Abstract
Various intraventricular tumors can present with calcifications; however, the choroid plexus can also have physiological calcifications. This is the first case report of meningiomas located at the bilateral foramen of Monro (FOM), concealed by a grossly calcified choroid plexus, presenting with obstructive hydrocephalus. A 60-year-old woman with disturbed consciousness was admitted by ambulance. Head computed tomography revealed significantly high-density lesions that smoothly extended from the choroid plexus of the lateral ventricles to the third ventricle. They occupied both sides of the FOM, resulting in obstructive hydrocephalus. The diagnostic endoscopic biopsy was performed using a flexible neuroendoscopic system, and an egg shell-like grossly calcified choroid plexus was found to smoothly extend toward the FOM. Resection was not selected because the calcified lesions had tightly adhered to the veins and fornix; therefore, the patient underwent ventriculo-peritoneal shunting. The lesions were histologically identified as psammomatous meningiomas with low proliferation potential (the Ki-67 labeling index was lower than 1%). She was discharged 10 days after surgery without neurological deficits. As calcifications can have tumoral and nontumoral origins, we considered neuroendoscopic exploration to be essential in order to achieve an accurate diagnosis and select optimal management.
Keywords: Calcification, choroid plexus, neuroendoscope, obstructive hydrocephalus
Introduction
Various neoplasms may arise in the ventricular system, and include ependymomas, subependymomas, central neurocytomas, subependymal giant cell astrocytomas, choroid plexus neoplasms, gliomas, pseudotumors, and meningiomas.[1,2] Although these lesions are often associated with calcifications, approximately 12–66.2% of the choroid plexus cases reported to date have had physiological calcifications without any evidence of disease.[3,4]
A meningioma is one of the most common tumors detected in the ventricles; however, the foramen of Monro (FOM) is an uncommon site of origin.[5,6] Meningiomas have been associated with calcifications, and histologically with psammomatous bodies.[7,8,9] While partial calcification is typically detected in some large tumors, small meningiomas at the bilateral FOM, which are indistinguishable from a contiguous calcified choroid plexus, are extremely rare.
We herein presented a rare case of grossly calcified meningiomas at the bilateral FOM causing obstructive hydrocephalus. The application of a neuroendoscope was useful to achieve an accurate diagnosis and appropriate treatment options.
Case Report
A 60-year-old woman with disturbed consciousness was admitted by ambulance. Her Glasgow Coma Scale was 14 (E4V4M6). She had no treatment history of endocrinological diseases. Head computed tomography without contrast material revealed dilated lateral ventricles without third or fourth ventricle dilatation. Significantly high-density lesions smoothly extended from the choroid plexus of the lateral ventricles to the third ventricle and occupied both sides of the FOM [Figure 1a and b]. Magnetic resonance imaging showed that the choroid plexuses were modestly enhanced with gadolinium, but there was no obvious tumoral lump, which indistinguishable from the contiguous choroid plexus [Figure 1c]. The diagnostic endoscopic biopsy was performed using a flexible neuroendoscopic system (EVIS LUCERA SPECTRUM Video Imaging System, Olympus, Tokyo) via the left lateral ventricle. Egg shell-like entirely calcified lesions that smoothly extended toward the FOM were detected [Figure 2a and b]. The contralateral FOM was inspected through the spontaneously perforated septum pellucidum and was also found to be occluded by the calcified lesions. Most of these calcified lesions were too hard to resect; therefore, a biopsy was performed to obtain a small specimen from relatively less calcified lesions near the FOM. Resection was not selected because the calcified lesions had tightly adhered to the veins and fornix; therefore, the patient underwent ventriculo-peritoneal shunting via the same tract [Figure 1d]. A histological examination of the specimen revealed a number of psammoma bodies with round and spindle tumor cells [Figure 3a]. Mitosis was scarcely observed, and the immunohistochemical staining index for Ki-67 was <1% [Figure 3b]. She was histopathologically diagnosed with psammomatous meningiomas (WHO Grade I). She was alert and conscious postoperatively and was subsequently discharged 10 days after surgery.
Figure 1.
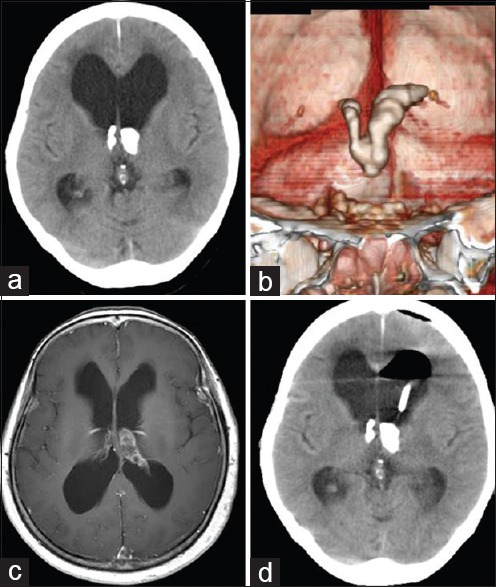
(a) Head computed tomography showing ventricular dilatation and foramen of Monro occlusion with significantly high-density lesions. (b) The coronal view of three-dimensional computed tomography revealed that the high-density lesions continuously extended from the choroid plexus of the lateral ventricles to the third ventricle. (c) Head magnetic resonance imaging is showing modest enhancement of the choroid plexus by gadolinium without an obvious tumoral lump. (d) Postoperative computed tomography showing that the placement of the ventriculo-peritoneal shunt
Figure 2.
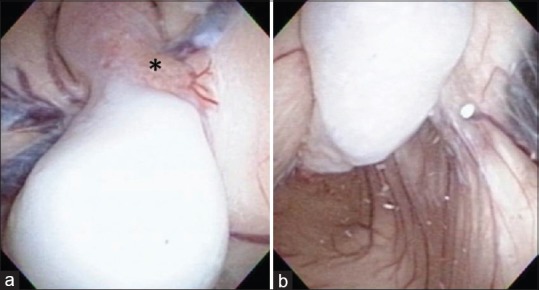
(a and b) Intraoperative view with a flexible neuroendoscope showing an entirely calcified lesion consecutive from the choroid plexus in the ventricle body (a) toward the foramen of Monro (b). Biopsy was performed, and a small specimen was obtained from the relatively less calcified part (a) asterisk
Figure 3.
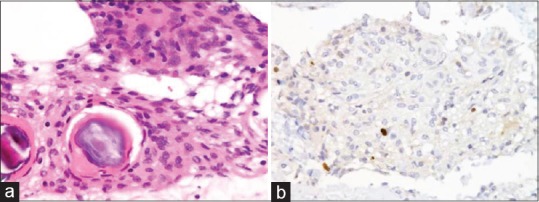
(a) Hematoxylin and eosin staining showing a meningioma with abundant psammoma bodies. (b) Immunohistochemical staining for Ki-67 showing a low staining index of <1%
Discussion
To the best of our knowledge, this is the first case report of FOM meningiomas concealed by a grossly calcified choroid plexus, presenting with obstructive hydrocephalus. Some tumors around the FOM such as central neurocytomas, subependymomas, and subependymal giant cell astrocytomas have been reported with calcifications and are known to cause obstructive hydrocephalus.[2,10,11] While meningiomas have also been associated with calcifications,[9] bilateral FOM meningiomas, which are indistinguishable from a contiguous calcified choroid plexus, are extremely rare and apparently unique.
Calcified tumors are empirically considered to be slow growing. Nakasu et al. reported that calcified meningiomas had lower proliferation potentials than those without calcifications.[12] Our case was histologically shown to have no malignancy, and the Ki-67 labeling index was <1%. Grossly calcified tumors may expand slowly but steadily at both sides of the FOM, thereby causing obstructive hydrocephalus. This may be an extremely rare situation.
In our case, the origin of the calcified tissue is uncertain whether the meningioma or choroid plexus itself, because the biopsied specimen is small. Furthermore, the underlying mechanism of the unusual calcification remains unclear. Psammoma bodies are considered to be formed by a process of dystrophic calcification associated with arachnoid cells and collagen fibers.[7] It may occur at the site of inflammation or in the choroid plexus and arachnoid under physiological conditions. Barresi et al. reported that osteoblastic meningiomas expressed osteogenic markers such as osteopoietin.[13] Although calcified meningiomas are generally believed to be the precursors of osteoblastic meningiomas, a difference may exist between calcification and ossification.[14] We did not perform a more extensive immunohistochemical analysis because the specimen obtained was too small and biopsied from the less-calcified part of the tumor. Further examinations of osteogenic markers should address this important issue.
Aggressive tumor resection was another option for our patient. However, our neuroendoscopic findings strongly suggested massive calcification of the choroid plexus with an egg shell-like appearance, and no border was detected within the calcified lesions. Furthermore, the lesions had tightly adhered to vital structures around the FOM such as the fornix, thalamostriate, and septal veins. Based on the benign nature of these tumors, the patient underwent ventriculo-peritoneal shunting to reduce the risk of memory disturbances and bleeding.
Conclusion
We presented an extremely rare case of meningiomas concealed within a grossly calcified choroid plexus. Although preoperative radiographical images were interesting but nondiagnostic, intraoperative neuroendoscopic findings were outstanding. The neuroendoscope was invaluable for exploring the attributes of intraventricular tumors and deciding treatment strategies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bramwit M, Kalina P, Rustia-Villa M. Inflammatory pseudotumor of the choroid plexus. AJNR Am J Neuroradiol. 1997;18:1307–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Smith AB, Smirniotopoulos JG, Horkanyne-Szakaly I. From the radiologic pathology archives: Intraventricular neoplasms: Radiologic-pathologic correlation. Radiographics. 2013;33:21–43. doi: 10.1148/rg.331125192. [DOI] [PubMed] [Google Scholar]
- 3.Daghighi MH, Rezaei V, Zarrintan S, Pourfathi H. Intracranial physiological calcifications in adults on computed tomography in Tabriz, Iran. Folia Morphol (Warsz) 2007;66:115–9. [PubMed] [Google Scholar]
- 4.Sedghizadeh PP, Nguyen M, Enciso R. Intracranial physiological calcifications evaluated with cone beam CT. Dentomaxillofac Radiol. 2012;41:675–8. doi: 10.1259/dmfr/33077422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erman T, Göcer AI, Erdogan S, Boyar B, Hacyakupoglu S, Zorludemir S. Intraventricular meningiomas: A review and report of eight cases. Neurosurg Q. 2004;14:154–60. [Google Scholar]
- 6.Ødegaard KM, Helseth E, Meling TR. Intraventricular meningiomas: A consecutive series of 22 patients and literature review. Neurosurg Rev. 2013;36:57–64. doi: 10.1007/s10143-012-0410-5. [DOI] [PubMed] [Google Scholar]
- 7.Alcolado JC, Moore IE, Weller RO. Calcification in the human choroid plexus, meningiomas and pineal gland. Neuropathol Appl Neurobiol. 1986;12:235–50. doi: 10.1111/j.1365-2990.1986.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 8.Das DK. Psammoma body: A product of dystrophic calcification or of a biologically active process that aims at limiting the growth and spread of tumor? Diagn Cytopathol. 2009;37:534–41. doi: 10.1002/dc.21081. [DOI] [PubMed] [Google Scholar]
- 9.Oya S, Kim SH, Sade B, Lee JH. The natural history of intracranial meningiomas. J Neurosurg. 2011;114:1250–6. doi: 10.3171/2010.12.JNS101623. [DOI] [PubMed] [Google Scholar]
- 10.Chen CL, Shen CC, Wang J, Lu CH, Lee HT. Central neurocytoma: A clinical, radiological and pathological study of nine cases. Clin Neurol Neurosurg. 2008;110:129–36. doi: 10.1016/j.clineuro.2007.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain A, Amin AG, Jain P, Burger P, Jallo GI, Lim M, et al. Subependymoma: Clinical features and surgical outcomes. Neurol Res. 2012;34:677–84. doi: 10.1179/1743132812Y.0000000064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakasu S, Nakajima M, Matsumura K, Nakasu Y, Handa J. Meningioma: Proliferating potential and clinicoradiological features. Neurosurgery. 1995;37:1049–55. doi: 10.1227/00006123-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Barresi V, Caffo M, Ieni A, Alafaci C, Tuccari G. Osteoblastic meningiomas: Clinico-pathological and immunohistochemical features of an uncommon variant. J Neurooncol. 2011;105:225–32. doi: 10.1007/s11060-011-0588-3. [DOI] [PubMed] [Google Scholar]
- 14.Kitagawa M, Nakamura T, Aida T, Iwasaki Y, Abe H, Nagashima K. Clinicopathologic analysis of ossification in spinal meningioma. Noshuyo Byori. 1994;11:115–9. [PubMed] [Google Scholar]


