SUMMARY
Trans-cutaneous bone conduction (BC) stimulators, when coupled to the HB (BC-HB), are generally used to predict the results that could be achieved after bone conductive implant (BCI) surgery, and their performance is generally considered inferior to that provided by the definitive percutaneous system. The aim of the present study was to compare the performances between BC-HB and BCI of the same typology, when the former's sound processor is fitted in accordance to the individual auditory situation. Twenty-two patients selected for surgical application of a BCI were evaluated and the same audiological protocol was used to select the candidate and assess the final outcome. The BC-HB was properly fitted based on individual hearing loss and personal auditory targets, and tested as primary step of the protocol to obtain the most reliable predictive value. The BAHA Divino and BP100 sound processors were applied in 12 patients with conductive/mixed hearing loss (CMHL) and in 10 subjects with single sided deafness (SSD). Audiometric evaluation included the pure tone average (PTA3) threshold between 250-1000 Hz; the PTA thresholds at 2000 and 4000 Hz; intelligibility scores as percentage of word recognition (WRS) in quiet and in noise; and subjective evaluation of perceived sound quality by a visual analogue scale (VAS). Statistical evaluation with a student's t test was used for assessment of efficacy of BC-HB and BCI compared with the unaided condition. Spearman's Rho coefficient was used to confirm the reliability of the BC-HB simulation test as a predictor of definitive outcome. The results showed that the mean PTA difference between BCI and BC-HB ranged from 2.54 to 8.27 decibels in the CMHL group and from 1.27 to 3.9 decibels in the SSD group. Compared with the BC-HB, BCI showed a better WRS both in CMHL (16% in quiet and 12% in noise) and in SSD (5% in quiet and a 1% in noise) groups. Spearman's Rho coefficient, calculated for PTA, WRS in quiet and in noise and VAS in the two aided conditions, showed a significant correlation between BC-HB and BCI, between PTA and VAS and between WRS in quiet and VAS. It is possible to conclude that the headband test, when the sound processor of the selected bone conductive implant is fitted and personalised for individual hearing loss and auditory targets of the candidate, may provide highly predictive data of the definitive outcome after BCI implant surgery.
KEY WORDS: Bone conductive implant, Headband test, Hearing loss, Pure tone audiometry, Speech audiometry, VAS
RIASSUNTO
Gli stimolatori transcutanei per via ossea, quando accoppiati ad un archetto o headband (HB), vengono utilizzati per predire i risultati che potranno essere ottenuti dopo l'applicazione chirurgica di impianti uditivi a conduzione ossea (BCI). Generalmente, la loro efficacia viene considerata inferiore a quella fornita dal sistema percutaneo definitivo. In questo studio si è voluta comparare l'efficacia del sistema transcutaneo accoppiato all'HB (BC-HB) ed adattato alla situazione audiologica individuale, con i dati post-operatori ottenuti utilizzando lo stesso processore percutaneo. Ventidue pazienti, selezionati per l'applicazione chirurgica di un BCI, sono stati inclusi in questo studio e sono stati sottoposti ad uno stesso protocollo audiologico, sia per la loro candidatura che per la valutazione post-operatoria. Il BC-HB è stato accuratamente adattato all'ipoacusia ed agli obiettivi uditivi propri per ciascun soggetto, per poter acquisire il massimo valore predittivo. Sono stati utilizzati i processori BAHA Divino and BP100 in 12 pazienti con ipoacusia trasmissiva/mista, ed in 10 pazienti con sordità profonda monolaterale (single sided deafness o SSD). La valutazione audiologica ha incluso la soglia audiometrica tonale media tra 250 e 1000 Hz (PTA3); quella a 2000 e 4000 Hz; la percentuale di intelligibilità per le parole (WRS) in quiete e nel rumore; e la valutazione soggettiva di qualità del suono percepito usando la scala analogica visiva (VAS). Il coefficiente Spearman Rho è stato utilizzato per valutare l'attendibilità del BC-HB come indicatore del risultato definitivo. I risultati hanno dimostrato che la differenza media tonale tra sistema percutaneo e simulatore varia dai 2,54 e gli 8,27 decibel nel gruppo con ipoacusia trasmissiva/mista, e dall'1,27 ed i 3,9 decibel nel gruppo SSD. Rispetto al simulatore, con il sistema impiantato si è osservato una migliore WRS: del 16% in quiete e del 12% nel rumore nei soggetti con ipoacusia trasmissiva/mista; e del 5% in quiete e dell'1% nel rumore nel gruppo con SSD. Si è in questo modo evidenziata una significativa correlazione tra i dati del simulatore e quelli dell'impianto percutaneo definitivo, tra il PTA ed il VAS, così come tra il WRS in quiete ed il VAS. Si può quindi concludere che il test con simulatore, quando il processore sonoro utilizzato viene adattato e personalizzato alle necessità uditive di ciascun soggetto, può fornire dati altamente predittivi del risultato definitivo di un BCI.
Introduction
Bone conduction (BC) hearing provides a different pathway for sound transmission and represents an alternative to physiologic airborne conduction 1 2. Although the actual mechanisms that produce the hearing sensation when sound is transmitted through bone have not being fully elucidated, bone conduction hearing devices, such as conventional hearing aids (HA) or bone-conductive implants (BCI), have allowed to overcome some limitations that an air conduction HA carries in relation to, for example, post-operative sequels from middle ear surgery or external ear canal chronic diseases 3 4. In fact, in the last decades, BCI have been successfully applied not only to patients with conductive or mixed hearing loss of different aetiology, but also to those affected by single-sided sensorineural deafness (SSD) by reproducing a contralateral routing of offside signal (CRO S) amplification 5. For nearly three decades, percutaneous BCIs have been adopted worldwide, allowing the osseointegrated device to directly drive bone stimulation to the cochlea, bypassing the damping effect of the skin and subcutaneous tissue. In case of small children, in whom reduced skull thickness is unlikely to retain the implanted screw, the BC sound processor is usually stabilised with a band, called soft-band, that provides transcutaneous stimulation. Likewise, a transcutaneous BC variant, coupled to the HB, is routinely used during the selection process of potential candidates, since it allows not only to perform the audiological evaluation, but also permits patients to familiarise themselves and subjectively perceive its possible benefit.
It is general opinion that the functional outcome of a transcutaneous bone-conductive system is different from what can be achieved by an osseointegrated implant. The variables in play for the reduced performance of the transcutaneous stimulation are position of the bone vibrator, surface contact area, skin thickness and frequency stimulation. In particular, when considering the frequency range of transmission of osteointegrated and transcutaneous BC devices, an overlapping sensitivity has to be expected below 500 Hz since, up to this frequency, the interposed skin produces no attenuation 6. Beyond 500 Hz, contrarily, progressive separation of the percutaneous and transcutaneous BC thresholds occurs, the former being superior by approximately 4 to 7 dB when the speech reception threshold values are considered 6.
The present study was performed to assess the clinical validity of carrying out the preoperative simulation test with HB, when the coupled sound processor has been customised to the patient's hearing loss and auditory targets, as a reliable predictor of the final outcome of BCI.
Materials and methods
Twenty-two adult subjects (10 males, 12 females), implanted at a University Hospital Implanting Center with a single BCI system (BAHA®, Cochlear, Mölnlycke, Sweden) were included in this retrospective study (Table I). Thirteen subjects presented with conductive-mixed hearing loss (CMHL), with mean bone-conduction threshold of 36.5 dB, mean air-conduction threshold of 73.1 dB and mean airbone gap of 36.6 dB; 9 subjects were affected by single sided deafness (SSD), with a contralateral mild, downsloping sensorineural hearing loss presumably caused by aging (Table II). A BP100 sound processor (SP) was used in 10 patients and a Divino SP in the remaining 12.
Table I.
Demographics and clinical characteristics of subjects included in the study. M: male; F: female; COM: chronic otitis media; SSD: single sided deafness.
| Patient | Age | Gender | Aetiology | Type of hearing loss |
|---|---|---|---|---|
| A.M. | 53 | F | Bilateral COM | Mixed bilateral |
| G.B. | 52 | M | Right COM | Mixed right |
| R.B. | 40 | F | Bilateral COM | Mixed bilateral |
| M.C. | 35 | M | Franceschetti S. | Mixed bilateral |
| B.C. | 35 | F | Bilateral COM | Mixed bilateral |
| V.E. | 45 | F | Right COM | Mixed right |
| A.F. | 56 | F | Bilateral COM | Mixed bilateral |
| C.M. | 56 | F | Bilateral COM | Mixed bilateral |
| A.T. | 63 | F | Bilateral COM | Mixed bilateral |
| A.R.2 | 63 | F | Bilateral COM | Mixed bilateral |
| A.R.1 | 51 | M | Goldenhar S. | Mixed bilateral |
| V.S. | 51 | M | Bilateral COM | Mixed bilateral |
| L.T. | 55 | F | Bilateral COM | Mixed bilateral |
| C.T. | 57 | F | Sudden hearing loss | SSD |
| S.A. | 60 | M | Sudden hearing loss | SSD |
| S.A. | 64 | F | Ear surgery | SSD |
| R.F. | 51 | M | Ear surgery | SSD |
| E.M. | 66 | F | Ear surgery | SSD |
| DBL | 57 | M | Ear surgery | SSD |
| D.C. | 74 | F | Sudden hearing loss | SSD |
| G.F. | 67 | M | Ear surgery | SSD |
| O.A. | 60 | F | Sudden hearing loss | SSD |
Table II.
Pre-operative audiometric data of subjects with mixed hearing loss, as bone-conduction and air-conduction threshold levels. PTA: pure tone audiometry.
| Patient | Bone conduction thresholds | Air conduction thresholds | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 250 | 500 | 1000 | 2000 | 4000 | 250 | 500 | 1000 | 2000 | 4000 | |
| A.M. | 5 | 15 | 15 | 50 | 35 | 70 | 60 | 50 | 60 | 55 |
| G.B. | 35 | 50 | 55 | 60 | 60 | 105 | 95 | 85 | 90 | 115 |
| R.B. | 10 | 20 | 35 | 30 | 25 | 55 | 60 | 55 | 65 | 60 |
| M.C. | 5 | 25 | 35 | 45 | 40 | 65 | 60 | 65 | 65 | 75 |
| B.C. | 5 | 15 | 20 | 35 | 30 | 45 | 45 | 50 | 60 | 35 |
| V.E. | 40 | 45 | 45 | 65 | 75 | 105 | 100 | 110 | 105 | 110 |
| A.F. | 5 | 20 | 35 | 45 | 40 | 45 | 55 | 65 | 65 | 80 |
| C.M. | 20 | 35 | 40 | 60 | 70 | 85 | 90 | 70 | 90 | 100 |
| A.T. | 20 | 25 | 20 | 25 | 35 | 65 | 70 | 60 | 50 | 110 |
| A.R.2 | 15 | 35 | 40 | 55 | 45 | 80 | 70 | 75 | 65 | 75 |
| A.R.1 | 10 | 25 | 40 | 55 | 50 | 60 | 85 | 90 | 100 | 100 |
| V.S. | 15 | 40 | 55 | 65 | 75 | 55 | 60 | 80 | 65 | 95 |
| L.T. | 50 | 40 | 35 | 55 | 50 | 50 | 60 | 55 | 70 | 90 |
A preoperative simulation test was performed with an individualised fitting of the two different SPs according to type and degree of hearing loss. In the Divino SP, volume level and gain at the low frequencies were manually changed for CMHL patients while, in the SSD ones, the gain at low frequencies was down-regulated in favour of high frequencies. The microphone was always set in the omnidirectional configuration. The BP100 SP was fully programmed using dedicated preset parameters for CMHL and SSD, optimising the fitting software in each patient. In mixed hearing loss, the wide band dynamic range compression was activated. Automatic noise management, active feedback cancellation, acoustic shock protection and the dynamic output stabiliser were also activated in all patients. Even with this SP, the microphone was set in the omnidirectional configuration.
Audiological assessment included:
Pure tone and speech audiometry, performed inside a soundproof booth with headphones, for choosing the ear (or the first ear) to be implanted;
Sound-field PTA, word recognition score (WRS) in quiet (at 65 dB HL), and WRS in noise (S/N ratio +10 dB) as maximum percentage of intelligibility at the stimulation level of 80 dB, as maximum output of the loudspeaker, for collecting data. For the speech in noise tests, babble noise and speech were delivered through separate channels calibrated independently, with a S/N ratio +10, to the loudspeakers located in the CMHL group at 0° (speech) and 180° (noise), while in the SSD group the multi-talker babble was directed to the better hearing ear, and speech to the poorer one. In the CMHL group, the better ear was always occluded during tests. The speech material consisted in three lists specific to the patients' mother tongue 7.
Single values were recorded for the unaided, BC-HB and post-operative BCI outcomes.
All patients also underwent subjective evaluation of sound quality under the three different situations, using a visual analogue scale (VAS), with scores ranging from 0 to 10.
Mean values obtained in the CMHL and SSD groups with the BC-HB and the BCI compared with the unaided situation were used to assess the gain of the two aided situations compared with the unaided one. For statistical analysis, a non-parametric distribution of data was used. Spearman's Rho correlation coefficient (> 0.80 with p value < 0.05) was used to evaluate the correlation and significance of BC-HB values in predicting BCI performance, in the CMHL and SSD groups separately and together, for the following variables:
the PTA, separately, for low (250-1000 Hz) and high (2000-4000 Hz) frequencies, since at high frequencies different thresholds levels were recorded in the two aided situations 6 13;
the percentage of WRS in quiet;
the maximum WRS in noise;
VAS as sound quality.
Spearman's rho (ρ) coefficient was also used to assess the correlation of the VAS with both the 2-4 kHz PTA and the WRS in quiet, at baseline, BC-HB and BCI conditions.
The study was performed in accordance with the principles of the 1983 Declaration of Helsinki.
Results
Conductive-mixed hearing loss (CMHL) PTA
The mean PTA values in the unaided, BC-HB and BCI conditions are shown in Figure 1. Improvement was found with the BC-HB and the BCI compared with the unaided situation. The mean gain at low-mid frequencies (250- 1000 Hz) was 19.47 dB with the BC-HB and 22.01 dB with the BCI; at high frequencies (2000-4000 Hz) it was 14.42 dB with the BC-HB and 22.07 with the BCI. The BCI gain exceeded that with the BC-HB by 2.54 dB at low frequencies and by 8.27 dB at high frequencies.
Fig. 1.
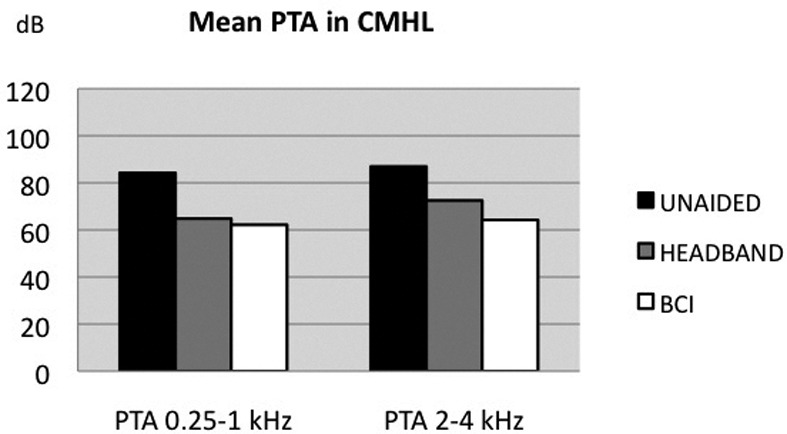
a) Pure tone average (PTA) in conductive-mixed hearing loss (CMHL) subjects in the unaided, headband and bone-conductive implant (BCI) conditions. b) Pure tone average (PTA) in single-sided deafness (SSD) subjects in the unaided, headband and bone-conductive implant (BCI) conditions.
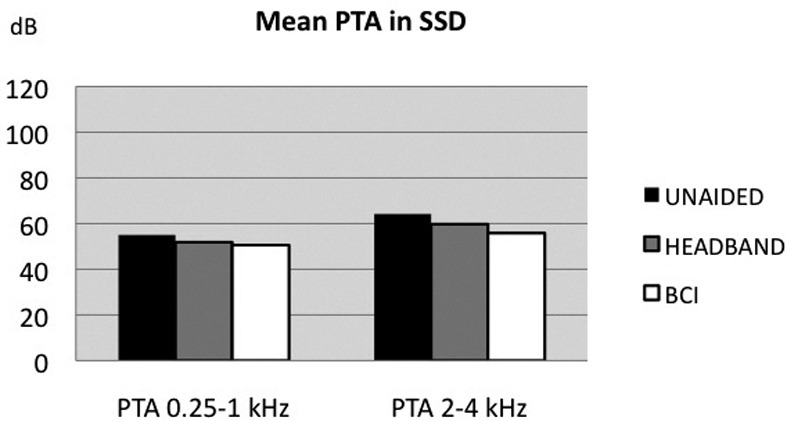
Speech audiometry in quiet – WRS
The mean WRS values at 65 dB in quiet are shown in Figure 2. The WRS values improved with both the BCHB and BCI. When considering the BC-HB and the BCI compared with the unaided condition, the mean WRS gain was 21% with the BC-HB, and 37% with the BCI, with a 16% difference (Fig. 2).
Fig. 2.
a) Percentage of word recognition score (WRS) at 65 dB HL in quiet, in conductive-mixed hearing loss (CMHL) subjects, in the unaided, headband and bone-conductive implant (BCI) conditions. b) Percentage of WRS at 65 dB HL in quiet, in single- sided deafness (SSD) subjects, in the unaided, headband and BCI conditions.
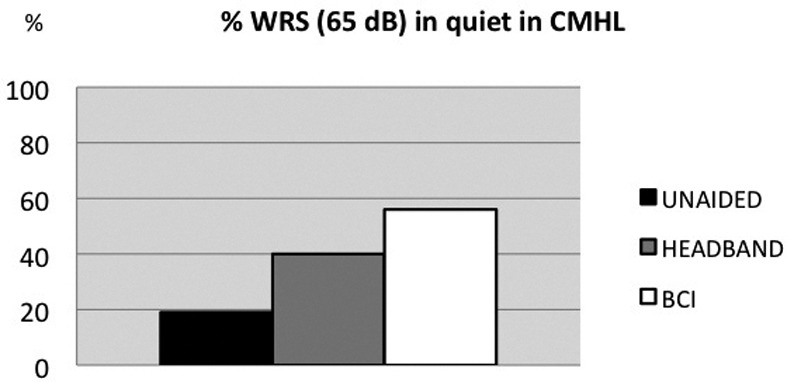
Speech audiometry in noise (S/R + 10) – Maximum WRS
The mean maximum percentage of word recognition in noise in the three different conditions is shown in Figure 3. The percentage of intelligibility improved with both the BC-HB and BCI. The mean gain compared with the unaided condition was 12.3% with the BC-HB and 24.5% with BCI, with a difference of 12.2% between the two aided conditions (Fig. 3).
Fig. 3.
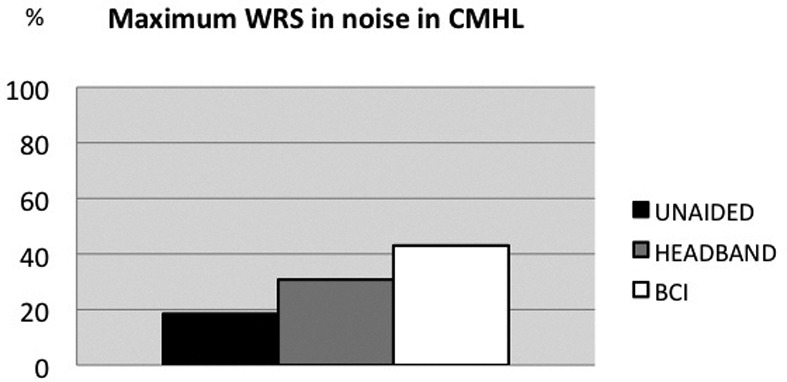
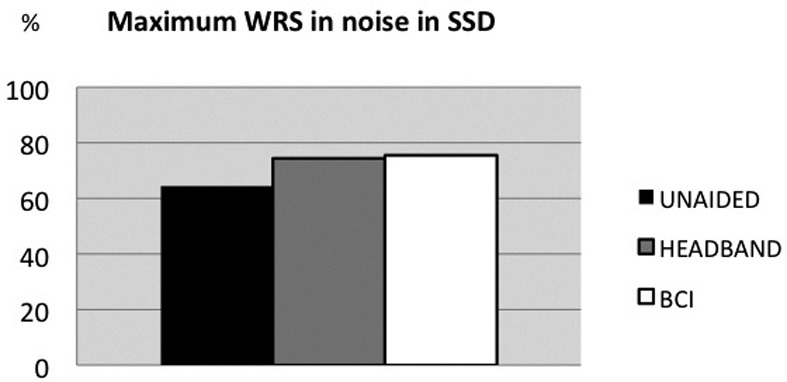
a) Maximum percentage of word recognition score (WRS) in noise, at stimulation level of maximum WRS in quiet, in conductive-mixed hearing loss (CMHL) subjects, in the unaided, headband and bone-conductive implant (BCI) conditions. b) Maximum percentage of WRS in noise, at stimulation level of maximum WRS in quiet, in single-sided deafness (SSD) subjects, in the unaided, headband and BCI conditions.
Single sided deafness PTA
The PTA results in all three situations are shown in Figure 1. PTA improvement was found with both the BC-HB and BCI at low and high frequencies. The mean gain at low frequencies was 3.17 dB with the BC-HB and 4.44 dB with the BCI; at high frequencies, the gain was 4.44 dB with the BC-HB and 8.33 dB with the BCI. The gain difference between the two aided modalities was 1.27 dB at low frequencies and 3.9 dB at high frequencies.
Speech audiometry in quiet – WRS
The mean WRS results in all three conditions are shown in Figure 2. The percentage of word recognition at 65 dB improved with both the BC-HB and BCI. The WRS gain was 9% with the BC-HB and 14% with the BCI; the difference between the two aided modalities was 5%.
Speech audiometry in noise (S/N + 10)
The mean maximum percentage of word recognition in noise in the three different conditions is shown in Figure 3. The mean gain was 1.11% with the BC-HB and 11.11% with the BCI compared with the unaided condition. A 10% percentage difference between the two aided modalities was found. The mean gain was 2 dB with the BC-HB and 5.5 dB with BCI.
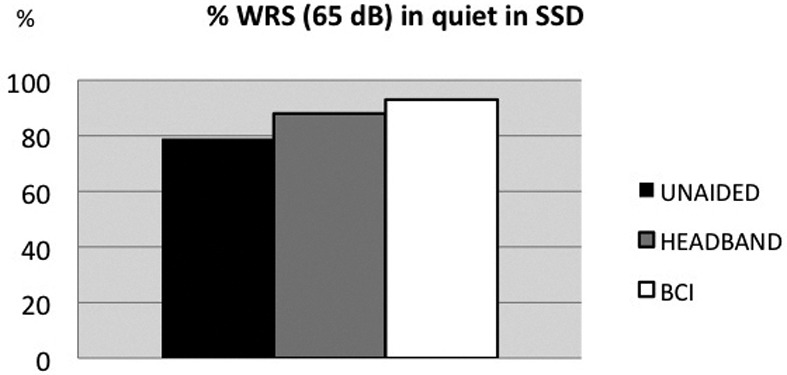
VAS of sound quality
The mean VAS values obtained under the unaided, BCHB and BCI conditions, in the CMHL and SSD groups, are shown in Figure 4.
Fig. 4.
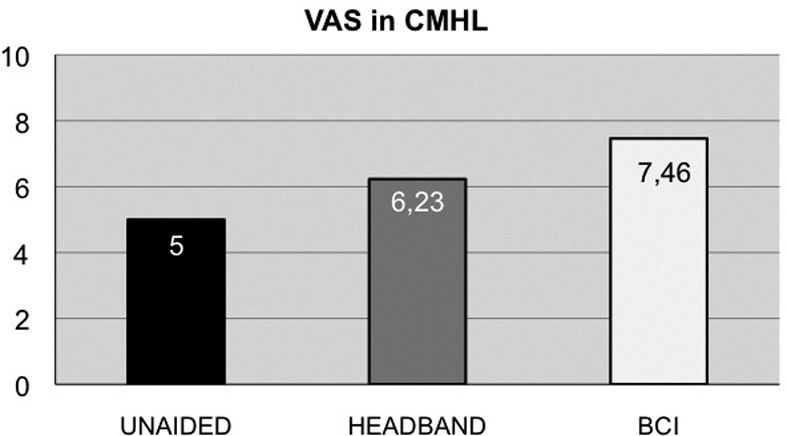
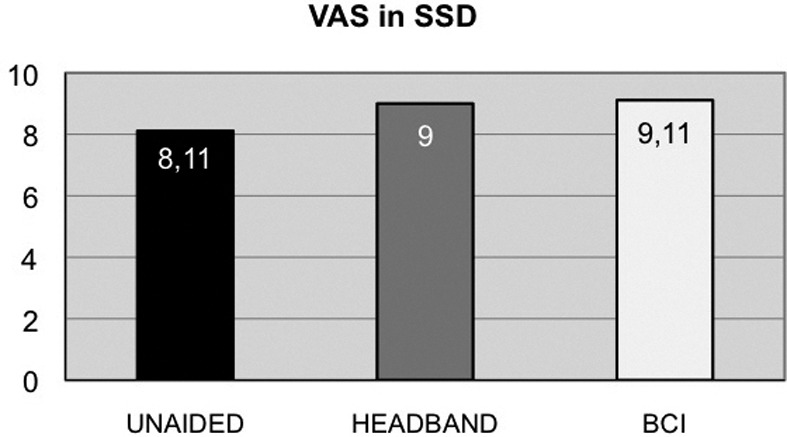
a) Mean visual analogue scale (VAS) score for conductive- mixed hearing loss (CMHL) subjects in the unaided, headband and bone-conductive implant (BCI) conditions. b) Mean VAS score for single-sided deafness (SSD) subjects in the unaided, headband and BCI conditions.
In the CMHL group, a strict correlation (ρ =0.85, p < 0.001) between the PTA thresholds at 250-1000 Hz of the BC-HB and BCI was found, which was also significant for all other parameters (Table III). In the SSD group, the correlation between BC-HB and BCI was also very close and significant for all parameters, except for PTA values at 250-1000 Hz. When considering the patients together, strong correlation was found for the entire PTA range, which was significant for all parameters considered (Table IV).
Table III.
Correlation level (Spearman's rho) and significance (p) of the intra-individual changes in variables between the BC-HB and the BCI, for conductive-mixed hearing loss (CMHL, n = 13) and single-sided deafness (SSD, n = 9) subjects. PTA: Pure tone average; WRS: word recognition score.
| Predictive Index of pre-operative BC-HB for the BCI outcome | ||
|---|---|---|
| Variable | Spearman's Rho | p value |
| CMHL (n = 13) | ||
| Sound quality (VAS) | 0.68 | 0.011 |
| PTA 250-500-1000 Hertz (dB) | 0.85 | < 0.001 |
| PTA 2-4 KHz (dB) | 0.68 | 0.011 |
| WRS in quiet | 0.69 | 0.010 |
| WRS in noise (%) | 0.73 | 0.005 |
| SSD (n = 9) | ||
| Sound quality (VAS) | 0.90 | 0.001 |
| PTA 250-500-1000 Hertz (dB) | 0.56 | 0.119 |
| PTA 2-4 KHz (dB) | 0.88 | 0.002 |
| WRS in quiet | 0.92 | 0.001 |
| WRS in noise (%) | 0.87 | 0.002 |
Table IV.
Correlation level (Spearman's rho) and significance (p) of the intra-individual changes in variables between the BC-HB and the BCI, in the entire study group. PTA: pure tone average; WRS: word recognition score.
| Correlation between the intra-individual changes after the BC-HB and the BCI in all subjects | ||
|---|---|---|
| Variable | Spearman's Rho | p value |
| PTA 250-500-1000 hertz (dB) | 0.85 | < 0.001 |
| PTA 2000-4000 hertz (dB) | 0.83 | > 0.001 |
| WRS in quiet (%) | 0.61 | 0.003 |
| WRS in noise (%) | 0.76 | < 0.001 |
In the CMHL, a high and significant correlation was found between the WRS in quiet and VAS in the unaided (ρ = 1.00; p < 0.001), BC-HB (ρ =0.99; p < 0.001) and BCI (ρ = 0.99; p < 0.001) conditions. A significant correlation was also found between PTA 2-4 kHz and the VAS in the unaided (p= 0.010), BC-HB (p= 0.004) and BCI (p < 0.001) conditions.
In SSD, a high and significant correlation was found between the WRS in quiet and the VAS in the unaided (ρ = 1,00; p < 0.001), BC-HB (ρ =1.00; p < 0.001) and BCI (ρ = 0.87; p < 0.003) conditions. No correlation was found between the VAS and PTA 2-4 kHz in the unaided (p > 0.05), BC-HB (p = 0.05) or BCI (p > 0.05) conditions.
Discussion
The differences between the transcutaneous and percutaneous modality of sound conduction of bone generally influence the mean auditory gain, even when a single frequency range is taken into consideration. At high frequencies, for instance, percutaneous BCI usually provides better gain than a transcutaneous system 8. In clinical practice, a preoperative trial period and audiometric tests carried out with the transcutaneous simulation system, such as the headband (HB), allow the patient to get acquainted with the sound delivered by the device, and also help the audiologist and surgeon to select the right candidate and anticipate the definitive post-operative result. Pre-operative HB tests enable recording data with a transcutaneous mode of stimulation, and to compare them at a later stage with those obtained via the definitive BCI. Similarly to all HA-related tests, even in this situation audiometric tests are performed in sound fields with variables related to intrinsic (type and severity of hearing loss, uni- or bilateral hearing loss) and extrinsic factors (type and level of stimulation, loudspeaker position in the azimuth). Generally, in spite of striking methodological differences, few information is usually available in the literature that describes the specific setting of the simulation device, which is instead analysed with fixed stimulation parameters, such as delivering the maximum volume without balancing the frequency gain in relation to the patients' hearing loss and listening need. One may assume that this latter adjustment is meant to compensate for the inferior efficacy of the transcutaneous bone stimulator compared with the percutaneous one. Furthermore, the information collected by simulation tests should be different in individuals affected by CMHL from those with SSD due to the different problems associated with the two hearing conditions, such as for instance loss of binaural hearing that is usually targeted only in SSD. The literature in this regard has mainly focused on CMHL, because after more than 30 years of application of a BCI in this form of hearing impairment, the major target has uniquely been PTA gain 9-11. A recent study compared the pre-operative transcutaneous and postoperative percutaneous conditions, reporting differences in the hearing threshold (5-20 dB for the range 1-4 kHz and 6 dB for that 0.5-1 kHz) as well as in speech recognition thresholds (SRT improvement of 4-7 dB) 12. Other investigators have found that the predictive value at low-frequency was more reliable than at high frequencies, with a hearing gain ranging from 1 to 18 dB 13. Snapp et al. 14 commented on the low sensitivity of common audiological tests for predicting and monitoring BCI outcomes in SSD patients, stressing that the tests with speech recognition in noise should play a major role for appropriate assessment.
At our department, all patients candidate for a BCI, being affected by either conductive, mixed or profound unilateral sensorineural hearing loss (SSD), routinely undergo a preoperative trial wearing a HB coupled to the same sound processor that has been chosen to be coupled to the implanted fixture. The specific sound processor is individually fitted, selecting the parameters that would mostly be beneficial for the individual patient. In the present study, two types of sound processors of the same manufacturer were used: the BP100 and the Divino. For the BP100 SP, the fitting parameters set by default for conductive-mixed hearing loss and SSD were modified on the basis of the patient's listening characteristics; for the Divino SP, the volume at the low frequencies was manually regulated depending on the type of hearing loss: in SSD, the gain at low frequencies was decreased to allow better speech perception, especially in noisy environments, while in CMHL, low frequency amplification was only finalised to improve the signal to noise ratio. Due to the limitation of the available devices, which do not allow a home-trial period, the potential candidate was left with the BC-HB for a few hours in different listening environments, before performing a series of audiological tests that have always included the measurement of verbal perception, in quiet and noise, as well as a questionnaire on the quality of the perceived sound in the different listening situations.
The present study has taken into consideration hearing function assessed both with the BC-HB and with the activated BCI, in terms of:
hearing threshold as PTA (250-4000 Hertz);
percentage of WRS at 65 dB in quiet;
maximum percentage of WRS in noise (S/N +10, fixing the stimulation loudness at 80 dB, corresponding to the maximum output of the loudspeaker in sound-field);
quality of perceived sound with VAS compared with the unaided condition, and the statistical difference of the same parameters between the simulation pre-operative effects and definitive post-operative outcome.
The effect of the BCI, in the simulation and definitive configurations, was significantly better than in the unaided condition for all the qualitative and quantitative parameters. Apart from this easily predictable result, the major target of this study was to assess how close the two aided conditions would perform, so as to highlight the predictive role of the BC-HB.
In conductive and mixed hearing loss, a mean intra-individual improvement after BCI was found for the PTA between 250 and 4000 Hz, for word discrimination in quiet and noise, and for the quality of sound. The PTA differences between the BCI and the BC-HB were minimal (around 2.5 dB for low frequencies and 8 dB for high frequencies), while the speech performance with the BCI was better than with the BC-HB (16% in quiet and 12% in noise).
In the SSD group, the performance of the BCI was superior to that of the BC-HB in all parameters considered. The mean PTA gain with the BCI, compared with the BC-HB condition, was minimal (around 1 dB) for low frequencies and up to only 4 dB for high frequencies. When testing speech discrimination, a better percentage of intelligibility was found with the BCI than with the BC-HB, of about 5% in quiet and 10% in noise. The mean VAS values in the CMHL and SSD groups, taken together, showed that the definitive BCI provided a clearer and better sound than both the unaided and the BC-HB condition.
The prediction of the BCI effect derived from the correlation between the intra-individual changes of the variables in the two aided situations was extremely significant in the CMHL group for low-middle frequencies, and to a lesser degree, but still significant, for the other parameters; in the SSD group, however, the correlation for low frequencies was poor. This latter finding is related to the fitting characteristics for the SSD situation and to the minimal gain deliberately received at low frequencies to privilege high frequency gain, while trying to optimise some of the binaural function features. Considering the patients together (CMHL + SSD), close correlation was found for the entire PTA range, which was significant for all parameters.
The correlation between VAS and the other variables revealed differences between the CMHL and SSD groups in the three different situations. In CMHL, in all situations, a close and significant correlation was found between the good perceived quality of sound in terms of clearness and openness and speech perception in quiet. When considering the correlation between VAS and 2000-4000 Hz PTA, it was shown to be significant in all auditory situations, but correlated highly only with the BCI. The correlation between sound quality, sound-field speech perception and high-frequency gain with a BCI has already been recently shown 13. In the SSD group, in contrast, a high and significant correlation of VAS was shown only with the WRS percentage in quiet, in all three situations. This finding means that in the SSD, verbal and speech perception are related with directional hearing and follow two separate analytic processing cues, the first simply auditory and the second linked to multi-sensorial inputs.
Apart from the efficacy of the BCI compared to the unaided situation in the CMHL and SSD groups, the present study showed that the use of a personalised, well-fitted SP coupled to a HB in pre-operative simulation tests is reliable in predicting the final BCI advantages not only for hearing improvement, but also for speech perception in noise and quality of listening. The accuracy of the outcome prediction is motivated by the fact that, contrary to previous reports, the differences between PTA and WRS in the two aided conditions were minimal 14. This assumption is also confirmed by the strong and significant correlation with all variables taken into consideration, as well as in the VAS when comparing hearing function with the BC-HB with that of the definitive implant.
It is possible to comment that the main reason for preoperatively assessing a BCI candidate with a transcutaneous HB-coupled processor is to allow the subject to experience the actual advantages of bone conduction stimulation carried out using a modality that is mostly reproduced by the definitive BCI. In our opinion, these simulation tests can be reliable only if the drawback of the skin attenuation related to the transcutaneous condition is partially compensated by fitting the SP simulator on the basis of individual hearing loss, as well as the needs and individual targets of each candidate, rather than using a preset configuration.
Conclusions
The present study shows that when using pre-operative audiological assessment with a BC-HB simulator as a predictor of a BCI outcome, the simulation device should be fitted with the same modality used for the definitive BCI, while assessing audiological performances not only as PTA auditory gain, but mostly as speech perception in noise and improvement of the quality of perceived sound.
The outcome of such an evaluation may allow patients, audiologists and surgeons to obtain an accurate estimate of the final outcome after BCI application.
References
- 1.Tonndorf J. Bone conduction. Studies in experimental animals. Acta Otolaryngol. 1966;(Suppl 213):1–1. [PubMed] [Google Scholar]
- 2.Stenfelt S, Goode RL. Bone conducted sound: Physiological and clinical aspects. Otol Neurotol. 2005;26:1245–1261. doi: 10.1097/01.mao.0000187236.10842.d5. [DOI] [PubMed] [Google Scholar]
- 3.Håkansson B, Tjellström A, Rosenhall U, et al. The boneanchored hearing aid. Acta Otolaryngo. 1985;100:229–239. doi: 10.3109/00016488509104785. [DOI] [PubMed] [Google Scholar]
- 4.Albrektsson T, Brånemark PI, Jacobsson M, et al. Present clinical applications of osteointegrated percutaneus implants. Plast Riconstr Surg. 1987;79:721–731. doi: 10.1097/00006534-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Vanecloo FM, Ruzza I, Hanson JN, et al. The monoaural psuedo-stereophonic hearing aid (BAHA) in unilateral total deafness: a study of 29 patients. Rev Laryngol Otol Rhinol (Bord) 2001;122:343–350. [PubMed] [Google Scholar]
- 6.Håkansson B, Tjellström A, Carlsson P. Percutaneous vs. transcutaneous transducers for hearing by direct bone conduction. Otolaryngol Head Neck Surg. 1990;102:339–344. doi: 10.1177/019459989010200407. [DOI] [PubMed] [Google Scholar]
- 7.Turrini M, Cutugno F, Maturi P, et al. Nuove parole bisillabiche per audiometria vocale in lingua italiana. Acta Otorhinolaryngol Ital. 1993;13:63–77. [PubMed] [Google Scholar]
- 8.Stenfelt S, Håkansson B, Tjellström A. Vibration characteristics of bone conduction sound in vitro. J Acoustic Soc Am. 2000;107:422–431. doi: 10.1121/1.428314. [DOI] [PubMed] [Google Scholar]
- 9.Mylanus EA, Snik AF, Cremers CW. Influence of the thickness of the skin and subcutaneous tissue covering the mastoid on bone-conduction thresholds obtained transcutaneously vs. percutaneously. Scand Audiol. 1994;23:201–203. doi: 10.3109/01050399409047509. [DOI] [PubMed] [Google Scholar]
- 10.Håkansson B, Tjellström A, Rosenhall U. Hearing thresholds with direct bone conduction vs. conventional bone conduction. Scand Audiol. 1984;13:3–13. doi: 10.3109/01050398409076252. [DOI] [PubMed] [Google Scholar]
- 11.Hodgetts WE, Scollie SD, Swain R. Effects of applied contact force and volume control setting on output force levels of the Baha softband. Int J Audiol. 2006;45:301–308. doi: 10.1080/14992020600582133. [DOI] [PubMed] [Google Scholar]
- 12.Verstraeten N, Zarowski AJ, Somers T, et al. Comparison of the audiologic results obtained with the bone-anchored hearing aid attached to the headband, the testband, and to the "snap" abutment. Otol Neurotol. 2008;30:70–75. doi: 10.1097/MAO.0b013e31818be97a. [DOI] [PubMed] [Google Scholar]
- 13.Heywood RL, Patel PM, Jonathan DA. Comparison of hearing thresholds obtained with BAHA preoperative assessment tools and those obtained with the osseointegrated implant. Ear Nose Throat J. 2011;90:21–27. doi: 10.1177/014556131109000514. [DOI] [PubMed] [Google Scholar]
- 14.McNeil ML, Gulliver M, Morris DP, et al. Can audiometric results predict qualitative hearing improvements in bone-anchored hearing aid recipients? J Laryngol Otol. 2014;128:35–42. doi: 10.1017/S0022215113003150. [DOI] [PubMed] [Google Scholar]


