Abstract
Discectomy for lumbar disc provides faster relief in acute attack than does conservative management. Long-term results of open, microscopy-, and endoscopy-assisted discectomy are same. Early results of endoscopy-assisted surgery are better as compared to that of open surgery in terms of better visualization, smaller incision, reduced hospital stay, better education, lower cost, less pain, early return to work, and rehabilitation. Although microscopic discectomy also has comparable advantages, endoscopic-assisted technique better addresses opposite side pathology. Inter laminar technique (ILT) and trans foraminal technique (TFT) are two main endoscopic approaches for lumbar pathologies. Endoscopy-assisted ILT can be performed in recurrent, migrated, and calcified discs. All lumbar levels including L5-S1 level, intracanalicular, foraminal disc, lumbar canal and lateral recess stenosis, multiple levels, and bilateral lesions can be managed by ILT. Migrated, calcified discs, L5-S1 pathology, lumbar canal, and lateral recess stenosis can be better approached by ILT than by TFT. Most spinal surgeons are familiar with anatomy of ILT. It can be safely performed in foramen stenosis and in uncooperative and anxious patients. There is less risk of exiting nerve root damage, especially in short pedicles and in presence of facet osteophytes as compared to TFT. On the other hand, ILT is more invasive than TFT with more chances of perforations of the dura matter, pseudomeningocele formation, and cerebrospinal fluid fistula in early learning curve. Obtaining microsurgical experience, attending workshops, and suitable patient selection can help shorten the learning curve. Once adequate skill is acquired, this procedure is safe and effective. The surgeon must be prepared to convert to an open procedure, especially in early learning curve. Spinal endoscopy is likely to achieve more roles in future. Endoscopy-assisted ILT is a safer alternative to the microscopic technique.
Keywords: Endoscopic lumbar discectomy, lumbar disc herniation, percutaneous lumbar disc decompression, spinal endoscopy
Introduction
Lumbar disc disease is quite common. Surgical discectomy for carefully selected patients with sciatica due to lumbar disc prolapse provides faster relief from an acute attack than does conservative management.[1] Removal of a herniated disc using an operative microscope was first performed by Yasargil in 1977. It was, and remains, the “gold standard” for surgical treatment of lumbar disc herniation and the method used by the vast majority of spinal surgeons.[2]
Role of surgery by minimally invasive techniques for lumbar disc remains unclear in the Cochrane review.[1] Neuroendoscopy has grown rapidly in recent times as a therapeutic modality for treating a variety of brain and spinal disorders.[3,4,5,6,7] Endoscopy has some significant advantages over open surgery, such as better visualization of the lesion, smaller incision size with reduced morbidity, reduced hospital stay, and, ultimately, lower cost. In addition, spinal endoscopy allows observers and operating room staff to be more involved and is therefore better for education. Although microscopic discectomy also has comparable advantages, endoscopy-assisted technique can better address opposite side pathology. On the other hand, spinal endoscopy carries additional risks and the surgeon must always be prepared to convert it to an open procedure. The learning curve for spinal endoscopy is steep. Nevertheless, with training and experience, spine surgeon can achieve better outcomes, reduced morbidity, and better cosmetic results. As technology evolves and more experience is obtained, neuroendoscopy is likely to achieve further roles in spine surgery.[4] This review includes all articles published in PubMed and Google in the last 20 years. It is based on thorough search on topics published until October 2012 and personal experience of more than 500 endoscopy-assisted lumbar surgeries performed by the senior author. The present article is aimed to review the indications and results of endoscopy-assisted inter laminar technique (ILT) for lumbar diseases.
Preoperative assessment and investigations
Detailed history and thorough physical examination should be done in all cases to find out the exact level of pathology responsible for symptoms of the patients. Magnetic resonance imaging (MRI) is the investigation of choice in most cases. Although MRI is good for the evaluation of sequestered lumbar disc herniation, it has its limitations, especially in the detection of fragment lying dorsal to thecal sac or the root.[8] Computed tomography (CT) scan and myelography CT can provide useful information in some cases. Myelography CT and discography CT can help in accurate orientation of the diseased disc and nerve root before ILT procedure, thereby decreasing the possibility of nerve damage.[9]
Endoscopy-assisted ILT
Surgery is performed in prone position on a radiolucent table, usually under general anesthesia, although it can be done under local anesthesia as well. The choice of anesthesia depends on the preference of the surgeon and anesthesiologist performing the operation. The skin incision is made after confirming level under image guidance. Incision is made at about 1-1.5 cm away from the midline. Although various techniques are known, but most endoscopic spine surgeries utilize dilatation technology to create surgical access through soft tissue (skin, subcutaneous fat, fascia, and muscle) instead of cutting in order to minimize tissue trauma. The operative sheath is directed toward the ligamentum flavum and lamina. Soft tissues on the lamina, facet joint, and ligamentum flavum are removed. Burrs, trephines, and rongeurs can be used to allow resection of bone in order to expand the operative field. Part of superior and inferior lamina, along with the medial facet, is removed [Figure 1]. Ligamentum flavum can be removed or preserved; depending on the pathology and surgeons’ experience,[10,11] a part of the offending disc is removed.
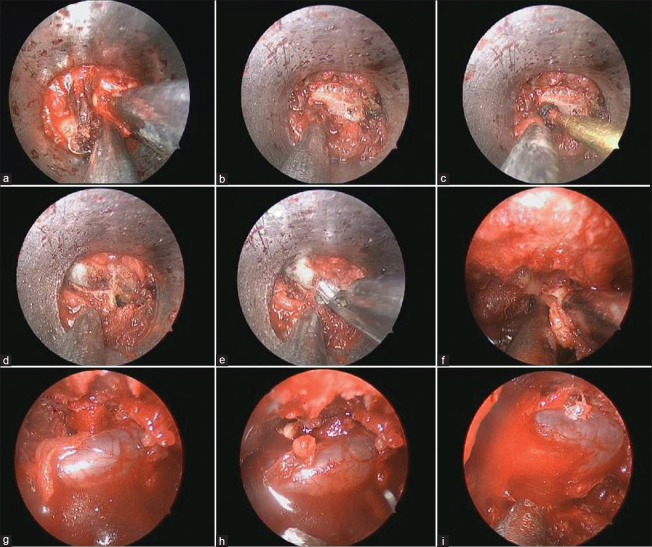
Figure 1.
(a) Steps of endoscopic interlaminar technique showing soft tissue lying on the lamina; (b) lamina free from overlying soft tissue; (c) part of lamina being removed by high-speed drill; (d) thin part of the inner cortex of the lamina left behind to protect underlying soft tissue; (e) thinned out lamina being removed using Kerrison punch; (f) ligamentum flavum being removed; (g, h) opposite side thecal sac and nerve root being decompressed; and (i) thecal sac after bilateral decompression
Two level pathologies can be addressed by moving and with angulations of the sheath using the same incision. Removal of opposite side ligamentum flavum, osteophytes of the opposite facet, and under cutting of opposite side lamina can be done using same incision [Figure 2]. Endoscopy-assisted technique can better address opposite side pathologies than the microscopic procedures. There is increased risk of dural tear when dealing with opposite side pathology, canal stenosis, central disc, and multiple levels. Such procedures should be done after achieving sufficient experience.[12,13] Another limitation of endoscopy-assisted techniques is two-dimensional visualizations as against three-dimensional visualizations in microscopic technique.
Figure 2.
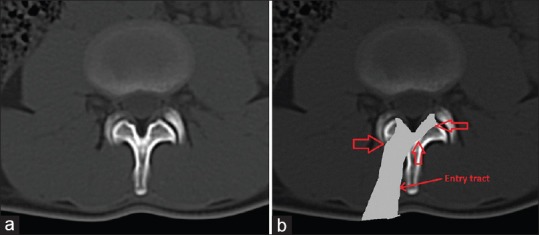
(a) Normal axial CT scan image at lumbar disc level; (b) Diagrammatic representation of bilateral decompression using ipsilateral approach, showing removal of ipsilateral medial facet and lamina (arrow head to right), base of the spine (arrow head up), and undersurface of opposite side lamina and medial part of opposite side facet joint (arrow head to left)
Various systems like Destandau (Karl Storz GmbH and Co KG Tuttlingen Germany), EasyGO (Karl Storz GmbH and Co KG Tuttlingen Germany), SMART (Karl Storz GmbH and Co KG Tuttlingen Germany), and Dr. Husain System (AVM healthcare products Pvt. Ltd. New Delhi India) are available commercially.[14,15,16,17] All these systems are effective and safe. This technique can be combined with trans foraminal technique (TFT) and lumbar interbody fusion in selected patients with instability of lesser than grade II listhesis.[18]
Advantages of Endoscopy-assisted Approaches Over Microsurgery or Open Techniques
Endoscopic procedures are increasingly used for the management of lumbar disease in recent times.[19,20] Although the systematic review using the Cochrane Collaboration guidelines, including all randomized or “quasi-randomized” clinical trials, observed similar long-term outcome, results in terms of blood loss, systemic repercussions, and duration of hospital stay was superior in microsurgical and endoscopic techniques as compared to the conventional open technique for the treatment of single-level lumbar disc herniations.[19] Although endoscopic technique offers similar short-term clinical outcome as compared to open discectomy, it can be achieved with smaller incision, less tissue trauma, and quicker recovery.[20,21,22,23] The clinical results of the endoscopic technique are equal to those of the microsurgical technique.[24] The results of microscopic discectomy using tubular retractor are equally good and safe.[25] This technique is also equally comparable to endoscopic technique in terms of minimal invasiveness. The operative time is short and the blood loss is minimal in microscopic technique using tubular retractor.[25] Endoscopic trans laminar technique has been found to be safe and effective for the treatment of lumbar disc herniation in the hidden zone.[26]
Endoscopy-assisted ILT is a less traumatic procedure as compared to open surgery, and it gives comparable visualization of the nerve structures as compared to open surgery; this has been observed in electromyography (EMG) activity.[27] The minimally invasive nature of endoscopic ILT is further supported by the less systemic cytokine responses in this technique as compared to open procedure. Systemic cytokine are markers of operative tissue trauma after surgery.[28] The mean creatine phosphokinase levels, as a measure of muscle damage, were lower for the endoscopic group than for the microscopic group at days 3 and 5.[29] On the other hand, the postoperative MRI changes on the nerve roots, cauda equine, and entry tract were similar in endoscopic procedure and open surgery.[30]
Indications of ILT
Contained and migrated disc
High-canal compromise and migrated disc patients can be effectively addressed by ILT. The decompression results of ILT are equivalent to those of conventional procedures.[31,32] Endoscopy-assisted ILT is effective and safe in achieving good decompression of canal in high-grade, down-migrated disc herniation.[33]
Lumbar disc herniations at all level including L5-S1
Endoscopy-assisted ILT is a safe, effective, and minimally invasive procedure for the treatment of intracanalicular disc herniations at all lumbar levels including L5-S1. TFT is difficult at L5-S1 site because of anatomic constraints.[34]
Recurrent disc
Results of ILT are either equivalent or superior to conventional surgery for recurrent disc.[35,36,37,38,39,40,41] Dissection of scar tissue should be done from the medial facet joint rather than from separation of scar from the neural tissue.[40]
Foraminal and extra foraminal lumbar disc herniations and foraminal stenosis
Although foraminal and extra foraminal disc excision is difficult without removal of facet joint by interlaminar technique; such discectomy can be done by exposing area lateral to facet joint in between two transverse processes.[42] Far lateral migrated disc at L5-S1 can be removed without facet removal by ILT.[43] Endoscopy-assisted techniques are also useful for the treatment of lumbar foraminal stenosis.[44]
Lumbar canal and lateral recess stenosis
Extensive decompression with laminectomy is often described as the method of choice in surgery for lumbar canal and lateral recess stenosis. Nonetheless, tissue-sparing endoscopic techniques have become the standard in many areas because of the advantages they offer in surgical technique and in rehabilitation. Although endoscopic decompression for lumbar canal stenosis is difficult in the initial learning curve, endoscopic ILT can be used effectively in lumbar canal stenosis (LCS) and lateral recess stenosis after gaining sufficient experience in endoscopic surgeries.[12,13,45,46] The area of the dural tube can be increased to an average of 408.0% after surgery (range: 211-774%). Bilateral decompression with unilateral approach can be achieved safely and effectively by endoscopy-assisted ILT.[47,48] Although the clinical results were equal after endoscopic ILT in lumbar lateral stenosis as compared to microsurgical technique in Ruetten et al., series, complications and revisions was significantly reduced in the endoscopic group.[49] The results of endoscopic surgery in lumbar stenosis were comparable to that of open surgery with less trauma and early rehabilitation.[50]
Calcified disc
Endoscopy assisted ILT is safe and effective for the treatment of calcified herniated disc.[51,52]
Multiple level discs
Endoscopy-assisted ILT can also be used in multiple level disc disease.[53]
Results of the Endoscopy-assisted ILT
Early outcome, in terms of less pain, minimal trauma, and early rehabilitation, is better after the endoscopy surgery as compared that by conventional surgery. Over 90% of patients usually experience excellent to good outcome, about 5% and 3% show fair and poor results, respectively, according to the modified MacNab criteria at long-term follow-up.[47,48,54,55] Complications after this technique can be revision surgeries, dural lacerations, pseudomeningocele, and disc infection.[54,55]
Advantage of ILT Over Endoscopic TFT
The ILT can decompress root or the thecal sac caused by disc fragment, ligamentum flavum, facet hypertrophy, or the osteophytes, while TFT mainly relieves compression secondary to disc fragment. Although current evidence on the effectiveness of endoscopic TFT is poor and does not provide valid information to either support or refute using this surgery in symptomatic lumbar disc herniations,[56] proponents of TFT consider this procedure as the future gold standard for disc diseases.[57]
Disc herniations at L5-S1
The endoscopy-assisted ILT is a safe, effective, and minimally invasive procedure for the treatment of disc herniations at the L5-S1 level as compared to TFT.[34,58] Although trans iliac approach for L5-S1 disc is described in TFT,[59] it is technically difficult especially in the beginning. Although endoscopic TFT at the L5-S1 level remains a challenge because of the limited access by a high iliac crest, the sacral ala, large transverse processes of L5, and hidden disc fragments lateral to the zygapophyseal joint, foraminal retreat technique can be effective treatment method in appropriately selected patients.[60]
High-canal compromise and migrated disc
The results of central high-canal compromised (>50%) disc herniations are much better in ILT than in TFT. Similarly, high-grade migrations have higher failure rate as compared to low-grade migrations in TFT. Open surgery or ILT should be considered for herniations with high-canal compromise and high-grade migration. The decompression results of endoscopic ILT are equivalent to those of conventional procedures in high-canal stenosis and migrated disc. Endoscopy-assisted ILT can be used comfortably for highly migrated disc herniation even by less-experienced surgeons due to the familiar anatomy, as observed in open surgery.[61] Trauma to the access pathway and the spinal canal structures is reduced. Epidural scarring is minimized.[31,62] Although there are reports of treatment of migrated lumbar disc herniation just medial to pedicle with narrow ipsilateral intervertebral foramen via a contralateral route by TFT,[63] it is very difficult. Difficulty in treating migrated disc by TFT can also be overcome by “half-and-half” technique, “epiduroscopic” technique, and by using semi-rigid flexible curved probe by expert surgeons.[64]
Better outcome
Liu et al., analyzed results of both ILT and TFT and found that both the techniques are minimally invasive with similar safety profile for lumbar disc herniation. The long-term outcome of the ILT group, in term of Oswestry disability index (ODI) was better than that in TFT.[65]
Familiar anatomy
Most spinal surgeons are familiar to the anatomy of ILT than that of TFT.
Calcified disc
Endoscopy-assisted ILT is very effective in calcified disc. On the other hand, endoscopic TFT generally is not indicated for calcified discs.[66]
Uncooperative and anxious patient
Endoscopy-assisted ILT can be safely done under both general as well as local anesthesia. Surgery can be done in uncooperative and anxious patients in ILT. Moreover, the chances of root injury increase when general anesthesia is used in TFT. Psoas hematoma, though rare, can develop due to segmental vessel injury in TFT.[67]
Lumbar canal and lateral recess stenosis
Endoscopy-assisted ILT can be used effectively in LCS and lateral recess stenosis. The area of the dural tube can be increased up to 408.0% by ILT (range: 211-774%).[12,13,45,46] On the other hand, there is no valid evidence about the effectiveness of TFT endoscopic surgery for LCS.[68]
Exiting nerve root injury
The chance of exiting nerve root injury in ILT is extremely rare.[13] On the other hand, intraoperative risks of injury to the exiting root and blood vessel are more in TFT, especially when there is advanced loss of disc height, in patients with short pedicles, and osteophytes at the facet joint if general anesthesia is used.
Disadvantage of ILT Over TFT
Symptomatic recurrence
Symptomatic recurrences are more after ILT as compared to that after TFT. The disc herniation is postero lateral and, in the open space, after TFT; thus, the risk of subsequent sequestration of the disc material producing symptomatic recurrence is reduced.
Invasiveness
Endoscopy-assisted ILT is comparatively more invasive than TFT. Removal of the lower part of the superior lamina, the ligamentum flavum, and the medial part of the facet joint is required in ILT, while these structures are spared in TFT.
Complications
Complications such as perforations of the dura matter, pseudomeningocele formation, cerebrospinal fluid fistula, and meningitis are more common in ILT, especially in the initial learning curve.[55,65,69]
Simultaneous removal of intra spinal, foraminal, and extra foraminal herniated disc
Endoscopic TFT enables removal of the disc fragments from the intra spinal and extra spinal spaces simultaneously by a single approach.[70]
Learning curves
The learning curve of the TFT is steep and easy to learn, while it is flat and hard to master in the ILT.[71]
Limitations of ILT
Steep learning curve
Although posterior endoscopy-assisted ILT discectomy has advantages such as better illumination, good magnification, excellent visualization, minimal bone loss, less epidural fibrosis, less postoperative pain, better cosmetic results, shorter hospitalization, early mobilization, and shorter recovery, this procedure has a steep learning curve and the operative time is usually longer than that with open procedures in the beginning. Two-dimensional vision of endoscopic technique may cause loss of depth perception.[72] Obtaining microsurgical experience, attending workshops, and suitable patient selection can help shorten the learning curve and decrease complications.[73] Complications such as dural tears remains a concern during the learning stage of ILT.[55,69] Once definite learning curve is over and expertise is acquired, the results of this procedure are safe and effective.[74,75]
Conversion to open technique
Chances of conversion to open surgery decreases as the surgeon gains experience. Misplacement of working portal in relation to the pathology, bleeding, and difficulty in indentifying anatomy are potential causes for conversion to open surgery in the initial adoption to endoscopic technique. Endoscopic experience, proper patient selection, and specific radiographic examination can reduce incidence of conversion.[76]
Complications
Although most observers report similar complications rate in endoscopic, microsurgery, and open surgery, Teli et al. observed more complications after endoscopy technique.[69]
Conclusions
Endoscopy-assisted ILT has its merits and flaws. Patient selection and the surgeon's skill is critical to a successful procedure. It is important to properly select the patient and to strictly adhere to inclusion and exclusion criteria of the procedure to ensure a good outcome. When these criteria are disregarded, the results could be disappointing and may be dangerous. This procedure will stand the test of time and clinical trials and will prove to be valuable to the spine surgeons for treating lumbar diseases. Initial complications in this endoscopy-assisted technique could be more due to its steep learning curve. Obtaining endoscopic experience, attending workshops, and suitable patient selection can help shorten the learning curve and decrease complications. Once definite learning curve is achieved and expertise is acquired, this procedure is safe and effective.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gibson JN, Waddell G. Surgical interventions for lumbar disc prolapse: Updated Cochrane Review. Spine (Phila Pa 1976) 2007;32:1735–47. doi: 10.1097/BRS.0b013e3180bc2431. [DOI] [PubMed] [Google Scholar]
- 2.Postacchini F, Postacchini R. Operative management of lumbar disc herniation: The evolution of knowledge and surgical techniques in the last century. Acta Neurochir Suppl. 2011;108:17–21. doi: 10.1007/978-3-211-99370-5_4. [DOI] [PubMed] [Google Scholar]
- 3.Yadav YR, Yadav S, Sherekar S, Parihar V. A new minimally invasive tubular brain retractor system for surgery of deep intracerebral hematoma. Neurol India. 2011;59:74–7. doi: 10.4103/0028-3886.76870. [DOI] [PubMed] [Google Scholar]
- 4.Baron EM, Levene HB, Heller JE, Jallo JI, Loftus CM, Dominique DA. Neuroendoscopy for spinal disorders: A brief review. Neurosurg Focus. 2005;19:e5. doi: 10.3171/foc.2005.19.6.6. [DOI] [PubMed] [Google Scholar]
- 5.Yadav YR, Parihar V, Sinha M, Jain N. Endoscopic treatment of the suprasellar arachnoid cyst. Neurol India. 2010;58:280–3. doi: 10.4103/0028-3886.63772. [DOI] [PubMed] [Google Scholar]
- 6.Zohdi A, Elkheshin S. Endoscopic anatomy of the velum interpositum: A sequential descriptive anatomical study. Asian J Neurosurg. 2012;7:12–6. doi: 10.4103/1793-5482.95689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar A. Advances in neurosurgery: The Fujita Health University experience. Asian J Neurosurg. 2011;6:32–8. doi: 10.4103/1793-5482.85633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu BS, Xia Q, Ma XL, Yang Q, Ji N, Shah S, et al. The usefulness of magnetic resonance imaging for sequestered lumbar disc herniation treated with endoscopic surgery. J Xray Sci Technol. 2012;20:373–81. doi: 10.3233/XST-2012-0336. [DOI] [PubMed] [Google Scholar]
- 9.Li Q, Tian W, Liu B, Hu L, Wang YQ, Yuan N. Accurate nerve orientation before micro endoscopic discectomy for lumber disc prolapse. Zhonghua Yi Xue Za Zhi. 2007;87:1013–6. [PubMed] [Google Scholar]
- 10.Zhou Y, Wang J, Chu TW, Wang WD, Zheng WJ, Hao Y, et al. The clinical comparison of microendoscopic lumbar diskectomy with and without preservation of the ligamentum flavum. Zhonghua Wai Ke Za Zhi. 2005;43:1321–4. [PubMed] [Google Scholar]
- 11.Kim CH, Chung CK. Endoscopic interlaminar lumbar discectomy with splitting of the ligament flavum under visual control. J Spinal Disord Tech. 2012;25:210–7. doi: 10.1097/BSD.0b013e3182159690. [DOI] [PubMed] [Google Scholar]
- 12.Wada K, Sairyo K, Sakai T, Yasui N. Minimally invasive endoscopic bilateral decompression with a unilateral approach (endo-BiDUA) for elderly patients with lumbar spinal canal stenosis. Minim Invasive Neurosurg. 2010;53:65–8. doi: 10.1055/s-0030-1247559. [DOI] [PubMed] [Google Scholar]
- 13.Ikuta K, Tono O, Tanaka T, Arima J, Nakano S, Sasaki K, et al. Surgical complications of microendoscopic procedures for lumbar spinal stenosis. Minim Invasive Neurosurg. 2007;50:145–9. doi: 10.1055/s-2007-985152. [DOI] [PubMed] [Google Scholar]
- 14.Lysoń T, Mariak Z, Jadeszko M, Kochanowicz J, Lewko J. Results of Destandau microendoscopic lumbar discectomy. Neurol Neurochir Pol. 2008;42:105–11. [PubMed] [Google Scholar]
- 15.Oertel JM, Mondorf Y, Gaab MR. A new endoscopic spine system: The first results with “Easy GO”. Acta Neurochir (Wien) 2009;151:1027–33. doi: 10.1007/s00701-009-0454-7. [DOI] [PubMed] [Google Scholar]
- 16.Chiu JC. Endoscopic assisted lumbar microdecompressive spinal surgery with a new SMART endoscopic spine system. Surg Technol Int. 2006;15:234–41. [PubMed] [Google Scholar]
- 17.Husain M, Jha DK, Agrawal S, Husain N, Gupta RK. Conical working tube: A special device for endoscopic surgery of herniated lumbar discs. J Neurosurg Spine. 2005;2:265–70. doi: 10.3171/spi.2005.2.3.0265. [DOI] [PubMed] [Google Scholar]
- 18.Zhou W, Li LJ, Tan J. Treatment of degenerative lumbar spondylolisthesis by transforaminal lumbar interbody fusion with microendoscopic surgery. Zhongguo Gu Shang. 2010;23:251–3. [PubMed] [Google Scholar]
- 19.Gotfryd A, Avanzi O. A systematic review of randomised clinical trials using posterior discectomy to treat lumbar disc herniations. Int Orthop. 2009;33:11–7. doi: 10.1007/s00264-008-0559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li SH, Li HZ, Zhao JR. Clinical comparison between micro-endoscopic discectomy (MED) and open discectomy for treatment of lumbar disc herniation. Zhongguo Gu Shang. 2008;21:349–51. [PubMed] [Google Scholar]
- 21.Righesso O, Falavigna A, Avanzi O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: Results of a randomized controlled trial. Neurosurgery. 2007;61:545–9. doi: 10.1227/01.NEU.0000290901.00320.F5. [DOI] [PubMed] [Google Scholar]
- 22.Ruetten S. Full-endoscopic operations of the spine in disk herniations and spinal stenosis. Surg Technol Int. 2011;21:284–98. [PubMed] [Google Scholar]
- 23.Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes: Full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007;6:521–30. doi: 10.3171/spi.2007.6.6.2. [DOI] [PubMed] [Google Scholar]
- 24.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–9. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 25.Palmer S. Use of a tubular retractor system in microscopic lumbar discectomy: 1 year prospective results in 135 patients. Neurosurg Focus. 2002;13:e5. doi: 10.3171/foc.2002.13.2.6. [DOI] [PubMed] [Google Scholar]
- 26.Dezawa A, Mikami H, Sairyo K. Percutaneous endoscopic translaminar approach for herniated nucleus pulposus in the hidden zone of the lumbar spine. Asian J Endosc Surg. 2012;5:200–3. doi: 10.1111/j.1758-5910.2012.00142.x. [DOI] [PubMed] [Google Scholar]
- 27.Schick U, Döhnert J, Richter A, König A, Vitzthum HE. Microendoscopic lumbar discectomy versus open surgery: An intraoperative EMG study. Eur Spine J. 2002;11:20–6. doi: 10.1007/s005860100315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang TJ, Hsu RW, Li YY, Cheng CC. Less systemic cytokine response in patients following microendoscopic versus open lumbar discectomy. J Orthop Res. 2005;23:406–11. doi: 10.1016/j.orthres.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 29.Shin DA, Kim KN, Shin HC, Yoon do H. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. doi: 10.3171/SPI-08/01/039. [DOI] [PubMed] [Google Scholar]
- 30.Muramatsu K, Hachiya Y, Morita C. Postoperative magnetic resonance imaging of lumbar disc herniation: Comparison of microendoscopic discectomy and Love's method. Spine (Phila Pa 1976) 2001;26:1599–605. doi: 10.1097/00007632-200107150-00022. [DOI] [PubMed] [Google Scholar]
- 31.Ruetten S, Komp M, Godolias G. A New full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6-mm endoscopes: Prospective 2-year results of 331 patients. Minim Invasive Neurosurg. 2006;49:80–7. doi: 10.1055/s-2006-932172. [DOI] [PubMed] [Google Scholar]
- 32.Wang B, Lü GH, Li J, Kang YJ, Deng YW, Liu WD, et al. Contrast study of full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation. Zhonghua Wai Ke Za Zhi. 2011;49:74–8. [PubMed] [Google Scholar]
- 33.Choi G, Prada N, Modi HN, Vasavada NB, Kim JS, Lee SH. Percutaneous endoscopic lumbar herniectomy for high-grade down-migrated L4-L5 disc through an L5-S1 interlaminar approach: A technical note. Minim Invasive Neurosurg. 2010;53:147–52. doi: 10.1055/s-0030-1254145. [DOI] [PubMed] [Google Scholar]
- 34.Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58(Suppl 1):ONS59–68. doi: 10.1227/01.neu.0000192713.95921.4a. [DOI] [PubMed] [Google Scholar]
- 35.Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:e12. doi: 10.3171/foc.2003.15.3.12. [DOI] [PubMed] [Google Scholar]
- 36.Isaacs RE, Podichetty V, Fessler RG. Microendoscopic discectomy for recurrent disc herniations. Neurosurg Focus. 2003;15:e11. doi: 10.3171/foc.2003.15.3.11. [DOI] [PubMed] [Google Scholar]
- 37.Zhou Y, Wang J, Chu TW, Li CQ, Zhang ZF, Wang WD, et al. Micro-endoscopic strategies and options for recurrent lumbar disc herniation. Zhonghua Wai Ke Za Zhi. 2008;46:1475–9. [PubMed] [Google Scholar]
- 38.Smith JS, Ogden AT, Shafizadeh S, Fessler RG. Clinical outcomes after microendoscopic discectomy for recurrent lumbar disc herniation. J Spinal Disord Tech. 2010;23:30–4. doi: 10.1097/BSD.0b013e318193c16c. [DOI] [PubMed] [Google Scholar]
- 39.Ruetten S, Komp M, Merk H, Godolias G. Recurrent lumbar disc herniation after conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech. 2009;22:122–9. doi: 10.1097/BSD.0b013e318175ddb4. [DOI] [PubMed] [Google Scholar]
- 40.Kim CH, Chung CK, Jahng TA, Yang HJ, Son YJ. Surgical outcome of percutaneous endoscopic interlaminar lumbar diskectomy for recurrent disk herniation after open diskectomy. J Spinal Disord Tech. 2012;25:e125–33. doi: 10.1097/BSD.0b013e31825bd111. [DOI] [PubMed] [Google Scholar]
- 41.Koga S, Sairyo K, Shibuya I, Kanamori Y, Kosugi T, Matsumoto H, et al. Minimally invasive removal of a recurrent lumbar herniated nucleus pulposus by the small incised microendoscopic discectomy interlaminar approach. Asian J Endosc Surg. 2012;5:34–7. doi: 10.1111/j.1758-5910.2011.00118.x. [DOI] [PubMed] [Google Scholar]
- 42.O’Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: Cadaveric dissection and technical case report. Spine J. 2007;7:414–21. doi: 10.1016/j.spinee.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 43.Tonogai I, Sairyo K, Higashino K, Sakai T, Katoh S, Yasui N. Minimally invasive endoscopic removal of a herniated nucleus pulposus that had migrated to the S1 nerve root foramen. Minim Invasive Neurosurg. 2007;50:173–7. doi: 10.1055/s-2007-982510. [DOI] [PubMed] [Google Scholar]
- 44.Yoshimoto M, Takebayashi T, Kawaguchi S, Tsuda H, Ida K, Wada T, et al. Minimally invasive technique for decompression of lumbar foraminal stenosis using a spinal microendoscope: Technical note. Minim Invasive Neurosurg. 2011;54:142–6. doi: 10.1055/s-0031-1279716. [DOI] [PubMed] [Google Scholar]
- 45.Sairyo K, Sakai T, Higashino K, Inoue M, Yasui N, Dezawa A. Complications of endoscopic lumbar decompression surgery. Minim Invasive Neurosurg. 2010;53:175–8. doi: 10.1055/s-0030-1262814. [DOI] [PubMed] [Google Scholar]
- 46.Zhai XJ, Bi DW, Fu H, Zu G. Treatment of lumbar disc herniation with lateral recess stenosis by microendoscopic discectomy. Zhongguo Gu Shang. 2008;21:120–1. [PubMed] [Google Scholar]
- 47.Komp M, Hahn P, Merk H, Godolias G, Ruetten S. Bilateral operation of lumbar degenerative central spinal stenosis in full-endoscopic interlaminar technique with unilateral approach: Prospective 2-year results of 74 patients. J Spinal Disord Tech. 2011;24:281–7. doi: 10.1097/BSD.0b013e3181f9f55e. [DOI] [PubMed] [Google Scholar]
- 48.Yang B, Chen R, Xie P, Liu B, Dong J, Rong L. Microendoscopic decompression via unilateral approach for lumbar spinal stenosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2011;25:1158–63. [PubMed] [Google Scholar]
- 49.Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: A prospective, randomized, controlled study. J Neurosurg Spine. 2009;10:476–85. doi: 10.3171/2008.7.17634. [DOI] [PubMed] [Google Scholar]
- 50.Lu X, Peng H, Ling S, Wei W. Comparison of microendoscopic discectomy with open discectomy for degenerative lumbar spinal stenosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23:1200–3. [PubMed] [Google Scholar]
- 51.Inui A, Sairyo K, Katoh S, Higashino K, Sakai T, Shiiba M, et al. Extruded lumbar osseous endplate causing long-term radiculopathy in an adult: An endoscopic excision. Minim Invasive Neurosurg. 2006;49:55–7. doi: 10.1055/s-2005-919165. [DOI] [PubMed] [Google Scholar]
- 52.Matsumoto M, Watanabe K, Tuji T, Ishii K, Takaishi H, Nakamura M, et al. Microendoscopic discectomy for lumbar disc herniation with bony fragment due to apophyseal separation. Minim Invasive Neurosurg. 2007;50:335–9. doi: 10.1055/s-2007-993202. [DOI] [PubMed] [Google Scholar]
- 53.Zhang XB. Endoscopic surgical procedures for the treatment of multi-segment lumbar intervertebral disc herniation with posterior approach. Zhongguo Gu Shang. 2009;22:295–6. [PubMed] [Google Scholar]
- 54.Zhou Y, Wang M, Wang J, Chu TW, Zhang ZF, Li CQ. Clinical experience and results of lumbar microendoscopic discectomy: A study with a five-year follow-up. Orthop Surg. 2009;1:171–5. doi: 10.1111/j.1757-7861.2009.00039.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chang SS, Fu TS, Liang YC, Lia PL, Niu CC, Chen LH, et al. Results of microendoscopic discectomy performed in the 26 cases with a minimum 3 years follow-up. Chang Gung Med J. 2009;32:89–97. [PubMed] [Google Scholar]
- 56.Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for symptomatic lumbar disc herniations: A systematic review of the literature. Eur Spine J. 2010;19:181–204. doi: 10.1007/s00586-009-1155-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gibson JN, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: The future ‘gold standard’ for discectomy?-A review. Surgeon. 2012;10:290–6. doi: 10.1016/j.surge.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 58.Chen HT, Tsai CH, Chao SC, Kao TH, Chen YJ, Hsu HC, et al. Endoscopic discectomy of L5-S1 disc herniation via an interlaminar approach: Prospective controlled study under local and general anesthesia. Surg Neurol Int. 2011;2:93. doi: 10.4103/2152-7806.82570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choi G, Kim JS, Lokhande P, Lee SH. Percutaneous endoscopic lumbar discectomy by transiliac approach: A case report. Spine (Phila Pa 1976) 2009;34:e443–6. doi: 10.1097/BRS.0b013e31817c4f39. [DOI] [PubMed] [Google Scholar]
- 60.Lübbers T, Abuamona R, Elsharkawy AE. Percutaneous endoscopic treatment of foraminal and extraforaminal disc herniation at the L5-S1 level. Acta Neurochir (Wien) 2012;154:1789–95. doi: 10.1007/s00701-012-1432-z. [DOI] [PubMed] [Google Scholar]
- 61.Kim CH, Chung CK, Woo JW. Surgical Outcome of Percutaneous Endoscopic Interlaminar Lumbar Discectomy for Highly Migrated Disc Herniation. J Spinal Disord Tech. 2012 Oct 15; [Google Scholar]
- 62.Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, et al. Operative failure of percutaneous endoscopic lumbar discectomy: A radiologic analysis of 55 cases. Spine (Phila Pa 1976) 2006;31:e285–90. [PubMed] [Google Scholar]
- 63.Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: A technical case report. Spine (Phila Pa 1976) 2011;36:e1173–8. doi: 10.1097/BRS.0b013e3182264458. [DOI] [PubMed] [Google Scholar]
- 64.Chae KH, Ju CI, Lee SM, Kim BW, Kim SY, Kim HS. Strategies for noncontained lumbar disc herniation by an endoscopic approach: Transforaminal suprapedicular approach, semi-rigid flexible curved probe, and 3-Dimensional reconstruction CT with discogram. J Korean Neurosurg Soc. 2009;46:312–6. doi: 10.3340/jkns.2009.46.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu WG, Wu XT, Min J, Guo JH, Zhuang SY, Chen XH, et al. Long-term outcomes of percutaneous lumbar discectomy and microendoscopic discectomy for lumbar disc herniation. Zhonghua Yi Xue Za Zhi. 2009;89:750–3. [PubMed] [Google Scholar]
- 66.Ranjan A, Lath R. Microendoscopic discectomy for prolapsed lumbar intervertebral disc. Neurol India. 2006;54:190–4. [PubMed] [Google Scholar]
- 67.Kim HS, Ju CI, Kim SW, Kim JG. Huge psoas muscle hematoma due to lumbar segmental vessel injury following percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2009;45:192–5. doi: 10.3340/jkns.2009.45.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nellensteijn J, Ostelo R, Bartels R, Peul W, van Royen B, van Tulder M. Transforaminal endoscopic surgery for lumbar stenosis: A systematic review. Eur Spine J. 2010;19:879–86. doi: 10.1007/s00586-009-1272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, et al. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19:443–50. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kitagawa Y, Sairyo K, Shibuya I, Kitahama Y, Kanamori Y, Koga S, et al. Minimally invasive and simultaneous removal of herniated intracanal and extracanal lumbar nucleus pulposus with a percutaneous spinal endoscope. Asian J Endosc Surg. 2012;5:183–6. doi: 10.1111/j.1758-5910.2012.00144.x. [DOI] [PubMed] [Google Scholar]
- 71.Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2012 doi: 10.1007/s00586-012-2540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Oztürk C, Tezer M, Aydogan M, Sarier M, Hamzaoglu A. Posterior endoscopic discectomy for the treatment of lumbar disc herniation. Acta Orthop Belg. 2006;72:347–52. [PubMed] [Google Scholar]
- 73.Wang B, Lü G, Patel AA, Ren P, Cheng I. An evaluation of the learning curve for a complex surgical technique: The full endoscopic interlaminar approach for lumbar disc herniations. Spine J. 2011;11:122–30. doi: 10.1016/j.spinee.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 74.Jhala A, Mistry M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J Orthop. 2010;44:184–90. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yadav YR, Parihar V, Namdev H, Agarwal M, Bhatele PR. Endoscopic inter laminar management of lumbar disc disease. J Neurol Surg A Cent Eur Neurosurg. 2013;74:77–81. doi: 10.1055/s-0032-1333127. [DOI] [PubMed] [Google Scholar]
- 76.Wang B, Lü G, Liu W, Cheng I, Patel AA. Full-endoscopic interlaminar approach for the surgical treatment of lumbar disc herniation: The causes and prophylaxis of conversion to open. Arch Orthop Trauma Surg. 2012;132:1531–8. doi: 10.1007/s00402-012-1581-9. [DOI] [PubMed] [Google Scholar]