Abstract
Advances in wireless devices and mobile technology offer many opportunities for delivering just-in-time adaptive interventions (JITAIs)--suites of interventions that adapt over time to an individual’s changing status and circumstances with the goal to address the individual’s need for support, whenever this need arises. A major challenge confronting behavioral scientists aiming to develop a JITAI concerns the selection and integration of existing empirical, theoretical and practical evidence into a scientific model that can inform the construction of a JITAI and help identify scientific gaps. The purpose of this paper is to establish a pragmatic framework that can be used to organize existing evidence into a useful model for JITAI construction. This framework involves clarifying the conceptual purpose of a JITAI, namely the provision of just-in-time support via adaptation, as well as describing the components of a JITAI and articulating a list of concrete questions to guide the establishment of a useful model for JITAI construction. The proposed framework includes an organizing scheme for translating the relatively static scientific models underlying many health behavior interventions into a more dynamic model that better incorporates the element of time. This framework will help to guide the next generation of empirical work to support the creation of effective JITAIs.
Introduction
Advances in mobile technology offer many opportunities for delivering interventions that accommodate an individual’s immediate needs (Riley et al., 2011). The term just-in-time adaptive interventions (JITAIs) (Spruijt-Metz & Nilsen, 2014) is used to describe a suite of interventions that adapt over time to an individual’s time-varying status, with the goal to address the individual’s changing needs for support. The widespread, everyday use of technologies such as mobile phones, smartphones, laptops and tablets, along with the variety of sensors included in these tools (e.g., accelerometer, GPS, light sensor, microphone) make these interventions increasingly more feasible. Further, mobile health (mHealth) interventions that provide timely support exist for a wide range of behavioral health issues, such as physical activity (King et al. 2013), alcohol use (Gustafson et al., 2014), smoking cessation (Riley, Obermayer, & Jean-Mary, 2008), obesity (Patrick et al., 2009), and mental illnesses (Ben-Zeev et al., 2014). These interventions are either used as standalone programs or in conjunction with traditional treatments (Price et al., 2014; Ben Zeev et al., 2014).
Despite their appealing nature, a major gap exists between the technological capacity to deliver JITAIs and existing health behavior models. Establishing a scientific model is an important step in developing interventions (Collins, Murphy, & Bierman, 2004). The models currently used to guide the design behavioral interventions largely emphasize static relationships, focusing on risk and protective factors that change relatively slowly, such as psychiatric diagnoses, or not at all, such as past high-risk behaviors (Spruijt-Metz et al., 2015). JITAIs, however, seek to address risk and protective factors that change (often rapidly) over time, such as mood, location and social interactions (Csikszentmihalyi & Rathunde, 1993). A major challenge concerns the integration of existing knowledge on health behavior or mechanisms of behavior change into a scientific model that can inform the construction of a JITAI.
The aim of this paper is to establish a pragmatic framework that can be used to organize existing and new evidence into a useful model for JITAI construction. This framework can help JITAI developers think through key factors and effects in a way that can inform the design of JITAIs and guide further empirical work. We first clarify the conceptual purpose of a JITAI and review its elements. We then offer questions to guide the establishment of a useful scientific model. We conclude with a discussion of limitations and directions for future research.
What is a JITAI?
To clarify the conceptual purpose of JITAIs, we elaborate on the two key concepts that distinguish these interventions from standard intervention designs: just-in-time and adaptive.
Just-In-Time (JIT)
The concept JIT has long traditions in various fields. For example, in industrial management and operation research, JIT is a philosophy that seeks to “produce the right item, at the right time, in the right quantities” (Canel, Rosen & Anderson, 2000, pp.52). It is based on a management plan that emphasizes continuous improvement and eliminates “waste”— defined as anything that does not add value to the product. In education, the term JIT is rooted in instructional approaches that focus on real-life tasks as the driving force for learning. Because these tasks and the real-life context in which they are performed involve high cognitive load, these approaches emphasize the need to take the limited human-processing capacity into account. Hence, strategies for scaffolding include JIT support, meaning providing the type of support needed, precisely when needed, and only when needed (Merrienboer, Kirschner, & Kester, 2003). Overall, these and other traditions (e.g., Drews et al., 2007; Karolak & Karolak, 1995), conceptualize JIT as the effective provision of timely support, operationalized by offering the type of support needed, precisely when needed, in a way that minimizes waste (i.e., anything that does not benefit the person) and accommodates the real-life setting in which support is needed.
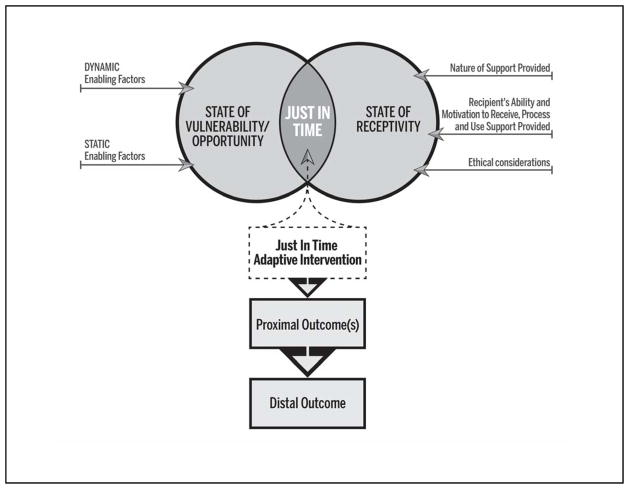
We build on the traditions above, as well as others (e.g., Morris, Intille & Beaudin, 2005) to define the JIT approach in the context of health behavior interventions as the precise provision of support whenever the person is (a) vulnerable and/or open to positive changes, and (b) receptive. To make this concrete, throughout the paper we discuss the case of ‘Joe,’ an employed individual who engages in hazardous drinking (HD)1 mainly after work hours and weekends.
State of vulnerability/opportunity
Stress-vulnerability and coping theories (e.g., Lazarus, 1993; Zubin & Spring, 1977) conceptualize a vulnerable state as the person’s transient tendency to experience adverse health outcomes or to engage in maladaptive behaviors. A vulnerable state is a function of the interplay between relatively stable factors (e.g., socioeconomic status) and more dynamic factors ranging from relatively rare major life events (e.g., unemployment), to more transient experiences (e.g., conflict with coworkers).
For example, consider a scenario where Joe, an adult child of an alcoholic parent, experiences a conflict with a coworker. The interplay between Joe’s (stable) pre-dispositions for HD and the (dynamic) stressful experiences at work mark a state of vulnerability to HD. That is, these condictions increase the chances that Joe will engage in HD at the end of the work day. To break the link between the vulnerable state and HD, JIT support might be provided to help Joe regulate the negative emotions induced by the conflict (e.g., in the form of a recomandation to engage in emotion–regulation excecises).
With regard to opportunities for positive change, various learning and motivational theories highlight the importance of concepts such as shaping (i.e., training by reinforcing successively improving approximations of a desired behavior: Bouton, 2007; Ferster & Skinner, 1957) and teachable moments (i.e., a time when a person is more likely to internalize information and take action; e.g., Fisher, Piazza, & Roane, 2011). The underlying assumption is that in order to facilitate improvement in some behavioral or cognitive domain, it is important to identify transient oportunities for learning and provide the type of support needed, only when needed in order to gradually move the person’s actions/cognitions in the desired direction.
For example, when Joe is in a bar with his friends, JIT support might be provided in the form of questions (delivered via an app notification) that help Joe become more aware of his drinking, learn how it is influenced by his friends, and reflect on potential consequences (see Walters et al., 2009).
State of receptivity
To further minimize waste and accommodate the real-life setting in which support is often needed, it is critical to ensure that the person is in a state where s/he is receptive to support. Integrating research in the area of supportive communication and ubiquitous computing (e.g., Ho & Intille, 2005; McIntosh, Seaton, & Jeffrey, 2007; Sarker et al., 2014), we define receptivity as the conditions in which the person can receive, process, and use the support provided. A variety of facets can impact receptivity.
The dual process theory of supportive communication outcomes (Burleson, 2009) suggests that receptivity is a function of two elements. The first– the nature of support– emphasizes how demanding the support is on the individual. This is influenced by aspects related to the type and the design of support, including the content (e.g., complicated messages would be more demanding), the media deployed (e.g., text, video, audio; see Mohr et al., 2014) and the use of paraverbal and/or nonverbal cues that are less cognitively demanding (e.g., images or colors that trigger specific associations or heuristics; see Castelo et al., 2012; Evans, 2008; Friesen, Hamel & McLeod, 2013). The second – the recipient’s ability or motivation to receive, process and use the support – can be influenced by stable (e.g., personality, working memory capacity) and dynamic factors (e.g., emotions, presence of distracters; Burleson, 2009).
Research in human-computer interaction articulates ways to enhance motivation/ability by improving the usability of interventions. For example, Consolvo, McDonald, and Landay (2009) generated eight guidelines (e.g., abstract and reflective, unobtrusive) to guide the design of support for real-world use. Other research has focused on the balance between perceived usefulness/value and perceived burden of support (e.g., Polonsky, Fisher, Hessler, & Edelman, 2014), along with heuristics to simplify supportive content (Fogg, 2009).
An important facet to consider with regard to receptivity is the ethics of intervening in a real-life setting. Ethical considerations such as privacy, confidentiality, safety and the general welfare of the recipient might lead to the decision not to provide certain types of support (although they are needed), or to modify the type of support provided (including the media deployed to deliver support: Kjeldskov, Skov, Als, & Høegh, 2004). For example, if Joe is experiencing distress2 while driving a car, it might not be safe to deliver an emotion-regulation recommendation in the form of a text message because Joe might get distracted; and if Joe is experiencing distress while in a meeting, providing an emotion-regulation recommendation in the form of a phone call or a ping might be disruptive (De Costa et al., 2010).
Other evidence can help explain (e.g., Naughton, Jamison, & Sutton, 2013), and devise strategies for addressing (e.g., systems that manage mobile phone interruptions: Zulkernain, Madiraju, & Ahamed, 2010) unreceptivity, building the foundation for future research aiming to identify and accommodate conditions in which a person might not be receptive to specific types of support.
Adaptation
The discussion above suggests that JIT support can be operationalized by offering the right type of support only when the person is (a) vulnerable or open to positive changes, and (b) receptive to support. This requires a strategy for adapting support provision.
For clarity, we use the term individualization to describe the use of information about the individual to make decisions concerning when, where and how to intervene. We distinguish between individualization that is static, where relatively stable information (e.g., gender, baseline severity of symptoms) is used to make intervention-related decisions (e.g., to offer intervention package A or B); and dynamic, where time-varying information (e.g., changes in psychological distress, response to an intervention) is used to make intervention decisions during the course of the intervention (e.g., changing the type, dosage, or timing of support). The term adaptive is used to describe this dynamic form of individualization (Collins et al., 2004).
Building on the above terminology, we conceptualize the JITAI as an intervention design that uses a dynamic form of individualization to operationalize the provision of JIT support. JITAIs operationalize the individualization of support provision based on ongoing assessments of the individual’s state and ecological context. The goal is to offer the right type of support precisely when, and only when, the person is in a state of vulnerability/opportunity and receptivity. For example, in the case of Joe, adaptation might be in the form of using ongoing information about Joe’s emotions, behaviors and context to trigger a recommendation only when Joe is experiencing distress (state of vulnerability) and is not driving a car (state of receptivity).
The detection of such states, and hence the feasibility of JITAIs, becomes increasingly possible with the growing availability of technology such as wearable and ubiquitous computing sensors (e.g., wearable activity monitors, home automation systems such as a smart thermometer), mobile-phone-based sensing (e.g., GPS, light sensors, microphones), digital footprints (e.g., social media interactions, email, digital calendars), and low-effort self-reporting (e.g., ecological momentary assessment [EMA]) (Hekler, Klasnja, Traver, & Hendriks, 2013).
Elements of a JITAI
With the conceptual purpose of a JITAI established, we turn to its key elements (see Nahum-Shani et al., 2014). The distal outcome is the ultimate goal of the JITAI. The proximal outcomes are the short-term goals the intervention is intended to achieve and are often mediators of the distal outcome. Decision points are times when an intervention option is selected based on currently available information (e.g., at 2pm, every hour). Intervention options are the array of possible type/dose/timing/delivery-mode of support that might be employed at any given decision point. Tailoring variables are baseline and time-varying information that informs which intervention option to offer at each decision point (e.g., distress, driving). Finally, decision rules operationalize the individualization by specifying which intervention option to offer at each decision point. Figure 1 provides concrete examples of these elements.
Figure 1.
JITAI Example
The Technology-Science Gap
Current scientific models guiding the development of health behavior interventions fail to capture the dynamic processes underlying states of vulnerability/opportunity and receptivity (Riley 2014). Even dynamic models that acknowledge the role of episodic factors in health behavior (see e.g., Witkiewitz & Marlatt, 2004) do not specify the temporal nature of each factor in a way that informs when, where, or how to intervene. Although many health behavior models acknowledge individual differences in response to treatment, in most cases these models can only inform static individualization (i.e., using information such as age or baseline symptom severity to make intervention decisions). A major step in building the scientific foundation for developing effective JITAIs is to articulate a pragmatic framework guided by specific questions that must be answered to create a JITAI. Below, we offer a set of pragmatic questions to help JITAI developers lay out key factors and effects in a way that can inform the dynamic individualization required for JIT support. These questions can be used to develop and refine scientific models and inform prioritization of future studies.
New Pragmatic Framework
To build high quality JITAIs, existing evidence should be organized into a scientific model that can help investigators identify and devise a plan to address states of vulnerability/opportunity and receptivity. The following questions can be used to facilitate the development of such a model. For illustration, we will use a hypothetical example in which an investigator wishes to build an intervention for full-time employees (ages 30–65) who exhibit HD. These questions can be broken down into three areas of emphasis: (1) defining the problem; (2) defining JIT in this context; and (3) formulating the adaptation strategy. Figure 2 provides a conceptual summary of the proposed framework.
Figure 2.
Summary of Pragmatic Framework for Developing JITAIs
Defining the Problem
(1) Whom are you trying to help?
The goal is to identify a target population and articulate key attributes of the target population that should be considered (e.g., employed individuals might be unable to use time-intensive interventions at work). This step can be aided by using formative work, such as clinical experience with the target population and user-centered design methods (e.g., interviews, sketching to elicit opinions; Buxton, 2010).
(2) What is the distal outcome of the JITAI?
This involves articulating a clinically meaningful goal. In our hypothetical example, a distal outcome might be to transition employees who engage in HD to non-hazardous drinking patterns in the course of a year.
(3) What is the temporal progression of key factors towards the distal outcome?
This involves articulating a dynamic model that incorporates the element of time. Because this is a unique and essential step in the process of establishing a useful model for constructing a JITAI, we describe this step in great detail, providing an organizing scheme.
The goal of this organizing scheme is to help JITAI developers think through key factors and effects and specify their temporal progression towards the distal outcome. The term temporal progression refers to the way in which the process leading to the distal outcome unfolds over time and what role each factor and effect plays. Note that progression is not necessarily linear or straightforward3. The task of describing the temporal progression can be simplified by using timescales to organize the key factors and their effects.
Building on theories in organizational research (Zaheer, Albert & Zaheer, 1999), we define a timescale as the size of the temporal interval used to build or test a theory about a process, pattern, phenomenon, or event. Timescales partition the temporal continuum into units, and can be conceptualized as levels in a hierarchy, with lower levels representing shorter timescales, and higher levels representing longer timescales. For example, hours can be conceptualized as lower level units nested within a day, and as a higher level unit within which minutes are nested. The same phenomenon can be associated with several types of timescales. The meaning of the phenomenon and the relationships between factors might vary depending on the timescale (Zaheer et al., 1999).
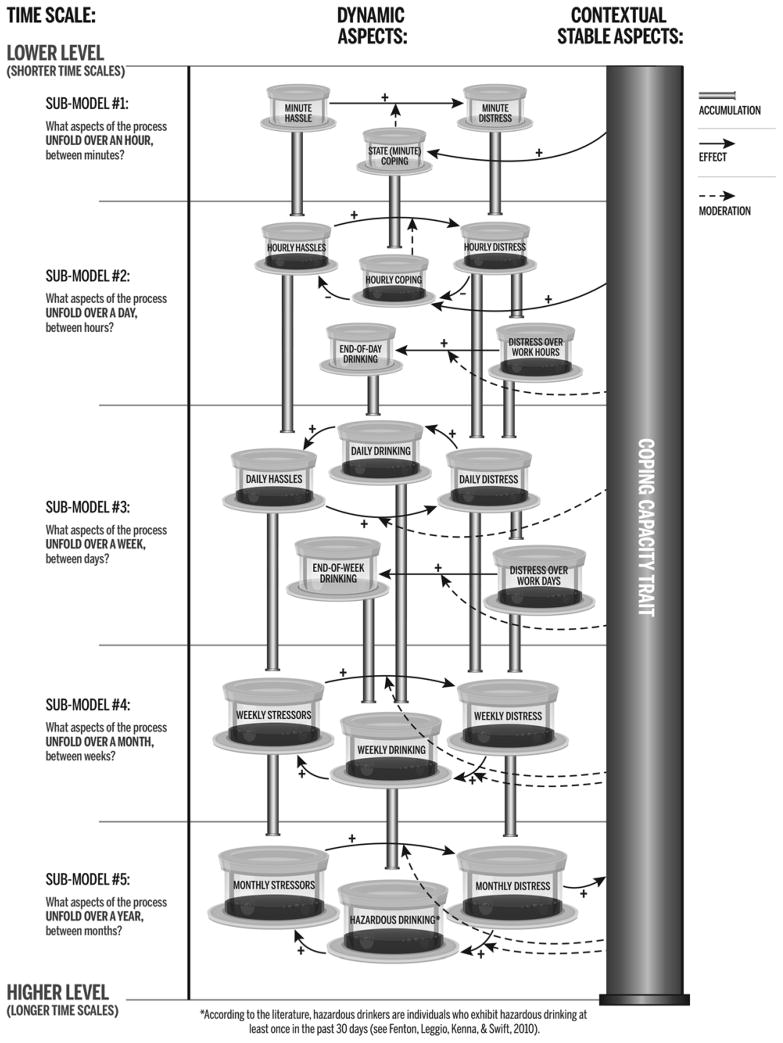
Here, we offer an approach for using timescales to organize existing and new evidence in a way that can describe progression towards the distal outcome and enable investigators to identify open scientific questions. This approach involves (a) identifying different time scales; (b) specifying dynamics within each time scale; and (c) specifying how factors and effects at different timescales are related. Below, we illustrate this approach by using a relatively simplified4 hypothetical model of stress, coping and employee drinking5 (see Figure 3).
Figure 3.
Illustrative Dynamic Model of Employee Stress Reactivity, Coping and Drinking
Identifying different timescales
The goal is to identify different timescales, within which the process leading to the distal outcome might unfold. For example, the hypothetical model in Figure 3 builds on existing evidence on stress, coping, and employee drinking to identify five key timescales within which the process leading to hazardous drinking patterns is expected to unfold (i.e., an hour, day, week, month and a year; where a year is the unit of the distal outcome).
Specifying dynamics within each timescale
This involves specifying what aspects of the process are likely to occur within each timescale, using key factors and effects at a lower level (i.e., shorter) timescale. The focus should be on describing how key factors and effects are ordered and related over time.
Returning to our hypothetical model6, the process in Figure 3 begins with hours as the higher level units, seeking to describe aspects of the process that unfold between minutes or several minutes (Sub-model #1). Here, we build on research suggesting that work-related hassles (e.g., losing things, arguments; Kanner, Coyne, Schaefer, & Lazarus, 1981) can occur at any given minute and generate rather immediate psychological distress (Sinha et al., 2003). This immediate stress reaction can be attenuated to the extent that the person’s state coping capacity is high (i.e., the extent to which, at a given time point, the person is able to employ adaptive strategies to manage psychological stress; Lazarus, 1993). State coping capacity is a function of the trait coping capacity of the person (Roesch et al., 2010)--defined as a variety of relatively stable “trait-like” attributes (e.g., hardiness, dispositional optimism) that contribute to the management of stress (Hobfoll, 1989; Kessler et al., 1985; Roesch et al., 2010). Of course, state coping capacity is a function other important contextual variables, which for simplicity are not captured in this model.
We then move up the timescale, seeking to describe aspects of the process leading to employee drinking that unfold over a day, using hours as the unit for variables and effects (sub-model #2); followed by describing aspects of the process that unfold in the course of a week, using days as the unit for variables and effects (sub-model #3); then describing aspects of the process that unfold over a month, using weeks as the unit for variables and effects (sub-model #4); and finally, describing aspects of the process that unfold over a year, using months as the unit for variables and effects (sub-model #5).
Specifying how factors and effects at different timescales are related
To facilitate this, we recommend using of a “fluid analogy” (Navarro-Barrientos, Rivera & Collins, 2010) to illustrate the accumulation of factors and effects over time from lower level (e.g., minutes) to higher level units (e.g., hours). Specifically, “tanks of fluid” can be used to describe factors that accumulate over time, with smaller tanks representing lower-level (faster) timescales and larger tanks representing higher level (slower) timescales. “Pipes” can be used to describe how factors and effects that occur at a lower level accumulate over time to form a higher level factor. For example, in Figure 3 we use these features to illustrate how repeated exposure to hassles at a minute level can accumulate over time to form a new factor, hourly hassles, which can accumulate over time to daily hassles and then to weekly and monthly stressors (where a stressor is defined as an “aspect of the environment that is demanding on an ongoing and relatively unchanging basis” Hahn & Smith, 1999; p.90). Notice that the meaning of this phenomenon changes as we move up the timescales, since an important aspect that distinguishes (chronic) stressors and hassles is the frequency with which they occur over longer periods of time (Pratt & Barling, 1988).
Additionally, attention should be given to specifying how factors and effects that occur at a higher level (e.g., a year) can affect factors/effects that occur later, at a lower level (e.g., a minute), either directly, or by facilitating change in relatively stable factors like personality traits, habits, values and chronic disorders. Returning to our illustrative model (Figure 3), in sub-model #5, distress accumulated over several months is expected to attenuate the trait coping capacity of the person. This is based on research suggesting that sustained or repetitive exposure to stressors (i.e., chronic stress) may “trigger maladaptive changes in some individuals, producing a vulnerable phenotype” that facilitates increased risk of illness (Blugeot et al., 2011, p. 12889). This illustrates how dynamics that accumulate over a long period of time (e.g., months) can facilitate momentary vulnerability (e.g., poor state coping capacity) by affecting more stable aspects of vulnerability (e.g., the more generalized coping capacity of the person).
(4) What are contender proximal outcomes?
The goal is to select factors that can capture intermediate progress towards the distal outcome. This is an important step because, as we discuss below, the proximal outcomes guide the definition of JIT in the context of the identified problem, as well as the formulation of the adaptation strategy. For study purposes, the proximal outcomes provide intermediate metrics of response or success in achieving progression from the current state (e.g., hazardous drinking) to the desired distal outcome (e.g., non-hazardous drinking patterns).
To select the proximal outcomes, investigators can build on the previously established dynamic model, beginning with the shortest timescale as a starting point for this iterative process. We suggest starting with the shortest timescale because targeting it might (a) facilitate early prevention of “snowballing effects,” whereby a single occurrence (e.g., lapse) or experience (e.g., negative mood) escalates into an adverse health outcome (e.g., total relapse; Sapienza & Masten, 2011), and/or (b) lead to improved scaffolding strategies that target short-term progress and goal attainment (Drews et al., 2007).
Returning to our example, one might begin selecting proximal outcomes by attending to minute level outcomes (e.g., minute-level distress), then possible outcomes at the hour level (e.g., hour-level coping capacity), then possible outcomes at the daily level (e.g., daily drinking) and so on. The goal is to select proximal outcomes that are expected to have the most meaningful impact on the distal outcome, and that can be influenced in a meaningful manner by providing support. A JITAI can target multiple proximal outcomes simultaneously.
Defining Just in Time in the Context of the Identified Problem
(5) What factors mark a state of vulnerability/opportunity?
The goal is to identify the conditions in which a person would be more vulnerable to experiencing adverse outcomes or more open to positive changes. Adverse outcomes and positive changes are defined by the candidate proximal outcomes. Identifying factors that mark (i.e., capture) a state of vulnerability/opportunity for a target proximal outcome can aid in the selection of decision points (as well as in the selection of tailoring variables, as we discuss below).
Returning to our example, consider minute-level distress as a candidate proximal outcome. The model in Figure 3 suggests that exposure to hassles at any given minute might lead to immediate reactivity in the form of distress. Hence, minute-level exposure to hassles marks a state of vulnerability to minute-level distress. For this proximal outcome, a state of vulnerability might occur at any minute and thus there might be a decision point every minute. Practically, this requires frequent assessments of hassles to reduce missed opportunities for support.
(6) What possible intervention options can affect the proximal outcomes?
The focus is on identifying intervention options that (a) can affect the candidate proximal outcomes; and (b) can be delivered JIT (i.e., precisely when the person is in a state of opportunity/vulnerability).
An important part of this process is to explore whether and which intervention options are feasible and effective given the timescale of each candidate proximal outcome. In our example, the lowest level proximal outcome is distress at the minute level but given the immediacy and automaticity of physiological reactivity to stress (Smeets et al., 2012; Sinha et al., 2003), it might not be feasible to intervene JIT. However, other forms of support (e.g., training sessions designed to help the person learn coping skills), might be suitable for improving this proximal outcome although such support is not offered precisely, and only upon exposure to hassles (see Lindquist & Cooper, 1999).
Turning to hour-level coping capacity as a candidate proximal outcome, empirical evidence suggests that brief recommendations that integrate elements of cognitive behavioral therapy (CBT) and/or acceptance and commitment therapy (ACT) can be delivered in a timely manner to help individuals regulate hourly or daily negative emotions (e.g., Witkiewitz et al., 2014; Norberg et al., 2013). The provision of such interventions has the potential to break the link between hour-level distress (which marks a state of vulnerability) and reduced coping capacity (the candidate proximal outcome). In the absence of empirically based intervention options, JITAI developers can either direct efforts towards building and evaluating new intervention options or attend to other candidate proximal outcomes (e.g., daily drinking).
Finally, given that in a JIT setting, support should be provided only when the person is (a) in a state of vulnerability/opportunity; and (b) receptive, it is important to include a “provide nothing” intervention option to minimize waste, intrusiveness, and burden (Nahum-Shani et al., 2014). In the current example, assume that two intervention options are considered: (1) recommendation to engage in emotion-regulation techniques building on principals of CBT and/or ACT (Yovel, Mor, & Shakarov, 2014); and (2) provide nothing.
(7) What factors mark a state of unreceptivity to the selected intervention options?
The goal is to identify the conditions in which a person is unlikely to (or should not, ethically) receive, process, or use the intervention options. As discussed above, this depends on the nature of the intervention options and the factors that influence the person’s ability/motivation to receive, process and use them. Some of these factors can be obvious, such as the example provided above where driving a car marks a state of unreceptivity for a recommendation in the form of a text-message. Other factors might be less obvious and require further investigation. For example, the number of recommendations the person received previously might lead to burden, and high negative affect might hinder the use of emotion-regulation techniques. Additional research is needed to better define states of unreceptivity to JIT interventions.
Formulating the Adaptation Strategy
(8) What are the tailoring variables?
The goal is to identify what information about the person can be useful in deciding what intervention option to offer. The tailoring variables should include factors that mark a state of vulnerability/opportunity and receptivity.
To illustrate this, consider that hourly distress marks a state of vulnerability for reduced hourly coping capacity (proximal outcome). This implies that information about hourly distress might be useful in identifying the conditions in which offering an emotion-regulation recommendation would lead to a better proximal outcome compared to offering nothing. Hence, information about hourly distress can be used to decide whether an emotion-regulation recommendation should be offered or not. Further, given that in our example driving a car marks a state of unreceptivity to this intervention option, information about driving can also be used to decide whether a recommendation should be offered or not. Hence, in this setting, hourly distress and driving a car might be selected as tailoring variables. Throughout, practical implications related to the feasibility of properly measuring the tailoring variables at the selected timescale should be taken into account (Kumar at el., 2013).
(9) For each possible level of the tailoring variable, which intervention option is likely to have the desired effect on the proximal outcome?
The goal is to think through the implications of delivering each intervention option at various levels of the tailoring variables. In our example, it is expected that individuals who experienced high distress in the past hour are likely to benefit from a recommendation compared to receiving nothing. However, there is insufficient empirical evidence to identify the cut-point of distress that differentiates when the recommendation might be beneficial versus unnecessary (i.e., providing a recommendation will lead to similar or worse proximal outcome compared to providing nothing). Further research is required to identify cut-points in various situations.
(10) What plausible decision rules can be generated to operationalize effective adaptation?
This final step involves the creation of appropriate decision rules that link all the information above in a systematic manner. The decision rule in Figure 1 builds on some of the ideas established above regarding our illustrative example.
Discussion
This manuscript provides a pragmatic framework for organizing existing evidence into a scientific model that can guide JITAI construction. This framework builds on the idea that existing evidence should be organized in a way that helps JITAI developers identify and devise a plan to address states of vulnerability/opportunity and receptivity to support.
Limitations and Further Research
As with most organizing perspectives, our pragmatic framework is subject to limitations. First, a key element in the proposed framework is using timescales to describe the progression of key factors towards the distal outcome. However, extant empirical evidence often does not provide insight into how key factors are ordered and related over time. This gap makes identifying timescales and describing the dynamics within each timescale rather challenging. Research attention should be given to implementing study designs and analytic methods that directly inform how and why distal outcomes unfold over time.
Studies that involve the collection of intensive longitudinal data can be highly useful in this setting (Bolger & Laurenceau, 2013). For example, study designs involving immediate reporting of experiences in the everyday life of individuals (e.g., EMAs) offer many opportunities for investigating dynamics within different timescales (Stone et al. 2007). Recent advances in mobile and wearable sensors provide many opportunities for frequent monitoring with reduced burden on the participant (Kumar et al., 2013).
A challenge relating to such study designs is the volume of information they produce. As noted by Kaplan and Stone (2013), “Most psychologists were trained to use statistical inference techniques designed for the study of agronomy in the 1930s. Although these methods have become much more sophisticated, inferential statistics can be meaningless for data sets composed of hundreds of millions of data points” (p. 492). Contemporary approaches involving data mining, machine learning, control systems engineering techniques, and other modern analytic methods are needed to allow JITAI developers to capitalize on intensive longitudinal data to identify factors that mark a state of vulnerability/opportunity and receptivity (for reviews of such data analytic approaches see Smith & Walls, 2015; Ye, Dobson & McKeever, 2012).
A second limitation concerns the precision of existing evidence. Even when a relationship between a candidate tailoring variable and a proximal outcome is well known (e.g., distress is highly predictive of poor coping capacity), existing evidence often asserts merely an association, lacking details about the cut-points (or levels) of the tailoring variable that differentiate between conditions in which one intervention option would lead to better proximal outcome compared to another. Intensive longitudinal research designs that allow direct comparison of various intervention options under different levels of candidate tailoring variables are needed. For example, to identify the levels of hourly distress at which a recommendation will be more beneficial than the alternative, an ideal study design would allow investigators to assess the causal effect of providing a recommendation compared to the alternative on the proximal outcome under different levels of hourly distress. In this context, Murphy and colleagues (Liao et al., 2015) offer the micro-randomized trial design – a form of a sequential factorial design that involves random assignment of intervention options at each (of numerous) decision point(s).
A third limitation concerns the limited behavioral research devoted to identifying markers of receptivity. Insights can likely be gleaned from the field of human-computer interaction, which focuses on ensuring systems are useful, usable, and enjoyable; but much more work is needed. Future studies should be designed to allow the simultaneous investigation of various factors that can potentially mark a state of receptivity (e.g., location, emotions, and presence of other people) to a given type of support. Investigators should consider collecting information following support provision such as whether support was received, attended to, used, or appreciated. Throughout, ethical considerations should be reviewed and addressed, in light of the intervention options under consideration and the population targeted.
Finally, a key assumption of the current framework is that existing evidence can be used to specify good (effective) decision rules a-priori. However, existing evidence is often insufficient to inform the formulation of good decision rules as it does not fully capture between-person and within-person variability in the conditions that mark a state of vulnerability/opportunity and receptivity. Such conditions might vary from one person to another and are likely to change over time within a person (e.g., as the person progresses through an intervention program). Given the limited models related to how states of vulnerability/opportunity and receptivity might vary between and within a person, new data analytic methods are needed to improve, in real-time, the decision rules specified a priori by JITAI developers. Specifically, methods are needed to analyze the ongoing information obtained from the person as s/he experiences the JITAI, and “train” the decision rules to accommodate changes in what constitutes a state of vulnerability/opportunity and receptivity for that particular person (see Dallery, Kurti & Erb, 2015; Kumar et al., 2013 for further discussion).
Conclusion
The pragmatic framework proposed in this manuscript builds the foundation for defining scientific models that inform the construction of JITAIs. While it offers ways to integrate and build on existing evidence to inform JITAI development, it also clearly highlights the scientific questions and methodological gaps that must be addressed in order to move the science of JITAIs forward.
Acknowledgments
This project was supported by the following awards: NIH U54 EB020404 01, NIH/NIDA R01 DA039901 01, NIH/NIDA P50 DA039838, NIH/NIAAA R01 AA023187 01 (Nahum-Shani); NIH/SEPA R25RR032159 (Spruijt-Metz); NSF IIS-1449751 (Hekler).
Footnotes
Hazardous (or “at-risk”) drinking is defined as drinking above the National Institute on Alcohol Abuse and Alcoholism low risk guidelines: ≤14 drinks per week and ≤4 drinks per occasion for men, and ≤7 drinks per week and ≤3 drinks per occasion for women.
Distress is defined as a discomforting mental state experienced in response to stress exposure (Kessler, 1979).
For example, chronic disorders like depression and substance use follow a waxing and waning course, involving periods of remission followed by symptom recurrence and exacerbation or relapse (and vice versa). Similarly, learning a new skill is not a linear process. “The learning brain naturally assimilates concepts in a spiraling, progressive manner” (Hamid, 2001: 315), and the pace of learning is parabolic in nature, with relatively slow early progress followed by more rapid learning (Case & Gunstone, 2002).
For clarity we specified a relatively simple dynamic model; however more complex models can be specified.
Additional details and justification for this hypothetical model can be obtained from the first author.
As very limited empirical evidence exists concerning the ordering of stressors, psychological distress, and drinking behaviors (Armeli, Todd, & Mohr, 2005), the factors and effects specified within each time scale rely heavily on existing theories and logic. Still, this exercise, by design, is meant to facilitate better understanding of existing gaps in the literature
Contributor Information
Inbal Nahum-Shani, Email: Inbal@umich.edu, Institute for Social Research, University of Michigan.
Eric B. Hekler, Email: ehekler@asu.edu, School of Nutrition and Health Promotion, Arizona State University
Donna Spruijt-Metz, Email: dmetz@usc.edu, Center for Economic and Social Research, University of Southern California.
References
- Armeli S, Todd M, Mohr C. A daily process approach to individual differences in stress-related alcohol use. Journal of Personality. 2005;73(6):1657–1686. doi: 10.1111/j.0022-3506.2005.00362.x. [DOI] [PubMed] [Google Scholar]
- Ben-Zeev D, Brenner CJ, Begale M, Duffecy J, Mohr DC, Mueser KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia Bulletin. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zeev D, Schueller SM, Begale M, Duffecy J, Kane JM, Mohr DC. Strategies for mHealth research: Lessons from 3 mobile intervention studies. Administration and Policy in Mental Health and Mental Health Services Research. 2014:1–11. doi: 10.1007/s10488-014-0556-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blugeot A, Rivat C, Bouvier E, Molet J, Mouchard A, Zeau B, Becker C. Vulnerability to depression: from brain neuroplasticity to identification of biomarkers. The Journal of Neuroscience. 2011;31(36):12889–12899. doi: 10.1523/JNEUROSCI.1309-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger N, Laurenceau JP. Intensive longitudinal methods: An introduction to diary and experience sampling research. New York, NY: Guilford Press; 2013. [Google Scholar]
- Bouton M. Learning and behavior: A contemporary synthesis. Sunderland, MA: Sinauer Associates; 2007. [Google Scholar]
- Burleson BR. Understanding the outcomes of supportive communication: A dual- process approach. Journal of Social and Personal Relationships. 2009;26(1):21–38. [Google Scholar]
- Buxton B. Sketching user experiences: Getting the design right and the right design. San Francisco, CA: Morgan Kaufmann; 2010. [Google Scholar]
- Canel C, Rosen D, Anderson EA. Just-in-time is not just for manufacturing: A service perspective. Industrial Management & Data Systems. 2000;100(2):51–60. [Google Scholar]
- Case J, Gunstone R. Metacognitive development as a shift in approach to learning: an in-depth study. Studies in Higher Education. 2002;27(4):459–470. [Google Scholar]
- Castelo N, Reiner PB, Felsen G. Balancing autonomy and decisional enhancement: An evidence-based approach. The American Journal of Bioethics. 2012;12(2):30–31. doi: 10.1080/15265161.2011.634951. [DOI] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Bierman KL. A conceptual framework for adaptive preventive interventions. Prevention Science. 2004;5(3):185–196. doi: 10.1023/b:prev.0000037641.26017.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolvo S, McDonald DW, Landay JA. Theory-driven design strategies for technologies that support behavior change in everyday life. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; ACM; 2009. Apr, pp. 405–414. [Google Scholar]
- Csikszentmihalyi M, Rathunde K. The measurement of flow in everyday life: Toward a theory of emergent motivation. In: Jacobs JE, editor. Developmental perspectives on motivation. Vol. 40. Lincoln, NE: University of Nebraska; 1993. pp. 57–97. [PubMed] [Google Scholar]
- Dantzig S, Geleijnse G, Halteren AT. Toward a persuasive mobile application to reduce sedentary behavior. Personal and Ubiquitous Computing. 2013;17(6):1237–1246. [Google Scholar]
- Dallery J, Kurti A, Erb P. A New Frontier: Integrating Behavioral and Digital Technology to Promote Health Behavior. The Behavior Analyst. 2015;38:19–49. doi: 10.1007/s40614-014-0017-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Costa A, Shet A, Kumarasamy N, Ashorn P, Eriksson B, Bogg L, Diwan VK. Design of a randomized trial to evaluate the influence of mobile phone reminders on adherence to first line antiretroviral treatment in South India-the HIVIND study protocol. BMC Medical Research Methodology. 2010;10(1):25. doi: 10.1186/1471-2288-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drews FA, Picciano P, Agutter J, Syroid N, Westenskow DR, Strayer DL. Development and evaluation of a just-in-time support system. Human Factors: The Journal of the Human Factors and Ergonomics Society. 2007;49(3):543–551. doi: 10.1518/001872007X200166. [DOI] [PubMed] [Google Scholar]
- Evans JSB. Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology. 2008;59:255–278. doi: 10.1146/annurev.psych.59.103006.093629. [DOI] [PubMed] [Google Scholar]
- Fenton M, Leggio L, Kenna GA, Swift RM. HIV testing in hazardous drinking: a survey analysis. Substance Use & Misuse. 2010;45(1–2):204–212. doi: 10.3109/10826080902882839. [DOI] [PubMed] [Google Scholar]
- Ferster CB, Skinner BF. Schedules of reinforcement. East Norwalk, CT: Appleton-Century-Crofts; 1957. [Google Scholar]
- Fisher WW, Piazza CC, Roane HS. Handbook of applied behavior analysis. New York, NY: Guilford Press; 2011. [Google Scholar]
- Fogg B, editor. A behavior model for persuasive design. Proceedings of the 4th international Conference on Persuasive Technology; New York, NY: ACM; 2009. [Google Scholar]
- Friesen MR, Hamel C, McLeod RD. A mHealth application for chronic wound care: Findings of a user trial. International Journal of Environmental Research and Public Health. 2013;10(11):6199–6214. doi: 10.3390/ijerph10116199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG, Shah D. A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA psychiatry. 2014;71(5):566–572. doi: 10.1001/jamapsychiatry.2013.4642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SE, Smith CS. Daily hassles and chronic stressors: Conceptual and measurement issues. Stress and Health. 1999;15(2):89–101. [Google Scholar]
- Hamid AA. e-Learning: Is it the “e” or the learning that matters? The Internet and Higher Education. 2001;4(3):311–316. [Google Scholar]
- Hekler E, Klasnja P, Traver V, Hendriks M. Realizing effective behavioral management of health: The metamorphosis of behavioral science methods. Pulse, IEEE. 2013;4(5):29–34. doi: 10.1109/MPUL.2013.2271681. [DOI] [PubMed] [Google Scholar]
- Ho J, Intille SS. Using context-aware computing to reduce the perceived burden of interruptions from mobile devices. Paper presented at the Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; Portland, Oregon, USA. 2005. [Google Scholar]
- Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. American Psychologist. 1989;44(3):513. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- Jimison H, Gorman P, Woods S, Nygren P, Walker M, Norris S, Hersh W. Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PMC free article] [PubMed] [Google Scholar]
- Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: Daily hassles and uplifts versus major life events. Journal of Behavioral Medicine. 1981;4(1):1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- Kaplan RM, Stone AA. Bringing the laboratory and clinic to the community: mobile technologies for health promotion and disease prevention. Annual Review of Psychology. 2013;64:471–498. doi: 10.1146/annurev-psych-113011-143736. [DOI] [PubMed] [Google Scholar]
- Karolak DW, Karolak N. Software engineering risk management: A just-in-time approach. Los Alamitos, CA: IEEE Computer Society Press; 1995. [Google Scholar]
- Kessler RC. Stress, social status, and psychological distress. Journal of Health and Social behavior. 1979:259–272. [PubMed] [Google Scholar]
- Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: Stress, social support, and coping processes. Annual Review of Psychology. 1985;36(1):531–572. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- Kjeldskov J, Skov MB, Als BS, Høegh RT. Mobile Human-Computer Interaction-Mobile HCI 2004. Berlin: Springer Heidelberg; 2004. Is it worth the hassle? Exploring the added value of evaluating the usability of context-aware mobile systems in the field; pp. 61–73. [Google Scholar]
- Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, Spruijt-Metz D. Mobile health technology evaluation: The mhealth evidence workshop. American Journal of Preventive Medicine. 2013;45(2):228–236. doi: 10.1016/j.amepre.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS. Coping theory and research: past, present, and future. Psychosomatic Medicine. 1993;55(3):234–247. doi: 10.1097/00006842-199305000-00002. [DOI] [PubMed] [Google Scholar]
- Liao P, Klasnja P, Tewari A, Murphy SA. University of Michigan Technical Report 537. Ann Arbor, MI: University of Michigan; 2015. Micro--Randomized trials in mHealth. [Google Scholar]
- Lindquist TL, Cooper CL. Using lifestyle and coping to reduce job stress and improve health in ‘at risk’ office workers. Stress and Health. 1999;15(3):143–152. [Google Scholar]
- McGowan J, Hogg W, Campbell C, Rowan M. Just-in-time information improved decision-making in primary care: A randomized controlled trial. PloS one. 2008;3(11):e3785. doi: 10.1371/journal.pone.0003785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh BS, Seaton RAF, Jeffrey P. Tools to think with? Towards understanding the use of computer-based support tools in policy relevant research. Environmental Modelling & Software. 2007;22(5):640–648. [Google Scholar]
- Mohr CD, Armeli S, Tennen H, Carney MA, Affleck G, Hromi A. Daily interpersonal experiences, context, and alcohol consumption: crying in your beer and toasting good times. Journal of Personality and Social Psychology. 2001;80(3):489. doi: 10.1037/0022-3514.80.3.489. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Schueller SM, Montague E, Burns MN, Rashidi P. The behavioral intervention technology model: an integrated conceptual and technological framework for eHealth and mHealth interventions. Journal of Medical Internet Research. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris M, Intille SS, Beaudin JS. Embedded Assessment: overcoming barriers to early detection with pervasive computing. In: Gellersen HW, Want R, Schmidt A, editors. Proceedings of PERVASIVE 2005. Berlin Heidelberg: Springer-Verlag; 2005. pp. 333–346. [Google Scholar]
- Murimi MW, Chrisman MS, Hughes K, Taylor C, Kim Y, McAllister TL. Effects of school-based point-of-testing counselling on health status variables among rural adolescents. Health Education Journal. 2014 0017896914552000. [Google Scholar]
- Nahum-Shani I, Smith S, Tewari A, Witkiewitz K, Collins LM, Spring B, Murphy S. Just-in- time adaptive interventions (JITAIs): An organizing framework for ongoing health behavior support. University Park, PA: The Methodology Center, Penn State; 2014. Methodology Center technical report No. 14-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naughton F, Jamison J, Sutton S. Attitudes towards SMS text message smoking cessation support: A qualitative study of pregnant smokers. Health Education Research. 2013:cyt057. doi: 10.1093/her/cyt057. [DOI] [PubMed] [Google Scholar]
- Navarro-Barrientos JE, Rivera DE, Collins LM. Advances in Social Computing. Berlin Heidelberg: Springer; 2010. A dynamical systems model for understanding behavioral interventions for weight loss; pp. 170–179. [Google Scholar]
- Norberg MM, Rooke SE, Albertella L, Copeland J, Kavanagh DJ, Lau AY. The first mHealth app for managing cannabis use: Gauging its potential helpfulness. Journal of Addictive Behaviors Therapy & Rehabilitation. 2013 doi: 10.4172/2324-9005.1000117. Advance online publication. [DOI] [Google Scholar]
- Patrick K, Raab F, Adams MA, Dillon L, Zabinski M, Rock CL, Norman GJ. A text message–based intervention for weight loss: Randomized controlled trial. Journal of Medical Internet Research. 2009;11(1):e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plarre K, Raij A, Hossain SM, Ali AA, Nakajima M, Al’absi M, Wittmers LE. Continuous inference of psychological stress from sensory measurements collected in the natural environment. Proceedings From the 10th International Conference on Information Processing in Sensor Networks (IPSN); Chicago, IL: IEEE; 2011. pp. 97–108. [Google Scholar]
- Polonsky WH, Fisher L, Hessler D, Edelman SV. What is so tough about self-monitoring of blood glucose? Perceived obstacles among patients with Type 2 diabetes. Diabetic Medicine. 2014;31(1):40–46. doi: 10.1111/dme.12275. [DOI] [PubMed] [Google Scholar]
- Pratt LI, Barling J. Differentiating between daily events, acute and chronic stressors: A framework and its implications. In: Hurel JJ, Murphy LR, Sauter SL, Cooper CL, editors. Occupational stress: Issues and development in research. London: Taylor and Francis; 1988. pp. 41–51. [Google Scholar]
- Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: A mechanism to deliver more accessible, more effective mental health care. Clinical Psychology & Psychotherapy. 2014;21(5):427–436. doi: 10.1002/cpp.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley WT. Theoretical Models to Inform Technology-Based Health Behavior Interventions. In: Marsch LA, Lord SE, Dallery J, editors. Behavioral Health Care and Technology: Using Science-Based Innovations to Transform Practice. New York, NY: Oxford; 2014. pp. 13–26. [Google Scholar]
- Riley WT, Obermayer J, Jean-Mary J. Internet and mobile phone text messaging intervention for college smokers. Journal of American College Health. 2008;57(2):245–248. doi: 10.3200/JACH.57.2.245-248. [DOI] [PubMed] [Google Scholar]
- Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Translational Behavioral Medicine. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roesch SC, Aldridge AA, Stocking SN, Villodas F, Leung Q, Bartley CE, Black LJ. Multilevel factor analysis and structural equation modeling of daily diary coping data: Modeling trait and state variation. Multivariate Behavioral Research. 2010;45(5):767–789. doi: 10.1080/00273171.2010.519276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapienza JK, Masten AS. Understanding and promoting resilience in children and youth. Current Opinion in Psychiatry. 2011;24(4):267–273. doi: 10.1097/YCO.0b013e32834776a8. [DOI] [PubMed] [Google Scholar]
- Sarker H, Sharmin M, Ali AA, Rahman MM, Bari R, Hossain SM, Kumar S. Assessing the availability of users to engage in just-in-time intervention in the natural environment. Proceedings of the 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing; New York, NY: ACM; 2014. Sep, pp. 909–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology. 2003;170(1):62–72. doi: 10.1007/s00213-003-1525-8. [DOI] [PubMed] [Google Scholar]
- Smeets T, Cornelisse S, Quaedflieg CW, Meyer T, Jelicic M, Merckelbach H. Introducing the Maastricht acute stress test (MAST): A quick and non-invasive approach to elicit robust autonomic and glucocorticoid stress responses. Psychoneuroendocrinology. 2012;37(12):1998–2008. doi: 10.1016/j.psyneuen.2012.04.012. [DOI] [PubMed] [Google Scholar]
- Smith DM, Walls TA. mHealth Analytics. In: Marsch LA, Lord SE, Dallery J, editors. Behavioral Health Care and Technology: Using Science-Based Innovations to Transform Practice. New York, NY: Oxford; 2014. pp. 153–167. [Google Scholar]
- Spruijt-Metz D, Hekler E, Saranummi N, Intille S, Korhonen I, Nilsen W, Pavel M. Building new computational models to support health behavior change and maintenance: new opportunities in behavioral research. Translational Behavioral Medicine. 2015;5(2):1–12. doi: 10.1007/s13142-015-0324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruijt-Metz D, Nilsen W. Dynamic models of behavior for just-in-time adaptive interventions. Pervasive Computing, IEEE. 2014;13(3):13–17. [Google Scholar]
- Stone AA, Shiffman S, Atienza A, Nebling L, editors. The science of real-time data capture: Self-reports in health research. New York, NY: Oxford; 2007. [Google Scholar]
- Van Merriënboer JJ, Kirschner PA, Kester L. Taking the load off a learner’s mind: Instructional design for complex learning. Educational Psychologist. 2003;38(1):5–13. [Google Scholar]
- Walters ST, Vader AM, Harris TR, Jouriles EN. Reactivity to alcohol assessment measures: an experimental test. Addiction. 2009;104(8):1305–1310. doi: 10.1111/j.1360-0443.2009.02632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was zen, this is tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Desai SA, Bowen S, Leigh BC, Kirouac M, Larimer ME. Development and evaluation of a mobile intervention for heavy drinking and smoking among college students. Psychology of Addictive Behaviors. 2014;28(3):639–650. doi: 10.1037/a0034747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye J, Dobson S, McKeever S. Situation identification techniques in pervasive computing: A review. Pervasive and Mobile Computing. 2012;8(1):36–66. [Google Scholar]
- Yovel I, Mor N, Shakarov H. Examination of the core cognitive components of cognitive behavioral therapy and acceptance and commitment therapy: An analogue investigation. Behavior Therapy. 2014;45:482–494. doi: 10.1016/j.beth.2014.02.007. [DOI] [PubMed] [Google Scholar]
- Zaheer S, Albert S, Zaheer A. Time scales and organizational theory. Academy of Management Review. 1999;24(4):725–741. [Google Scholar]
- Zubin J, Spring B. Vulnerability: A new view of schizophrenia. Journal of Abnormal Psychology. 1977;86(2):103. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- Zulkernain S, Madiraju P, Ahamed SI. Mobile Wireless Middleware, Operating Systems, and Applications. Vol. 48. Springer; Berlin Heidelberg: 2010. A Context Aware Interruption Management System for Mobile Devices; pp. 221–234. [Google Scholar]