Abstract
Carbon monoxide (CO) poisoning is common in the United States, accounting for hundreds of deaths and thousands of emergency department visits annually. It is believed that most accidental CO poisoning is preventable through public education, warning labels on consumer products, and uniform use of residential CO alarms. However, cost effectiveness of these prevention strategies has not been demonstrated in the United States to date. It was the objective of this study to estimate societal cost of accidental CO poisoning and evaluate the cost-effectiveness of universal installation of residential CO alarms.
Published studies and data from the English language literature were used in to estimate direct hospital costs and lost earnings resulting from accidental CO poisoning. The study was performed in the US in 2015.
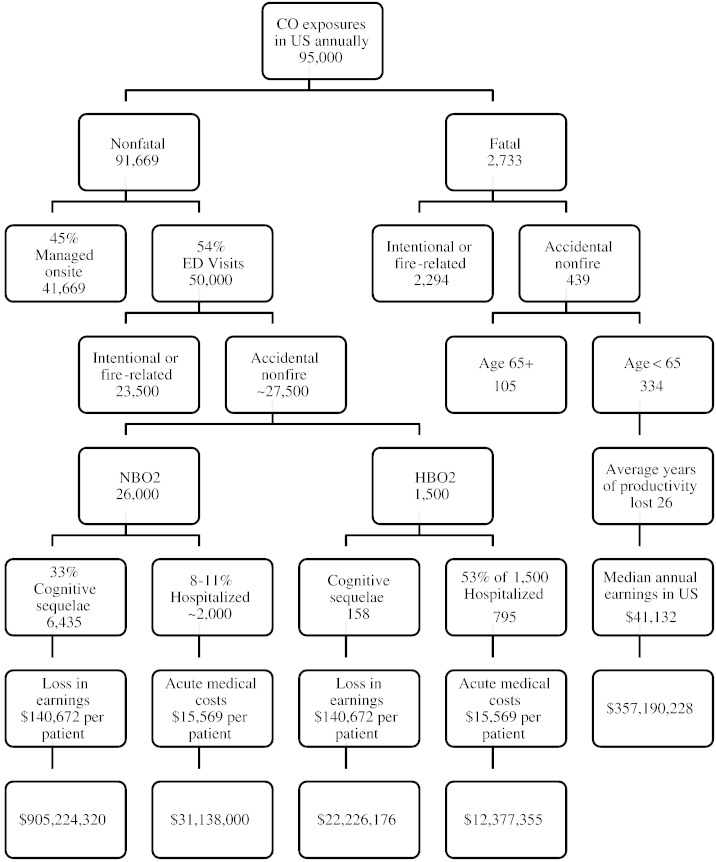
Approximately 6600 individuals are estimated to sustain long-term cognitive sequela annually, with total loss in earnings of approximately $925 million, 334 individuals die from accidental, non-fire related CO poisoning with an average loss of 26 years of productivity accounting for $355 million, and 2800 are hospitalized with acute medical care costs of $33 million.
Available data indicate that accidental CO poisoning in the US conservatively costs society over $1.3 billion, resulting from direct hospital costs and lost earnings. Further, it demonstrates a positive cost-benefit ratio for the uniform use of residential CO alarms.
Keywords: Carbon monoxide poisoning, Prevention, Cost
Highlights
-
•
CO poisoning results in acute hospitalization costs and lost wages due to disability and death.
-
•
Accidental, non-fire related poisoning accounts for over $1.3 billion annually in societal costs.
-
•
This estimate of costs is a conservative figure and the true costs are probably much higher.
-
•
Residential carbon monoxide alarms are cost-effective in prevention of accidental poisoning.
Introduction
Carbon monoxide (CO) poisoning is a major health problem in the United States, accounting for thousands of deaths and tens of thousands of healthcare visits annually. CO poisoning can be accidental or intentional, with suicidal poisoning accounting for the majority of deaths. It is generally believed that most accidental CO poisonings are preventable through use of public education, warning labels on consumer products, and residential CO alarms.
CO poisoning does not result in only acute care costs from emergency department visits and hospitalizations. Cognitive impairment from neurologic injury is CO poisoning's most common and serious chronic sequelae. Since a majority of CO poisoned individuals are 15 to 44 years old (Centers for Disease Control and Prevention, 2008), cognitive dysfunction or death affecting ability to work may impact earning potential for decades, with lost wages dwarfing acute medical costs.
In order to appropriately prioritize government spending for programs such as disease prevention through education or development of effective warning labels, one must estimate the cost of the disease burden on society. Only one cost-benefit analysis of residential CO poisoning prevention has been published to date, performed in Great Britain (Mason and Brown, 2010, UK Department of Communities and Local Governments, na). While it favored the use of CO alarms, applicability to the US is unknown. The large body of information published on CO poisoning in the US over the past two decades now makes it possible to estimate the annual cost of potentially preventable accidental poisoning. When done, decisions regarding allocation of finite resources can be made from a position of knowledge rather than opinion.
Accidental nonfatal CO poisoning
Incidence
The US Centers for Disease Control and Prevention (CDC) estimated 15,200 emergency department (ED) visits annually from 2001–2003 for nonfatal, accidental, non-fire-related CO exposure (Centers for Disease Control and Prevention, 2005). Cases with unknown intent of poisoning were included as accidental. CO exposures occurred in homes in 64%. The investigators tracked disposition of cases from the ED, noting that 11% were hospitalized.
The CDC subsequently revised the number of ED visits to 20,626 annually from 2004–2006, the increase felt possibly to be the result of improved data acquisition (Centers for Disease Control and Prevention, 2008). Residential exposures accounted for 73% of cases and 8% of those seen in an ED were hospitalized.
In 2007, Hampson and Weaver used ED visit rates for CO poisoning from five states to extrapolate an estimate of 50,000 CO-related ED visits for accidental and intentional cases combined in the US annually (Hampson and Weaver, 2007). Data from the states analyzed were corrected for known regional variation in CO exposure (Centers for Disease Control and Prevention, 2007) when calculating the national estimate.
Accidental vs. intentional poisoning
Since prevention initiatives are more likely to mitigate accidental than intentional poisoning, it is reasonable to limit estimates of disease cost to accidental cases. The most accurate information differentiating numbers of accidental and intentional exposures comes from death certificate data. However, because CO is such an effective poison and those determined to commit suicide are not likely to leave the contaminated environment or seek medical care, CO death data are biased toward intentional poisonings and will not accurately reflect the distribution of non-fatal poisonings.
In a series of 1473 CO poisonings treated at one institution from 1978 to 2005, 1435 were nonfatal (Hampson and Hauff, 2008). Of these, 1007 (70%) were accidental and 854 (60%) were both accidental and non-fire related. The intent was unknown for seven patients and these were included in the accidental group, as per earlier studies (Centers for Disease Control and Prevention, 2008, Centers for Disease Control and Prevention, 2005).
The Undersea and Hyperbaric Medical Society, in conjunction with the CDC, operated a voluntary national surveillance program of CO poisoning cases treated with hyperbaric oxygen from 2008 to 2011 (Hampson et al., 2012). Among 1915 patients reported over 36 months, 1641 (86%) were accidental and 1494 (78%) both accidental and non-fire related. The intent was unknown for 36 patients and they were included in the accidental group. Exposures were residential in 73%. These two large series suggest that it is reasonable to use 70–85% as an estimate for the frequency of CO exposures in the US that are nonfatal and accidental, and 60–78% for the frequency of nonfatal, accidental and non-fire related.
If 70% is applied to the 50,000 ED visit estimate above (Hampson and Weaver, 2007), a number of 35,000 accidental, non-fire ED visits for CO exposure annually is achieved. This is of similar magnitude as the CDC estimate of 20,626 visits for this category (Centers for Disease Control and Prevention, 2008). As such, 27,500 is used as the incidence figure for this subgroup in these calculations (Fig. 1).
Fig. 1.
Annual costs of accidental carbon monoxide poisoning. Analysis performed in the United States in 2015.
Cost of nonfatal CO poisonings
According to the National Poison Data System, 45% of CO exposure cases reported to US poison control centers from 2000–2009 were managed at the scene and 54% transported to health-care facilities (Centers for Disease Control and Prevention, 2011). Poisonings occurred in a residence in 78%. “Health-care facility” is not defined in the report cited, but is assumed to be an ED for the purposes of this analysis. No data exist from which to estimate the costs associated with those not receiving medical management, although some proportion of even mildly poisoned patients will develop cognitive and affective disorders (Chambers et al., 2008), thereby incurring costs for subsequent medical care.
In a report prepared by US Consumer Product Commission, contactors tasked with determining the cost of a case of accidental, non-fire, non-motor vehicle CO poisoning, a charge of $15,769 was calculated for acute medical care of cases admitted to the hospital (Miller and Bhattacharya, 2013). They also estimated an average 15% loss in lifetime earnings for those suffering from cognitive dysfunction following poisoning and assigned this a value of $140,672 per affected individual, based upon estimated lifetime earnings of $937,835 as calculated from the age and sex distribution of the series of 1915 CO-poisoned patients reported earlier (Hampson et al., 2012).
In a 2002 study by Weaver et al., CO-poisoned patients were randomized to hyperbaric or normobaric oxygen treatment, then followed with neuropsychiatric testing for twelve months (Weaver et al., 2002). The incidence of cognitive abnormality on testing at one year was 18% in the hyperbaric group and 33% in the normobaric oxygen group. In Weaver's study, 5% of 460 patients diagnosed with CO poisoning in an ED and assessed for enrollment were excluded due to delay greater than 24 h. Weaver also excluded patients less than 16 years of age, accounting for another 20% of the population assessed.
Since the incidence of chronic cognitive abnormality in these last two subgroups is therefore unknown, it will be assumed that the incidence is zero to be conservative and they are removed from the calculation of patients with chronic sequelae. It has been estimated that 1500 CO poisoned patients are referred for hyperbaric oxygen therapy annually (Hampson and Little, 2005). Of these 1500 receiving hyperbaric oxygen, 78% or 1170 patients would be expected to be accidental non-fire related, as noted earlier (Hampson et al., 2012). Removing 25% from that at-risk pool leaves 878, about 158 of whom (18%) would be predicted to develop chronic brain injury. After removing 25% from the remaining 26,000 ED visits for accidental non-fire CO poisoning treated with normobaric oxygen, about 19,000 remain at risk and some 6435 (33%) are predicted to develop chronic brain injury
Loss of lifetime earnings is estimated to average $140,672 per individual experiencing cognitive brain damage due to CO poisoning (Miller and Bhattacharya, 2013). Combining those manifesting persistent sequelae who receive hyperbaric oxygen (158) with those treated with normobaric oxygen (6435) results in a composite loss of earnings of $927,450,496.
While about one-half (53%) of all hyperbaric-treated patients are admitted to the hospital (Hampson et al., 2012), only 8–11% of all ED visits for accidental, non-fire related CO poisonings are admitted (Centers for Disease Control and Prevention, 2008, Centers for Disease Control and Prevention, 2005, Iqbal et al., 2012). If 10% is applied to the 27,500 ED visit patients, 2750 are hospitalized annually. This includes 53% of the 1500 patients (795) who receive hyperbaric oxygen therapy and the balance (about 2000) from those treated with normobaric oxygen. The 2750 who are admitted each year account for acute care charges totaling $43,515,355.
Accidental fatal CO poisoning
In 2007, the CDC published estimates of death from CO poisoning for the period 1999–2004 (Centers for Disease Control and Prevention, 2007). Mortality rates were calculated from death certificate data obtained from the National Vital Statistics System. For the six-year period examined, 16,400 CO total deaths occurred; 2631 (16%) accidental, non-fire related and 13,764 intentional and/or fire-related. An average of 439 deaths per year were accidental and non-fire-related. Of these, 334 annually were less than age 65 years.
If one assumes that the average person's productive working life is 47 years (age 18–65) and applies the age distribution of accidental, non-fire CO deaths in the CDC report (Centers for Disease Control and Prevention, 2007), an average loss of 26 years of productivity per death is calculated. In 2014, median per capita annual income in the US was $41,132 (Bureau of Labor Statistics and United States Department of Labor). Using these figures, the accidental non-fire-related deaths that occur in the US each year account for an estimated societal loss in productivity of $357,190,288.
Discussion
Accidental, non-fire-related CO poisoning in the US appears to account for over $1.3 billion in acute medical expenses and lost earnings annually. At many decision points in this analysis, there was a range of choices available and a midrange estimate was utilized in each instance. As such, the actual societal cost of accidental CO poisoning is likely much higher than is calculated here. It should also be emphasized that this cost is annual and recurring.
The study was limited by the inability to include several intangible costs, further contributing to underestimation. This unknown cost of long-term medical care for brain-injured individuals, either those that come through the medical system and are counted as having cognitive sequelae or the unquantifiable number who never seek acute medical care for their CO exposure was not included. Those who survive acute CO poisoning have been shown to have an increased rate of death compared to the normal population (Hampson et al., 2009) and the related loss of earnings from premature death was not counted. In addition, moderate to severe traumatic brain injury has been shown to be associated with an increased risk of dementia over 5–7 years, even in those less than 65 years old (Gardner et al., 2014). If this also occurs with CO-associated brain injury, health care costs and loss of wages would be incurred.
If public education programs, development of effective warning labels and universal application of home CO alarms can significantly impact the incidence of accidental CO poisoning as is believed, the investment appears favorable from a cost-benefit ratio. Residential CO alarms will be used as an example to illustrate this
These devices typically cost from $15–60 and contain CO sensors that last five to ten years, depending upon the model. For the purposes of this analysis, a $45 model with a sealed battery and lasting ten years with no maintenance costs will be used (The Home Depot).
If such a CO alarm were installed in each of the 115 million households in the US (United States Census Bureau), the annual expense would be $517 million. To be cost effective, it would be necessary for alarms to reduce accidental, non-fire CO costs by at least 39% (reducing CO costs from $1.33 billion to $813 million). Since approximately 70% of accidental non-fire exposures are residential and this is the location where these devices would be installed, home exposures would need to be reduced 55% by CO alarms to achieve this degree of cost savings.
No large studies have been published that examine the effectiveness of CO alarms in preventing CO exposure. On the other hand, smoke alarms for prevention of fire injury have been in residential use much longer and are currently present in 96–97% of US homes (Ahrens M. National Fire Protection Agency, 2014). Extensive experience with their performance is available. The risk of injury or death from home fires is reduced 88% in residences with operational smoke alarms, as compared to those without (Ahrens M. National Fire Protection Agency, 2014). In the British cost-benefit analysis of residential CO alarms, 75% effectiveness was utilized (UK Department of Communities and Local Governments).
If residential CO alarms are as effective as smoke alarms, or even 75% as effective, the cost-benefit ratio for their universal application is overwhelmingly favorable. Benefit from CO poisoning prevention initiatives that are less costly, such as development of enduring public education materials or product warning labels, have the potential to be even more cost-effective. Overall, accidental carbon monoxide poisoning should be seen as largely preventable and the societal benefit from expenditures to do this positive in every regard.
Conflict of interest statement
The author declares that there are no conflicts of interest.
References
- Ahrens M. Smoke alarms in U.S. home fires. National Fire Protection Agency March 2014. http://www.nfpa.org/research/reports-and-statistics/fire-safety-equipment/smoke-alarms-in-us-home-fires (Accessed August 13, 2015)
- Bureau of Labor Statistics, United States Department of Labor Labor force statistics from the current population survey. http://www.bls.gov/cps/cpsaat39.htm (Accessed November 20, 2015)
- Centers for Disease Control and Prevention Unintentional non-fire-related carbon monoxide exposures — United States, 2001–2003. MMWR. 2005;54:36–39. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Carbon monoxide-related deaths — United States, 1999–2004. MMWR. 2007;56(50):1309–1312. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Nonfatal, unintentional non-fire-related carbon monoxide exposures — United States 2004–2006. MMWR. 2008;57:896–899. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Carbon monoxide exposures — United States, 2000–2009. MMWR. 2011;60:1014–1017. [PubMed] [Google Scholar]
- Chambers C.A., Hopkins R.O., Weaver L.K., Key C. Cognitive and affective outcomes of more severe compared to less severe carbon monoxide poisoning. Brain Inj. 2008;22:387–395. doi: 10.1080/02699050802008075. [DOI] [PubMed] [Google Scholar]
- Gardner R.C., Burke J.F., Netticksimmons J., Kaup A., Barnes D.E., Yaffe K. Dementia risk after traumatic brain injury vs. nonbrain injury: the role of age and severity. JAMA Neurol. 2014;71(12):1490–1499. doi: 10.1001/jamaneurol.2014.2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson N.B., Hauff N.M. Risk factors for short term mortality from carbon monoxide poisoning treated with hyperbaric oxygen. Crit. Care Med. 2008;36(9):2523–2527. doi: 10.1097/CCM.0b013e31818419d8. [DOI] [PubMed] [Google Scholar]
- Hampson N.B., Little C.E. Hyperbaric treatment of patients with carbon monoxide poisoning in the United States. Undersea Hyperb. Med. 2005;32:21–26. [PubMed] [Google Scholar]
- Hampson N.B., Weaver L.K. Carbon monoxide poisoning: a new incidence for an old disease. Undersea Hyperb. Med. 2007;34(3):163–168. [PubMed] [Google Scholar]
- Hampson N.B., Hauff N.M., Rudd R.A. Increased long-term mortality among survivors of acute carbon monoxide poisoning. Crit. Care Med. 2009;37(6):1941–1947. doi: 10.1097/CCM.0b013e3181a0064f. [DOI] [PubMed] [Google Scholar]
- Hampson N.B., Dunn S.L., Yip S.Y., Clower J.H., Weaver L.K. The UHMS/CDC carbon monoxide poisoning surveillance program: three-year data. Undersea Hyperb. Med. 2012;39(2):667–685. [PubMed] [Google Scholar]
- Iqbal S., Law H.Z., Clower J.H., Yip F.Y., Elixhauser A. Hospital burden of carbon monoxide poisoning in the United States — 2007. Am. J. Emerg. Med. 2012;30(5):657–664. doi: 10.1016/j.ajem.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Mason J., Brown M.J. Estimates of costs for housing-related interventions to prevent specific illnesses and deaths. J. Public Health Manag. Pract. 2010;16(5 Suppl.):579–589. doi: 10.1097/PHH.0b013e3181e28b2e. [DOI] [PubMed] [Google Scholar]
- Miller T., Bhattacharya S. Incidence and cost of carbon monoxide poisoning for all ages, pool and spa submersions for ages 0–14, and lead poisoning for ages 0–4. Final report. Consumer Product Safety Commission Contract D-09-003. 2013. http://www.cpsc.gov//Global/Research-and-Statistics/Injury-Statistics/Carbon-Monoxide-Posioning/IncidenceandCostofCarbonMonoxidePoisoningPoolandSpaSubmersionandLeadPosioning.pdf (March 28, Accessed November 20, 2015)
- The Home Depot Worry Free 10-year Lithium Ion Battery Operated CO Alarm with Digital Display. http://www.homedepot.com/p/Kidde-Worry-Free-10-Year-Lithium-Ion-Battery-Operated-CO-Alarm-with-Digital-Display-21009720/203728677 (Accessed November 20, 2015)
- UK Department of Communities and Local Governments Study on the provision of CO detectors under the building regulations(BD2754) http://webarchive.nationalarchives.gov.uk/20120919132719/http://www.communities.gov.uk/documents/planningandbuilding/pdf/1324663 (Accessed November 20, 2015)
- United States Census Bureau Quick facts United States. U.S. Department of Commerce. http://quickfacts.census.gov/qfd/states/00000.html (Accessed August 13, 2015)
- Weaver L.K., Hopkins R.O., Chan K.J. Hyperbaric oxygen for acute carbon monoxide poisoning. N. Engl. J. Med. 2002;347(14):1057–1067. doi: 10.1056/NEJMoa013121. [DOI] [PubMed] [Google Scholar]