Abstract
Chronic inflammation has a decisive role in tumorigenesis, particularly in gastric carcinogenesis. The CC chemokine ligand 2 (CCL2), an important inflammatory cytokine, is involved in the initiation, development and progression of various types of cancer. However, the role of CCL2 in gastric cancer remains to be elucidated. The present study demonstrated that recombinant CCL2 stimulation caused no effect on the morphology, proliferation and migration of human GES-1 gastric mucosa epithelial cells, in which the protein expression of CC-chemokine receptor 2 (CCR2) was markedly low. However, the expression of CCR2 was significantly upregulated in the GES-1 cells following pretreatment with the chemical carcinogen, N-methyl-N-nitro-N′-nitrosoguanidine (MNNG), for 12 h or transformed with MNNG (MC cells). The present study used CCL2 to stimulate MNNG pretreated GES-1 cells and MC cells, and demonstrated that CCL2 clearly promoted their migration and the epithelial-mesenchymal transition (EMT). However, no effect was observed on the proliferative ability of the cells. Taken together, these findings suggested that the CCL2/CCR2 chemokine signaling may regulate the EMT in gastric epithelial cells and resulted in gastric carcinogenesis in response to the intake of the carcinogen, MNNG.
Keywords: N-methyl-N-nitro-N′-nitrosoguanidine, CC chemokine ligand 2, gastric epithelial cells, migration, epithelial-mesenchymal transition
Introduction
Accumulating evidence supports that various types of cancer are triggered by infection and chronic inflammatory disease (1), and gastric cancer is a classical model of inflammation-associated cancer. Chronic inflammation actuates cellular events, which prompt malignant transformation of cells and even carcinogenesis (2). Previous studies have confirmed that inflammatory cytokines are significant in the oncogenesis of gastric cancer (3,4). In addition, a number of previous studies have suggested that polymorphisms in pro-inflammatory cytokine genes, including IL-1β, IL-6, CC chemokine ligand (CCL)2, IL-8, CCL5 and PDGF, are associated with cancer (5–8).
CCL2 is a member of the CC chemokine family, which predominantly binds with high affinity to the CC-chemokine receptor 2 (CCR2). CCL2 is a critical modulator of inflammation and is produced by a variety of cell types, including fibroblast cells, epithelial cells, mononuclear cells, astrocytes and certain tumor cells (9). Previous studies have reported that CCL2 is widely detected in several types of cancer and is important in cancer progression. In prostate cancer, CCL2 mediates the interactions between normal and malignant cells in the tumor microenvironment and promotes prostate cancer tumorigenesis and metastasis (10). A CCL2/reactive oxygen species autoregulation loop increases the growth of oral squamous cell carcinoma (11). In addition, in colon and breast cancers, CCL2 enhances endothelial cell activities in angiogenesis and metastasis (12). Rokavec et al (13) revealed that recombinant CCL2 (MCP-1) alone was sufficient to transform mammary epithelial cells and develop tumors. Notably, the expression of CCL2 has been demonstrated to be high in gastric cancer tissue and the peripheral blood of patients with gastric cancer (14,15). Whether CCL2 is involved in gastric carcinogenesis remains to be elucidated.
A number of factors contribute to the initiation and development of gastric cancer. Diet, smoking, obesity and chronic infections are all major factors, which are involved in the occurrence and development of cancer (16,17). The intake of salted foods, containing high levels of N-nitroso compounds (NOCs), which are powerful carcinogens, is a critical component of the carcinogenesis of gastric cancer (18). N-methyl-N-nitro-N′-nitrosoguanidine (MNNG) is one of the most active carcinogenic NOCs and has been used to establish stomach carcinomas successfully in animal models (19). Human GES-1 gastric mucosa epithelial cells can be transformed by MNNG into the precancerous cell model, termed MC cells, which are widely used to investigate the mechanism underlying gastric carcinogenesis (20).
In the present study, parental GES-1 cells and MNNG-pretreated GES-1 or MC cells were stimulated with CCL2. It was demonstrated that the expression of CCR2 was markedly low and CCL2 revealed no effect on the parental GES-1 cells. However, following pretreatment or transformation into MC cells by MNNG, the expression of CCR2 in the GES-1 cells was significantly increased. CCL2 promoted the migration of MNNG-pretreated GES-1 cells and MC cells through the induction of the epithelial-mesenchymal transition (EMT).
Materials and methods
Cell culture
The U937 and human gastric epithelial GES-1 cell lines were purchased from the Institute of Biochemistry and Cell Biology at the Chinese Academy of Sciences (Shanghai, China). The GES-1 cell line was transformed into an MC cell line using MNNG, as follows: MNNG (Sigma-Aldrich, St. Louis, MO, USA) was dissolved in dimethyl sulfoxide (Sigma-Aldrich) at a concentration of 0.2 mol/l and the GES-1 cells were induced with 2×10−5 mol/l MNNG for 24 h in the dark. Following the removal of MNNG, normal RPMI-1640 medium (Invitrogen Life Technologies, Carlsbad, CA, USA) was used to culture the cells and was changed every 3 days. During the following week, some of the cells initially died and subsequently the surviving cells grew out. The cells were cultured in RPMI-1640 medium, supplemented with 10% fetal bovine serum (FBS; Invitrogen Life Technologies) and were maintained at 37°C in a humidified chamber with 5% CO2.
Cell colony formation assay
The cells were collected and seeded into 6-well plates (1,000 cells/well) in growth medium in the presence or absence of CCL2 (10 ng/ml; R&D systems, Minneapolis, MN, USA). The cultures were grown for 10 days at 37°C in a humidified incubator and the growth medium was changed every 3 days. The colonies were fixed with 99.5% methanol for 30 min at room temperature and visualized by staining with 1% crystal violet solution (Beijing Airan Bio-Engineering Co., Ltd., Beijing, China) for 15 min on the indicated day. The cell colonies were counted for statistical analysis following images being captured (SX240 HS; Canon, Tokyo, Japan).
Transwell migration assay
The control cells or pretreated cells (1×105 in 200 µl) suspended in serum-free medium were seeded into the upper compartment of transwell chambers with 8 µm pore filters (Corning, Inc., Corning, NY, USA). Complete medium, containing 10% FBS (600 µl), with or without CCL2 (10 ng/ml) was added into the lower chamber as a chemoattractant. Following 10 h of incubation at 37°C, the insert was washed with phosphate-buffered saline (PBS) and the non-migrated cells in the top chamber were mechanically removed with cotton swabs. The cells migrating through the membrane were fixed with 99.5% methanol and stained with 1% crystal violet. The number of migrated cells were quantified manually under an inverted microscope (TI-TS100W; Nikon, Tokyo, Japan).
Western blotting
The cells were harvested and lysed with radioimmunoprecipitation buffer [Vazyme Biotech (Nanjing) Co., Ltd., Nanjing, China], supplemented with protease inhibitors. Equal quantities (150 µg) of individual proteins were prepared for electrophoresis on 8–12% SDS-PAGE gels (Biolink, Beijing, China) and were subsequently transferred onto polyvinylidene fluoride membranes (EMD Millipore, Billerica, MA, USA). Following blocking with 5% non-fat milk in Tris-buffered saline, containing 0.05% Tween-20 (TBST), for 1 h, the membranes were incubated with the appropriate dilutions of specific monoclonal antibodies overnight at 4°C. The following monoclonal antibodies were used: Rabbit monoclonal anti-E-cadherin (1:500; sc-7870; Santa Cruz Biotechnology, Inc., Dallas, TX, USA), rabbit monoclonal anti-N-cadherin (1:1,000; BS2224; Bioworld Technology, Louis Park, MN, USA), rabbit monoclonal anti-CCR2 (1:500; 2068–1; Wuhan Boster Bio-Engineering Co., Ltd., Wuhan, China) and mouse monoclonal anti-GAPDH (1:2,000; CW0100A; Kangcheng, Shanghai, China). Following washing with TBST, the membranes were incubated with the following secondary antibodies for 1 h: Horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G (IgG; 1:2,000; sc-2301) and anti-mouse IgG (1:2000; sc-358923) (Santa Cruz Biotechnology, Inc.). The protein bands were visualized by enhanced chemiluminescence, according to the manufacturer's instructions (EMD Millipore). GAPDH was used as a loading control.
Immunofluorescence staining
The cells (2×104) were seeded into a 24-well dish for 24 h and were subsequently washed with PBS twice, fixed with 4% paraformaldehyde for 2 h, permeabilized with 0.1% Triton X-100 for 10 min, blocked with 5% bovine serum albumin for 20 min (Wuhan Boster Bio-Engineering Co., Ltd.) and incubated with the primary antibodies overnight at 4°C. The primary antibodies were rabbit monoclonal anti-CCR2 (1:100; 2068–1; Wuhan Boster Bio-Engineering Co., Ltd.), rabbit monoclonal anti-E-cadherin (1:100; 21473; Signalway Antibody, College Park, MD, USA) and rabbit monoclonal anti-N-cadherin (1:200; BS2224; Bioworld Technology, Minneapolis, MN, USA). Following washing with PBS, the cells were incubated with fluorescein isothiocyanate-labeled donkey anti-rabbit IgG secondary antibody (1:500; A31572; Invitrogen Life Technologies) at 37°C. The nuclei were subsequently counterstained with Hoechst (1:200; Invitrogen Life Technologies) and all samples were imaged using a confocal immunofluorescence microscope (TI-TS100W; Nikon) at the same exposure times.
Statistical analysis
All statistical analyses were performed using of SPSS 16.0 software (SPSS Inc., Chicago, IL, USA). The data are presented as the mean ± standard deviation. Student's t-test was used for two-group comparisons. Each experiment was performed independently at least three times with similar results. P<0.05 was considered to indicate a statistically significant difference.
Results
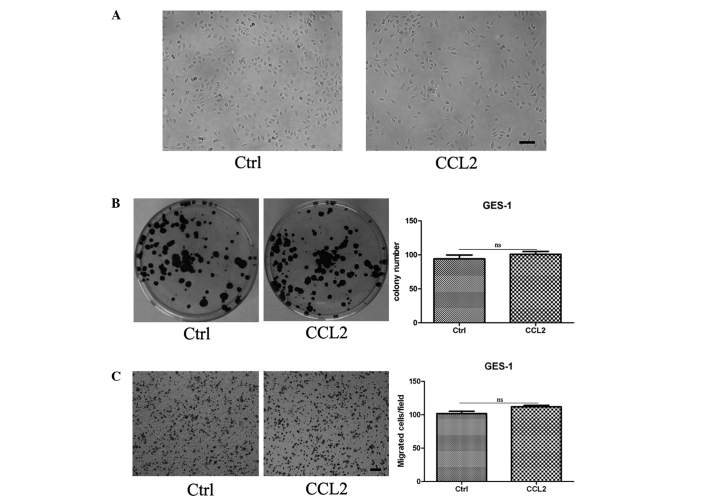
CCL2 has no effect on the morphology, proliferation and migration of GES-1 cells
To investigate the role of CCL2 in gastric carcinogenesis, GES-1, a human gastric epithelial cell line, was continuously pretreated with human recombinant CCL2 (10 ng/ml) for 9 days and collected for cell biology analysis. It was revealed that the cell morphology of the GES-1 cells pretreated with CCL2 was similar to the control group (Fig. 1A). A cell colony formation assay revealed no difference in the number and size of the cell colonies between the control group and the treated group (Fig. 1B). Transwell migration analysis revealed that the migration capacity of the GES-1 cells in the treated group was no different compared with the control group (Fig. 1C).
Figure 1.
CCL2 revealed no direct effect on the morphology, proliferation and migration of the GES-1 cells. Following persistent pretreatment with CCL2 for 9 days, the GES-1 cells were digested and collected for analysis. (A) Representative images of the cells (magnification, ×100; scale bar, 100 µm). (B) Representative images of the cell colony formation assay and the quantification of colony number. (C) Representative images of the Transwell migration assay (magnification, ×100; scale bar, 100 µm) and the quantification of the numbers of migrated cells. *P<0.05. Ctrl, GES-1 cells; CCL2, GES-1 cells treated with CC chemokine ligand 2 for 9 days; ns, non-significant.
To further investigate the direct effects of CCL2 on GES-1, a cell colony formation assay was performed for GES-1 cells in the presence or absence of CCL2. The results revealed that CCL2 had no effect on GES-1 (data not shown). The chemokine, CCL2, is best known for its chemotactic functions, whereas no differences were observed in the motility of gastric epithelial cells incubated with or without CCL2 in the lower chamber (data not shown). Therefore, CCL2 stimulation had no effect on the morphology, proliferation and migration of gastric epithelial cells.
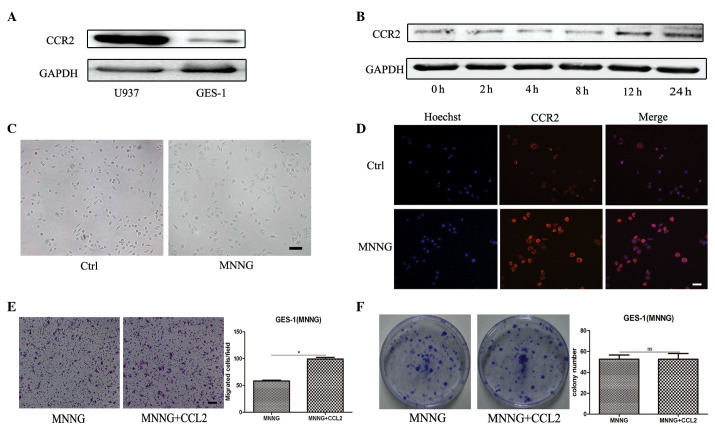
MNNG induces the expression of CCR2 in gastric epithelial cells
CCL2 signals primarily through the chemokine receptor, CCR2. It was hypothesized that GES-1 cells failed to respond to CCL2 as a result of a lack of CCR2. To confirm this hypothesis, the protein expression of CCR2 was determined in GES-1 cells by western blotting, using human U937 monocytes as the positive control. As shown in Fig. 2A, GES-1 demonstrated a considerably low expression of CCR2.
Figure 2.
Pretreatment with MNNG induces the expression of CCR2 in GES-1 cells. (A) Western blotting was performed to determine the protein expression of CCR2 in U937 and GES-1 cells. (B) Western blotting was performed to determine the protein expression of CCR2 in GES-1 cells treated with MNNG for 0, 2, 4, 8, 12 and 24 h. (C) Representative images of cells (magnification, ×100; scale bar, 100 µm). (D) Immunofluorescence staining of CCR2 was performed to determine the expression levels of CCR2 (magnification, ×200; scale bar, 50 µm). (E) A Transwell assay was performed to determine the migration capability of the cells. The cells were seeded onto the top of the upper chamber and the number of cells that migrated through the uncoated filter in response to CCL2 in the lower chamber was quantified (magnification, ×100; scale bar, 100 µm; *P<0.05). (F) A cell colony formation assay of the MNNG-pretreated GES-1 cells cultured alone or in the presence of CCL2 (*P<0.05). Ctrl, GES-1 cells; CCL2, CC chemokine ligand 2; ns, non-significant; MNNG, cells treated for 12 h with N-methyl-N-nitro-N′-nitrosoguanidine.
The cell model was changed and 1×10−5 mol/l of MNNG was used to pretreat the GES-1 cells for varying durations. To determine whether the expression of CCR2 in GES-1 cells was altered following exposure to MNNG, the duration-dependent effects of MNNG on the expression of CCR2 in GES-1 cells were investigated. Western blotting revealed that the expression of CCR2 was significantly increased in the GES-1 cells following treatment with MNNG for 12 and 24 h (Fig. 2B). Therefore, the present study focused on GES-1 pretreatment with MNNG for 12 h. The morphology of the GES-1 cells treated with MNNG exhibited more unclear cell edges and were flatter and bigger compared with the parental GES-1 cells (Fig. 2C). Immunofluorescence staining revealed that MNNG treatment significantly increased the fluorescence intensity of CCR2, which was consistent with the upregulation of CCR2 observed by immunoblotting (Fig. 2D). A Transwell migration assay demonstrated that CCL2 significantly induced the chemotaxis of the GES-1 cells pretreated with MNNG in vitro (Fig. 2E). However, the cell colony formation ability of the GES-1 cells was not affected by MNNG (Fig. 2F). These results indicated that MNNG induced the expression of CCR2 in GES-1 cells and the migration of GES-1 cells in response to CCL2.
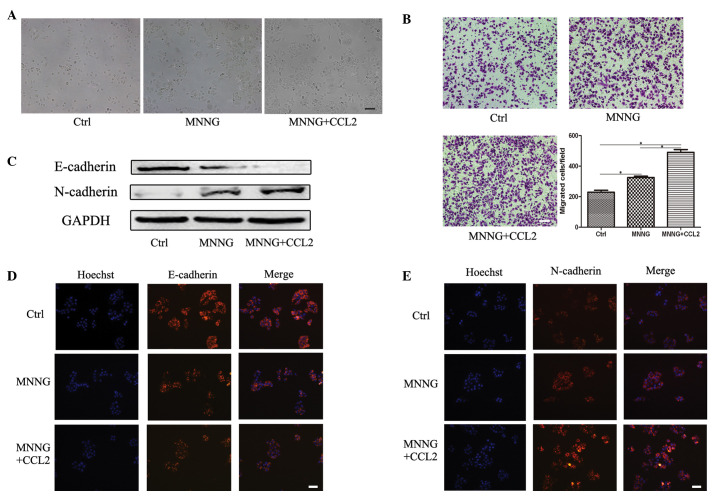
CCL2 induces the EMT of MNNG-pretreated GES-1 cells
Since treatment with MNNG induced the expression of CCR2 in GES-1 cells, whether MNNG treatment enhanced the role of CCL2 in GES-1 cells was assessed. Three experimental groups, including the parental GES-1 group, the MNNG-pretreated GES-1 group and the MNNG-pretreated GES-1 stimulated by CCL2 group, were used. As shown in Fig. 3A, the cells in the CCL2 treatment group exhibited a fibroblastic spindle-shaped morphology and were marginally more slender and longer compared with the cells in the MNNG-pretreated group. Treatment of MNNG-pretreated GES-1 cells with CCL2 for 9 days resulted in significant cell migration over 12 h, as determined by a Transwell migration assay (Fig. 3B). Western blotting revealed that CCL2 treatment notably decreased the expression of the epithelial cell marker, E-cadherin, and increased the expression of the mesenchymal cell marker, N-cadherin, in the MNNG-pretreated GES-1 cells (Fig. 3C). To confirm these results, immunofluorescence staining was performed to detect the expression of N-cadherin and E-cadherin. Consistent with the western blot analysis, CCL2 downregulated the expression of E-cadherin and upregulated the expression of N-cadherin in the MNNG-pretreated GES-1 cells (Fig. 3D and E). Taken together, CCL2 enhanced the migration capacity of the MNNG-pretreated GES-1 cells and prompted their EMT.
Figure 3.
CCL2 promotes the EMT in MNNG-pretreated GES-1 cells. The GES-1 cells were pretreated with MNNG and subsequently induced with CCL2 for 9 days. (A) Representative images of the cells (magnification, ×100; scale bar, 100 µm). (B) A Transwell migration assay was performed to assess the migration capacity of the cells (magnification, ×100; scale bar, 100 µm; *P<0.05). (C) Western blotting was performed to determine the protein expression levels of E-cadherin and N-cadherin. Immunofluorescence staining was performed to determine the protein expression levels of (D) E-cadherin and (E) N-cadherin (magnification, ×200; scale bar, 50 µm). Ctrl, GES-1 cells; MNNG, N-methyl-N-nitro-N′-nitrosoguanidine-pretreated GES-1 cells; CCL2, CC chemokine ligand 2; MNNG+CCL2, MNNG-pretreated GES-1 cells induced with CCL2 for 9 days.
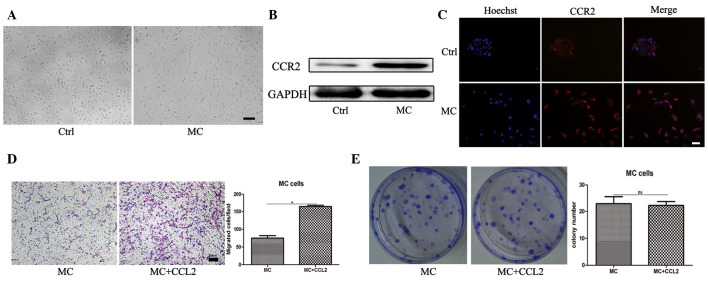
CCR2 upregulation in the MNNG transformed GES-1 cell line
The GES-1 cells transformed by MNNG (termed MC cells) have been regarded as a precancerous cell model. The present study established MC cells using MNNG (2×10−5 mol/l) for 24 h, as described previously (20) (Fig. 4A). To investigate whether the expression of CCR2 in MC cells was also increased, western blot analysis was performed and revealed CCR2 was significantly upregulated in the MC cells (Fig. 4B). This was further confirmed by an immunofluorescence staining assay (Fig. 4C). The results of the Transwell migration assay revealed that the migration capacity of the MC cells was significantly increased in response to CCL2 (Fig. 4D). However, CCL2 still revealed no effect on the MC cell proliferation, as determined by a cell colony formation assay (Fig. 4E). These data indicated that following transformation by MNNG, the expression of CCR2 in MC cells was markedly upregulated.
Figure 4.
CCR2 is upregulated in the MNNG transformed GES-1 cell line. (A) Representative images of the GES-1 and MC cells (magnification, ×100; scale bar, 100 µm). (B) Western blotting was performed to determine the protein expression of CCR2 in the GES-1 and MC cells. (C) Immunofluorescence staining of CCR2 was performed to assess the expression of CCR2 in the cells (magnification, ×200; scale bar, 50 µm). (D) A Transwell assay was performed to determine the migration ability of the MC cells. The MC cells were seeded onto the top of upper chamber and the number of cells that migrated through the uncoated filter in response to CCL2 in the lower chamber was quantified (magnification, ×100; scale bar, 100 µm; *P<0.05). (E) A cell colony formation assay of the MC cells cultured alone or in the presence of CCL2 was performed (*P<0.05). Ctrl, GES-1 cells; MC, MC cells; CCR2, CC chemokine ligand 2.
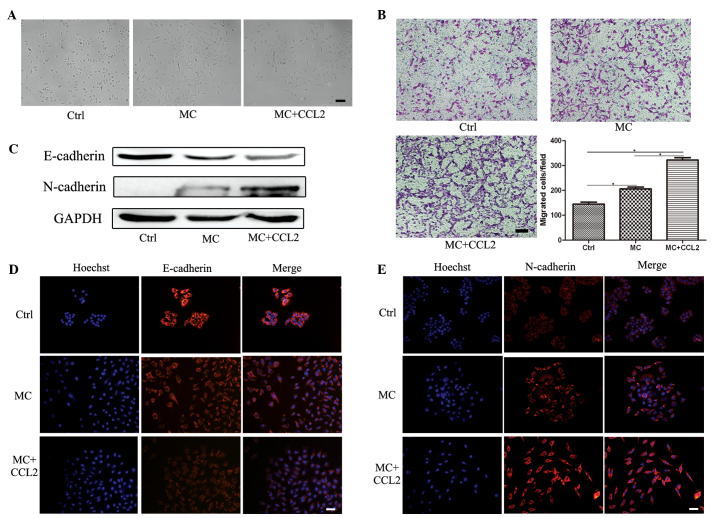
CCL2 promotes the EMT in MNNG transformed GES-1 cells
The MC cells were continuously stimulated with CCL2 for 9 days and collected for analysis. Following treatment with CCL2, the mesenchymal-like morphology of the MC cells revealed no change (Fig. 5A). A Transwell migration assay revealed that the migration ability of the MC cells stimulated by CCL2 was the most marked (Fig. 5B). Western blot analysis revealed that the MC cells expressed a lower level of E-cadherin and a higher level of N-cadherin following CCL2 treatment (Fig. 5C). Immunofluorescence staining further supported the results of the western blotting (Fig. 5D and E), demonstrating that the levels of E-cadherin were downregulated and the levels of N-cadherin were upregulated. These results suggested that CCL2 promoted the migration capacity and the EMT of the MNNG transformed GES-1 cell line.
Figure 5.
CCL2 promotes the EMT in the MNNG transformed GES-1 cell line. The MNNG transformed GES-1 cells (MC cells) were stimulated with CCL2 for 9 days. (A) Representative images of the cells (magnification, ×100; scale bar, 100 µm). (B) A Transwell migration assay was performed to determine the migration ability of the cell line (magnification, ×100; scale bar, 100 µm; *P<0.05). (C) Western blotting was performed to determine the protein expression levels of E-cadherin and N-cadherin. Immunofluorescence staining was performed to asses the protein expression of (D) E-cadherin and (E) N-cadherin (magnification, ×200; scale bar, 50 µm). Ctrl, GES-1 cells; MC, MC cells; CCL2, CC chemokine ligand 2; MC + CCL2, MC cells were stimulated with CCL2 for 9 days.
Discussion
A number of types of human cancer appear to be initiated by chronic inflammation (21). Epithelial cells are exposed to an inflammatory microenvironment in the long-term, leading to the EMT and malignant transformation (22,23). Significantly high expression of CCL2 is detectable in the epithelial region of certain tumor types, including breast cancer (24). There is evidence to support that CCL2 is expressed predominantly in the epithelial regions of prostate cancer tissues (25). Therefore, the present study hypothesized that CCL2 triggered the EMT and the malignant transformation of gastric epithelial cells.
However, the morphology, proliferation and migration capacity of GES-1 cells treated with CCL2 exhibited no changes. Since CCL2 exhibits a particular affinity for the receptor, CCR2, abundant evidence supports that the CCL2/CCR2 signaling axis may be important in carcinogenesis and cancer progression (26–28). Previous data demonstrates that cancer cell derived CCL2 can activate CCR2 on endothelial cells, leading to efficient tumor cell extravasation (29). Data from the present study suggested that the expression of CCR2 was very low in GES-1 cells. Gao et al (30) treated PC-3M cells with CCR2-small interfering RNA and revealed that the cell proliferation rate of the prostate cancer cells was significantly slow and the apoptotic rate was increased. CCR2 knockdown also reduced the migration and invasion ability of PC-3M cells (30). In addition, RNA interference of CCR2 in breast cancer cells markedly inhibits CCL2-induced migration (27). Therefore, these results may provide an explanation as to why CCL2 has no direct effect on the proliferation and migration of GES-1 cells.
CCL2 mediates its effects through the receptor, CCR2, the expression of which is relatively restricted to certain types of cell (9). The expression of the G protein-coupled receptor, CCR2, was increased in breast cancer (27), prostate cancer (31) and ovarian cancer (32), correlating with the expression of CCL2. It is generally accepted that the etiology of gastric cancer is multifactorial and predominantly a dietary habit. NOCs, including MNNG, have been implicated as one of major risk factors for gastric cancer. Notably, GES-1 cells pretreated or transformed with MNNG upregulated the expression of CCR2. Based on these cell models, CCL2 promoted the migration of MNNG-pretreated GES-1 cells and MC cells. In short, these findings suggested that MNNG induced the expression of CCR2, which is crucial for the CCL2-induced migration of GES-1 cells.
A crucial step in reinforcing cell migration may be the acquisition of the EMT phenotype, which reduces cell-cell adhesion and destabilizes the epithelial architecture. The EMT is well-characterized in the initiation and development of cancer and even the upregulation of cancer stemness (33). During the EMT, E-cadherin, which is involved in maintaining cell polarity and organizing the epithelium by strengthening intercellular adhesion, is downregulated and mesenchymal proteins, including N-cadherin, are upregulated (34). A crucial step in reinforcing GES-1 cell migration may be associated with the acquisition of the EMT phenotype. Following treatment with CCL2, the expression of the epithelial marker, E-cadherin, was markedly attenuated, while the expression of the mesenchymal marker, N-cadherin, was notably intensified. As an expectation, the EMT occurred in the MNNG pretreated GES-1 cells and MC cells following CCL2 stimulation. During the EMT process, epithelial cells acquire mesenchymal and stem cell phenotypes, and the EMT-induced cancer stem cell phenotypes may contribute to carcinogenesis in the stomach (35). These results suggested that CCL2 may be involved in the transformation progression of gastric epithelial cells during the chronic inflammatory microenvironment.
Although CCL2 induced the migration and the EMT of the GES-1 cells following treatment with MNNG, no confirmation as to whether GES-1 induced carcinogenesis following long-term exposure to CCL2 was demonstrated. Therefore, future work is required to assess the role of CCL2 in gastric carcinogenesis.
The present study suggested that although normal GES-1 cells lack the expression of CCR2, the chemical carcinogen, MNNG, significantly induced the expression of CCR2 in gastric epithelial cells, which is beneficial for CCL2 prompting the migration of gastric epithelial cells by facilitating the EMT. In conclusion, these findings suggested that the inflammatory cytokine, CCL2, and chemical carcinogens have a synergistic effect on the development of gastric carcinogenesis.
Acknowledgments
This study was supported by the Major Research Plan of the National Natural Science Foundation of China (no. 91129718), the National Natural Science Foundation of China (no. 81302119), the Natural Science Foundation of the Jiangsu Province (nos. BK2012709 and BK20130540), the Doctoral Program Foundation of State Education Ministry (no. 20113227110011), the Jiangsu Province for Natural Science Research in Colleges and Universities (no. 13KJB320001), the Jiangsu University Excellent Young Teacher Project, the Scientific Research Foundation of Jiangsu University for Senior Professional Talents (no. 13JDG088), the Jiangsu Province for Outstanding Sci-tech Innovation Team in Colleges and Universities (no. SJK2013–10) and a Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (no. LJ201117).
References
- 1.Hussain SP, Harris CC. Inflammation and cancer: An ancient link with novel potentials. Int J Cancer. 2007;121:2373–2380. doi: 10.1002/ijc.23173. [DOI] [PubMed] [Google Scholar]
- 2.Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014;2014(149185) doi: 10.1155/2014/149185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schetter AJ, Heegaard NH, Harris CC. Inflammation and cancer: Interweaving microRNA, free radical, cytokine and p53 pathways. Carcinogenesis. 2010;31:37–49. doi: 10.1093/carcin/bgp272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schauer IG, Zhang J, Xing Z, Guo X, Mercado-Uribe I, Sood AK, Huang P, Liu J. Interleukin-1β promotes ovarian tumorigenesis through a p53/NF-κB-mediated inflammatory response in stromal fibroblasts. Neoplasia. 2013;15:409–420. doi: 10.1593/neo.121228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin JT, Wang JY, Chen MK, Chen HC, Chang TH, Su BW, Chang PJ. Colon cancer mesenchymal stem cells modulate the tumorigenicity of colon cancer through interleukin 6. Exp Cell Res. 2013;319:2216–2229. doi: 10.1016/j.yexcr.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Anton K, Banerjee D, Glod J. Macrophage-associated mesenchymal stem cells assume an activated, migratory, pro-Inflammatory phenotype with increased IL-6 and CXCL10 secretion. PLoS One. 2012;7:e35036. doi: 10.1371/journal.pone.0035036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang F, Wang M, Yang T, Cai J, Zhang Q, Sun Z, Wu X, Zhang X, Zhu W, Qian H, Xu W. Gastric cancer-derived MSC-secreted PDGF-DD promotes gastric cancer progression. J Cancer Res Clin Oncol. 2014;140:1835–1848. doi: 10.1007/s00432-014-1723-2. [DOI] [PubMed] [Google Scholar]
- 9.Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): An overview. J Interferon Cytokine Res. 2009;29:313–326. doi: 10.1089/jir.2008.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J, Patel L, Pienta KJ. CC chemokine ligand 2 (CCL2) promotes prostate cancer tumorigenesis and metastasis. Cytokine Growth Factor Rev. 2010;21:41–48. doi: 10.1016/j.cytogfr.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li X, Xu Q, Wu Y, Li J, Tang D, Han L, Fan Q. A CCL2/ROS autoregulation loop is critical for cancer-associated fibroblasts-enhanced tumor growth of oral squamous cell carcinoma. Carcinogenesis. 2014;35:1362–1370. doi: 10.1093/carcin/bgu046. [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Duckworth CA, Fu B, Pritchard DM, Rhodes JM, Yu LG. Circulating galectins -2, -4 and -8 in cancer patients make important contributions to the increased circulation of several cytokines and chemokines that promote angiogenesis and metastasis. Br J Cancer. 2014;110:741–752. doi: 10.1038/bjc.2013.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rokavec M, Wu W, Luo JL. IL6-mediated suppression of miR-200c directs constitutive activation of inflammatory signaling circuit driving transformation and tumorigenesis. Mol Cell. 2012;45:777–789. doi: 10.1016/j.molcel.2012.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu J, Liu X, Wang Y. Predictive value of preoperative serum CCL2, CCL18 and VEGF for the patients with gastric cancer. BMC Clin Pathol. 2013;13(15) doi: 10.1186/1472-6890-13-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tao LL, Shi SJ, Chen LB, Huang GC. Expression of Monocyte chemotactic protein-1/CCL2 in gastric cancer and its relationship with tumor hypoxia. World J Gastroenterol. 2014;20:4421–4427. doi: 10.3748/wjg.v20.i15.4421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crew KD, Neugut AI. Epidemiology of gastric cancer. World J Gastroenterol. 2006;12:354–362. doi: 10.3748/wjg.v12.i3.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aggarwal BB, Gehlot P. Inflammation and cancer: How friendly is the relationship for cancer patients? Curr Opin Pharmacol. 2009;9:351–369. doi: 10.1016/j.coph.2009.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abe M, Yamashita S, Kuramoto T, Hirayama Y, Tsukamoto T, Ohta T, Tatematsu M, Ohki M, Takato T, Sugimura T, Ushijima T. Global expression analysis of N-methyl-N′-nitro-N-nitrosoguanidine-induced rat stomach carcinomas using oligonucleotide microarrays. Carcinogenesis. 2003;24:861–867. doi: 10.1093/carcin/bgg030. [DOI] [PubMed] [Google Scholar]
- 19.Raphael KR, Sabu M, Kumar KH, Kuttan R. Inhibition of N-Methyl-N′-nitro-N-nitrosoguanidine (MNNG) induced gastric carcinogenesis by Phyllanthus amarus extract. Asian Pac J Cancer Prev. 2006;7:299–302. [PubMed] [Google Scholar]
- 20.Li JX, Wang ZB, Zhu LQ, Niu FL, Cui W. Effects of Radix notoginseng extracts drug-containing serum on expressions of bcl-2, Bax and p21WAF1 proteins in MNNG transformed GES-1 cells. Zhong Xi Yi Jie He Xue Bao. 2008;6:817–820. doi: 10.3736/jcim20080809. [DOI] [PubMed] [Google Scholar]
- 21.Kundu JK, Surh YJ. Inflammation: Gearing the journey to cancer. Mutat Res. 2008;659:15–30. doi: 10.1016/j.mrrev.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Xu Y, Zhao Y, Xu W, Luo F, Wang B, Li Y, Pang Y, Liu Q. Involvement of HIF-2α-mediated inflammation in arsenite-induced transformation of human bronchial epithelial cells. Toxicol Appl Pharmacol. 2013;272:542–550. doi: 10.1016/j.taap.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 23.Luo F, Xu Y, Ling M, Zhao Y, Xu W, Liang X, Jiang R, Wang B, Bian Q, Liu Q. Arsenite evokes IL-6 secretion, autocrine regulation of STAT3 signaling and miR-21 expression, processes involved in the EMT and malignant transformation of human bronchial epithelial cells. Toxicol Appl Pharmacol. 2013;273:27–34. doi: 10.1016/j.taap.2013.08.025. [DOI] [PubMed] [Google Scholar]
- 24.Fujimoto H, Sangai T, Ishii G, Ikehara A, Nagashima T, Miyazaki M, Ochiai A. Stromal MCP-1 in mammary tumors induces tumor-associated macrophage infiltration and contributes to tumor progression. Int J Cancer. 2009;125:1276–1284. doi: 10.1002/ijc.24378. [DOI] [PubMed] [Google Scholar]
- 25.Lu Y, Cai Z, Galson DL, Xiao G, Liu Y, George DE, Melhem MF, Yao Z, Zhang J. Monocyte chemotactic protein-1 (MCP-1) acts as a paracrine and autocrine factor for prostate cancer growth and invasion. Prostate. 2006;66:1311–1318. doi: 10.1002/pros.20464. [DOI] [PubMed] [Google Scholar]
- 26.Li M, Knight DA, A Snyder L, Smyth MJ, Stewart TJ. A role for CCL2 in both tumor progression and immunosurveillance. Oncoimmunology. 2013;2:e25474. doi: 10.4161/onci.25474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fang WB, Jokar I, Zou A, Lambert D, Dendukuri P, Cheng N. CCL2/CCR2 chemokine signaling coordinates survival and motility of breast cancer cells through Smad3 protein- and p42/44 mitogen-activated protein kinase (MAPK)-dependent mechanisms. J Biol Chem. 2012;287:36593–36608. doi: 10.1074/jbc.M112.365999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma Y, Adjemian S, Galluzzi L, Zitvogel L, Kroemer G. Chemokines and chemokine receptors required for optimal responses to anticancer chemotherapy. Oncoimmunology. 2014;3:e27663. doi: 10.4161/onci.27663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wolf MJ, Hoos A, Bauer J, Boettcher S, Knust M, Weber A, Simonavicius N, Schneider C, Lang M, Stürzl M, et al. Endothelial CCR2 signaling Induced by colon carcinoma cells enables extravasation via the JAK2-Stat5 and p38MAPK Pathway. Cancer Cell. 2012;22:91–105. doi: 10.1016/j.ccr.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 30.Gao J, Wang A, Zhang M, Li H, Wang K, Han Y, Wang Z, Shi C, Wang W. RNAi targeting of CCR2 gene expression induces apoptosis and inhibits the proliferation, migration and invasion of PC-3M cells. Oncol Res. 2013;21:73–82. doi: 10.3727/096504013X13775486749173. [DOI] [PubMed] [Google Scholar]
- 31.Lu Y, Chen Q, Corey E, Xie W, Fan J, Mizokami A, Zhang J. Activation of MCP-1/CCR2 axis promotes prostate cancer growth in bone. Clin Exp Metastasis. 2009;26:161–169. doi: 10.1007/s10585-008-9226-7. [DOI] [PubMed] [Google Scholar]
- 32.Furukawa S, Soeda S, Kiko Y, Suzuki O, Hashimoto Y, Watanabe T, Nishiyama H, Tasaki K, Hojo H, Abe M, Fujimori K. MCP-1 promotes invasion and adhesion of human ovarian cancer cells. Anticancer Res. 2013;33:4785–4790. [PubMed] [Google Scholar]
- 33.Voulgari A, Pintzas A. Epithelial-mesenchymal transition in cancer metastasis: Mechanisms, markers and strategies to overcome drug resistance in the clinic. Biochim Biophys Acta. 2009;1796:75–90. doi: 10.1016/j.bbcan.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Zhang H, Liu L, Wang Y, Zhao G, Xie R, Liu C, Xiao X, Wu K, Nie Y, Zhang H, Fan D. KLF8 involves in TGF-beta-induced EMT and promotes invasion and migration in gastric cancer cells. J Cancer Res Clin Oncol. 2013;139:1033–1042. doi: 10.1007/s00432-012-1363-3. [DOI] [PubMed] [Google Scholar]
- 35.Peng Z, Wang CX, Fang EH, Wang GB, Tong Q. Role of epithelial-mesenchymal transition in gastric cancer initiation and progression. World J Gastroenterol. 2014;20:5403–5410. doi: 10.3748/wjg.v20.i18.5403. [DOI] [PMC free article] [PubMed] [Google Scholar]