Abstract
Current physical activity and fitness levels among adolescents are low, increasing the risk of chronic disease. Although the efficacy of high intensity interval training (HIIT) for improving metabolic health is now well established, it is not known if this type of activity can be effective to improve adolescent health. The primary aim of this study is to assess the effectiveness and feasibility of embedding HIIT into the school day. A 3-arm pilot randomized controlled trial was conducted in one secondary school in Newcastle, Australia. Participants (n = 65; mean age = 15.8(0.6) years) were randomized into one of three conditions: aerobic exercise program (AEP) (n = 21), resistance and aerobic exercise program (RAP) (n = 22) and control (n = 22). The 8-week intervention consisted of three HIIT sessions per week (8–10 min/session), delivered during physical education (PE) lessons or at lunchtime. Assessments were conducted at baseline and post-intervention to detect changes in cardiorespiratory fitness (multi-stage shuttle-run), muscular fitness (push-up, standing long jump tests), body composition (Body Mass Index (BMI), BMI-z scores, waist circumference) and physical activity motivation (questionnaire), by researchers blinded to treatment allocation. Intervention effects for outcomes were examined using linear mixed models, and Cohen's d effect sizes were reported. Participants in the AEP and RAP groups had moderate intervention effects for waist circumference (p = 0.024), BMI-z (p = 0.037) and BMI (not significant) in comparison to the control group. A small intervention effect was also evident for cardiorespiratory fitness in the RAP group.
Keywords: Physical activity, Exercise, Fitness, Health promotion, Intervention, Adolescent, High intensity interval training, School
Highlights
-
•
Both HIIT intervention groups resulted in moderate improvements in body composition.
-
•
The RAP group resulted in moderate improvements in cardiorespiratory fitness.
-
•
The intervention dose was practical and achievable for participants and teachers.
-
•
Teachers reported a willingness to embed HIIT within future PE lessons.
Introduction
Less than 20% of adolescents worldwide are participating in sufficient physical activity to accrue health benefits (Hallal et al., 2006); cardiorespiratory fitness levels among young people have steeply declined over the last 30-years (Tomkinson and Oliver, 2007). In Australia, only 15% of youth aged 12–17 accumulate 60-minutes of moderate-to-vigorous physical activity everyday (Cancer Council Victoria, 2010), and 65% of youth have aerobic fitness levels associated with reduced risk of poor cardiometabolic health (Hardy et al., 2010). Longitudinal studies have demonstrated that physical activity levels decline by 10% each year during adolescence (Dumith et al., 2011) and health behaviors established during this period continue into adulthood (Hallal et al., 2006, Menschik et al., 2008, McDavid et al., 2012). While adolescents are a high priority population for these reasons described, previous interventions to increase physical activity and improve fitness levels have been largely ineffective (Dobbins et al., 2013).
Schools represent an ideal setting for promoting physical activity and fitness in adolescent populations (Mura et al., 2015). As young people spend 6–8 h/day in schools, which have facilities, personnel and curriculum to provide opportunities for physical activity. Physical education (PE) is the primary vehicle associated with physical activity promotion in the school setting (CDC, 2013), yet physical activity levels within PE lessons are generally low (Rosenkranz et al., 2012, Lonsdale et al., 2013). In addition, lessons may not occur frequently enough to achieve health gains and students' opportunities for physical activity decrease in senior years. While increasing the duration and frequency of PE lessons would be ideal, this is not practical considering the challenges associated with the existing ‘crowded curriculum’ (Hills et al., 2015). Indeed, any strategy designed to increase activity and fitness in schools needs to be time efficient and scalable for easy implementation (Dobbins et al., 2013, Naylor et al., 2015).
A growing body of literature supports the efficacy of high intensity interval training (HIIT) for improving sport performance in athletes (Laursen and Jenkins, 2002) and cardiorespiratory fitness in adult populations (Weston et al., 2013). While there is not a standardized definition of this type of training, HIIT involves (a) short or long intervals (from ≤ 45 s to 2–4 min) of intense exercise (e.g., > 85% max heart rate) interspersed by short rest periods or (b) reoccurring short or long (< 10 s to 20–30 s) bouts of maximal sprints, interspersed by a rest period (Buchheit and Laursen, 2013). For adolescent populations the “all out” maximal type of HIIT would not be palatable for most individuals (Hardcastle et al., 2014). The main appeal of HIIT is that it can be completed in a short period of time (compared to traditional aerobic training), while resulting in equivalent physiological adaptations (Buchheit and Laursen, 2013).
Although the efficacy of HIIT for improving metabolic health in different population groups (including adolescents) is now well established, it is not known if this type of activity can be effective for population-level health promotion (Biddle and Batterham, 2015). Indeed, the majority of HIIT studies conducted with adolescents have examined running-based programs (Buchan et al., 2011a, Buchan et al., 2011b, Buchan et al., 2013, De Araujo et al., 2012) and most have been conducted in clinical settings with trained athletes. To the authors' knowledge, no previous study has evaluated the efficacy of embedding HIIT into the school day. The objective of this study was to evaluate the efficacy and feasibility of a three-arm randomized controlled trial design testing two HIIT protocols [aerobic exercise program (AEP) and resistance and aerobic exercise (RAP)] for improving health-related fitness, body composition and physical activity motivation in a sample of adolescents. Due to the effectiveness of HIIT on fitness in other population groups, we hypothesize that HIIT will be a successful strategy to improve health-related fitness outcomes in adolescents.
Methods
Ethics approval for the study was gained from the University of Newcastle Human Research Ethics Committee (H-2014-0083) and permission to conduct research from the relevant educational organization was granted. The study protocol has been registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12614000729628). To be included in this study the school needed to meet the following criteria: (a) co-educational; (b) provide at least 2 PE lessons per week; and, (c) not currently participating in a physical activity program in addition to regular PE. The school principal, parents and study participants provided written informed consent to participate in the study. Study participants (n = 65), were students in year 9–10 attending the study school, who consented to participate. The design, conduct and reporting for this randomized controlled trial adhere to the Consolidated Standards of Reporting Trials guidelines (Moher et al., 2010).
Study design
A three-arm school-based randomized controlled trial was conducted with adolescents attending one secondary school in Newcastle, to evaluate the effects of two 8-week training programs focused on improving fitness via the provision of short HIIT sessions three times/week (total: 24 sessions). Sessions ranged from eight to ten minutes in duration (weeks 1–3: 8 min; weeks 4–6: 9 min; weeks 7–8: 10 min), with a work to rest ratio of 30 s:30 s. The AEP and RAP sessions were delivered by the research team (PE qualified) at the study school.
Power calculations were based on change in the primary outcome (cardiorespiratory fitness, assessed using the multi-stage shuttle test (Léger et al., 1988)). Based on our previous research (Eather et al., 2015), a between-group difference of 10 laps was considered achievable. Assuming a standard deviation of 9 laps, 80% power with alpha levels set at 0.05, it was determined that 20 participants per group would provide adequate power to detect statistically significant effects.
Once baseline assessments of cardiorespiratory fitness, muscular fitness, body composition and physical activity motivation were conducted (research assistants blinded to treatment allocation), participants were randomized at the individual level using a random number-producing algorithm, by an independent researcher. A stratified random sampling procedure was conducted to ensure that equal numbers of boys and girls were allocated between the three groups.
Participants in the intervention groups participated in three HIIT sessions/week for eight weeks and all sessions were conducted inside the school hall. Two HIIT sessions/week were delivered in scheduled PE lessons, with a third session delivered at lunchtime. The focus of each of the three programs included:
-
i.
AEP: Participants completed HIIT sessions primarily involving gross motor cardiorespiratory exercises requiring minimal equipment (e.g., shuttle runs, jumping jacks, skipping);
-
ii.
RAP: Participants completed HIIT sessions that included a combination of cardiorespiratory and body weight resistance training exercises that required minimal equipment (e.g., body weight squats, push-ups, hovers); and
-
iii.
Control: Participants continued with their programmed PE and usual lunchtime activities over the 8-week intervention period. The control group received the AEP program once the intervention and follow-up assessments were completed (Fig. 1).
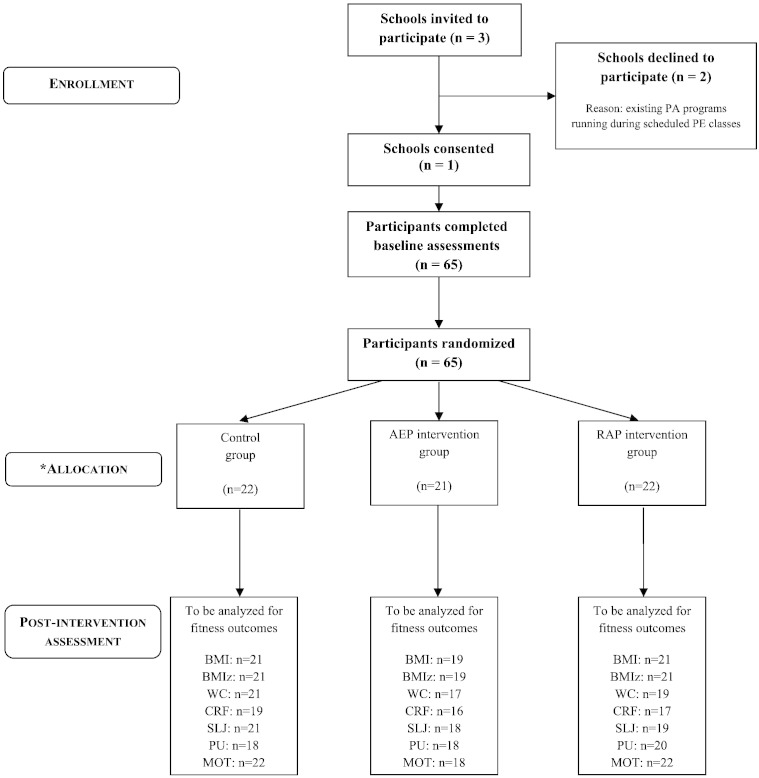
Fig. 1.
Flow of participants through the study. Note: BMI: body mass index; WC: waist circumference; CRF: cardiorespiratory fitness; SLJ: standing long jump; PU: push up test; MOT: physical activity motivation; PA: physical activity; PE: physical education; AEP: aerobic exercise program; RAP: resistance and aerobic program. *Study conducted in Newcastle Australia in 2014.
The AEP and RAP groups engaged in HIIT sessions while the control group did their usual PE warm-up, then the groups were combined to complete the remainder of the PE lesson. HIIT session duration and intensity were the same for both intervention groups. To encourage maintenance of the appropriate exercise intensity, participants were fitted with heart rate monitors (Polar H7), which were connected to a central iPad application (Polar Team). Participants were able to view this information on a projector screen during sessions.
To promote exercise adherence, sessions were designed to be enjoyable, with fun warm-up and cool-down activities. In addition, sessions were completed in pairs, with one participant undertaking the ‘work’ phase, while their partner completed the ‘rest’ phase. Sessions focused on promoting encouragement and support to peers, ‘Trainer of the Day’ certificates were awarded to one pair at the completion of each session. Awards were given to participants who provided positive feedback and motivation for their partner and demonstrated outstanding effort and dedication during the workout. At the conclusion of the intervention the pair awarded the most certificates received a prize (e.g., a gift voucher). As the intervention progressed and exercises were mastered, participants were given additional elements of choice including: music (student playlists used weeks 2–8), exercise choices during a workout (weeks 4–6) and choice of workout (between two workouts previously completed; weeks 7 and 8).
Outcomes
All assessments were conducted by trained members of the research team blinded to group allocation (baseline and post-test). A protocol manual including specific instructions for conducting all assessments was used by research assistants for accuracy and consistency. Physical assessments were conducted in a sensitive method (e.g. weight/waist circumference were measured in a private setting) and questionnaires were completed under exam-like conditions.
Primary outcome
The primary outcome was cardiorespiratory fitness assessed using the Progressive Aerobic Cardiovascular Endurance Run shuttle test (Léger et al., 1988) using FITNESSGRAM® testing procedures (Cooper Institute for Aerobics Research, 2013). This test is recommended by the Institute of Medicine (IOM) (Institute of Medicine, 2012) as the most accurate and appropriate field-based measure of cardiorespiratory fitness in young people. Total number of laps completed was converted to estimate aerobic fitness (VO2max) using the equation:
41.76799 + (0.49261 × PACER) − (0.00290 × PACER2) − (0.61613 × BMI) + (0.34787 × gender × age) (Mahar et al., 2011).
Note: PACER = number of laps completed; gender: 1 = boy and 0 = girl; and age in years.
Secondary outcomes
Muscular fitness: A modified version of the 90° push-up test was used as a measure of upper body muscular endurance (Cooper Institute for Aerobics Research, 2004); this test has acceptable test–retest reliability in adolescents (ICC [95% CI] = .90 [.80 to .95]) (Lubans et al., 2011). The standing long jump was used as a measure of lower body muscular strength (Castro-Pinero et al., 2010) and has acceptable reliability and validity in adolescents (Ortega et al., 2008).
Body composition: Weight was measured in light clothing without shoes using a portable digital scale (Model no. UC-321PC, A&D Company Ltd., Tokyo Japan) to the nearest 0.1 kg. Height was recorded to the nearest 0.1 cm using a portable stadiometer (Model no. PE087, Mentone Educational Centre, Australia). BMI was then calculated using the formula weight (kg)/height (m)2. Waist circumference was measured to the nearest 0.1 cm against the skin using a non-extensible steel tape (KDSF10-02, KDS Corporation, Osaka, Japan) in line with the umbilicus.
Physical activity motivation: Autonomous motivation to engage in physical activity was assessed using an 8-item validated questionnaire examining benefits, fun, importance, enjoyment, effort, pleasure, restlessness and satisfaction related to physical activity participation (Markland and Tobin, 2004). Cronbach's alpha was used as a measure of scale reliability [baseline: (α = 0.90) and post-test: (− α = 0.91)].
Process evaluation
Program feasibility was assessed based on the following: consent rate (how many participants offered the program agreed to be involved), retention rate (how many participants completed the intervention and participated in baseline/post-intervention testing), adherence (weekly session attendance of 3 sessions delivered/week (total: 24), average session heart rate across the 8 weeks totalling 10 min inclusive of warm-up/cool-down phase) and participants' satisfaction with the program (I enjoyed participating in the HIIT sessions on 5-point Likert scale: 5 = strongly agree to 1 = strongly disagree). In addition, teachers were asked to report their confidence to deliver the HIIT programs at the end of the study period (I am confident that I could deliver the HIIT/body weight sessions at the start of my PE lessons on 5-point Likert scale: 5 = strongly agree to 1 = strongly disagree).
Statistical analyses
Statistical analyses of the primary and secondary outcomes were conducted using linear mixed models with IBM SPSS Statistics for Windows, Version 20.0 (2010 SPSS Inc., IBM Company Armonk, NY). Cohen's d was used to provide a measure of effect size (adjusted difference between HIIT and control groups over time divided by the pooled standard deviation of change). Moderators of HIIT effects were explored using linear mixed models with interaction terms for the following: i) sex (boys versus girls), ii) and baseline fitness level (i.e., healthy fitness zone versus needs improvement). Subgroup analyses were conducted if the interaction term was statistically significant (p = 0.10) (Assmann et al., 2000).
Results
The number of participants involved at each phase of the study is reported in Fig. 1. One secondary school was successfully recruited and 65 adolescents from three classes (45 males, 20 females, mean age: 15.8(0.6)) from years 9–10 completed baseline testing (see Table 1). The intervention groups were similar for baseline characteristics. Of the 65 participants, 52 were classified as within the ‘Healthy Fitness Zone’ (HFZ) and six were identified as ‘Needs Improvement’ for cardiorespiratory fitness at baseline. Cardiorespiratory fitness was not reported for seven participants.
Table 1.
Participant baseline demographics.
| Demographic factor |
Group 1 (control) Mean (SD) |
Group 2 (AEP) Mean (SD) |
Group 3 (RAP) Mean (SD) |
|---|---|---|---|
| n | n = 22 | n = 21 Males: 16, females: 5 |
N = 22 Males: 15, females: 7 |
| Age (months) | 15.6 (0.6) | 15.7 (0.7) | 15.5 (0.6) |
| Weight (kg) | 66.0 (15.8) | 64.7 (9.8) | 67.0 (12.9) |
| Height (cm) | 171.3 (10.6) | 172.3 (8.6) | 173.8 (7.1) |
| BMI (kg/m2) | 22.29 (3.53) | 21.72 (2.10) | 22.08 (3.56) |
| BMI-z | 0.51 (0.94) | 0.43 (0.60) | 0.45 (1.05) |
| Estimated VO2max (ml·kg·min) | 50.3 (6.6) | 49.3 (6.6) | 47.3 (7.4) |
Note: AEP = aerobic exercise program; RAP = resistance and aerobic exercise program; BMI = body mass index. Study conducted in Newcastle Australia, in 2014.
Changes in primary outcome
Changes for all outcomes are reported in Table 2. Analyses of efficacy (adjusted difference between group and Cohen's d effect sizes) identified a small intervention effect for the RAP condition for the primary outcome, cardiorespiratory fitness (5.2 laps, 95% CI = − 4.2 to 14.7; d = 0.4). After converting laps to estimated VO2max (Mahar et al., 2011), a between group difference of 5.9 ml·kg·min was found in favor of the RAP condition.
Table 2.
Changes in primary and secondary outcomes post-intervention.
| Variable | Control group |
AEP group |
RAP group |
Adjusted difference between groupsa |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AEP–control |
RAP–control |
|||||||||||
| Baseline Mean (95% CI) |
Posttest Mean (95% CI) |
Baseline Mean (95% CI) |
Posttest Mean (95% CI) |
Baseline Mean (95% CI) |
Posttest Mean (95% CI) |
Mean Change (95% CI) |
p value | Cohen's d | Mean Change (95% CI) |
p value | Cohen's d | |
| Cardio-respiratory fitness (laps) | 60.8 (49.3, 72.4) |
60.6 (49.9, 71.3) |
59.6 (47.3, 71.9) |
61.9 (50.3, 73.4) |
59.5 (47.9, 71.2) |
64.5 (53.5, 75.6) |
2.5 (− 7.2, 12.3) |
0.605 | 0.1 | 5.2 (− 4.2, 14.7) |
0.571 | 0.4 |
| BMI (kg/m2) | 22.29 (20.95, 23.64) |
22.63 (21.31, 23.95) |
21.72 (20.27, 23.16) |
21.80 (20.38, 23.22) |
22.00 (20.66, 23.35) |
22.07 (20.75, 23.38) |
− 0.27 (− 0.57, 0.04) |
0.086 | − 0.5 | − 0.28 (− 0.57, 0.02) |
0.067 | − 0.5 |
| BMI z-scores | 0.51 (0.13, 0.83) |
0.59 (0.22, 0.95) |
0.43 (0.03, 0.84) |
0.41 (0.02, 0.80) |
0.45 (0.07, 0.82) |
0.45 (0.08, 0.81) |
− 0.10 (− 0.20, − 0.01) |
0.037⁎ | − 0.6 | − 0.08 (− 0.17, 0.01) |
0.093 | − 0.5 |
| Waist circumference (cms) | 77.1 (73.2, 80.9) |
77.7 (73.6, 81.9) |
76.6 (72.5, 80.8) |
75.8 (71.3, 80.3) |
78.7 (74.9, 82.6) |
77.3 (73.1, 81.5) |
− 1.5 (− 3.4, 0.4) |
0.113 | − 0.5 | − 2.1 (− 4.0, − 0.3) |
0.024⁎ | − 0.7 |
| Standing long jump (cms) | 170.3 (155.2, 185.4) |
179.0 (162.0, 196.1) |
164.5 (148.4, 180.7) |
174.7 (156.4, 193.1) |
179.7 (164.7, 194.7) |
184.9 (167.7, 202.1) |
1.4 (− 9.3, 12.1) |
0.789 | 0.1 | 3.6 (− 14.2, 6.9) |
0.492 | − 0.2 |
| Push-ups (repetitions) | 13.3 (9.2, 17.5) |
16.6 (12.1, 21.1) |
13.8 (9.5, 18.1) |
17.6 (12.9, 22.3) |
15.1 (11.1, 19.1) |
17.8 (13.4, 22.1) |
0.5 (− 2.6, 3.7) |
0.731 | 0.1 | 0.7 (− 3.7, 2.4) |
0.668 | − 0.1 |
| Motivation (score/40) | 34.59 (32.13, 37.06) |
34.05 (31.27, 36.82) |
31.70 (29.11, 34.29) |
31.75 (28.79, 34.71) |
32.23 (29.76, 34.69) |
32.05 (29.27, 34.82) |
0.60 (− 1.89, 3.08) |
0.632 | 0.1 | 0.36 (− 1.99, 2.72) |
0.759 | 0.1 |
Adjusted difference between groups and 95% confidence interval between intervention and control groups after the 8-week intervention (AEP minus control; RAP minus control).
p < 0.05
Changes in secondary outcomes
There was a moderate intervention effect for BMI in the AEP (− 0.27 kg/m2, 95% CI = − 0.57 to 0.04; d = − 0.53) and the RAP groups (− 0.28 kg/m2, 95% CI = − 0.57 to 0.02; d = − 0.53). Intervention effects for waist circumference were moderate for the AEP group (− 1.5 cm, 95% CI = − 3.4 to 0.4; d = − 0.5) and large and statistically significant for the RAP group (− 2.1 cm, 95% CI = − 4.0 to − 0.3; d = − 0.7; p = 0.024). Moderate and statistically significant intervention effects were found for BMI-z for the AEP group (− 0.10, 95% CI = − 0.20 to − 0.01; d = 0.63; p = 0.037) and moderate intervention effects for the RAP group (− 0.08, 95% CI = − 0.17 to 0.01; d = − 0.50). There were no intervention effects for muscular fitness for either HIIT group. Motivation remained stable in both intervention groups from baseline to post-test (AEP: 0.60, 95% CI = − 1.89 to 3.08, d = 0.10; RAP: 0.36, 95% CI = − 1.99 to 2.72; d = 0.10). As there were no significant (p < .10) interaction effects for any of the potential moderators, subgroup analyses were not conducted.
Process evaluation
The program achieved good recruitment (consent rate: 86%), adherence (average attendance: 2.2 of 3 sessions/week) and retention (90.8%). Heart rate targets were met, with a higher average heart rate evident for the RAP (AEP: 74.04% of max, 148.09 bpm; RAP: 77.58% of max, 155.15 bpm) (average across all session weeks 1-8 inclusive of warm-up/cool-down phase). Of the 43 intervention participants 31 completed the post-program evaluation questionnaire and reported on a 5-point Likert scale (5 = strongly agree to 1 = strongly disagree) that the program was enjoyable (x̄ = 4.2). Similarly, the four teachers involved in the study all agreed that: (i) their students had enjoyed participating in the intervention, (ii) they could confidently deliver the HIIT sessions at the start of their lessons with minimal professional learning and, (iii) they intend to include HIIT in their physical education lessons in the future.
Conclusions
The aim of this study was to evaluate the preliminary efficacy and feasibility of embedding HIIT into the school day. Although not statistically significant, small improvements in cardiorespiratory fitness were observed for the RAP condition. In addition, participants in both HIIT groups improved their body composition in comparison to the control group. Overall, the strongest intervention effects were observed for participants in the RAP group, which included resistance and aerobic exercises during sessions. In regards to feasibility, the program achieved high recruitment, good adherence and retention. Participants enjoyed participating in the HIIT sessions and supervising teachers reported a willingness to embed HIIT within future PE lesson.
The RAP intervention condition achieved small intervention effects for cardiorespiratory fitness, an increase of 5.2 laps on the shuttle test was achieved in comparison to controls, which converts to an estimated VO2Max increase of 5.5 mL·kg·min (6.1% improvement). Similarly, a recent systematic review and meta-analysis (Costigan et al., 2015) revealed that HIIT can improve cardiorespiratory fitness [unstandardized mean difference (MD) = 2.6 mL·kg·min, 95% CI = 1.8 to 3.3, p < 0.001] in comparison to moderate-intensity exercise and non-exercising control conditions in adolescents. However, results of our study were not statistically significant, which may be explained by the small sample size. In contrast, the AEP resulted in only trivial improvements in cardiorespiratory fitness, this difference is of interest given that both HIIT conditions had an aerobic component and the same training volume and intensity. It may be that muscle performance was enhanced by the lower body strength exercises (e.g., body weight squats) performed as part of the RAP condition and this contributed to larger performance improvements and higher average session heart rates.
There was a moderate intervention effect for BMI and BMI-z in both groups. High BMI values are associated with various adverse health outcomes (Buncher et al., 2015, Weber et al., 2014, Twig et al., 2014), therefore even moderate improvements can be meaningful at the population level. The favorable intervention effects on BMI in our study are supported by findings of a recent systematic review and meta-analysis which reported HIIT to be a feasible and time efficient approach for improving body composition in adolescent populations, reporting a moderate and statistically significant intervention effect for BMI [(MD = − 0.6 kg/m2, 95% CI = − 0.9 to − 0.4, p < .001) (d = − .37, 95% CI = − 0.68 to − .05)] (Costigan et al., 2015).
Moderate intervention effects were found for waist circumference for the AEP and large statistically significant intervention effects for RAP. Intervention effects on waist circumference for HIIT are supported by a range of other studies in adolescent populations (Buchan et al., 2013, Boer et al., 2014, Farah et al., 2014, Racil et al., 2013, Tjønna et al., 2009). Of these studies, four utilized sprints-based training (Buchan et al., 2013, Farah et al., 2014, Racil et al., 2013, Tjønna et al., 2009), and one study used sprint cycling (Boer et al., 2014). Follow-up periods of these studies ranged between post-intervention and 3-weeks, therefore it is unknown whether participating in these activities would result in continued participation and long-term improvement in waist circumference for adolescents. In addition, it is unknown whether participating in the same type of activity (e.g., cycling or sprints) for an extended time period is appealing for adolescents given three of the five studies reported low retention rates (44-50% (Buchan et al., 2013, Farah et al., 2014, Tjønna et al., 2009)).
There was a negligible effect on objective measures of muscular fitness in comparison to the control condition. Similarly, a recent systematic review found the overall effect of HIIT on muscular fitness was not statistically significant (MD = 0.8 cm, 95% CI = − 1.8 to 3.4, p = 0.5) (Costigan et al., 2015). In our study, muscular fitness improvements for the control group were similar to the HIIT conditions, which may be explained by the learning effect associated with fitness testing. In addition, the lack of intervention effect could also be attributed to the ability of the tests to detect change. For instance, we used field-based tests to assess muscle performance but it may be that more sophisticated laboratory-based assessments are able to detect modest improvements in performance resulting from HIIT. There is clearly a need for further studies to examine the long-term impact of HIIT on muscular fitness in adolescent populations. It could be necessary for interventions to implement a higher dose and to be conducted for longer duration for muscular fitness improvements.
The intervention effect of HIIT on physical activity motivation was trivial. However, this in itself may be an encouraging outcome, given recent commentaries have suggested that prescribing intense exercise (specifically sprints training) to general/sedentary populations may lead to feelings of incompetence and failure resulting in reduced physical activity motivation and participation (Hardcastle et al., 2014). Numerous studies have reported positive associations between young people's physical activity and various measures of motivation (Owen et al., 2014) (e.g., autonomous motivation (Vierling et al., 2007, Standage et al., 2012); intrinsic and introjected physical activity motivation (Verloigne et al., 2011); self-determined motivation (Owen et al., 2013)). If delivered using an authoritarian teaching style, HIIT could be unenjoyable. However, our HIIT intervention was developed in reference to self-determination theory (Deci and Ryan, 1985) and the sessions were designed to satisfy participants' basic psychological needs for autonomy (e.g., choice of music, exercise choices during a workout and choice of workout), competence (e.g., provision of challenging yet achievable workouts, positive feedback and heart rate data) and relatedness (e.g., working in pairs, sessions focused on promoting encouragement and support to peers). We suggest that HIIT can be delivered using an autonomy supportive manner, but teachers may require appropriate professional learning to ensure that programs support rather than thwart young people's basic psychological needs.
Based on the high retention rates, session attendance, satisfaction and adherence to heart rate targets, the HIIT protocols and delivery methods were acceptable for participants and teachers. Intervention strategies appealed to participants and resulted in continued involvement in the program. Further investigation of technology-based strategies such as smartphone applications and text messaging (Smith et al., 2014, Thompson et al., 2014) to promote adherence and participation beyond the school setting are clearly warranted. In addition, qualitative research is needed to inform future studies of additional strategies for sustained intervention fidelity and the perceptions and pragmatic aspects of introducing HIIT within the school context.
Strengths and limitations
This study has a number of strengths including the randomized design, assessor blinding and high levels of intervention fidelity. Importantly, the retention and session attendance rates were high, demonstrating that the program was appealing to the target group. However, some limitations should also be acknowledged. The small sample size may limit the generalizability of our findings, as the study was conducted in one school with more boys than girls. Laboratory-based methods such as DXA for body composition and isokinetic/isotonic muscle performance testing may have detected more substantial changes resulting from the intervention. physical activity undertaken outside of school time was not taken into account, which could affect the changes in some outcome measures. Finally, cardiorespiratory fitness was assessed using the multi-stage fitness test; while this test is considered the most appropriate field-based measure of cardiorespiratory fitness (Pate and Daniels, 2013), VO2max testing is considered to be the gold standard.
Conclusions and future directions
Evidence from this study highlights the potential of embedding HIIT within PE for improving cardiorespiratory fitness and body composition among adolescents. While an 8-week, school-based HIIT intervention appears to be a promising approach for improving fitness outcomes; some results were not statistically significant and therefore require further examination on a larger scale. In addition, the long-term effectiveness and sustainability of this approach should be assessed both quantitatively and qualitatively, and the potential of successfully training teachers to deliver the program also requires investigation. In summary, HIIT appears to be a feasible approach for improving fitness for adolescents in a school-based setting. Further longitudinal research with longer follow-up periods, investigating a larger sample of adolescents from different schools should be conducted.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Transparency document
Transparency document.
Acknowledgments
DRL is supported by an Australian Research Council Future Fellowship (FT140100399). RCP is supported by a National Health and Medical Research Council Senior Research Fellowship (APP1023602). This project was supported by a Hunter Medical Research Institute Project Grant (Children's Research in Cardiovascular) (G1500311).
Footnotes
The Transparency document associated with this article can be found, in the online version.
Contributor Information
S.A. Costigan, Email: sarah.costigan@newcastle.edu.au.
N. Eather, Email: narelle.eather@newcastle.edu.au.
R.C. Plotnikoff, Email: ron.plotnikoff@newcastle.edu.au.
D.R. Taaffe, Email: dtaaffe@uow.edu.au.
E. Pollock, Email: emma.pollock@newcastle.edu.au.
S.G. Kennedy, Email: sarah.kennedy@newcastle.edu.au.
D.R. Lubans, Email: david.lubans@newcastle.edu.au.
References
- Assmann S.F., Pocock S.J., Enos L.E. Subgroup analysis and other (mis) uses of baseline data in clinical trials. Lancet. 2000;355(9209):1064–1069. doi: 10.1016/S0140-6736(00)02039-0. [DOI] [PubMed] [Google Scholar]
- Biddle S.J., Batterham A.M. High-intensity interval exercise training for public health: a big HIT or shall we HIT it on the head? IJBNPA. 2015;12(1):95. doi: 10.1186/s12966-015-0254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boer P.-H., Meeus M., Terblanche E. The influence of sprint interval training on body composition, physical and metabolic fitness in adolescents and young adults with intellectual disability: a randomized controlled trial. Clin. Rehabil. 2014;28(3):221–231. doi: 10.1177/0269215513498609. [DOI] [PubMed] [Google Scholar]
- Buchan D., Ollis S., Thomas N. Physical activity interventions: effects of duration and intensity. Scand. J. Med. Sci. Sports. 2011;21(6):e341–e350. doi: 10.1111/j.1600-0838.2011.01303.x. [DOI] [PubMed] [Google Scholar]
- Buchan D.S., Ollis S., Young J.D. The effects of time and intensity of exercise on novel and established markers of CVD in adolescent youth. Am. J. Hum. Biol. 2011;23(4):517–526. doi: 10.1002/ajhb.21166. [DOI] [PubMed] [Google Scholar]
- Buchan D.S., Ollis S., Young J.D. High intensity interval running enhances measures of physical fitness but not metabolic measures of cardiovascular disease risk in healthy adolescents. BMC Public Health. 2013;13:498. doi: 10.1186/1471-2458-13-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchheit M., Laursen P.B. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013;43(5):313–338. doi: 10.1007/s40279-013-0029-x. [DOI] [PubMed] [Google Scholar]
- Buncher R., Helmrath M., Brandt M.L. 2015. Cardiovascular Risk Factors in Severely Obese Adolescents the Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Council, Victoria . 2010. National Secondary Students' Diet and Activity (NaSSDA) Survey. [Google Scholar]
- Castro-Pinero J., Ortega F.B., Artero E.G. Assessing muscular strength in youth: usefulness of the standing long jump as a general index of muscular fitness. J. Strength Cond. Res. 2010;24:1810–1817. doi: 10.1519/JSC.0b013e3181ddb03d. [DOI] [PubMed] [Google Scholar]
- CDC . Department of Health and Human Services; Atlanta, GA: US: 2013. Comprehensive School Physical Activity Programs: A Guide for Schools. [Google Scholar]
- Cooper Institute for Aerobics Research . 3rd Ed. Human Kinetics; Campaign, IL: 2004. The Prudential Fitnessgram: Test Administration Manual. [Google Scholar]
- Cooper Institute for Aerobics Research . The Cooper Institute; Dallas, TX: 2013. Fitnessgram/Activitygram Reference Guide (4th Edition) [Google Scholar]
- Costigan S., Eather N., Plotnikoff R. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. BJSM. 2015;49(19):1253–1261. doi: 10.1136/bjsports-2014-094490. (bjsports-2014-09449010.1136/bjsports-2014-094490) [DOI] [PubMed] [Google Scholar]
- De Araujo A.C.C., Roschel H., Picanço A.R. Similar health benefits of endurance and high-intensity interval training in obese children. PONE. 2012;7(8) doi: 10.1371/journal.pone.0042747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci E.L., Ryan R.M. Springer Science & Business Media; 1985. Intrinsic Motivation and Self-determination in Human Behavior. [Google Scholar]
- Dobbins M., Husson H., DeCorby K. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2013;2 doi: 10.1002/14651858.CD007651.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumith S.C., Gigante D.P., Domingues M.R. Physical activity change during adolescence: a systematic review and a pooled analysis. Int. J. Epidemiol. 2011;40(3):685–698. doi: 10.1093/ije/dyq272. [DOI] [PubMed] [Google Scholar]
- Eather N., Morgan P.J., Lubans D.R. Improving health-related fitness in adolescents: the CrossFit Teens™ randomised controlled trial. J. Sports Sci. 2015:1–15. doi: 10.1080/02640414.2015.1045925. (ahead-of-print) [DOI] [PubMed] [Google Scholar]
- Farah B.Q., Ritti-Dias R.M., Balagopal P. Does exercise intensity affect blood pressure and heart rate in obese adolescents? A 6-month multidisciplinary randomized intervention study. Pediatr. Obes. 2014;9(2):111–120. doi: 10.1111/j.2047-6310.2012.00145.x. [DOI] [PubMed] [Google Scholar]
- Hallal P.C., Victora C.G., Azevedo M.R. Adolescent physical activity and health. Sports Med. 2006;36(12):1019–1030. doi: 10.2165/00007256-200636120-00003. [DOI] [PubMed] [Google Scholar]
- Hardcastle S.J., Ray H., Beale L. Why sprint interval training is inappropriate for a largely sedentary population. Front. Psychol. 2014:5. doi: 10.3389/fpsyg.2014.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy L.L.K.L., Espinel P., Cosgrove C., Bauman A. NSW Ministry of Health; Sydney: 2010. NSW Schools Physical Activity and Nutrition Survey (SPANS): Full Report. [Google Scholar]
- Hills A.P., Dengel D.R., Lubans D.R. Supporting public health priorities: recommendations for physical education and physical activity promotion in schools. Prog. Cardiovasc. Dis. 2015;57(4):368–374. doi: 10.1016/j.pcad.2014.09.010. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . National Academies Press; Washington, DC: 2012. Fitness Measures and Health Outcomes in Youth. [PubMed] [Google Scholar]
- Laursen P.B., Jenkins D.G. The scientific basis for high-intensity interval training. Sports Med. 2002;32(1):53–73. doi: 10.2165/00007256-200232010-00003. [DOI] [PubMed] [Google Scholar]
- Léger L.A., Mercier D., Gadoury C. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988;6(2):93–101. doi: 10.1080/02640418808729800. [DOI] [PubMed] [Google Scholar]
- Lonsdale C., Rosenkranz R.R., Peralta L.R. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev. Med. 2013;56(2):152–161. doi: 10.1016/j.ypmed.2012.12.004. [DOI] [PubMed] [Google Scholar]
- Lubans D.R., Morgan P., Callister R. Test–retest reliability of a battery of field-based health-related fitness measures for adolescents. J. Sports Sci. 2011;29(7):685–693. doi: 10.1080/02640414.2010.551215. [DOI] [PubMed] [Google Scholar]
- Mahar M.T., Guerieri A.M., Hanna M.S. Estimation of aerobic fitness from 20-m multistage shuttle run test performance. Am. J. Prev. Med. 2011;41(4):S117–S123. doi: 10.1016/j.amepre.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Markland D., Tobin V. A modification of the Behavioral Regulation in Exercise Questionnaire to include an assessment of amotivation. J. Sport Exerc. Psychol. 2004;26(2):191–196. [Google Scholar]
- McDavid L., Cox A.E., Amorose A.J. The relative roles of physical education teachers and parents in adolescents' leisure-time physical activity motivation and behavior. Psychol. Sport Exerc. 2012;13(2):99–107. [Google Scholar]
- Menschik D., Ahmed S., Alexander M.H. Adolescent physical activities as predictors of young adult weight. Arch. Pediatr. Adolesc. Med. 2008;162(1):29–33. doi: 10.1001/archpediatrics.2007.14. [DOI] [PubMed] [Google Scholar]
- Moher D., Hopewell S., Schulz K.F. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340 doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mura G., Rocha N.B., Helmich I. Physical activity interventions in schools for improving lifestyle in European countries. CP & EMH. 2015;11(Suppl. 1 M5):77. doi: 10.2174/1745017901511010077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor P., Nettlefold L., Race D. Implementation of school based physical activity interventions: a systematic review. Prev. Med. 2015 doi: 10.1016/j.ypmed.2014.12.034. [DOI] [PubMed] [Google Scholar]
- Ortega F.B., Artero E.G., Ruiz J.R. Reliability of health-related physical fitness tests in European adolescents. The HELENA Study. Int. J. Obes. 2008;32:S49–S57. doi: 10.1038/ijo.2008.183. [DOI] [PubMed] [Google Scholar]
- Owen K.B., Astell-Burt T., Lonsdale C. The relationship between self-determined motivation and physical activity in adolescent boys. J. Adolesc. Health. 2013;53(3):420–422. doi: 10.1016/j.jadohealth.2013.05.007. [DOI] [PubMed] [Google Scholar]
- Owen K.B., Smith J., Lubans D.R. Self-determined motivation and physical activity in children and adolescents: a systematic review and meta-analysis. Prev. Med. 2014;67:270–279. doi: 10.1016/j.ypmed.2014.07.033. [DOI] [PubMed] [Google Scholar]
- Pate R.R., Daniels S. Institute of Medicine report on fitness measures and health outcomes in youth. JAMA Pediatr. 2013;167(3):221–222. doi: 10.1001/jamapediatrics.2013.1464. [DOI] [PubMed] [Google Scholar]
- Racil G., Ben Ounis O., Hammouda O. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur. J. Appl. Physiol. 2013;113(10):2531–2540. doi: 10.1007/s00421-013-2689-5. [DOI] [PubMed] [Google Scholar]
- Rosenkranz R.R., Lubans D.R., Peralta L.R. A cluster-randomized controlled trial of strategies to increase adolescents' physical activity and motivation during physical education lessons: the motivating active learning in physical education (MALP) trial. BMC Public Health. 2012;12(1):834. doi: 10.1186/1471-2458-12-834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J.J., Morgan P.J., Plotnikoff R.C. Smart-phone obesity prevention trial for adolescent boys in low-income communities: the ATLAS RCT. Pediatrics. 2014;134(3):e723–e731. doi: 10.1542/peds.2014-1012. [DOI] [PubMed] [Google Scholar]
- Standage M., Gillison F.B., Ntoumanis N. Predicting students' physical activity and health-related well-being: a prospective cross-domain investigation of motivation across school physical education and exercise settings. J. Sport Exerc. Psychol. 2012;34:37–60. doi: 10.1123/jsep.34.1.37. [DOI] [PubMed] [Google Scholar]
- Thompson D., Cantu D., Bhatt R. Texting to increase physical activity among teenagers (TXT Me!): rationale, design, and methods proposal. JMIR Res. Protoc. 2014;3(1) doi: 10.2196/resprot.3074. (e1410.2196/resprot.3074) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjønna A.E., Stølen T.O., Bye A. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clin. Sci. 2009;116(4):317–326. doi: 10.1042/CS20080249. [DOI] [PubMed] [Google Scholar]
- Tomkinson G.R., Oliver S. Secular changes in pediatric aerobic fitness test performance: the global picture. Med. Sport Sci. 2007;50:46–68. doi: 10.1159/000101075. (10.1159/000101075) [DOI] [PubMed] [Google Scholar]
- Twig G., Afek A., Shamiss A. Adolescence BMI and trends in adulthood mortality: a study of 2.16 million adolescents. J. Clin. Endocrinol. Metab. 2014;99(6):2095–2103. doi: 10.1210/jc.2014-1213. [DOI] [PubMed] [Google Scholar]
- Verloigne M., De Bourdeaudhuij I., Tanghe A. Self-determined motivation towards physical activity in adolescents treated for obesity: an observational study. Int. J. Behav. Nutr. Phys. Act. 2011;8(1):97–107. doi: 10.1186/1479-5868-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierling K.K., Standage M., Treasure D.C. Predicting attitudes and physical activity in an “at-risk” minority youth sample: a test of self-determination theory. Psychol. Sport Exerc. 2007;8(5):795–817. [Google Scholar]
- Weber D.R., Leonard M.B., Shults J. A comparison of fat and lean body mass index to BMI for the identification of metabolic syndrome in children and adolescents. J. Clin. Endocrinol. Metab. 2014;99(9):3208–3216. doi: 10.1210/jc.2014-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston K.S., Wisløff U., Coombes J.S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. BJSM. 2013 doi: 10.1136/bjsports-2013-092576. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document.