Abstract
Context
National Collegiate Athletic Association (NCAA) legislation requires that member institutions have policies to guide the recognition and management of sport-related concussions. Identifying the nature of these policies and the mechanisms of their implementation can help identify areas of needed improvement.
Objective
To estimate the characteristics and prevalence of concussion-related protocols and preparticipation assessments used for incoming NCAA student-athletes.
Design
Cross-sectional study.
Setting
Web-based survey.
Patients or Other Participants
Head athletic trainers from all 1113 NCAA member institutions were contacted; 327 (29.4%) completed the survey.
Intervention(s)
Participants received an e-mail link to the Web-based survey. Weekly reminders were sent during the 4-week window.
Main Outcome Measure(s)
Respondents described concussion-related protocols and preparticipation assessments (eg, concussion history, neurocognitive testing, balance testing, symptom checklists). Descriptive statistics were compared by division and football program status.
Results
Most universities provided concussion education to student-athletes (95.4%), had return-to-play policies (96.6%), and obtained the number of previous concussions sustained by incoming student-athletes (97.9%). Fewer had return-to-learn policies (63.3%). Other concussion-history–related information (eg, symptoms, hospitalization) was more often collected by Division I universities. Common preparticipation neurocognitive and balance tests were the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT; 77.1%) and Balance Error Scoring System (46.5%). In total, 43.7% complied with recommendations for preparticipation assessments that included concussion history, neurocognitive testing, balance testing, and symptom checklists. This was due to moderate use of balance testing (56.6%); larger proportions used concussion history (99.7%), neurocognitive testing (83.2%), and symptom checklists (91.7%). More Division I universities (55.2%) complied with baseline assessment recommendations than Division II (38.2%, χ2 = 5.49, P = .02) and Division III (36.1%, χ2 = 9.11, P = .002) universities.
Conclusions
National Collegiate Athletic Association member institutions implement numerous strategies to monitor student-athletes. Division II and III universities may need additional assistance to collect in-depth concussion histories and conduct balance testing. Universities should continue developing or adapting (or both) return-to-learn policies.
Key Words: traumatic brain injuries, return-to-play guidelines, evaluation
Key Points
Approximately 4 in 10 universities complied with recommendations for preparticipation assessments that included concussion history, neurocognitive testing, balance testing, and symptom checklists; this low proportion was partially attributable to 43.4% not using balance testing.
Division I universities complied with baseline assessment recommendations more than Division II and III universities did.
Approximately 1 in 3 universities (36.7%) lacked return-to-learn policies.
Knowledge of concussions and concussion symptomatology has dramatically increased as researchers have explored the acute and prolonged effects of concussions among collegiate student-athletes. In 2010, the National Collegiate Athletic Association (NCAA) passed legislation in all 3 divisions requiring its member institutions to develop and maintain policies to guide the identification and management of student-athletes with sport-related concussion. Furthermore, the same legislation requires that concussion policies (1) provide concussion-related education for all student-athletes and coaches, (2) ensure that a student-athlete identified with a concussion is removed from play and is evaluated by a medical professional with education and training in concussion, (3) guarantee that a student-athlete with a concussion will not return to practice or competition the same day as the concussion, and (4) stipulate that clearance to return to practice or competition is provided by a medical doctor or his or her designee. Within this broad framework, member institutions have the flexibility to implement specific policies and procedures to satisfy the requirements of the legislation.1
Although literature2,3 exists regarding conformity with recommendations related to diagnosing sport-related concussion, currently minimal literature is specifically related to the implementation of concussion-related protocols and preparticipation assessments, particularly for incoming NCAA student-athletes. For example, some schools may struggle to implement baseline assessments because of insufficient staff or financial resources or both. To our knowledge, only 1 group4 has examined concussion-management plans at the collegiate level, and they did not examine return-to-learning components. Another group5 examined preparticipation assessments in the NCAA but only among Division I athletic trainers (ATs). It is imperative that the use of concussion-related protocols and preparticipation assessments be explored at all levels of NCAA athletic participation before appropriate mandates can be implemented for all member institutions. In addition, because concussion rates are highest in football,6,7 universities with football programs may differ in their implementation of concussion-related protocols and preparticipation assessments.
The purpose of our study was to examine the prevalence of concussion-related protocols used in the 1113 member institutions of the NCAA as of the 2013–2014 academic year. Our specific aims were to
-
1.
Estimate the prevalence of concussion-related protocols in member institutions;
-
2.
Determine what concussion-history information is collected from incoming student-athletes, including number of previous concussions and resulting hospitalization, symptoms, and recovery times;
-
3.
Examine concussion-assessment batteries, including which specific tests are performed and which student-athletes are tested;
-
4.
Evaluate conformity with recommendations for concussion preparticipation assessments (ie, use of concussion history and a concussion-assessment battery); and
-
5.
Determine differences in concussion-related protocols and preparticipation assessments by division or whether the member institution has a football program.
In addition, we were also interested in exploring other relevant clinical tests (eg, vision, mental health) that might be conducted along with the concussion-assessment batteries.
METHODS
Study Design and Recruitment
We used a cross-sectional design. Head ATs from all 1113 NCAA member institutions (from here on referred to as universities) were contacted. These head ATs were invited to complete an online self-administered survey hosted on SurveyMonkey (Palo Alto, CA). Respondents received a weekly reminder during the 4-week data-collection window.
The Research Review Board of the NCAA approved all aspects of this study, deeming it exempt from human subjects protections approval because it informed researchers about institutional practices, as opposed to individual behaviors. We reminded respondents that all answers would remain anonymous, not be attached to the member institution where they were employed, and be presented in aggregate form.
Survey Instrument
University Information
Respondents provided information pertaining to their university as of the 2013–2014 academic year. Items included NCAA division (ie, Division I, III, or III), number of sports covered by medical staff, number of student-athletes, and whether their university had a football program.
Concussion-Related Protocols
We inquired about whether their universities enacted policies related to sport-related concussions, including concussion education for student-athletes and coaches, return-to-play protocols, and return-to-learn protocols.
Preparticipation Assessments
Respondents provided information on preparticipation assessments used with incoming student-athletes. Concussion history examined the number of previous concussions; associated hospitalization, symptoms, and recovery time; and whether previous concussions were related or not related to sport.
We also inquired about which components (eg, neurocognitive tests, balance tests, symptom checklist) were included in their school's concussion-assessment battery. For neurocognitive and balance tests, we included a list of widely used tools, such as Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT)8 and the Balance Error Scoring System (BESS),9 from which respondents selected all tools that were used in the 2013–2014 academic year. An “other” category with fill-in responses was also available. Although various symptom checklists exist, we opted to ask only if respondents' universities used a symptom checklist for incoming student-athletes. Last, we also inquired about neurostatus tests (eg, Standardized Assessment of Concussion [SAC]10 and Sport Concussion Assessment Tool 3 [SCAT3]11), vision tests (eg, Snellen chart, King-Devick test), and other tests or assessments (eg, anxiety/depression, sleep, quality of life). An “other” category with fill-in responses was also available for these tests.
Statistical Analyses
We computed the proportion of universities at which ATs used each concussion-related protocol and preparticipation assessment. We then calculated the proportion of universities that complied with NCAA recommendations to have student-athletes undergo a preparticipation assessment that included concussion history, neurocognitive testing, balance testing, and symptom checklist.12
Tests of homogeneity examined whether responding universities were homogeneous in the proportions of concussion-related protocols or preparticipation assessments used as described earlier. The independent variables that distinguished these variables were division and presence of a football program. Resulting χ2 test statistics, or Fisher exact test statistics when assumptions for χ2 tests were not satisfied, that yielded a P value <.05 were considered statistically significant. For all analyses, we were concerned with the percentages of universities subscribing to each concussion-assessment strategy. As a result, respondents who noted that they did not use a concussion-related protocol or did not respond to the survey item were treated as not subscribing to the protocol. Findings did not differ when compared with excluded missing data. We analyzed data using SAS Enterprise Guide software (version 4.3; SAS Inc, Cary, NC).
RESULTS
University Information
We received responses from head ATs at 327 universities (29.4% response rate). Respondents originated from all 3 divisions, the majority of which had a football team in the 2013–2014 academic year (64.7%; Table 1). Respondents reported an average of 17.7 (SD = 5.0) sports covered by medical staff and 411.8 student-athletes (SD = 173.1) present at their universities. Compared with the entire NCAA membership, we had a larger proportion of Division I universities in our sample (38.7% versus 31.1%; χ2 = 6.58; P = .01). However, the proportion of respondents with football programs (64.7%) was not different from that of the NCAA membership (59.7%; χ2 = 2.68; P = .10).
Table 1. .
Characteristics of Responding National Collegiate Athletic Association Member Institutions, 2013–2014 Academic Year (N = 327)a
| Category |
No. (%) |
| Division (n = 323) | |
| I | 125 (38.7) |
| II | 76 (23.5) |
| III | 122 (37.8) |
| Football program? (n = 323) | |
| Yes | 209 (64.7) |
| No | 114 (35.3) |
| No. of sports covered by medical staff (n = 327) | |
| 10 or fewer | 19 (5.8) |
| 11–15 | 86 (26.3) |
| 16–20 | 138 (42.2) |
| 21–25 | 62 (19.0) |
| 26 or more | 22 (6.7) |
| No. of student-athletes (n = 326) | |
| 200 or fewer | 35 (10.7) |
| 201–300 | 56 (17.2) |
| 301–400 | 91 (27.9) |
| 401–500 | 67 (20.6) |
| 501–600 | 55 (16.9) |
| 601 or more | 22 (6.7) |
Of the 327 respondents, data were missing for division (n = 4), football program (n = 4), and number of student-athletes (n = 1).
Concussion-Related Protocols
Most universities had protocols for concussion management, including return to play (96.6%; Table 2). However, return-to-learn policies were less prevalent (63.3%). In fact, only 3.1% of responding universities involved academic support in the management of concussed athletes. No differences related to return-to-play and return-to-learn policies existed by division or whether universities had a football team.
Table 2. .
Concussion-Related Protocols Provided by National Collegiate Athletic Association Member Institutions (N = 327) by Division and Whether University Had Football Team, No. (%)
| Category |
Total |
Division |
Football Team? |
|||
| I |
II |
III |
Yes |
No |
||
| Concussion education | ||||||
| Provided to student-athletesa | 312 (95.4) | 115 (92.0)b | 73 (96.1) | 120 (98.4) | 200 (95.7) | 108 (94.7) |
| Provided to coachesa | 295 (90.2) | 107 (85.6)b | 71 (93.4) | 114 (93.4) | 187 (89.5) | 104 (91.2) |
| Return-to-play protocola | 316 (96.6) | 120 (96.0) | 73 (96.1) | 119 (97.5) | 202 (96.7) | 110 (96.5) |
| Return-to-learn protocola | 207 (63.3) | 84 (67.2) | 46 (60.5) | 76 (62.3) | 136 (65.1) | 68 (59.6) |
Sums of divisions and presence of football teams do not equal total because of missing data.
Indicates lower percentage than Division III (P < .05).
Most universities provided concussion education to student-athletes (95.4%) and coaches (90.2%; Table 2). A smaller proportion of universities from Division I provided concussion education than those from Division II and III. However, differences were significant only between Division I and Division III (student-athlete education, 98.4% versus 92.0%, χ2 = 5.40, P = .02; coach education, 93.4% versus 85.6%, χ2 = 6.58, P = .04). The presence of football made no difference to the existence of concussion education.
Preparticipation Assessments
Among those universities currently using preparticipation assessments, student-athletes from an average of 12.0 sports (SD = 5.2) were assessed. This included an average of 6.5 women's sports (SD = 2.9) and 5.5 men's sports (SD = 2.7). Sponsorship of individual sports varied among responding universities. The largest sponsorship was in women's basketball (n = 305), women's soccer (n = 293), and men's basketball (n = 292); the smallest sponsorship was in men's rifle (n = 0), women's bowling (n = 3), and women's fencing (n = 3).
Concussion History
A large majority of respondents noted that their universities collected some form of concussion history from their incoming student-athletes (99.7%), with the most common information being the number of concussions previously sustained (97.9%; Table 3). No differences existed by division or for having a football program in regard to documenting the number of concussions previously sustained by incoming student-athletes. However, additional information regarding concussion history aside from the number of concussions previously sustained (eg, resulting hospitalization, symptoms, and recovery time related to previous concussions) was more often collected among Division I universities and universities with a football program (Table 3).
Table 3. .
Concussion-History Information Obtained From Incoming Student-Athletes and Provided by National Collegiate Athletic Association Member Institutions (N = 327) by Division and Whether University Had Football Team, No. (%)
| Division |
Football Team? |
|||||
| Category |
Total |
I |
II |
III |
Yes |
No |
| No. of previous concussionsa | 320 (97.9) | 124 (99.2) | 74 (97.4) | 118 (96.7) | 206 (98.6) | 110 (96.5) |
| Whether hospitalization was needed for previous concussiona | 233 (71.3) | 100 (80.0)b | 51 (67.1) | 81 (66.4) | 156 (74.6)c | 73 (64.0) |
| Symptoms related to previous concussiona | 189 (57.8) | 87 (69.6)b | 38 (50.0) | 62 (50.8) | 133 (63.6)c | 52 (45.6) |
| Whether concussions were sport relateda | 168 (51.4) | 79 (63.2)b | 34 (44.7) | 54 (44.3) | 116 (55.5)c | 50 (43.9) |
| Concussion recovery timea | 151 (46.2) | 75 (60.0)b | 24 (31.6) | 50 (41.0) | 108 (51.7)c | 42 (36.8) |
Sums of divisions and presence of football teams do not equal total because of missing data.
Indicates greater percentage than Divisions II and III (P < .05).
Indicates greater percentage than universities without a football program (P < .05).
Concussion-Assessment Batteries
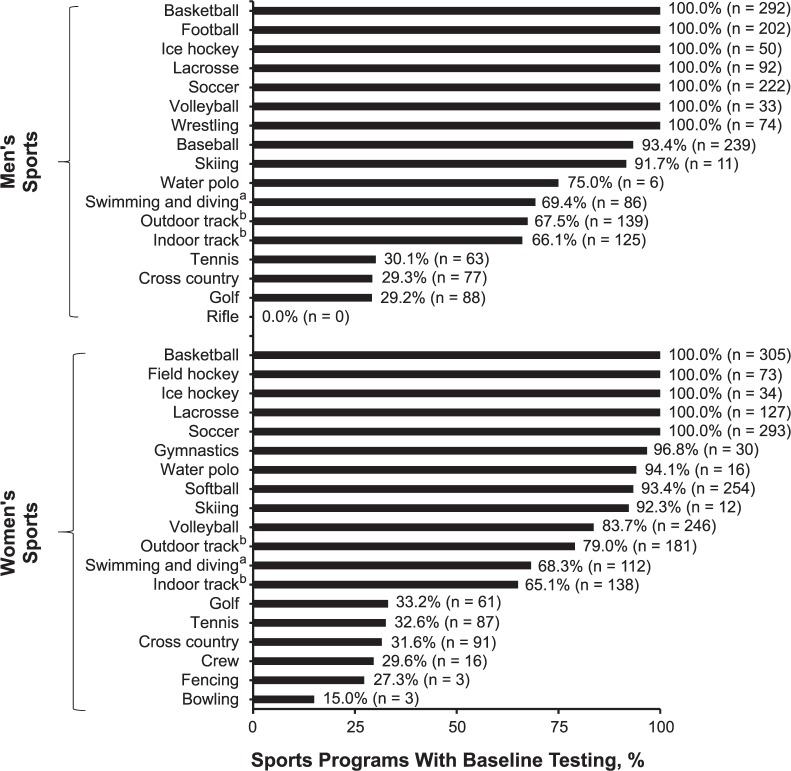
Most responding universities, across all 3 divisions, implemented some form of concussion-assessment battery in the 2013–2014 academic year (96.0%). However, of the 13 without preparticipation assessments, 6 planned to introduce them in the 2014–2015 academic year. Use of preparticipation assessments varied within these individual sports (Figure). For example, all responding universities with men's basketball conducted preparticipation assessments for those student-athletes. Other sports with 100% use of preparticipation assessments were men's football, ice hockey, lacrosse, soccer, volleyball, and wrestling and women's basketball, field hockey, ice hockey, lacrosse, and soccer (Figure). On the other hand, many noncontact sports had low proportions of sponsoring universities that conducted preparticipation assessments for those student-athletes. These sports included golf (29.2%) and cross-country (29.3%) and women's bowling (15.0%), fencing (27.3%), and crew (29.6%).
Figure. .
Sports at National Collegiate Athletic Association member institutions (n = 327) whose student-athletes underwent a preparticipation assessment. Percentages are for the number of sports programs with preparticipation assessments out of the number of sports programs existing among the responding universities. For example, 17 responding universities had women's water polo programs, of which 16 (94.1%) conducted preparticipation assessments. Percentages exclude schools that did not provide sports-program–related information. aIncludes sports programs in which only divers have preparticipation assessments. b Includes sports programs in which only pole vaulters or high jumpers have preparticipation assessments.
Most responding universities implemented some form of concussion-assessment battery in the 2013–2014 academic year (96.0%). The most used neurocognitive test at baseline was ImPACT (77.1%) and the most used balance test was the BESS (46.5%; Table 4). A larger proportion of Division I universities (71.2%) implemented baseline balance testing than universities from Divisions II (46.1%, χ2 = 12.65, P < .001) and III (51.6%, χ2 = 9.98, P = .002). In addition, other assessments were used, such as neurostatus and vision tests. A larger proportion of Division I universities (61.6%) implemented baseline vision testing compared with universities from Divisions II (34.2%, χ2 = 14.19, P < .001) and III (23.0%, χ2 = 37.74, P < .001).
Table 4. .
Preparticipation Assessments Performed by National Collegiate Athletic Association Member Institutions (N = 327)
| Test |
No. (%) |
| Compliance with National Collegiate Athletic Association guidelines for having concussion history, symptom checklist, neurocognitive testing, and balance testing | 141 (43.1) |
| Concussion history | 326 (99.7) |
| Symptom checklist | 300 (91.7) |
| Neurocognitive tests | 272 (83.2) |
| Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT, ImPACT Applications, Inc, Pittsburgh, PA) | 252 (77.1) |
| Headminder Concussion Resolution Index (no longer available) | 8 (2.4) |
| CCAT Axon Sports Computerized Cognitive Assessment Tool (formerly called CogSport; CogState, Wausau, WI) | 7 (2.1) |
| CNS Vital Signs (CNS Vital Signs, LLC, Morrisville, NC) | 7 (2.1) |
| Paper-pencil tests (eg, Symbol Digit Modalities Test, Delis-Kaplan Executive Function System [Pearson Education, Inc, San Antonio, TX], Trail Making Test) | 5 (1.5) |
| Automated Neuropsychological Assessment Metrics (Vista LifeSciences, Parker, CO) | 0 (0.0) |
| Other | 7 (2.1) |
| Balance tests | 185 (56.6) |
| Balance Error Scoring System | 156 (47.7) |
| Romberg Test | 22 (6.7) |
| Sensory Organization Test | 14 (4.3) |
| Force plate/platform | 10 (3.1) |
| Sway Balance (Sway Medical LLC, Tulsa, OK) | 4 (1.2) |
| Nintendo Wii Balance Board (Nintendo of America Inc, Redmond, WA) | 3 (0.9) |
| Other | 18 (5.5) |
| Neurostatus tests | 118 (36.1) |
| Standardized Assessment of Concussion (SAC) | 57 (17.4) |
| Sport Concussion Assessment Tool 2 (SCAT2) | 51 (15.6) |
| Sport Concussion Assessment Tool 3 (SCAT3) | 39 (11.9) |
| Sideline ImPACT | 7 (2.1) |
| Visual tests | 131 (40.1) |
| Standard eye exam (Snellen chart) | 116 (35.5) |
| King-Devick Test (Mayo Foundation for Medical Education and Research, Oakbrook Terrace, IL) | 15 (4.6) |
| Other | 6 (1.8) |
| Other tests/assessments | |
| Headache/migraine history | 128 (39.1) |
| Anxiety/depression | 113 (34.6) |
| Sleep | 102 (31.2) |
| General mood | 94 (28.7) |
| Behavioral | 79 (24.2) |
| Quality of life | 56 (17.1) |
| Neck strength | 15 (4.6) |
| Evoked potentials | 4 (1.2) |
| Smell testing | 4 (1.2) |
| Taste testing | 4 (1.2) |
| Other | 20 (6.1) |
Compliance With NCAA Guidelines
Among all responding universities, 43.7% followed recommendations that preparticipation assessments include concussion history, neurocognitive testing, balance testing, and a symptom checklist (Table 4).12 However, 99.7%, 95.7%, and 93.0% used at least 1, 2, or 3, respectively, of the recommended components. The difference between using at least 2 and all 3 of the components was due to moderate use of balance testing (57.5%), whereas almost all used some form of concussion history (99.7%), neurocognitive testing (83.2%), and symptom checklist (91.7%). A larger proportion of Division I universities (55.2%) complied with baseline assessment recommendations compared with universities from Divisions II (38.2%, χ2 = 5.49, P = .02) and III (36.1%, χ2 = 9.11, P = .002). Also, a larger proportion of universities with a football program (47.9%) complied with recommendations than did universities without a football program (36.0%, χ2 = 4.23, P = .04).
DISCUSSION
Determining the current concussion-management practices of NCAA member institutions can provide its members, staff, researchers, and clinicians with a better understanding of the level of care being delivered to patients with concussions. This study is the first, to our knowledge, to examine concussion-related protocols and preparticipation assessment practices in the collegiate setting across all divisions. Our findings suggest that at the collegiate level, almost all responding universities implemented some form of preparticipation assessment and tested student-athletes from numerous sports.6,13–15
Concussion-Related Protocols
As noted in previous studies,4 our findings reveal that most universities have protocols for student-athlete return to play after a concussion and also provide education to both student-athletes and coaches. However, because the NCAA requires all member institutions to have a concussion-management plan and provide concussion education to student-athletes, we had expected all respondents to indicate compliance. In addition, our results suggest that Division II and III universities were more likely to educate student-athletes and coaches than were Division I universities. It is also possible that personnel other than the ATs, such as the compliance staff, is providing the education, and consequently, the head AT respondents are not reporting it in our survey. However, the implementation of concussion education varies and can range from in-depth lectures to distribution of the NCAA Concussion Fact Sheet.16 Our study did not discern the type of education provided to student-athletes and coaches.
Barriers to implementation of these protocols were also not examined, although previous researchers4 have found that many NCAA coaches, sports medicine clinicians, and compliance administrators thought that their protocols protected athletes well. Importantly, future investigators must develop interventions that evaluate the effectiveness of each means of distributing concussion information to better ascertain which contribute(s) to increased knowledge, recognition, and reporting of concussion.17,18 Simply providing an informational pamphlet or relying on concussion legislation is likely not enough to produce true behavioral change.19 Future study needs to be done at the collegiate level throughout the various divisions to ensure that this important portion of the preparticipation protocol is implemented as effectively as possible.
We also found that approximately one-third of responding universities lacked return-to-learn protocols. Furthermore, only 3% of universities described academic services as being involved in concussion management. The importance of formalized and graduated return-to-learn strategies has only recently been established, and more attention has been given to this concern among youth and secondary school athletes, for whom federally mandated accommodations such as 504 plans and individualized education plans are available.12 Although no research related to the NCAA environment exists, there is no reason to believe that the return to the university classroom is any less complicated by an active concussion. It is possible that our study failed to capture the strategies that are implemented by universities to assist students with academic-related concerns as they recover from concussions. Nevertheless, the NCAA should work with universities to develop or adapt existing return-to-learn protocols20,21 suitable for the college or university student-athlete, especially because guidelines are available.12
Acquiring Student-Athletes' Previous Concussion History
All but 1 university in our sample collected concussion-history information, particularly the number of previous concussions, from incoming student-athletes. Nevertheless, we advocate for universities to obtain more in-depth information, such as resulting hospitalizations, symptoms, and recovery times. Such information can help athletic health care providers better identify and educate athletes who may be at high risk for cumulative effects related to concussion.22 We found that Division II and III universities and universities without football programs may acquire less concussion-history information. Two possible explanations exist for this. First, institutions with smaller staffs may have an increased time burden to conduct a comprehensive assessment protocol, thus resulting in less in-depth baseline assessments. Second, football may have sensitized the staff to the concussion risk, so the absence of a football program removes a motivating factor to use best practices. However, to our knowledge, no literature related to these explanations exists, and further examination is warranted. In addition, because incoming student-athletes may withhold previous concussion information for fear of not being able to play, we recommend researchers develop interventions that will help emphasize the value of disclosing concussion history.
Compliance With NCAA Recommendations for Preparticipation Assessments
In our sample of universities, 43.7% conformed completely with NCAA recommendations for preparticipation assessments to include at least a concussion history, neurocognitive testing, balance testing, and symptom checklist.12 In addition, 93.0% used at least 3 components of the recommendation and 95.7% used at least 2 components. All but 1 school documented incoming student-athletes' concussion histories. These findings parallel those reported among Division I ATs.5 However, these results suggest a few areas for improvement.
First, a low level of conformity with the NCAA recommendations was mostly attributable to the fact that about 4 in 10 universities did not conduct balance testing as part of their preparticipation assessment. In contrast, a large majority of universities conducted neurocognitive testing and symptom checklists at the time of preparticipation assessment. This difference may be due to the resource-dependent nature of balance testing. Symptom checklists can be completed rather quickly by student-athletes. They are also widely available for free and provided as components of tools such as the SCAT3, although we did not examine the source(s) of the symptom checklists. Neurocognitive testing can be implemented in computer laboratories that can house multiple student-athletes at once, although this may not be ideal, as it may lead to invalid scores.23 However, balance testing may require more logistic support. For example, the BESS, which was the most used balance-testing measure in the current study and in previous research,5 requires 1 tester per student-athlete and may take up to 10 minutes per person to complete. Other tests, such as the Sensory Organization Test, require specialized and expensive equipment and are not portable.24 Thus, cost and labor may prevent smaller universities, such as those in Divisions II and III, from implementing balance testing at baseline. Nevertheless, given that the number of concussed student-athletes is drastically smaller than the number of student-athletes who are assessed at baseline, it is much more feasible for universities to conduct postinjury balance testing alongside neurocognitive testing and symptom checklists.
However, it is important to emphasize that the clinical strengths and limitations of various neurocognitive tests, balance tests, and symptom checklists have been previously discussed.23,25–30 In particular, the 2012 Zurich consensus statement22 noted that although baseline neurocognitive testing may supplement concussion assessments, it was not recommended as a required component. As a result, use of these components of baseline testing may depend on each university's impression of the psychometrics and measurement properties of these tests. Continued research examining these tests will help to better inform team medical staff.
Changing Policy Landscape
Recently, the NCAA released the “Inter-Association Consensus: Diagnosis and Management of Sport-Related Concussion Guidelines.”12 Within these guidelines are recommendations for (1) concussion-related protocols, including education of student-athletes and coaches, (2) return-to-play and return-to-learn guidelines, and (3) a 1-time preparticipation assessment that includes a concussion history and a concussion-assessment battery.12 This concussion-assessment battery is a series of tests that help the team medical staff determine the concussed athlete's immediate injury status as well as the appropriate timing for return to play. These tests are typically performed at baseline (before sport participation) and again after an athlete is suspected of sustaining a concussion. Results of the baseline battery then help the team medical staff evaluate whether a concussed athlete should return to play or remain inactive. The NCAA recommendations advocate including neurocognitive testing, balance testing, and a symptom checklist,12 and other groups offer parallel recommendations.22,24,31
The “Inter-Association Consensus: Diagnosis and Management of Sport-Related Concussion Guidelines”12 was created to provide NCAA member institutions with best-practice recommendations, based on the consensus of expert medical groups, for the management of patients with sport-related concussion. Our study focused on those aspects of concussion management that affect student-athletes at the beginning of their collegiate sports careers (ie, policies related to education, return-to-play guidelines, return-to-learn guidelines, and preparticipation assessments). As a result, future research on the additional components of the guidelines, such as recognition and diagnosis, and more in-depth examinations of postconcussion management are warranted.
LIMITATIONS
This study is not without its limitations. We caution readers' interpretation of the current findings based on our response rate (29.4%). This rate is slightly smaller than that of previous studies,2,3,32 and our results may not represent nonresponding universities. It is possible that nonrespondents used concussion-related protocols less than respondents did. For example, our sample had overrepresentation from Division I universities, which were more likely to comply with baseline-assessment recommendations. At the least, 12.8% (143 of the 1113 NCAA member institutions) have complied with baseline-assessment recommendations.
We elected to survey head ATs, as we believed that they would have better knowledge of concussion-related protocols implemented across all sports. However, it is possible that the day-to-day responsibilities of head ATs may have also prevented them from knowing every detail related to concussion protocols that their AT staffs conduct. Furthermore, we were unable to study varying protocols within universities by sport, as this would have increased the respondent burden. Also, we did not ask respondents about university compliance with concussion-related policies. Having a policy at a university does not ensure that the policy is being carried out appropriately. Future investigators should examine compliance with and feasibility of enacting concussion-related policies.
Finally, we focused primarily on the management before the suspected concussions, including baseline assessments and policies and protocols set forth by universities. As a result, we did not examine postconcussion testing, particularly the tools and assessments used for sideline evaluations and return-to-play decisions. However, these topics have been covered by recent researchers.2 Despite these limitations, we believe this study provides an in-depth examination of concussion-related protocols performed by ATs for incoming student-athletes at NCAA member institutions.
CONCLUSIONS
Our findings suggest that numerous universities within the NCAA are implementing baseline assessments. In addition, many universities have enacted policies to provide concussion education to all student-athletes and to guide the management of concussed athletes as they recover and return to the sports and classroom settings. Given the current improvements in knowledge and training regarding the management of sport-related concussion, we believe that our results, alongside those of future prospective researchers, will demonstrate continued improvements in concussion management. Our findings also highlight areas for improvement. Division II and Division III universities may need additional assistance and resources to collect in-depth concussion-history information and to conduct more time-consuming strategies, such as balance testing.
REFERENCES
- 1.Klossner D. 2013–14 NCAA sports medicine handbook. National Collegiate Athletic Association Web site. 2015 http://www.ncaa.org/sites/default/files/SMHB%20Mental%20Health%20INterventions.pdf. Accessed August 6. [Google Scholar]
- 2.Lynall RC, Laudner KG, Mihalik JP, Stanek JM. Concussion-assessment and -management techniques used by athletic trainers. J Athl Train. 2013;48(6):844–850. doi: 10.4085/1062-6050-48.6.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Notebaert AJ, Guskiewicz KM. Current trends in athletic training practice for concussion assessment and management. J Athl Train. 2005;40(4):320–325. [PMC free article] [PubMed] [Google Scholar]
- 4.Baugh CM, Kroshus E, Daneshvar DH, Filali NA, Hiscox MJ, Glantz LH. Concussion management in United States college sports: compliance with National Collegiate Athletic Association concussion policy and areas for improvement. Am J Sports Med. 2015;43(1):47–56. doi: 10.1177/0363546514553090. [DOI] [PubMed] [Google Scholar]
- 5.Kelly K, Jordan EM, Joyner AB, Burdette GT, Buckley TA. National Collegiate Athletic Association Division I athletic trainers' concussion-management practice patterns. J Athl Train. 2014;49(5):665–673. doi: 10.4085/1062-6050-49.3.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men's football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):221–233. [PMC free article] [PubMed] [Google Scholar]
- 7.Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40(4):747–755. doi: 10.1177/0363546511435626. [DOI] [PubMed] [Google Scholar]
- 8.Iverson GL, Lovell MR, Collins MW. Validity of ImPACT for measuring processing speed following sports-related concussion. J Clin Exp Neuropsychol. 2005;27(6):683–689. doi: 10.1081/13803390490918435. [DOI] [PubMed] [Google Scholar]
- 9.Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36(3):263–273. [PMC free article] [PubMed] [Google Scholar]
- 10.McCrea M, Kelly JP, Randolph C, et al. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13(2):27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Guskiewicz KM, Register-Mihalik J, McCrory P, et al. Evidence-based approach to revising the SCAT2: introducing the SCAT3. Br J Sports Med. 2013;47(5):289–293. doi: 10.1136/bjsports-2013-092225. [DOI] [PubMed] [Google Scholar]
- 12.Diagnosis and management of sport-related concussion guidelines. National Collegiate Athletic Association Web site. 2015 http://www.ncaa.org/health-and-safety/concussion-guidelines. Accessed August 6. [Google Scholar]
- 13.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 14.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 15.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 16.Kroshus E, Daneshvar DH, Baugh CM, Nowinski CJ, Cantu RC. NCAA concussion education in ice hockey: an ineffective mandate. Br J Sports Med. 2014;48(2):135–140. doi: 10.1136/bjsports-2013-092498. [DOI] [PubMed] [Google Scholar]
- 17.O'Donoghue EM, Onate JA, Van Lunen B, Peterson CL. Assessment of high school coaches' knowledge of sport-related concussions. Athl Train Sports Health Care. 2009;1(3):120–132. [Google Scholar]
- 18.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014;28(8):1009–1021. doi: 10.3109/02699052.2014.904049. [DOI] [PubMed] [Google Scholar]
- 19.Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, Herring SA. The effect of coach education on reporting of concussions among high school athletes after passage of a concussion law. Am J Sports Med. 2014;42(5):1197–1203. doi: 10.1177/0363546514521774. [DOI] [PubMed] [Google Scholar]
- 20.McGrath N. Supporting the student-athlete's return to the classroom after a sport-related concussion. J Athl Train. 2010;45(5):492–498. doi: 10.4085/1062-6050-45.5.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halstead ME, McAvoy K, Devore CD, et al. Returning to learning following a concussion. Pediatrics. 2013;132(5):948–957. doi: 10.1542/peds.2013-2867. [DOI] [PubMed] [Google Scholar]
- 22.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 23.Moser RS, Schatz P, Neidzwski K, Ott SD. Group versus individual administration affects baseline neurocognitive test performance. Am J Sports Med. 2011;39(11):2325–2330. doi: 10.1177/0363546511417114. [DOI] [PubMed] [Google Scholar]
- 24.Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finnoff JT, Peterson VJ, Hollman JH, Intrarater Smith J. and interrater reliability of the Balance Error Scoring System (BESS) PM R. 2009;1(1):50–54. doi: 10.1016/j.pmrj.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Valovich McLeod TC, Perrin DH, Guskiewicz KM, Shultz SJ, Diamond R, Gansneder BM. Serial administration of clinical concussion assessments and learning effects in healthy young athletes. Clin J Sport Med. 2004;14(5):287–295. doi: 10.1097/00042752-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Wilkins JC. Valovich McLeod TC, Perrin DH, Gansneder BM. Performance on the Balance Error Scoring System decreases after fatigue. J Athl Train. 2004;39(2):156–161. [PMC free article] [PubMed] [Google Scholar]
- 28.Barr WB, McCrea M. Sensitivity and specificity of standardized neurocognitive testing immediately following sports concussion. J Int Neuropsychol Soc. 2001;7(6):693–702. doi: 10.1017/s1355617701766052. [DOI] [PubMed] [Google Scholar]
- 29.Alla S, Sullivan SJ, Hale L, McCrory P. Self-report scales/checklists for the measurement of concussion symptoms: a systematic review. Br J Sports Med. 2009;43(suppl 1):i3–i12. doi: 10.1136/bjsm.2009.058339. [DOI] [PubMed] [Google Scholar]
- 30.Schatz P, Sandel N. Sensitivity and specificity of the online version of ImPACT in high school and collegiate athletes. Am J Sports Med. 2013;41(2):321–326. doi: 10.1177/0363546512466038. [DOI] [PubMed] [Google Scholar]
- 31.Broglio SP, Macciocchi SN, Ferrara MS. Sensitivity of the concussion assessment battery. Neurosurgery. 2007;60(6):1050–1057. doi: 10.1227/01.NEU.0000255479.90999.C0. [DOI] [PubMed] [Google Scholar]
- 32.Braithwaite D, Emery J, De Lusignan S, Sutton S. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20(5):545–551. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]