Abstract
Objective
To investigate correlates of changes in waist-to-height ratio (WHtR) in primary school children in order to identify modifiable factors usable for prevention.
Methods
Outcome evaluation of a statewide health promotion program in Baden-Württemberg, Germany. Baseline (2010) and follow-up (2011) measurements provided data for the calculation of changes in WHtR. Further information on the health and living conditions of the children were assessed in parental questionnaires. Anthropometric measures were taken in 1733 (50.8% male) first and second grade children (age at baseline 7.1 ± 0.6 years) by staff trained according to ISAK-standards. Stepwise linear regression analysis was applied to identify variables with influence on changes in WHtR.
Results
According to the resulting regression model, changes in WHtR towards an increase were influenced by at least one parent being overweight/obese, at least one parent who smoked, low household income, higher age of the child and the skipping of breakfast. There was no clustering effect in schools observed.
Conclusion
A promising target for prevention of gain in WHtR in primary school children is to ensure the regularity of breakfast. Smoking cessation as well as dietary improvements would not only help children's health but also the health of their parents. The socioeconomic influence on the development of an unhealthy weight status has already been acknowledged and should be extensively targeted by all of society and policy makers.
Keywords (MeSH): Abdominal obesity, Etiology, Prevention & control, Child, Food habits
Introduction
Abdominal obesity is an underestimated, if not ignored, health risk with a high contribution to several non-communicable diseases (NCD) (Smith and Haslam, 2007, Balkau et al., 2007, Scholze et al., 2007). To define abdominal obesity, a threshold of waist-to-height ratio (WHtR) of 0.5 as recommended by Ashwell and Hsieh (Ashwell & Hsieh, 2005), and confirmed in the systematic review by Browning et al. (Browning et al., 2010) can be used and is also applicable for children. Some researchers have detected rising numbers of abdominal obesity in children (Griffiths et al., 2013, Garnett et al., 2011, Li et al., 2006), while others have reported a leveling off in terms of overweight and obesity defined by body mass index (BMI) (Olds et al., 2011, Rokholm et al., 2010, Wabitsch et al., 2014). The latter may, inter alia, be due to the fact that BMI fails to identify over a quarter of children with excess body fat percentage (Javed et al., 2014). Abdominal obesity is very likely to continue from childhood to adolescence (Chrzanowska et al., 2012). Children with abdominal obesity experience lower health-related quality of life (HRQoL), are more often sick, and have more visits to a physician than their lean peers (Kesztyüs et al., 2013, Kesztyüs et al., 2014). Each missed day at school implies a hazard to academic achievement and each additional visit to a physician is related to higher health care costs (Kesztyüs et al., 2013).
Obesity and NCDs pose an enormous economic burden on states and national economies. Macroeconomic simulations suggest a cumulative output loss of 75% of global GDP in 2010 for NCDs (Bloom et al., 2011). The direct costs of obesity are estimated to €22.4 billion in Germany in 2020, plus indirect costs of €3.3 billion through losses in productivity (Knoll & Hauner, 2008). In the United States, obesity-attributable medical costs for non-institutionalized adults were estimated at $190.2 billion or 20.6% of national health expenditures in 2005 (Cawley, 2013). Additionally, childhood obesity was responsible for $14.1 billion in direct medical costs annually (2002–2005) (Trasande & Chatterjee, 2009). An early implementation of evidence-based health promotion in childhood could help to reverse the trend, but successful and cost-effective programs are rare (Waters et al., 2011, Langford et al., 2014). For abdominal obesity in children, it is crucial to find associated factors that are modifiable and can be targeted by preventive measures.
There is a vast amount of literature concerning correlates of weight gain based on BMI, but little is known on the factors leading to abdominal obesity in school children. The importance of this measure especially in children in comparison to BMI is described above. To our knowledge, this is the first study investigating correlates of longitudinal changes in WHtR in primary school children, representing changes in abdominal obesity. The aim is to identify modifiable correlates of changes in WHtR in primary schoolchildren and to consider their usability for primary prevention and health promotion.
Materials and methods
Study design
This research is based on the outcome evaluation of a health promotion program for primary schools in the state of Baden-Württemberg, Germany. The underlying program “Join the healthy boat” provides scientifically developed materials for teachers, pupils and their parents aiming at the development of healthy choices and a healthy lifestyle. To assess the effects, a cluster-randomized controlled trial (“Baden-Württemberg Study”) was set up, with baseline measurements in 2010 and a follow-up after one year in 2011. The ethics committee of Ulm University approved the study protocol and the study is registered on the German Clinical Trials Register (DRKS) under the DRKS-ID: DRKS00000494. Details on the study have already been published elsewhere (Dreyhaupt et al., 2012).
Participants and data
Parents were asked for their written informed consent. Data from direct measurements of children's height, weight and waist circumference (WC) at both baseline and follow-up, were available for 1733 participants, data from parental questionnaires for 1545 (89%) participants. Parents provided information on their own lifestyles, health behavior, and anthropometric data and the lifestyle, health behavior, physical activity patterns and the living environment of their children.
Demographics
The parental level of education was assessed and assigned to the respective level according to the CASMIN classification (Brauns & Steinmann, 1999). Family education level was determined as the highest level of two parents or the level of a single parent who cared for the child. Family education was dichotomized for analysis; elementary and intermediate education levels were taken together in one group, tertiary level in another. The child's migration background was defined as at least one parent being born abroad or at least one parent mainly having spoken a foreign language during the child's first years of life. Household income was graded according to the German KiGGS survey (Lange et al., 2007) and dichotomized for analysis into two groups, the lower group including monthly household incomes of < €1750.
Health and lifestyle characteristics
Parents gave information about maternal smoking during pregnancy, and breastfeeding. Items concerning children's behavior were taken from the validated questionnaires of the German KiGGS survey (Kurth, 2007). They were answered using a 5-point Likert scale: frequency of consuming softdrinks, frequency of playing outside (nearly every day, 3–5 times a week,1–2 times a week, less than 1 time a week, never), and time spent with screen media (never, about 30 min/day, about 1–2 h/day, about 3–4 h/day, more than 4 h/day). Variables were dichotomized for analyses (soft drinks > 1 time per week, playing outside > 60 min/day, screen media > 1 h/day). Parents stated the frequency of breakfast before school for their children on a 4-point scale, the results were subsequently dichotomized for analyses (never, rarely vs. often, always). Furthermore, they were asked on how many days a week their children were physically active on a moderate to vigorous level for at least 60 min a day, as recommended by the WHO (World Health Organisation (WHO), 2010). This variable was dichotomized for analyses at the median (physically active ≥ 4 days/week ≥ 60 min/day). Additionally, parents gave information about their own health behavior such as smoking, and were asked to rate their health awareness on a 4-point scale, the results were then dichotomized for analyses (not at all, little vs. strong, very strong).
Anthropometric measurements
Anthropometric measurements of the children were taken by trained staff according to ISAK-standards (Marfell-Jones et al., 2006). The children's height was measured to the nearest 0.1 cm (Stadiometer, Seca®, Germany), and body weight to the nearest 0.1 kg using calibrated and balanced portable digital scales (Seca®, Germany). WC was measured midway between ileac crest and lower costal arch to the nearest 0.1 cm using a flexible metal tape (Lufkin Industries Inc., Texas, USA). The children's BMI was calculated as weight divided by height squared (kg/m2). Excess weight and obesity were defined at or above the 90th and 97th age- and gender-specific BMI percentiles according to German reference data (Kromeyer-Hauschild et al., 2001). WHtR was calculated as the ratio of WC and height in centimeters, and subsequently participants with a WHtR ≥ 0.5 were categorized as abdominally obese (McCarthy & Ashwell, 2006).
Parental BMI was calculated from self-reported weight and height data in the questionnaires, and categorized as overweight (BMI > 25.0) and obese (BMI > 30.0), according to the international classification of the World Health Organization (WHO) (World Health Organisation (WHO), 1995). Parental WHtR was calculated as the ratio of self-reported WC to height and abdominal obesity defined at and above a WHtR threshold of 0.5 (Vandenbroucke et al., 2007).
Missing data
Common to observational studies is the problem of missing data, which may lead to bias (Ahrens et al., 2014). Baseline differences between records with and without missing variables for the final regression model were examined as described in the statistical analysis section.
Statistical analyses
Differences in baseline characteristics between boys and girls as well as between participants with and without missing values for the final regression model were tested for their statistical significance. The Mann–Whitney-U test or t-test for continuous data and Fisher's exact test for categorical data were applied as appropriate to scale level and distribution of the data. The significance level was set at α < 0.05 for two-sided tests. All analyses were carried out using the statistical software packages IBM SPSS Release 21.0 for Windows (SPSSInc, Chicago, IL, USA).
The changes in height, WC and WHtR were calculated as the differences between the values at baseline and the respective values at follow-up. Because of their small size after the decimal point, the resulting numbers of WHtR were then multiplied by 102 in order to receive understandable and interpretable values in the regression model. Thus, one unit in dependent variable of the regression model represents 0.01 WHtR. Based on the relevance of content and association with the outcome, all variables listed in Table 1 were included in the stepwise, linear regression analysis as potential explanatory variables. To account for the clustering of data in schools, a possible school-effect was examined in a linear mixed model using the statistical software R Release 3.1.2 for Windows (http://cran.r-project.org/).
Table 1.
Baseline characteristics of participants in the Baden-Württemberg Study (2010–2011).
| Missing |
Girls |
Boys |
Total |
|
|---|---|---|---|---|
| Values | (n = 852) | (n = 881) | (n = 1733) | |
| Child characteristics | ||||
| Age, years [m (sd)] | 0 | 7.07 (.64) | 7.09 (.63) | 7.08 (.63) |
| Migration background, n (%) | 244 | 235 (31.6) | 227 (30.5) | 462 (31.0) |
| BMI, [m (sd)] | 0 | 15.99 (2.19) | 15.97 (2.08) | 15.98 (2.14) |
| BMIPERC, [m (sd)] | 0 | 48.96 (27.74) | 48.15 (27.57) | 48.55 (27.65) |
| Overweight, n (%) | 0 | 82 (9.6) | 83 (9.4) | 165 (9.5) |
| Obesity, n (%) | 0 | 30 (3.5) | 38 (4.3) | 68 (3.9) |
| Waist circumference, cm [m (sd)] | 0 | 55.15 (5.91)⁎⁎⁎ | 55.79 (5.54) | 55.48 (5.73) |
| Height, cm [m (sd)] | 0 | 123.21 (6.30)⁎⁎⁎ | 124.39 (6.35) | 123.81 (6.35) |
| WHtR, [m (sd)] | 0 | 0.45 (.04) | 0.45 (.04) | 0.45 (.04) |
| Abdominal obesity, n (%) | 0 | 78 (9.2)⁎ | 57 (6.5) | 135 (7.8) |
| Parental characteristics | ||||
| Single parent, n (%) | 218 | 85 (11.3) | 71 (9.3) | 156 (10.3) |
| Tertiary family educational level, n (%) | 269 | 237 (32.6) | 238 (32.3) | 475 (32.4) |
| Household income < €1750, n (%) | 381 | 88 (13.1) | 83 (12.2) | 171 (12.6) |
| Overweight (mother or father), n (%) | 374 | 492 (73.2) | 477 (69.4) | 969 (71.3) |
| Abdominal obesity (mother or father), n (%) | 838 | 382 (85.8) | 373 (82.9) | 755 (84.4) |
| Smoking (mother or father), n (%) | 222 | 281 (37.3) | 274 (36.2) | 555 (36.7) |
| Health awareness (mother), n (%) | 240 | 437 (58.5) | 436 (58.4) | 873 (58.5) |
| Health awareness (father), n (%) | 334 | 299 (43.0) | 325 (46.2) | 624 (44.6) |
| Health and lifestyle characteristics | ||||
| Maternal smoking during pregnancy, n (%) | 196 | 65 (8.5)⁎ | 91 (11.8) | 156 (10.1) |
| Breastfeeding, n (%) | 194 | 651 (85.1) | 535 (82.0) | 1286 (83.6) |
| Playing outside > 60 min/day, n (%) | 248 | 462 (62.9)⁎⁎⁎ | 558 (74.4) | 1020 (68.7) |
| Physically active ≥ 4 days/week ≥ 60 min/day, n (%) | 263 | 161 (22.1)⁎⁎⁎ | 238 (32.1) | 399 (27.1) |
| Screen media > 1 h/day, n (%) | 205 | 86 (11.3)⁎ | 119 (15.5) | 205 (13.4) |
| Soft drinks > 1 time per week, n (%) | 197 | 173 (22.6) | 191 (24.8) | 364 (23.7) |
| Skipping breakfast, n (%) | 195 | 116 (15.2)⁎⁎ | 82 (10.6) | 198 (12.9) |
m (sd), mean (standard deviation).
p < .05.
p < .01.
p < .001.
Results
Baseline characteristics
The primary school children who took part in this research had a mean age of 7.1 ± 0.6 years, 50.8% of them were boys. Table 1 shows the baseline characteristics of the participants. Significant differences between boys and girls occurred in anthropometric variables where girls had a slightly lower waist circumference and were less tall. Mothers of girls more often refrained from smoking during pregnancy. Boys more often played outside and reached higher levels of physical activity. Girls spent less time with screen media and more regularly had breakfast.
Changes in anthropometrics
Girls and boys gained height and WC between the baseline and follow-up measurements. For WHtR a slight reduction was observed. Table 2 shows the exact values for the changes in anthropometrics. There were no statistically significant differences between boys and girls.
Table 2.
Differences in anthropometric measures between baseline and follow-up in the Baden-Württemberg Study (2010–2011).
| Girls | Boys | Total | |
|---|---|---|---|
| Differences in WC, cm [m (sd)] | 1.70 (3.03) | 1.87 (2.77) | 1.78 (2.91) |
| Differences in height, cm [m (sd)] | 6.13 (1.29) | 6.18 (1.10) | 6.16 (1.20) |
| Differences in WHtR, [m (sd)] | − .0082 (.023) | − .0071 (.021) | − .0076 (.022) |
Note. N = 1733. WC Waist Circumference. WHtR Waist-to-Height Ratio.
m (sd), mean (standard deviation).
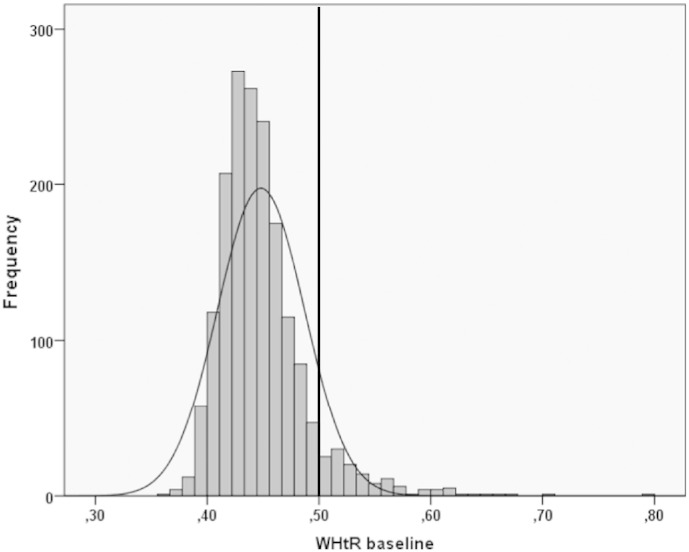
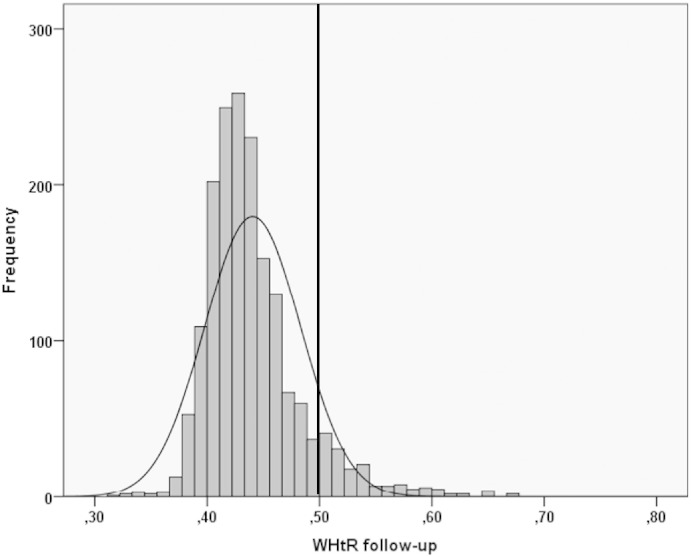
To visualize the distribution of WHtR, Fig. 1 shows a histogram of the data at baseline. The distribution is non-normal, with skewness of 2.04 (SE = .06) and kurtosis of 8.50 (SE = .12), whereas the data of the differences between baseline and follow-up are quasi-normally distributed (not shown). At follow-up, the histogram (Fig. 2) showed a distribution with skewness of 1.53 (SE = .06) and kurtosis of 3.95 (SE = .12), indicating a change in the shape of the distribution towards normality. However, the proportion of participants at and beyond the WHtR threshold of 0.5 indicating abdominal obesity is visibly higher (9.2% vs 7.8%, p < 0.001) at follow-up.
Fig. 1.
Histogram of the distribution of WHtR at baseline in the Baden-Württemberg Study (2010–2011). The added vertical line demarcates the threshold of 0.5 that indicates the borderline to abdominal obesity.
Fig. 2.
Histogram of the distribution of WHtR at follow-up in the Baden-Württemberg Study (2010–2011). The added vertical line demarcates the threshold of 0.5 that indicates the borderline to abdominal obesity.
Regression analysis of changes in WHtR
All variables depicted in Table 1 except for anthropometrics of the children were considered with regard to their potential influence on the outcome in the regression analysis. The final model consists of age, skipping breakfast, at least one parent smoking, at least one parent being overweight and household income below €1750. Because of the clustering of data in schools, the intra-class correlation coefficient (ICC) was calculated and revealed that 4.57% of the overall variance is attributable to differences between schools (95% CI [1.73, 7.41]). The underlying health promotion program did not show a significant influence on the metric changes in WHtR. Table 3 shows the results of the linear regression model and the linear mixed regression model, accounting for clustered data in schools.
Table 3.
Non-standardized estimators from a linear regression model (OLS) and fixed effects from a linear mixed regression model (ML) for changes in WHtR in the Baden-Württemberg Study (2010–2011).
| B (OLS) | B (ML) | |
|---|---|---|
| Intercept | − 3.04 (0.70)⁎⁎⁎ | − 3.10 (.74)⁎⁎⁎ |
| Age | .24 (0.10)⁎ | 0.25 (.10)⁎ |
| Skipping breakfast | .39 (.19)⁎ | .36 (.19)† |
| Smoking (mother or father) | .36 (.13)⁎⁎ | .36 (.13)⁎⁎ |
| Overweight (mother or father) | .49 (.13)⁎⁎⁎ | 0.43 (.13)⁎⁎ |
| Household income < €1750 | .77 (.20)⁎⁎⁎ | 0.79 (.20)⁎⁎⁎ |
| F (5, 1212) | 12.88⁎⁎⁎ | |
| R2 | 0.051 | |
| AIC | 5256 | 5258 |
Note. N = 1212. Estimates and standard errors (in parentheses). Ordinary least squares (OLS). Maximum likelihood (ML). Akaike's information criterion (AIC).
p < .10.
p < .05.
p < .010.
p < .001.
Missing data
Children with missing data in the independent variables were less likely to have been breastfed, were more likely to have a single parent, were significantly more often overweight, obese and abdominally obese. The average age of mothers at birth was lower and health awareness of fathers was significantly higher. At least one parent was more likely to be abdominally obese. Families more often had a household income of less than €1750 and they had a lower family education level.
Discussion
WHtR of first and second grade primary school children slightly decreased during one year with a mean of minus 0.0076 ± 0.022 between baseline and follow-up. This small overall change is physiologically not very significant and the minus may be mainly due to the natural process of growth of the children. Other researchers report similar small changes of WHtR in this age group (Ahrens et al., 2014). Nonetheless, the proportion of children at and beyond the threshold of WHtR = 0.5, marking the border to abdominal obesity, significantly increased. That makes it crucial to identify modifiable factors with influence on the increase in WHtR to set up targeted preventive measures. The most promising factor in this research is the regularity of breakfast, which can easily be addressed in all kind of interventions at different levels. At an interpersonal level, parents should be informed about the importance of regular breakfast, and at an organizational level, institutions like kindergarten and schools could offer regular breakfast for children. Breakfast frequency and quality may have positive effects for both parents and children (Pereira et al., 2011). Hence, the regularity of breakfast is also an important step in changing dietary patterns for overweight and obese parents, who represent another modifiable factor for changes in children's WHtR. The cessation of smoking as the third modifiable risk factor would have additional far-reaching positive effects on family health besides that of WHtR gain of children. As a further factor of influence, low household income is part of the economic and social disparities that are already well known contributors to the obesity epidemic (Loring & Robertson, 2014). Therefore, a special focus on the socially disadvantaged should always be an important part in developing measures for targeted prevention.
Strengths and limitations
The strength of this research lies within the strict protocol of a cluster-randomized controlled trial and the large number of children and parents that took part, covering the entire state of Baden-Württemberg. The response rate in terms of returned parental questionnaires was 89% at baseline and 87% at follow-up. The anthropometric measurements were of high quality, and taken by trained staff according to ISAK standards (Marfell-Jones et al., 2006). Both measurement periods were short, so that there were no significant differences in the time span between baseline and follow-up measurements per child that would have made it necessary to adjust for in the statistical analyses. Moreover, the possible clustering of data in schools was taken into account in the statistical analyses.
Limitations are mainly due to the observational character of the underlying study. Participation and data themselves may be biased in different ways. Concerning values of self-reported parental weight and smoking, eliminating underreporting and social desirability could result in a more distinct influence of parental excess weight and smoking on increases in children's WHtR. Nonetheless, particularly when keeping in mind underreporting and social desirability responding, the numbers of overweight and abdominal obese parents are alarming. Lastly, health-related behavior of the children like physical activity, screen media use and breakfast habits was not observed but was based on parental information.
Missing values occurred because parents did not return or completely fill in the questionnaires. This may lead to a form of selection bias, but in the best case, only lessen the precision of the study (Morshed et al., 2009). According to the differences in terms of explanatory variables detected in the missing data analysis, children with incomplete data share several critical characteristics, such as higher rates of abdominal obesity and lower household income. If these participants could have been included into the regression analysis, it would have of course accentuated the results.
Abdominal obesity
There is some discussion on how to define abdominal obesity. Some researchers consider WHtR as an accurate and practicable index to evaluate abdominal obesity, even in children and adolescents (Ashwell and Hsieh, 2005, McCarthy and Ashwell, 2006). In their systematic literature review, de Moraes et al. report that there is no consensus in the literature about the criteria to define abdominal obesity using WC (De Moraes et al., 2011). They report five different anatomical sites used for WC measurement and 18 different cut-off points, which makes it difficult to compare results. To adopt the procedure that is applied to define overweight and obesity according to age and sex specific percentiles for abdominal obesity, a representative reference group is needed. However, the German population in different regions is much too inhomogeneous, with regard to crucial determinants like socioeconomic status or migration background, to rely on such reference values. Therefore, WHtR as a measure of waist circumference adjusted to individual height is less biased than WC percentiles according to a reference group with differing background variables. Fact is, there is little doubt that already in childhood the health risk of abdominal obesity is higher than that of overall obesity (Reinehr and Wunsch, 2010, Rodríguez et al., 2004).
Correlates and risk factors in current research
Correlates of increases in WC and development of abdominal obesity in children is not subject to many investigations. According to results of Garnett et al., it may be assumed that most of the risk factors for general obesity also apply to abdominal obesity (Garnett et al., 2005). Another study by Taveras et al. found out that chronic sleep curtailment from infancy to mid-childhood was associated with total and central adiposity (Taveras et al., 2014). A further study in Malaysian adolescents confirms the present findings on the association of breakfast and abdominal obesity (Nurul-Fadhilah et al., 2013). A review of factors influencing visceral fat accumulation in children and adolescents reports a significant percentage of heritability but also differences due to sex, age and level of development. Moreover the author discusses stress, physical activity and positive energy balance in association with a higher amount of visceral adipose tissue (Suliga, 2009). Maternal smoking during pregnancy was found to be a risk factor for the development of abdominal obesity at later stages of puberty, but not for younger children (Syme et al., 2010) which confirms the present results where smoking during pregnancy was not significantly associated with changes in WHtR. Bradlee and colleagues did not find associations with food group intake and central obesity among children except for the meat intake among boys. For adolescents, they detected inverse associations with the intake of dairy, grains and total fruits and vegetables with central obesity (Bradlee et al., 2010). Kim and Lee report in their review on physical activity and abdominal obesity in youth limited evidence that aerobic types of exercise can alleviate the age-related increase in visceral fat in growing children and adolescents (Kim & Lee, 2009). The present study did not find significant associations between being physically active on at least three days a week or playing outside for a minimum of 60 min each day and changes in WHtR. Developing abdominal obesity is as multicausal as is developing general obesity and in this study we can only add a few pieces to the puzzle, therefore further research should be done to identify the crucial risk factors to initiate targeted preventive measures.
Conclusion
One promising target for the prevention of gain in WHtR in primary school children is to ensure the regularity of breakfast. Smoking cessation as well as dietary improvements in order to lose weight or to prevent further weight gain would not only help children's health but also the health of their parents. The socioeconomic influence on the development of an unhealthy weight status has already been acknowledged and should be extensively targeted by all of society and policy makers.
Conflict of interest
The authors declare that there are no conflicts of interest.
Acknowledgments
The program “Komm mit in das gesunde Boot — Grundschule” is financed by the Baden-Württemberg Stiftung. The Baden-Württemberg Stiftung had no influence on the content of the manuscript. Thanks to all members of the “Komm mit in das gesunde Boot” research group for their input. Most of all, we thank the teachers, pupils and their parents who participated in the Baden-Württemberg Study. Finally, we thank Sinéad McLaughlin for her language assistance.
References
- Ahrens W., Moreno L.A., Mårild S., Molnár D., Siani A., Henauw S. De. Metabolic syndrome in young children: definitions and results of the IDEFICS study. Int. J. Obes. 2014;38:S4–S14. doi: 10.1038/ijo.2014.130. [DOI] [PubMed] [Google Scholar]
- Ashwell M., Hsieh S.D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005;56(5):303–307. doi: 10.1080/09637480500195066. [DOI] [PubMed] [Google Scholar]
- Balkau B., Deanfield J.E., Després J.P., Bassand J.P., Fox K.A.A., Smith S.C. International day for the evaluation of abdominal obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168 000 primary care patients in 63 countries. Circulation. 2007;116(17):1942–1951. doi: 10.1161/CIRCULATIONAHA.106.676379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom D.E., Cafiero E.T., Jané-Llopis E., Abrahams-Gessel S., Bloom L.R., Fathima S. Geneva: World Economic Forum. 2011. The global economic burden of non-communicable diseases. [Google Scholar]
- Bradlee M.L., Singer M.R., Qureshi M.M., Moore L.L. Food group intake and central obesity among children and adolescents in the Third National Health and Nutrition Examination Survey (NHANES III) Public Health Nutr. 2010;13(6):797–805. doi: 10.1017/S1368980009991546. [DOI] [PubMed] [Google Scholar]
- Brauns H., Steinmann S. Educational reform in France, West-Germany and the United Kingdom: updating the CASMIN educational classification. ZUMA Nachr. 1999;23:7–44. [Google Scholar]
- Browning L.M., Hsieh S.D., Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0 · 5 could be a suitable global boundary value. Nutr. Res. Rev. 2010;23(2):247–269. doi: 10.1017/S0954422410000144. [DOI] [PubMed] [Google Scholar]
- Cawley J. NBER Reporter 2013 Number 4: Research Summary The Economics of Obesity [Internet] 2013. pp. 1–5.http://nber.org/reporter/2013number4/cawley.html (Available from:) [Google Scholar]
- Chrzanowska M., Suder A., Kruszelnicki P. Tracking and risk of abdominal obesity in the adolescence period in children aged 7–15. The cracow longitudinal growth study. Am. J. Hum. Biol. 2012;24(1):62–67. doi: 10.1002/ajhb.22204. [DOI] [PubMed] [Google Scholar]
- De Moraes C.F., Fadoni R.P., Ricardi L.M., Souza T.C., Rosaneli C.F., Nakashima T. Prevalence of abdominal obesity in adolescents: a systematic review. Obes. Rev. 2011;12(2):69–77. doi: 10.1111/j.1467-789X.2010.00753.x. [DOI] [PubMed] [Google Scholar]
- Dreyhaupt J., Koch B., Wirt T., Schreiber A., Brandstetter S., Kesztyüs D. Evaluation of a health promotion program in children: study protocol and design of the cluster-randomized Baden-Württemberg primary school study [DRKS-ID: DRKS00000494] BMC Public Health. 2012;12(1):157. doi: 10.1186/1471-2458-12-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett S.P., Cowell C.T., Baur L.A., Shrewsbury V.A., Chan A., Crawford D. Increasing central adiposity: the Nepean longitudinal study of young people aged 7–8 to 12–13 y. Int. J. Obes. 2005;29(11):1353–1360. doi: 10.1038/sj.ijo.0803038. [DOI] [PubMed] [Google Scholar]
- Garnett S.P., Baur L.A., Cowell C.T. The prevalence of increased central adiposity in Australian school children 1985 to 2007. Obes. Rev. 2011;12(15):887–896. doi: 10.1111/j.1467-789X.2011.00899.x. [DOI] [PubMed] [Google Scholar]
- Griffiths C., Gately P., Marchant P.R., Cooke C.B. A five year longitudinal study investigating the prevalence of childhood obesity: comparison of BMI and waist circumference. Public Health. 2013;127:1090–1096. doi: 10.1016/j.puhe.2013.09.020. [DOI] [PubMed] [Google Scholar]
- Javed A., Jumean M., Murad M.H., Okorodudu D., Kumar S., Somers V.K. Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis. Pediatr. Obes. 2014:1–11. doi: 10.1111/ijpo.242. [DOI] [PubMed] [Google Scholar]
- Kesztyüs D., Wirt T., Kobel S., Schreiber A., Kettner S., Dreyhaupt J. Is central obesity associated with poorer health and health-related quality of life in primary school children? Cross-sectional results from the Baden-Württemberg Study. BMC Public Health. 2013;13:260. doi: 10.1186/1471-2458-13-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesztyüs D., Schreiber A., Kobel S., Wartha O., Kesztyüs T., Kilian R. Illness and determinants of health-related quality of life in a cross-sectional sample of schoolchildren in different weight categories. Ger. Med. Sci. 2014;12 doi: 10.3205/000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Lee S. Physical activity and abdominal obesity in youth. Appl. Physiol. Nutr. Metab. 2009;34(4):571–581. doi: 10.1139/H09-066. [DOI] [PubMed] [Google Scholar]
- Knoll K.-P., Hauner H. Kosten der Adipositas in der Bundesrepublik Deutschland — Eine aktuelle Krankheitskostenstudie. Adipositas. 2008;2(4):204–210. [Google Scholar]
- Kromeyer-Hauschild K., Wabitsch M., Kunze D., Geller F., Geiß H.C., Hesse V. Perzentile für den Body-mass- Index für das Kindes- und Jugend- alter unter Heranziehung ver- schiedener deutscher Stichproben [Percentiles of bodymass index in children and adolescents evaluated from different regional German studies] Monatsschr. Kinderheilkd. 2001;149:807–818. [Google Scholar]
- Kurth B.-M. Der Kinder- und Jugendgesundheitssurvey (KiGGS): Ein Überblick über Planung, Durchführung und Ergebnisse unter Berücksichtigung von Aspekten eines Qualitätsmanagements TL — 50. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz. 2007;50(5–6):533–546. doi: 10.1007/s00103-007-0214-x. [DOI] [PubMed] [Google Scholar]
- Lange M., Kamtsiuris P., Lange C., Rosario A.S., Stolzenberg H., Lampert T. Messung soziodemographischer Merkmale im Kinder- und Jugendgesundheitssurvey (KiGGS) und ihre Bedeutung am Beispiel der Einschätzung des allgemeinen Gesundheitszustands [Sociodemographic characteristics in the German Health Interview and Examination Surve. Bundesgesundheitsbl. Gesundheitsforsch. Gesundheitsschutz. 2007;50(5–6):578–589. doi: 10.1007/s00103-007-0219-5. [DOI] [PubMed] [Google Scholar]
- Langford R., Bonell C.P., Jones H.E., Pouliou T., Murphy S.M., Waters E. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014;4(4) doi: 10.1002/14651858.CD008958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Ford E.S., Mokdad A.H., Cook S. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics. 2006;118(5):e1390–e1398. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- Loring B., Robertson A. Guidance for Addressing Inequities in Overweight and Obesity [Internet] World Health Organisation, Copenhagen; Copenhagen: 2014. Obesity and inequities; pp. 1–6.http://ec.europa.eu/health/social_determinants/docs/policybrief_obesity_en.pdf (Available from:) [Google Scholar]
- Marfell-Jones M., Olds T., Stewart A., Carter J.E.L., editors. International Standards for Anthropometric Assessment. North-West University; Potchefstroom, RSA: 2006. [Google Scholar]
- McCarthy H.D., Ashwell M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message —‘keep your waist circumference to less than half your height’. Int. J. Obes. 2006;30:988–992. doi: 10.1038/sj.ijo.0803226. [DOI] [PubMed] [Google Scholar]
- Morshed S., Tornetta P., Bhandari M. Analysis of observational studies: a guide to understanding statistical methods. J. Bone Joint Surg. Am. 2009;91(Suppl. 3):50–60. doi: 10.2106/JBJS.H.01577. [DOI] [PubMed] [Google Scholar]
- Nurul-Fadhilah A., Teo P.S., Huybrechts I., Foo L.H. Infrequent breakfast consumption is associated with higher body adiposity and abdominal obesity in Malaysian school-aged adolescents. PLoS One. 2013;8(3):1–6. doi: 10.1371/journal.pone.0059297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds T., Maher C., Zumin S., Péneau S., Lioret S., Castetbon K. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int. J. Pediatr. Obes. 2011;6(June):342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- Pereira M.A., Erickson E., McKee P., Schrankler K., Raatz S.K., Lytle L.A. Breakfast frequency and quality may affect glycemia and appetite in adults and children. J. Nutr. 2011;141(1):163–168. doi: 10.3945/jn.109.114405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinehr T., Wunsch R. Relationships between cardiovascular risk profile, ultrasonographic measurement of intra-abdominal adipose tissue, and waist circumference in obese children. Clin. Nutr. 2010;29(1):24–30. doi: 10.1016/j.clnu.2009.06.004. [DOI] [PubMed] [Google Scholar]
- Rodríguez G., Moreno L.A., Blay M.G., Blay V.A., Garagorri J.M., Sarría A. Body composition in adolescents: measurements and metabolic aspects. Int. J. Obes. Relat. Metab. Disord. 2004;28(Suppl. 3):S54–S58. doi: 10.1038/sj.ijo.0802805. [DOI] [PubMed] [Google Scholar]
- Rokholm B., Baker J.L., Sørensen T.I. The levelling off of the obesity epidemic since the year 1999 — a review of evidence and perspectives. Obes. Rev. 2010;11(12):835–846. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- Scholze J., Lilienthal W., Bramlage P. Kardiometabolische Hochrisikopatienten bei abdominaler Adipositas. MMW Fortschr. Med. 2007;149(S3):103–110. [PubMed] [Google Scholar]
- Smith S.C., Haslam D. Abdominal obesity, waist circumference and cardio-metabolic risk: awareness among primary care physicians, the general population and patients at risk—the Shape of the Nations survey. Curr. Med. Res. Opin. 2007;23(1):29–47. doi: 10.1185/030079906X159489. [DOI] [PubMed] [Google Scholar]
- Suliga E. Visceral adipose tissue in children and adolescents: a review. Nutr. Res. Rev. 2009;22(2):137–147. doi: 10.1017/S0954422409990096. [DOI] [PubMed] [Google Scholar]
- Syme C., Abrahamowicz M., Mahboubi A., Leonard G.T., Perron M., Richer L. Prenatal exposure to maternal cigarette smoking and accumulation of intra-abdominal fat during adolescence. Obesity (Silver Spring) 2010;18(5):1021–1025. doi: 10.1038/oby.2009.354. [DOI] [PubMed] [Google Scholar]
- Taveras E.M., Gillman M.W., Peña M.-M., Redline S., Rifas-Shiman S.L. Chronic sleep curtailment and adiposity. Pediatrics. 2014;133(6):1013–1022. doi: 10.1542/peds.2013-3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trasande L., Chatterjee S. The impact of obesity on health service utilization and costs in childhood. Obes (Silver Spring) 2009;17(9):1749–1754. doi: 10.1038/oby.2009.67. [DOI] [PubMed] [Google Scholar]
- Vandenbroucke J.P., Von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):1628–1654. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wabitsch M., Moss A., Kromeyer-Hauschild K. Unexpected plateauing of childhood obesity rates in developed countries. BMC Med. 2014;12:17. doi: 10.1186/1741-7015-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E., de Silva-Sanigorski A., Hall B.J., Brown T., Campbell K.J., Gao Y. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011;(12):1–212. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- World Health Organisation (WHO) World Health Organization technical report series. Report of a WHO Expert Committee; 1995. Physical status: the use and interpretation of anthropometry; p. 329. [PubMed] [Google Scholar]
- World Health Organisation (WHO) Global recommendations on physical activity for health. Geneva World Health Organ. 2010;60 [Google Scholar]