Abstract
Purpose
the efficacy and safety of using a suspensory button for femoral fixation in anatomical anterior cruciate ligament (ACL) reconstruction with bone-patellar tendon-bone (BPTB) graft have not been established. The purpose of the current study was to evaluate bone plug integration onto the femoral socket and migration of the bone plug and the EndoButton (EB) (Smith & Nephew, Andover, MA, USA) after rectangular tunnel ACL reconstruction with BPTB autograft.
Methods
thirty-four patients who underwent anatomical rectangular ACL reconstruction with BPTB graft using EB for femoral fixation and in whom three-dimensional (3D) computed tomography (CT) was performed one week and one year after surgery were included in this study. Bone plug integration onto the femoral socket, bone plug migration, soft tissue interposition, EB migration and EB rotation were evaluated on 3D CT. The clinical outcome was also assessed and correlated with the imaging outcomes.
Results
the bone plug was integrated onto the femoral socket in all cases. The incidence of bone plug migration, soft tissue interposition, EB migration and EB rotation was 15, 15, 9 and 56%, respectively. No significant association was observed between the imaging outcomes. The postoperative mean Lysholm score was 97.1 ± 5.0 points. The postoperative side-to-side difference, evaluated using a KT-2000 arthrometer, averaged 0.5 ± 1.3 mm. There were no complications associated with EB use. Imaging outcomes did not affect the postoperative KT side-to-side difference.
Conclusions
the EB is considered a reliable device for femoral fixation in anatomical rectangular tunnel ACL reconstruction with BPTB autograft.
Level of evidence
Level IV, therapeutic case series.
Keywords: anterior cruciate ligament reconstruction, bone-patellar tendon-bone, EndoButton, suspensory fixation
Introduction
Aperture fixation with interference screws has been commonly used for femoral fixation in anterior cruciate ligament (ACL) reconstruction using bone-patellar tendon-bone (BPTB) graft (1). By providing a secure fixation close to the articular surface (2), this technique avoids concerns related to graft-tunnel motion. However, complications associated with interference screw femoral fixation, including graft laceration, intra-articular migration and femur fracture have been reported (3–5). Meanwhile, femoral fixation with suspension buttons has been reported to be a reliable technique in ACL reconstruction using hamstring tendons (6–9), although it allows graft-tunnel motion (10). By contrast, there are only a few articles that report using only suspensory buttons in ACL reconstruction with BPTB graft (11). Shino et al. reported the use of an interference screw or the other fixation techniques including a suspensory button for femoral fixation in their anatomical rectangular tunnel ACL reconstruction using BPTB graft (12). To date, suspensory button fixation of BPTB grafts has not been thoroughly examined from the perspective of graft healing and risk of migration. Therefore, the purposes of the current study were to evaluate bone plug integration onto the femoral socket and migration of the bone plug and EndoButton (EB) (Smith & Nephew, Andover, MA, USA) after rectangular tunnel ACL reconstruction with BPTB autograft. Furthermore, we investigated the effect of these variables on the clinical evaluation. Our hypothesis was that the incidence of bone plug migration in the femoral socket and EB migration would be low following the procedure.
Methods
Participants
Of the 56 consecutive patients undergoing rectangular tunnel ACL reconstruction using BPTB autograft at our institute between July 2009 and August 2012, 34 were included in this study. The inclusion criteria for the study were as follows: i) no prior intra-articular ligament reconstruction or osteotomy around the knee joint had been performed; and ii) a 3D computed tomography (CT) scan of the operated knee had been performed at one week and one year after surgery. There were 17 patients who did not meet the first inclusion criterion, and 5 who did not meet the second; therefore, in total, 22 patients were excluded. The patients included in the study were 8 females and 26 males, with a median age of 25 years (range, 16–50 years). The patient information is summarized in Table 1. The institutional review board approved this retrospective study. The patients and their families were informed that data from their cases would be submitted for publication, and they all provided consent.
Table 1.
Preoperative patient information.
| Number of patients | 34 |
| Gender (female/male) | 8/26 |
| Age (years) | 25 (16–50) |
| Body height (cm) | 169 ± 6 |
| Body weight (kg) | 68 ± 14 |
| Body mass index (kg/m2) | 23.3 ± 3.8 |
| Tegner activity scale score | 7 (5–10) |
Data are given as means ± standard deviations or medians (range).
Interventions
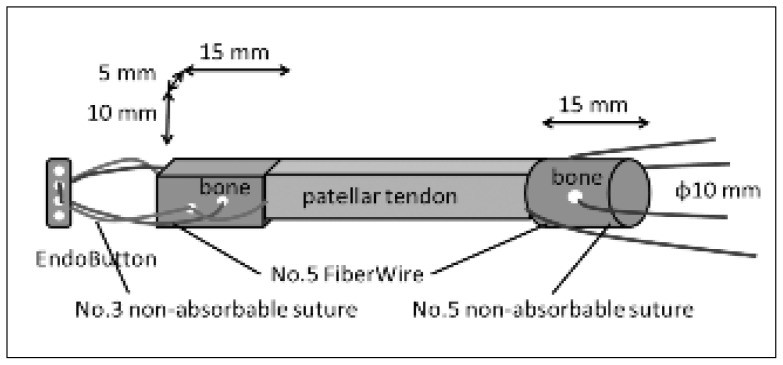
ACL reconstruction with BPTB was performed arthroscopically using a 3D fluoroscopy-based navigation system to create the rectangular femoral sockets, as described previously (13, 14). Autologous BPTB grafts were 10 mm in width and harvested with bone plugs at both ends from the central portion of the patellar tendon. The femoral bone plug for a rectangular socket was typically 5 × 10 × 15 mm as described by Shino et al. (15). It was connected to an EB (Smith & Nephew Endoscopy, Andover, MA, USA) using No. 5 Fiber Wire (Arthrex, Inc., Naples, FL, USA) and No. 3 non-absorbable suture (Fig. 1). The femoral insertion site for the rectangular socket was determined by monitoring the bony landmarks (i.e., the lateral intercondylar ridge and the lateral bifurcate ridge) both by arthroscopic view and on the navigation screen (Stealth Station TRIA™ plus, Medtronic, Louisville, CO, USA) (16, 17). The priority, in creating the femoral socket, was to position the femoral socket aperture within the femoral footprint of the ACL. Two parallel guidewires for the femoral socket were then placed and were overdrilled for an appropriate length using a 5-mm cannulated drill through a far anteromedial portal (18). The two sockets were interconnected using a dilator (Smith & Nephew) and the lateral femoral cortex was drilled through the center of the two sockets using an EB drill (Smith & Nephew Endoscopy). On the tibial side, a guidewire was positioned at the center of the tibial footprint of the ACL and overdrilled 25–35 mm. Then, two parallel guidewires were inserted just anterior and posterior to the guidewire which had been inserted previously using a parallel guide (Smith & Nephew). They were overdrilled the full length using a cannulated drill, and the two tunnels were interconnected using a dilator (Smith & Nephew Endoscopy). The tibial insertion site was arthroscopically determined in reference to the ACL remnant, posterior cruciate ligament, medial tibial eminence, intermeniscal ligament, and anterior horn of the lateral meniscus (19). After creating a femoral socket and tibial tunnel, the graft was passed through, and the EB loop was flipped outside of the femoral cortex in the usual manner. The bone plug was set far enough into the femoral socket so that the ligament end of the graft was inset 1 mm into the femoral socket to avoid protrusion of the bone plug from the femoral socket. Tibial fixation of the BPTB graft was accomplished over a suture-post fixation with a fully threaded 6.5-mm cancellous screw and washer (Meira Corp., Nagoya, Japan). The BPTB graft was fixed at full knee extension.
Fig. 1.
Scheme of bone-patellar tendon-bone graft.
The knee was not immobilized, but was protected for five weeks with a functional brace. Active and assisted range of motion exercises were initiated immediately after the surgery. Partial weight-bearing was allowed two days after surgery and full weight-bearing at one week. Running was allowed at four months, followed by return to previous sporting activity at an average of eight to nine months after surgery.
Outcome measurements
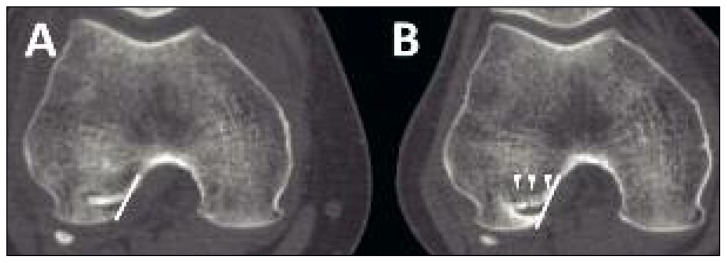
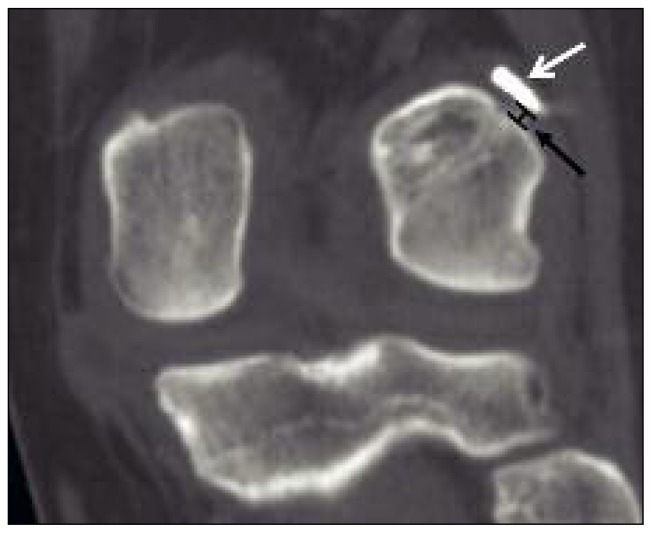
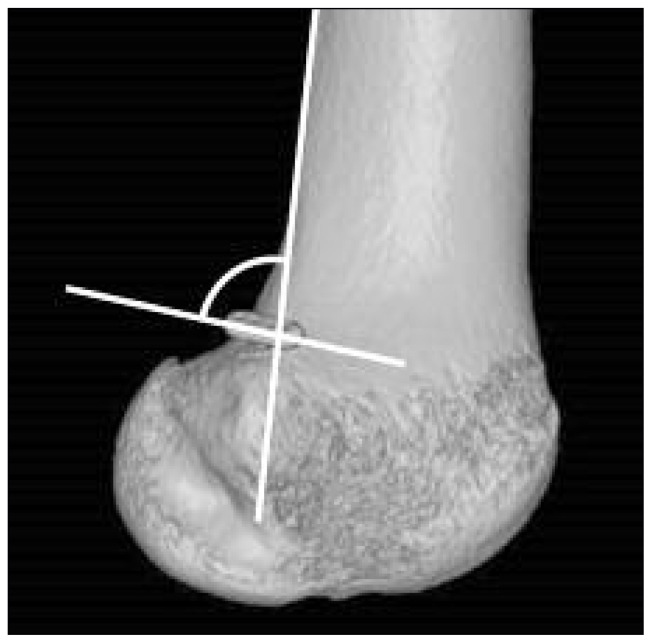
Bone integration was considered to be achieved when trabecular continuity without any gap between the bone plug and femoral bone socket was observed on at least three consecutive axial CT images (Fig. 2A). Two orthopedic surgeons evaluated the bone integration. Migration of the bone plug was measured on axial CT images. The shortest distance between the bone plug and the femoral socket aperture was measured, and the distance on the identical image at one year after surgery was compared with that at one week postoperatively (Fig. 2B). Bone plug migration was considered to have occurred when the bone plug end had moved more than 1 mm on the axial view postoperatively. EB migration and EB rotation were measured on CT images using the method described by Mae et al. (20). The shortest distance between the lateral femoral cortex and EB was measured on coronal CT images, and the distance on the identical image at one year after surgery was compared with that at one week postoperatively. Positive soft tissue interposition was considered present when there was a distance of more than 1 mm between the lateral femoral cortex and EB on the coronal CT image, and EB migration was considered present when the EB had moved more than 1 mm on the coronal view (Fig. 3). An angle formed by the posterior cortex and the long axis of EB was measured on the 3D reconstructed CT model. EB rotation was considered to have occurred when the EB had rotated by more than 5°, between one week and one year postoperatively (Fig. 4). An orthopedic surgeon evaluated bone plug migration, soft tissue interposition, EB migration and EB rotation.
Fig. 2.
Measurement on axial CT image.
The shortest distance between the bone plug end and the femoral socket aperture (white line) was measured on an axial computed tomography (CT) image taken one week after surgery (A) and one year after surgery (B). Bone integration was considered to be achieved when there was presence of trabecular continuity without any gap between the bone plug and femoral bone socket (white arrows) on axial CT images.
Fig. 3.
Measurement on coronal CT image.
The shortest distance between the lateral femoral cortex and the EndoButton was measured on a coronal computed tomography image (Black arrow). White arrow shows the one.
Fig. 4.
Measurement on 3D CT bone model.
An angle formed by the posterior cortex and the long axis of the EndoButton was measured on a 3D reconstructed computed tomography model.
A 3D CT scan of the operated knee was performed one week and one year after surgery in all patients, using a helical high-speed Aquilion 64™ 64 or Aquilion ONE™ (Toshiba Medical Systems Corp., Tokyo, Japan) CT machine. The axial images were obtained at 0.5-mm intervals. The ZIOSTATION software package (Ziosoft Inc., Tokyo, Japan) was used for coronal and 3D reconstruction of the operated knee. The coronal images were reconstructed at 2-mm intervals and a 3D bone model was also reconstructed. The tibia and the patella were removed from the 3D model. A true lateral view of the femur was established by superimposing the posterior aspects of the femoral condyles. Measurement of EB rotation was done on the surface of the lateral view of the 3D femoral model.
Clinical assessment was performed one year after surgery, which corresponded to the time period of CT assessment. All patients were subjectively evaluated using the Lysholm score. Anterior knee stability was quantitatively assessed using a KT-2000 arthrometer (MEDmetric Corp. San Diego, CA, USA).
Reconstructed and contralateral knees were measured with a 134-N anterior force applied to the proximal tibia at 20° of knee flexion. The side-to-side difference in anterior translation was used as a representative indicator of restored knee stability. The pivot shift test was graded as negative, glide, clunk or gross to determine rotational stability. The range of motion of both knees was also evaluated. Complications associated with EB use were also recorded.
Data analysis
Statistical analysis was performed using the EXCEL statistics 2012 software package for Microsoft Windows (SSRI Co., Ltd., Tokyo, Japan) and the Statistics for Microsoft Windows: the intraclass correlation coefficient (Vector Inc., Tokyo, Japan). Fisher’s exact test was used to evaluate the relationship between two out of four variables on CT: bone plug migration, EB migration, EB rotation, or soft tissue interposition. A Student’s t-test was used to analyze the clinical results according to the four variables on CT. The statistical significance level was set at p < 0.05. Inter-observer reliability for the evaluation of bone integration was assessed with Kappa statistics. Absolute agreement was observed for this variable (k coefficient = 1). Intra-observer reliability for the radiographic parameters was represented by intraclass correlation coefficients (ICCs). A period of four weeks elapsed between test and retest measurements. The ICCs in the pilot study of 10 cases, who were extracted from this case series, were 0.973 for distance measurement on CT and 0.952 for angle measurement on CT. Data in the text are expressed as means ± standard deviations (SDs) or as the incidence.
Results
CT evaluation
Bone integration was achieved in all cases one year after surgery. Bone plug migration was observed in 5 cases (15%) with a mean difference between the two time points (1 week and 1 year after surgery) of 0.4 ± 0.4 mm. Positive soft tissue interposition was observed in five cases (15%). EB migration and rotation were observed in 3 cases (9%) and 19 cases (56%), respectively, with a mean difference between the two time points of 0.4 ± 0.5 mm and 14° ± 15°, respectively (Tab. 2). There was no statistical relationship between any pair of the four variables on CT (Tab. 3).
Table 2.
Results of radiographic evaluation.
| Cases (%) | Mean difference | |
|---|---|---|
| Bone integration | 34 (100%) | |
| Bone plug migration | 5 (15%) | 0.4 ± 0.4 mm |
| Soft tissue interposition | 5 (15%) | 0.5 ± 0.5 mm |
| EndoButton migration | 3 (9%) | 0.4 ± 0.5 mm |
| EndoButton rotation | 19 (56%) | 14.1 ± 15.0° |
Data are given as means ± standard deviations or incidence.
Table 3.
Statistical relations between each phenomenon on CT.
| Bone plug migration | Soft tissue interposition | EndoButton migration | EndoButton rotation | |
|---|---|---|---|---|
| Bone plug migration | – | p = 1.00 | p = 0.39 | p = 0.35 |
| Soft tissue interposition | – | p = 1.00 | p = 1.00 | |
| EndoButton migration | – | p = 1.00 |
Clinical evaluation
The postoperative mean Lysholm score was 97.1 ± 5.0 points. The postoperative side-to-side difference in anterior translation measured with the KT-2000 arthrometer averaged 0.5 ± 1.3 mm. The postoperative pivot shift test was graded as negative in all cases. With respect to the range of motion of the knee, we observed no loss of extension or loss of flexion of more than 5 degrees compared with the contralateral knee. The KT side-to-side difference at one year was unaffected by any variables (bone plug migration, EB migration, EB rotation or soft tissue interposition) (Tab. 4). There were no complications, such as painful irritation, associated with EB use.
Table 4.
Relations between the KT side-to-side difference and CT evaluation.
| Positive | Negative | p value | |
|---|---|---|---|
| Bone plug migration | 1.0 ± 1.8 mm | 0.5 ± 1.2 mm | 0.43 |
| Soft tissue interposition | 1.0 ± 0.9 mm | 0.4 ± 1.4 mm | 0.39 |
| EndoButton migration | 0.0 ± 0.0 mm | 0.6 ± 1.3 mm | NA* |
| EndoButton rotation | 0.6 ± 1.3 mm | 0.5 ± 1.4 mm | 0.84 |
Data are given as means ± standard deviations.
NA: not available (p value could not be calculated, because the data of positive EndoButton migration did not have deviations).
Discussion
In all the cases in the current study, the bone plug was integrated onto the femoral socket following anatomical rectangular tunnel ACL reconstruction with BPTB graft using EB for femoral fixation. In addition, the incidence of bone plug migration was low and the mean distance of bone plug migration was short. Moreover, the current procedure provided satisfactory short-term clinical outcomes without complications associated with EB use. On the basis of these results, the EB can be considered a reliable fixation device for femoral fixation in rectangular tunnel ACL reconstruction with BPTB graft.
Short bone plug migration, as observed in the current study, did not affect postoperative knee stability. However, bone plug migration can result in loss of initial tension of the graft. Consequently, bone plug migration must be avoided. To avoid bone plug migration due to a breakage of the bone plug and detachment of thread, we not only threaded a hole created on the bone plug but also hooked an additional blade on the bone-tendon junction (Fig. 1). To avoid knot unraveling which can result in bone plug migration, it was also important to tie the knot tightly. We introduced a 5-throw square knot for sutures used to connect EB to the bone plug, and this may have contributed to the positive results in this study.
Mae et al. studied, on plain radiographs, migration of EB after anatomical double-bundle ACL reconstruction using hamstring tendon grafts (20). They reported that tissue interposition between EB and femoral cortex was found in 25.2% of EBs immediately after surgery; they also reported that EBs with tissue interposition migrated more frequently than those without. Soft tissue interposition affected by other variables, such as bone plug migration, EB migration or EB rotation, was not observed on CT. The small number of patients included have been the reason why no statistical relationship was obtained for these processes, in the present study. We did not find that tissue interposition or migration of EB affected the clinical outcomes. Similarly, no statistical relationship between any variables on CT and the KT side-to-side difference was found in our study. Our results showed that 9% of EBs had migrated after one year, while Mae et al. found that 35.1% of EBs showed migration during the same time period. There are several possible reasons why the incidence of EB migration in ACL reconstruction with BPTB graft was comparatively lower than that in double-bundle ACL reconstruction with hamstring tendon graft. First, the friction between the bone plug and the bone socket seemed to be high compared to that between the soft tissue and the bone socket; therefore, the BPTB graft was not as movable as the soft tissue graft. Moreover, the bone plug must be harder to move in a rectangular socket than in a cylindrical socket. Second, in ACL reconstruction with BPTB graft, bone-to-graft healing should be achieved faster and more securely compared with that achieved in ACL reconstruction with a soft tissue graft, and this would result in shorter graft or EB migration. Finally, the results could be affected by the timing of the first CT. We performed the first CT one week after surgery. Mae et al. found that more than half of the migrated EBs had moved within the first week postoperatively. Therefore, there was the possibility that EB migration or bone plug migration occurring immediately after surgery could not be detected in the current study; this may a reason for the low incidence.
In the current study, the bone plug was integrated in the femoral socket in all cases a year after surgery. The time period for graft-socket integration in ACL reconstruction with BPTB graft using a suspensory button as femoral fixation is uncertain. Suzuki et al. reported that bone plug-femoral tunnel integration was almost complete by eight weeks after rectangular tunnel ACL reconstruction with BPTB graft using an interference screw as a femoral fixation device (21). By contrast, Lomasney et al. reported that bone plug-tibial tunnel integration was obtained in only 34.5% of cases at five months postoperatively after conventional round tunnel ACL reconstruction with BPTB allograft using a bioabsorbable interference screw (22). Future studies are needed to investigate the time period for graft-socket integration using the procedure described in this study.
In the current study, no complications related to the use of a suspensory button for femoral fixation were observed, whereas serious complications associated with interference screw femoral fixation have been reported (3–5), as previously mentioned. Surgeons should be aware of potential complications related to suspensory button fixation, including tunnel enlargement, button migration, symptomatic extensor mechanism or iliotibial band irritation, and intratunnel fixation (20, 23–26). Although the incidence of EB migration or bone plug migration was low, considering that more than half of EBs were rotated, micro-motion of the bone plug in the femoral socket must occur. This phenomenon can result in tunnel widening after ACL reconstruction, even when using BPTB graft (27). Although aperture fixation with an interference screw should, in theory, decrease the micro-motion of the bone plug, it is unknown whether aperture fixation prevents tunnel widening after anatomical ACL reconstruction with BTPB graft compared to suspensory fixation. In the future, a study aiming to clarify whether any type of fixation device affects bone plug-socket integration, the clinical result, tunnel widening or complications associated with the fixation device in a newly-developed rectangular ACL reconstruction with BPTB graft is warranted. There were several limitations to this study. First, this was a retrospective study without a comparison group using an interference screw. Second, the current study involved a small number of patients. If the study had involved a large number of patients, statistical differences might have been found. Third, the study did not evaluate bone integration onto the tibial tunnel or bone plug migration in it. Although the femoral fixation method may affect these endpoints, we focused on the femoral side in this study. Fourth, tunnel widening after ACL reconstruction, which is one of the complications associated with suspensory fixation, was not evaluated in the current study. Finally, CT images at only two time points were available in this study. Therefore, as previously stated, there was the possibility that EB migration or bone plug migration that occurred immediately after surgery could not be detected.
In conclusion, the bone plug was integrated onto the femoral socket in all cases following anatomical rectangular tunnel ACL reconstruction with BPTB graft using EB for femoral fixation. Although micro-motion of the bone plug in the femoral socket was suspected, the incidence of bone plug and EB migration was low and there was a satisfactory short-term clinical outcome. The EB is considered to be a reliable fixation device for femoral fixation in the current procedure.
References
- 1.Kurosaka M, Yoshiya S, Andrish JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15:225–229. doi: 10.1177/036354658701500306. [DOI] [PubMed] [Google Scholar]
- 2.Brucker PU, Lorenz S, Imhoff AB. Aperture fixation in arthroscopic anterior cruciate ligament double-bundle reconstruction. Arthroscopy. 2006;22:1250.e1–6. doi: 10.1016/j.arthro.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 3.Konan S, Haddad FS. Femoral fracture following knee ligament reconstruction surgery due to an unpredictable complication of bioabsorbable screw fixation: a case report and review of literature. J Orthop Traumatol. 2010;11:51–55. doi: 10.1007/s10195-009-0079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthews LS, Soffer SR. Pitfalls in the use of interference screws for anterior cruciate ligament reconstruction: brief report. Arthroscopy. 1989;5:225–226. doi: 10.1016/0749-8063(89)90177-1. [DOI] [PubMed] [Google Scholar]
- 5.Resinger C, Vécsei V, Heinz T, et al. The removal of a dislocated femoral interference screw through a posteromedial portal. Arthroscopy. 2005;21:1398. doi: 10.1016/j.arthro.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 6.Muneta T, Sekiya I, Yagishita K, et al. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy. 1999;15:618–624. doi: 10.1053/ar.1999.v15.0150611. [DOI] [PubMed] [Google Scholar]
- 7.Fu FH, Shen W, Starman JS, et al. Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med. 2008;36:1263–1274. doi: 10.1177/0363546508314428. [DOI] [PubMed] [Google Scholar]
- 8.Brown CH, Jr, Wilson DR, Hecker AT, et al. Graft-bone motion and tensile properties of hamstring and patellar tendon anterior cruciate ligament femoral graft fixation under cyclic loading. Arthroscopy. 2004;20:922–935. doi: 10.1016/j.arthro.2004.06.032. [DOI] [PubMed] [Google Scholar]
- 9.Kousa P, Järvinen TL, Vihavainen M, et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med. 2003;31:174–181. doi: 10.1177/03635465030310020401. [DOI] [PubMed] [Google Scholar]
- 10.Höher J, Livesay GA, Ma CB, et al. Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc. 1999;7:215–219. doi: 10.1007/s001670050151. [DOI] [PubMed] [Google Scholar]
- 11.O’Brien SJ, Warren RF, Pavlov H, et al. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am. 1991;73:278–286. [PubMed] [Google Scholar]
- 12.Shino K, Nakata K, Nakamura N, et al. Anatomically oriented anterior cruciate ligament reconstruction with a bone-patellar tendon-bone graft via rectangular socket and tunnel: a snug-fit and impingement-free grafting technique. Arthroscopy. 2005;21:1402. doi: 10.1016/j.arthro.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 13.Nakagawa T, Takeda H, Nakajima K, et al. Intraoperative 3-dimensional imaging-based navigation-assisted anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:1161–1167. doi: 10.1016/j.arthro.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 14.Taketomi S, Inui H, Nakamura K, et al. Clinical outcome of anatomic double-bundle ACL reconstruction and 3D CT model-based validation of femoral socket aperture position. Knee Surg Sports Traumatol Arthrosc. 2014;22:2194–2201. doi: 10.1007/s00167-013-2663-0. [DOI] [PubMed] [Google Scholar]
- 15.Shino K, Nakata K, Nakamura N, et al. Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft to mimic natural fiber arrangement. Arthroscopy. 2008;24:1178–1183. doi: 10.1016/j.arthro.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 16.Ferretti M, Ekdahl M, Shen W, et al. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23:1218–1225. doi: 10.1016/j.arthro.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Fu FH, Jordan SS. The lateral intercondylar ridge--a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2007;89:2103–2104. doi: 10.2106/JBJS.G.00851. [DOI] [PubMed] [Google Scholar]
- 18.Shino K, Horibe S, Hamada M, et al. Allograft anterior cruciate ligament reconstruction. Techniques in Knee Surgery. 2002;1:78–85. [Google Scholar]
- 19.Ferretti M, Doca D, Ingham SM, et al. Bony and soft tissue landmarks of the ACL tibial insertion site: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2012;20:62–68. doi: 10.1007/s00167-011-1592-z. [DOI] [PubMed] [Google Scholar]
- 20.Mae T, Kuroda S, Matsumoto N, et al. Migration of EndoButton after anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1528–1535. doi: 10.1016/j.arthro.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 21.Suzuki T, Shino K, Nakagawa S, et al. Early integration of a bone plug in the femoral tunnel in rectangular tunnel ACL reconstruction with a bone-patellar tendon-bone graft: a prospective computed tomography analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(Suppl 1):S29–35. doi: 10.1007/s00167-011-1481-5. [DOI] [PubMed] [Google Scholar]
- 22.Lomasney LM, Tonino PM, Coan MR. Evaluation of bone incorporation of patellar tendon autografts and allografts for ACL reconstruction using CT. Orthopedics. 2007;30:152–157. doi: 10.3928/01477447-20070201-06. [DOI] [PubMed] [Google Scholar]
- 23.Karaoglu S, Halici M, Baktir A. An unidentified pitfall of Endobutton use: case report. Knee Surg Sports Traumatol Arthrosc. 2002;10:247–249. doi: 10.1007/s00167-002-0287-x. [DOI] [PubMed] [Google Scholar]
- 24.Muneta T, Yagishita K, Kurihara Y, et al. Intra-articular detachment of the Endobutton more than 18 months after anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:775–778. doi: 10.1016/s0749-8063(99)70013-7. [DOI] [PubMed] [Google Scholar]
- 25.Petit C, Millett PJ. Arthroscopic removal of EndoButton after anterior cruciate ligament reconstruction: case report and surgical technique. Am J Orthop (Belle Mead NJ) 2008;37:618–620. [PubMed] [Google Scholar]
- 26.Taketomi S, Inui H, Hirota J, et al. Iliotibial band irritation caused by the EndoButton after anatomic double-bundle anterior cruciate ligament reconstruction: report of two cases. Knee. 2013;20:291–294. doi: 10.1016/j.knee.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 27.Taketomi S, Inui H, Sanada T, et al. Eccentric femoral tunnel widening in anatomic anterior cruciate ligament reconstruction. Arthroscopy. 2014;30:701–709. doi: 10.1016/j.arthro.2014.02.016. [DOI] [PubMed] [Google Scholar]