Publisher's Note: There is an Inside Blood Commentary on this article in this issue.
Key Points
Deep clonal responses to chemotherapy are associated with improved renal and overall outcomes in patients with light chain deposition disease.
Deep clonal responses should be targeted, even in patients with advanced chronic kidney disease from light chain deposition disease.
Abstract
Light chain deposition disease (LCDD) is characterized by the deposition of monotypic immunoglobulin light chains in the kidney, resulting in renal dysfunction. Fifty-three patients with biopsy-proven LCDD were prospectively followed at the UK National Amyloidosis Center. Median age at diagnosis was 56 years, and patients were followed for a median of 6.2 years (range, 1.1-14.0 years). Median renal survival from diagnosis by Kaplan-Meier analysis was 5.4 years, and median estimated patient survival was 14.0 years; 64% of patients were alive at censor. Sixty-two percent of patients required dialysis, and median survival from commencement of dialysis was 5.2 years. There was a strong association between hematologic response to chemotherapy and renal outcome, with a mean improvement in glomerular filtration rate (GFR) of 6.1 mL/min/year among those achieving a complete or very good partial hematologic response (VGPR) with chemotherapy, most of whom remained dialysis independent, compared with a mean GFR loss of 6.5 mL/min/year among those achieving only a partial or no hematologic response (P < .009), most of whom developed end-stage renal disease (ESRD; P = .005). Seven patients received a renal transplant, and among those whose underlying clonal disorder was in sustained remission, there was no recurrence of LCDD up to 9.7 years later. This study highlights the need to diagnose and treat LCDD early and to target at least a hematologic VGPR with chemotherapy, even among patients with advanced renal dysfunction, to delay progression to ESRD and prevent recurrence of LCDD in the renal allografts of those who subsequently receive a kidney transplant.
Medscape Continuing Medical Education online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint providership of Medscape, LLC and the American Society of Hematology.
Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at http://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 2902.
Disclosures
Associate Editor Jesús San Miguel served as an advisor or consultant for Janssen, Onyx, Bristol-Myers Squibb, Merck Sharp and Dohme, Novartis, Celgene, and Millennium. The authors and CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, declare no competing financial interests.
Learning objectives
Describe renal outcomes in patients with light chain deposition disease (LCDD).
Discuss survival and extrarenal outcomes in patients with LCDD.
Distinguish the association between hematologic response to chemotherapy and renal outcome in patients with LCDD.
Release date: December 24, 2015; Expiration date: December 24, 2016
Introduction
Monoclonal immunoglobulin deposition disease is a group of multisystem disorders characterized by deposition of monoclonal immunoglobulin light or heavy chains in various organs.1 The most commonly diagnosed monoclonal immunoglobulin deposition disease is light chain deposition disease (LCDD) in which monoclonal immunoglobulin light chains (LCs) are deposited, the others being heavy chain deposition disease and light and heavy chain deposition disease.2,3 Clinical manifestations of LCDD vary, depending on which organs are involved.4 Because LCs are filtered by the glomeruli, reabsorbed in proximal tubules by receptor-mediated endocytosis, and degraded in tubular cells by lysosomal enzymes,4-6 the kidney is the principal target for LC deposition, and renal involvement and dysfunction usually dominate the clinical disease course.1,7 Hepatic, cardiac, and neural deposits have also been documented however, and need to be considered in all newly diagnosed patients with renal LCDD.6,8,9
LCDD typically presents with hypertension, microhematuria, and proteinuria, and, in the absence of therapy, the clinical course is one of inexorably progressive chronic kidney disease (CKD), leading to a requirement for renal replacement therapy (RRT).2,4,9-11 Reported outcomes with renal transplantation have generally been poor, with most allograft failures occurring within a few years from recurrent LCDD.12,13
Here, we report the clinical presentation, course, and outcome among 53 patients with LCDD who were prospectively followed at the UK National Amyloidosis Centre (NAC), highlighting the importance of aggressively treating the underlying monoclonal proliferative disease.
Methods
Patients
All 53 patients with biopsy-proven LCDD followed prospectively at the NAC between 2002 and 2015 were included in this study. Although this was not a formal protocolized study, patients attended the NAC for their initial evaluation and were prospectively and systematically followed at regular intervals (usually every 6 months) for evaluation of organ function and hematologic parameters. Attendance at the NAC included a comprehensive histologic and clinical review including an assessment at baseline for the presence of extrarenal involvement by LCDD. Investigations included a standardized 6-minute walk test, electrocardiography, detailed echocardiography, and serologic markers of cardiac (N-terminal pro-brain natriuretic peptide [NT-proBNP] and Hs-Troponin T), liver and bone function, as well as urine biochemistry. No patients were lost to follow-up.
All patients gave informed consent and were managed in accordance with the Declaration of Helsinki. The study was approved by the Royal Free Hospital Ethics Committee.
Histology
All renal biopsies were processed by standard techniques for light microscopy, immunofluorescence and/or immunohistochemistry, and electron microscopy. All biopsies were stained with Congo red dye, as well as antibodies to κ and λ immunoglobulin light chains.14,15 They were initially reported by local renal pathologists and then reviewed, where necessary after restaining, by a single renal pathologist at the Royal Free London National Health Service Foundation Trust (PB).9,12,16,17
Liver LCDD was confirmed histologically in both cases in which it was suspected biochemically, and lung LCDD was confirmed by surgical lung biopsy in a patient with panacinar emphysema.18
Hematologic investigations
All patients underwent a bone marrow biopsy at diagnosis to determine the plasma cell percentage and morphology. Detection and characterization of serum and urine monoclonal immunoglobulins were performed using conventional immunoelectrophoresis and immunofixation. Data on serum free light chains (FLCs) were not available for all patients at the time of diagnosis, as nephelemetric measurements of serum FLCs (Freelite, Binding Site, Birmingham, UK) only became available after 2002. In such cases, FLCs at the time of diagnosis were obtained from analysis of stored serum samples. At diagnosis, all patients were tested for hypercalcemia, anemia, and osteolytic lesions.19,20
Hematologic response to chemotherapy, in the face of polyclonal retention of FLCs associated with CKD, was defined according to the difference between pathogenic and nonpathogenic light chain concentration (dFLC), as previously described.21 Briefly, hematologic complete response (CR) was defined as normalization of FLC ratio in the absence of a detectable monoclonal protein by serum and urine immunofixation electrophoresis, hematologic very good partial response (VGPR) as a decrease in dFLC to <40 mg/L, hematologic partial response (PR) as >50% decrease in dFLC from baseline, and hematologic no response (NR) as ≤50% decrease in dFLC from baseline. FLCs and paraproteins were monitored monthly, and a formal hematologic response assessment was performed at 6 months from start of chemotherapy.
Other investigations
Proteinuria was measured from a 24-hour urine collection at presentation and every 6 months thereafter. Glomerular filtration rate was estimated (eGFR) using the Modification of Diet in Renal Disease formula. Nephrotic range proteinuria (NRP) was defined as 24-hour proteinuria ≥3 g and nephrotic syndrome was NRP accompanied by serum albumin of <2.5 g/dL and peripheral edema. Hypertension was defined by systolic blood pressure >140 mm Hg, diastolic blood presure >90 mm Hg, or a requirement for antihypertensive medication.
Renal course was determined by change in eGFR throughout follow-up. Renal survival was defined as time from diagnosis to RRT. Twenty-one patients were excluded from the analysis of renal response in relation to hematologic response (10 cases on RRT before diagnosis of LCDD and 11 cases, median eGFR 12 mL/min per year at diagnosis, who received RRT before chemotherapy), leaving 32 evaluable patients for this analysis.
Statistical methods
Renal outcomes (native and transplant) were censored at the date of last GFR measurement prior to 20 June 2015, and patient survival was censored on the same date. For analyses of renal survival, patients who died without a requirement for RRT were censored. Kaplan-Meier analyses were used to investigate both renal and patient survival, and the log-rank test was used to compare differences in stratified survival analyses. Univariate analysis was used to investigate the association of histologic features with GFR and proteinuria. Mann-Whitney U tests were used to compare outcomes between patients with different categories of hematologic response.
Study limitations
The diversity of local chemotherapy regimens and the small numbers receiving each regimen invalidated a comparison between each regimen.
Results
Patients
Fifty-one of 53 patients were diagnosed with LCDD on renal histology (Figure 1). Two patients were diagnosed with LCDD on liver biopsy; however, in both cases, there was established proteinuric CKD but a renal biopsy had not been performed. Median age at diagnosis was 56 years (range, 29-78 years), and the male/female ratio was 2.3:1. Patient demographics and clinical characteristics at the time of diagnosis, as well as results of hematologic investigations, are shown in Table 1. At diagnosis, 94% of patients were hypertensive and 90% had hematuria. The mean 24-hour urinary protein loss was 4.1 g (range, 0.1-15.5 g/24 hr). Ten patients received RRT before their diagnostic biopsy, including 1 patient who was diagnosed with LCDD on a renal transplant biopsy, performed to investigate deteriorating allograft function.
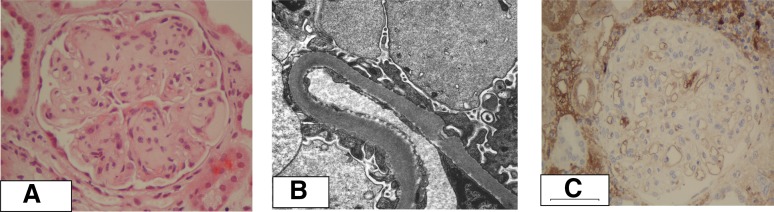
Figure 1.
Histology in LCDD. (A) Nodular glomerulosclerosis. High power view of a glomerulus exhibits mesangial expansion by periodic acid-Schiff–positive matrix that focally forms nodules with peripheral expansion producing lobules (periodic acid-Schiff stain, magnification ×400). (B) Granular electron dense deposits along the lamina rara interna of the glomerular basement membrane are seen on electron microscopy (magnification ×11 500). (C) Absence of specific mesangial staining with anti-λ antibodies, despite the presence of high background staining (magnification ×600).
Table 1.
Demographic, clinical, and hematologic characteristics at diagnosis
| Characteristic | Value |
|---|---|
| Median (range) age (years) | 56 (29-78) |
| Sex (male/female) (n) | 37/16 |
| Race (n) | |
| White | 51 |
| Black | 1 |
| Asian | 1 |
| Hypertension (n) | 50 (94%) |
| GFR (n) | |
| CKD stage 1 | 0 |
| CKD stage 2/3 | 23 (43%) |
| CKD stage 4/5 (including RRT) | 30 (57%) |
| Mean eGFR (mL/min per year)* | 27 (0-79) |
| RRT before diagnosis (n) | |
| Dialysis | 9 (17%) |
| Transplant | 1 (2%) |
| Mean (range) urinary protein loss (g/24 hours) | 4.1 (0.1-15.5) |
| Nephrotic range proteinuria (n)† | 24/45 (53%) |
| Nephrotic syndrome (n)† | 10/45 (22%) |
| Microscopic hematuria (n)‡ | 45/50 (90%) |
| Extrarenal light chain deposits (n) | 5 (9.4%) |
| Heart | 2 (3.8%) |
| Liver | 2 (3.8%) |
| Lung | 1 (1.9%) |
| Nerve | 0 (0%) |
| Hematologic investigations | |
| Abnormal serum FLC concentration and ratio (n) | 53 (100%) |
| LC isotype κ | 43/53 (81%) |
| Λ | 10/53 (19%) |
| Median (range) pathogenic free light chain concentration (mg/L) | |
| κ | 724 (25.6-25 700) |
| Λ | 147 (29.8-742) |
| Median (range) FLC ratio ĸ:λ | |
| κ | 29.2 (2.9-150.8) |
| Λ | 0.17 (0.05-0.2) |
| Bence Jones proteinuria (n) | 20 (44.4%) |
| Monoclonal protein in serum detected by immunofixation (n) | 23 (43.4%) |
| No monoclonal protein detected by immunofixation (n) | 19 (35.8%) |
| Bone marrow findings | |
| ≥10% clonal plasma cells (n) | 6 (11.3%) |
| <10% clonal plasma cells (n) | 46 (86.8%) |
| Chronic lymphatic leukemia (n) | 1 (2%) |
An eGFR of 0 was used for anuric patients on renal replacement therapy.
No 24-hour urine collection performed among 8 of those receiving dialysis at the time of renal biopsy.
No documentation of presence/absence of hematuria in 3 patients.
Renal histology
Characteristic granular electron-dense deposits along basement membranes were identified by electron microscopy in all renal biopsies, as well as in the 2 respective liver specimens (Figure 1B). Amyloid deposits were excluded by Congo red staining in all biopsies. Detailed renal biopsy findings are shown in supplemental Table 1 available on the Blood Web site. Briefly, light microscopy findings typically showed nodular mesangial sclerosis, tubular atrophy, and interstitial fibrosis associated with immunospecific staining of basement membranes with the causative light chain.
No particular histologic feature was significantly associated with either baseline GFR or degree of proteinuria. Furthermore, neither presence of nodular glomerulosclerosis (P = .639) nor interstitial fibrosis (P = .475) was significantly associated with renal survival.
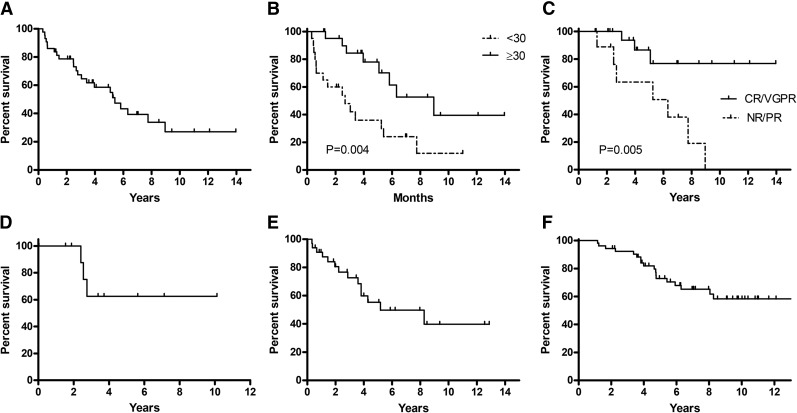
Renal outcomes in relation to baseline investigations
Median follow-up for the whole cohort was 6.2 years (range, 1.1-14.0 years). Among 43 patients who were not receiving RRT at the time of diagnosis, the mean rate of GFR decline (prior to RRT or death) was 3.7 mL/min per year. Twenty-three patients commenced dialysis during follow-up; median renal survival from diagnosis by Kaplan-Meier estimate for those who were not already receiving RRT at baseline was 5.4 years (Figure 2A). Unsurprisingly, CKD stage at diagnosis had a significant impact on renal survival with those who had CKD stage 2 or 3 at diagnosis remaining dialysis independent for a median of 9.0 years compared with only 2.7 years among those with CKD stage 4 or 5 at diagnosis (excluding the 10 patients already receiving RRT at the time of biopsy; P = .004; Figure 2B). There was no significant difference in renal survival between patients who had nephrotic range proteinuria (>3 g/24 hr) at diagnosis and those with subnephrotic proteinuria, although proteinuria >6 g/24 hr was associated with reduced renal survival (P = .017). Renal survival was not influenced by degree of bone marrow plasmacytosis.
Figure 2.
Renal and patient survival in LCDD. (A) Median renal survival from diagnosis of LCDD was 5.4 years. (B) Renal survival was significantly longer among those who were diagnosed, whereas eGFR was ≥30 mL/min per year compared with those diagnosed once GFR was <30 mL/min per year (P = .004). (C) Renal survival was significantly longer among patients who achieved a hematologic CR/VGPR with first-line chemotherapy compared with those who achieved a hematologic PR/NR (P = .005). (D) Renal survival from ASCT among 11 patients with median GFR of 24 mL/min per year at start of the procedure. (E) Patient survival from commencement of dialysis, censored at the time of transplantation. (F) Patient survival from diagnosis of LCDD; median estimated survival was 14.0 years.
Renal outcome in relation to hematologic response
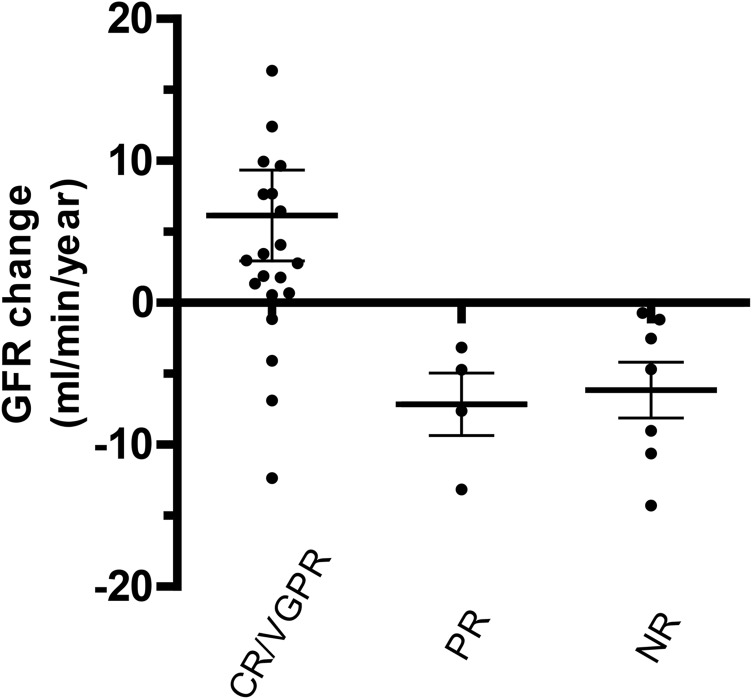
We compared renal outcomes among 32 evaluable patients who achieved different levels of clonal response (as determined by changes in their dFLC values) to first-line chemotherapy and/or autologous stem cell transplant (ASCT). The first-line chemotherapy regimens that were administered to these patients are shown in Table 2. There was a mean improvement in GFR of 6.1 mL/min per year from a baseline of 26 mL/min per year among 21 patients who achieved a hematologic CR/VGPR at 6 months compared with a mean GFR loss of 6.5 mL/min per year from a baseline of 34 mL/min per year among both those who achieved a hematologic PR (n = 4) or NR (n = 7; Figure 3; P < .009). Only 3 of 21 patients who achieved a hematologic CR/VGPR with first-line chemotherapy required RRT throughout follow-up compared with 7 of 11 patients who achieved an initial PR/NR (Figure 2C; P = .005). Median time to hematologic relapse among responders was 3.6 years.
Table 2.
First-line chemotherapy regimens and hematologic response
| n | CR | VGPR | PR | NR | |
|---|---|---|---|---|---|
| Thalidomide based | 11 | 3 | 2 | 1 | 5 |
| Bortezomib based | 9 | 8 | 0 | 1 | 0 |
| Alkylator based | 6 | 3 | 1 | 1 | 1 |
| Melphalan autologous stem cell transplant | 4 | 4 | 0 | 0 | 0 |
| Lenalidomide based | 1 | 0 | 0 | 1 | 0 |
| Steroids alone | 1 | 0 | 0 | 0 | 1 |
Figure 3.
Rate of change of GFR in relation to hematologic response. The scatter graph and plots below demonstrates the rate of change in GFR per year and the mean ± standard error of the mean for each dataset for patients with varying degrees of clonal response. GFR increased among those achieving either a hematologic CR or VGPR but declined among those who achieved only a PR or NR with chemotherapy (Mann-Whitney U test, P < .009).
Sixteen patients in the whole cohort (median age, 50 years; range, 38-72 years) received a melphalan-conditioned ASCT. Median pretreatment bone marrow plasmacytosis among those who underwent ASCT was 12% (range, 4-50%). Four patients were dialysis dependent prior to ASCT, the aim of which was to suppress the plasma cell dyscrasia to decrease the likelihood of disease recurrence following subsequent renal transplantation, and 1 patient had a functioning renal transplant at the time of ASCT. One patient with preexisting severe myopathy, aged 72 years, died during ASCT from pneumonia (transplant-related mortality, 6.7%). Median GFR prior to ASCT among 11 patients not requiring RRT was 24 mL/min per year (range, 11-51 mL/min per year), which had increased among the 10 surviving patients to 38 mL/min per year (range dialysis to >90 mL/min per year) at the end of follow-up. Thirteen of 15 patients who survived ASCT achieved a hematologic CR and 2 achieved PR. After a median follow-up from ASCT of 4.4 years (range, 0.04-12.2 years), only 2 of 14 patients required further chemotherapy for hematologic relapse, administered 5.2 and 5.5 years later. Only 3 of 11 patients who were not on RRT prior to ASCT, all of whom had CKD stage 4 at the time of ASCT, eventually required dialysis 2.4, 2.6, and 2.8 years after the procedure; it is notable that all 3 patients had persistent nephrotic-range proteinuria following ASCT, whereas proteinuria fell following ASCT in all patients who remained dialysis independent. Renal survival after ASCT (censored at death) by Kaplan-Meier analysis for the cohort of 11 dialysis-independent patients is shown in Figure 2D; at censor, median renal survival had not been reached.
Outcomes with RRT
Dialysis
Thirty-three (62%) patients from the whole cohort required dialysis during their disease course (including 10 from before the diagnosis of LCDD). Eight patients received peritoneal dialysis and 25 received hemodialysis. Median patient survival from commencement of dialysis, censored at transplantation, was 5.2 years (Figure 2E), and there was no difference in survival between those commencing different dialysis modalities (P = .336).
Renal transplantation
Seven patients from the whole cohort underwent renal transplantation, and in 3 of these cases, the transplant failed. Cause of renal allograft failure was biopsy-proven LCDD recurrence in 2 patients and rejection secondary to noncompliance with immunosuppression in the remaining patient. Neither patient whose LCDD recurred had received chemotherapy prior to renal allograft failure, which occurred after 1.6 and 1.9 years. The 4 remaining patients had GFRs of 45, 44, 50, and 50 mL/min per year at censor 9.7, 6.2, 5.1, and 0.8 years after renal transplantation, respectively, without clinical, biochemical, or histologic evidence of LCDD in their allografts. One of these patients underwent a high-dose melphalan ASCT shortly after renal transplantation without loss of GFR during the procedure, and the other 3 patients received an ASCT prior to renal transplantation. The latter 3 patients remained in complete hematologic remission at censor 9.6, 8.6, and 6.8 years after ASCT.
Extrarenal outcomes
There was improvement in cardiac (2 patients) and hepatic (2 patients) function among those with extrarenal LCDD who achieved a hematologic response. NT-proBNP values fell from 909 to 6 pmol/L and from 1714 to 296 pmol/L in association with an improvement in diastolic function on echocardiography in both patients with cardiac LCDD. Alkaline phosphatase levels fell from 276 to 71 UI/L (normal range, 38-126 IU/L) and from 522 to 159 IU/L in both patients with hepatic LCDD. One patient with pulmonary LCDD who achieved a hematologic CR has had stable spirometry but has failed to improve clinically and, at the time of censor, was awaiting lung volume reduction surgery with the aim of improving lung mechanics and gas exchange.
Patient survival
Median estimated patient survival from diagnosis by Kaplan-Meier analysis for the whole cohort was 14.0 years (Figure 2F). Nineteen patients died during follow-up, and causes of death were infection (n = 6), ischemic heart disease (n = 4), ESRD (n = 3), congestive cardiac failure (n = 2), cerebrovascular accident (n = 1), gastrointestinal hemorrhage (n = 1), and multiple myeloma (n = 2).
Discussion
The prolonged follow-up of this large cohort of patients highlights systematically for the first time in LCDD the relationship between the response to chemotherapy of the underlying hematologic disease and renal outcome. The rate of native GFR loss among those who did not achieve either a CR or VGPR hematologic response with chemotherapy was 6.5 mL/min per year, which is higher than that reported for CKD generally, where the average decline in GFR is between 0.5 and 2.5 mL/min per year.22,23 This is not surprising because these patients were continuing to deposit light chains in their kidneys. In contrast, those who did achieve a hematologic CR or VGPR with chemotherapy had a mean improvement in GFR of 6.1 mL/min per year throughout the time that their clonal response was sustained and only 3 of 21 such cases required dialysis during follow-up, despite a median GFR at the start of chemotherapy of only 26 mL/min per year. These data clearly indicate that one should strive to achieve a hematologic CR when treating patients with LCDD, even in the context of preexisting stage 4 CKD. In addition, the data demonstrate that ASCT can be successful, even when undertaken at a low GFR (median, 24 mL/min per year; range, 11-51 mL/min per year in this cohort), with little apparent risk of precipitating an acute renal decline. Despite these findings, it is notable that patients treated with chemotherapy while their GFR was >30 mL/min per year had a substantially better renal survival (median, ∼9 years) than patients who started chemotherapy having already reached CKD stage 4.
Our findings highlight important differences between LCDD and the more commonly diagnosed prototypic disease of monoclonal light chain deposition, renal AL (light chain) amyloidosis. Although renal AL amyloid deposition can be slowed or halted by chemotherapy, which successfully suppresses light chain production with accompanying prolongation of renal survival, overall prognosis in AL amyloidosis is markedly poorer than in LCDD, and renal prognosis among those diagnosed once stage 4 or 5 CKD has supervened is better among patients with LCDD than renal AL amyloidosis.24 Indeed, it is unusual to see substantial improvements in GFR among patients with renal AL amyloidosis once CKD stage 4 has supervened, even in the context of a complete hematologic response. Additionally, ASCT in AL amyloidosis is associated with a significant risk of transplant-related mortality and may precipitate an acute irreversible decline in GFR25; these risks appear to be lower in LCDD.
In the absence of a hematologic response, renal transplants failed rapidly from recurrence of LCDD, as previously reported.12 However, among those patients who achieved a hematologic CR or VGPR before or shortly after renal transplantation, there was no evidence of recurrent LCDD, even after prolonged follow-up. Both bortezomib-based regimens and melphalan-conditioned ASCT were associated with high rates of CR/VGPR in this cohort, and further prospective studies are required to determine the optimal chemotherapy protocol in patients with LCDD. Such studies will be difficult to conduct, however, due to the rarity of the disease, the variability of disease burden and responsiveness to chemotherapy of the underlying clonal diseases, and the complexities surrounding dose reduction of intravenous melphalan in the context of impaired renal function.26
Extrarenal light chain deposits were only identified in 4 patients (7.5%) from this cohort, with 1 patient having both cardiac and liver involvement. It is noteworthy that there did not appear to be an association between light chain concentration in the serum and presence of extrarenal disease. In all such cases, the extrarenal disease course mirrored that in the kidneys following chemotherapy, such that improvements in both cardiac and hepatic function were observed in association with hematologic CRs.
In conclusion, patient survival and tolerance of high-dose chemotherapy appears to be substantially better in LCDD than in systemic AL amyloidosis. LCDD should be aggressively treated with chemotherapy, because achieving a hematologic CR or VGPR prolongs renal survival, even if advanced renal impairment has supervened, while also preventing renal allograft failure from recurrent LCDD among those who receive renal transplants.
Acknowledgments
The authors thank our many physician colleagues for referring and caring for the patients, as well as the staff at the National Amyloidosis Centre.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: R.H.S. and J.D.G. designed the study, performed research, and wrote the manuscript; P.N.H. performed research and wrote the manuscript; A.D.W., S.M., S.S., M.F., K.P., C.J.W., and H.J.L. performed research; and J.A.G. and P.B. performed research and analyzed data.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Julian Gillmore, National Amyloidosis Centre, Division of Medicine, University College London, Royal Free Campus, Rowland Hill Street, London NW3 2PF, UK; e-mail: j.gillmore@ucl.ac.uk.
References
- 1.Randall RE, Williamson WC, Jr, Mullinax F, Tung MY, Still WJ. Manifestations of systemic light chain deposition. Am J Med. 1976;60(2):293–299. doi: 10.1016/0002-9343(76)90440-x. [DOI] [PubMed] [Google Scholar]
- 2.Nasr SH, Valeri AM, Cornell LD, et al. Renal monoclonal immunoglobulin deposition disease: a report of 64 patients from a single institution. Clin J Am Soc Nephrol. 2012;7(2):231–239. doi: 10.2215/CJN.08640811. [DOI] [PubMed] [Google Scholar]
- 3.Masai R, Wakui H, Togashi M, et al. Clinicopathological features and prognosis in immunoglobulin light and heavy chain deposition disease. Clin Nephrol. 2009;71(1):9–20. doi: 10.5414/cnp71009. [DOI] [PubMed] [Google Scholar]
- 4.Pozzi C, Locatelli F. Kidney and liver involvement in monoclonal light chain disorders. Semin Nephrol. 2002;22(4):319–330. [PubMed] [Google Scholar]
- 5.Batuman V, Guan S. Receptor-mediated endocytosis of immunoglobulin light chains by renal proximal tubule cells. Am J Physiol. 1997;272(4 Pt 2):F521–F530. doi: 10.1152/ajprenal.1997.272.4.F521. [DOI] [PubMed] [Google Scholar]
- 6.Ronco P, Plaisier E, Mougenot B, Aucouturier P. Immunoglobulin light (heavy)-chain deposition disease: from molecular medicine to pathophysiology-driven therapy. Clin J Am Soc Nephrol. 2006;1(6):1342–1350. doi: 10.2215/CJN.01730506. [DOI] [PubMed] [Google Scholar]
- 7.Matsuzaki K, Ohsawa I, Nishitani T, et al. Marked improvement by high-dose chemotherapy and autologous stem cell transplantation in a case of light chain deposition disease. J Nephrol. 2011;24(2):246–249. doi: 10.5301/jn.2011.6241. [DOI] [PubMed] [Google Scholar]
- 8.Pozzi C, Locatelli F. The patient with insidious chronic renal failure and the patient with the nephrotic syndrome--two manifestations of a protean and not so rare disease. Nephrol Dial Transplant. 1996;11(9):1876–1880. [PubMed] [Google Scholar]
- 9.Lin J, Markowitz GS, Valeri AM, et al. Renal monoclonal immunoglobulin deposition disease: the disease spectrum. J Am Soc Nephrol. 2001;12(7):1482–1492. doi: 10.1681/ASN.V1271482. [DOI] [PubMed] [Google Scholar]
- 10.Buxbaum J. Mechanisms of disease: monoclonal immunoglobulin deposition. Amyloidosis, light chain deposition disease, and light and heavy chain deposition disease. Hematol Oncol Clin North Am. 1992;6(2):323–346. [PubMed] [Google Scholar]
- 11.Pozzi C, Fogazzi GB, Banfi G, Strom EH, Ponticelli C, Locatelli F. Renal disease and patient survival in light chain deposition disease. Clin Nephrol. 1995;43(5):281–287. [PubMed] [Google Scholar]
- 12.Leung N, Lager DJ, Gertz MA, Wilson K, Kanakiriya S, Fervenza FC. Long-term outcome of renal transplantation in light-chain deposition disease. Am J Kidney Dis. 2004;43(1):147–153. doi: 10.1053/j.ajkd.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 13.Short AK, O’Donoghue DJ, Riad HN, Short CD, Roberts IS. Recurrence of light chain nephropathy in a renal allograft. A case report and review of the literature. Am J Nephrol. 2001;21(3):237–240. doi: 10.1159/000046254. [DOI] [PubMed] [Google Scholar]
- 14.Puchtler H, Sweat F, Levine M. On the binding of Congo red by amyloid. J Histochem Cytochem. 1962;10:355–364. [Google Scholar]
- 15.Tennent GA, Cafferty KD, Pepys MB, Hawkins PN. Congo red overlay immunohistochemistry aids classification of amyloid deposits. In: Kyle RA, Gertz MA, editors. Amyloid and Amyloidosis 1998. Pearl River, NY: Parthenon Publishing; 1999. pp. 160–162. [Google Scholar]
- 16.Chang A, Peutz-Kootstra CJ, Richardson CA, Alpers CE. Expanding the pathologic spectrum of light chain deposition disease: a rare variant with clinical follow-up of 7 years. Mod Pathol. 2005;18(7):998–1004. doi: 10.1038/modpathol.3800368. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz MM. Monoclonal immunoglublin deposition diseases. In: Jennete J, Olson JL, Schwartz MM, Silvia FG, editors. Hepinstalls’ Pathology of the Kidney. 6th ed. Baltimore: Williams & Wilkins; 2007. pp. 869–877. [Google Scholar]
- 18.Colombat M, Gounant V, Mal H, Callard P, Milleron B. Light chain deposition disease involving the airways: diagnosis by fibreoptic bronchoscopy. Eur Respir J. 2007;29(5):1057-1060. [DOI] [PubMed]
- 19.Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia. 2009;23(1):3–9. doi: 10.1038/leu.2008.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajkumar SV, Merlini G, San Miguel JF. Haematological cancer: Redefining myeloma. Nat Rev Clin Oncol. 2012;9(9):494–496. doi: 10.1038/nrclinonc.2012.128. [DOI] [PubMed] [Google Scholar]
- 21.Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30(36):4541–4549. doi: 10.1200/JCO.2011.37.7614. [DOI] [PubMed] [Google Scholar]
- 22.Turin TC, James M, Ravani P, et al. Proteinuria and rate of change in kidney function in a community-based population. J Am Soc Nephrol. 2013;24(10):1661–1667. doi: 10.1681/ASN.2012111118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies DF, Shock NW. Age changes in glomerular filtration rate, effective renal plasma flow, and tubular excretory capacity in adult males. J Clin Invest. 1950;29(5):496–507. doi: 10.1172/JCI102286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pinney JH, Lachmann HJ, Bansi L, et al. Outcome in renal Al amyloidosis after chemotherapy. J Clin Oncol. 2011;29(6):674–681. doi: 10.1200/JCO.2010.30.5235. [DOI] [PubMed] [Google Scholar]
- 25.Comenzo RL, Gertz MA. Autologous stem cell transplantation for primary systemic amyloidosis. Blood. 2002;99(12):4276–4282. doi: 10.1182/blood.v99.12.4276. [DOI] [PubMed] [Google Scholar]
- 26.Carlson K, Hjorth M, Knudsen LM Nordic Myeloma Study Group. Toxicity in standard melphalan-prednisone therapy among myeloma patients with renal failure—a retrospective analysis and recommendations for dose adjustment. Br J Haematol. 2005;128(5):631–635. doi: 10.1111/j.1365-2141.2005.05366.x. [DOI] [PubMed] [Google Scholar]