Scholar]
- Naylor M, Brooten D, Campbell R, Jacobsen B, Mezey M, Schwartz J. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. Journal of the American Medical Association. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- Rau J. Medicare To Penalize 2,217 Hospitals For Excess Readmissions. 2012 from http://www.kaiserhealthnews.org/stories/2012/august/13/medicare-hospitals-readmissions-penalties.aspx. [Google Scholar]
- Rau J. [Retrieved April 23, 2013];Medicare Revised Readmission Penalties Again. 2013 from http://www.kaiserhealthnews.org/Stories/2013/March/14/revised-readmissions-statistics-hospitals-medicare.aspx. [Google Scholar]
- Robinson S, Howie-Esquivel J, Vlahov D. Readmission risk factors after hospital discharge among the elderly. Population Health Management. 2012;15(6):338–351. doi: 10.1089/pop.2011.0095. [DOI] [PubMed] [Google Scholar]
- Streiner D, Norman G. ealth measurement scales: A practical guide to their development and use. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Wier LM, Barrett M, Steiner C, Jiang J. All-cause readmissions by payer and Age, 2008. Rockville, MD: AHRQ; 2011. [PubMed] [Google Scholar]