Abstract
OBJECTIVES
To examine the effect of the relationship between volume (number of hip fracture admissions during the 12 months before participant’s fracture) and other facility characteristics on outcomes.
DESIGN
Prospective observational study.
SETTING
U.S. skilled nursing facilities (SNFs) admitting individuals discharged from the hospital after treatment for hip fracture between 2000 and 2007 (N = 15,439).
PARTICIPANTS
Community-dwelling fee-for-service Medicare beneficiaries aged 75 and older admitted to U.S. hospitals for their first hip fracture and discharged to a SNF for postacute care from 2000 to 2007 (N = 512,967).
MEASUREMENTS
Successful discharge from SNF to community, defined as returning to the community within 30 days of hospital discharge to the SNF and remaining in the community without being institutionalized for at least 30 days, was examined using Medicare administrative data, propensity score matching, and instrumental variables.
RESULTS
The overall rate of successful discharge to the community was 31%. Of the 15,439 facilities, the facility interquartile range varied from 0% (25th percentile) to 42% (75th percentile). An important determinant of variation in discharge rate was SNF volume of hip fracture admissions. Unadjusted successful discharge from SNF to community was 43.7% in high-volume facilities (>24 admissions/year), versus 18.8% in low-volume facilities (1–6 admissions/year). This facility volume effect persisted after adjusting for participant and facility characteristics associated with outcomes (e.g., adjusted odds ratio = 2.06, 95% confidence interval = 1.91–2.21 for volume of 25 vs 3 admissions per year).
CONCLUSION
In community-dwelling persons with their first hip fracture, successful return to the community varies substantially according to SNF provider volume and staffing characteristics.
Keywords: volume effect, skilled nursing facility, postacute care, hip fracture
The Affordable Care Act and current initiatives by the Centers for Medicare and Medicaid Services have focused considerable attention on efforts such as pay for performance, accountable care organizations, and bundled hospital–postacute care (PAC) payments to improve quality of care and curtail growth in costs.1,2 An area of special interest in this regard is PAC after hospitalization. Medicare PAC expenditures doubled from $23 billion in 2000 to $49.5 billion in 2011, increasing from 27% to 42% of inpatient care expenditures.1,3,4 A recent Institute of Medicine study emphasized the importance of PAC use, reporting that PAC is by far the largest factor contributing to the substantial regional variation in Medicare spending, accounting for 73% of the unexplained variance across hospital referral regions (inpatient services was a distant second, explaining 27% of regional differences).5 Against this background, there is growing interest regarding the performance and quality of care of PAC providers.
Although PAC is provided in multiple healthcare settings, skilled nursing facilities (SNFs) are the most-common PAC setting, with a 63% share of posthospital PAC expenditures in 2011,4 but information on variation in PAC outcomes between SNF facilities and on the role of facility characteristics such as staffing and volume of hip fracture admissions in that variation is limited. Although a growing number of studies have found a relationship between staffing or facility volume of hip fracture admissions and quality in the acute care setting,6–15 little research has been done to examine this relationship in SNF care. A recent examination of all PAC admissions to U.S. SNFs found that facilities admitting more people had lower rehospitalization rates, but the authors did not differentiate between the effect of selection and the effect of volume per se, a problem that the heterogeneous population they studied exacerbated.16
Hip fracture is the fourth leading reason for admission of hospitalized individuals discharged to a SNF.17 For community-dwelling individuals experiencing their first hip fracture, the primary goal of PAC is being safely discharged to the community. To examine successful discharge to the community, Medicare claims and Minimum Data Set (MDS) assessments from 1999 through 2007 for all Medicare fee-for-service beneficiaries experiencing their first hip fracture were linked longitudinally. The objectives of the study were to document the differences in SNF discharge to community between facilities and to examine the relationship between selected SNF facility characteristics, such as staffing and volume of hip fracture admissions, and rate of successful return to the community of individuals with hip fracture. By isolating organizational factors associated with desired outcomes, providers can better target quality improvement efforts.
METHODS
Data Sources and Initial Cohort Definition
The cohort was defined using 100% Medicare inpatient claims to identify Medicare beneficiaries having their first hip fracture between 1999 and 2007 and using a 5-year look-back to confirm no previous hip fractures. Acute hip fracture was determined using the International Classification of Diseases, Ninth Edition, codes for hip fracture (820.00–820.32). The analytical sample included Medicare beneficiaries aged 75 and older at the time of the fracture (to exclude most trauma-induced fractures) discharged from a hospital in the 50 U.S. states with Medicare fee-for-service insurance and living in the community at the time of their fracture who underwent surgery repair within 30 days of hospital admission18 and were discharged to a SNF. Persons who died within 14 days of hospital discharge were excluded, because the nursing home (NH) may have been selected with knowledge of impending death. Individuals discharged from the hospital in 1999 (because facility volume was defined over the prior 12 months) or after October 1, 2007 (because their outcomes would be censored to follow-up) and those whose residence ZIP code was more than 150 miles away from the chosen SNF provider were also excluded. This resulted in a set of 512,967 community-dwelling individuals discharged to SNFs.
Beneficiaries’ Medicare enrollment file, Part A claims—consisting of inpatient, SNF, hospice, and home health services—their Medicare outpatient claims, and their MDS NH resident assessment records starting 1 year before their first hip fracture and ending December 31, 2007, were linked. The residential history file methodology was then used to construct a person-level longitudinal record detailing healthcare use and residential status (community vs institutionalized) over time.19
Skilled nursing facilities provider characteristics were obtained from two sources, the On-Line Survey Certification and Reporting System (OSCAR) annual survey that reports organizational, staffing, and resident characteristics and the website www.LTCFocUS.org, which contains provider summary data created from OSCAR, Medicare claims, and MDS records.20
Outcome Measure
For community-dwellers, the goal of hip fracture rehabilitation is successful discharge to the community. Therefore, a binary composite outcome measure denoting discharge to the community within 30 days of SNF admission and remaining in the community without institutionalization (hospitalization or admission to a PAC or NH) for at least 30 days was created. This composite outcome is a measure of the good quality of rehabilitative care that results in functional recovery that is fast (to return to the community setting as soon as possible) and sustained (allowing the individual to remain in the community longer).
Independent Variables and Potential Confounders
The primary independent variables were SNF provider characteristics. SNF volume was defined as the number of hip fracture admissions the SNF provider had during the 12 months before the participant’s fracture. Additional facility characteristics included whether the SNF was based in a hospital, its proprietary status, the number of beds, whether there was a dedicated rehabilitation unit, the number of registered nurses (RNs) and licensed practical nurses (LPNs) per 10 residents, the number of physical therapists (PTs) and occupational therapists (OTs) (therapists plus assistant therapists) per 10 residents receiving therapy, and the percentage of PTs and OTs who were employees versus contracted from outside the facility.21–23
Participant covariates included sociodemographic characteristics obtained from the Medicare enrollment file (age, race, sex) and characteristics obtained from the hip fracture hospitalization Medicare claims and from the admission MDS SNF assessment. Characteristics from the hospitalization included type of fracture (femoral neck vs pertrochanteric), occurrence of any hospital complications (e.g., postoperative myocardial infarction, postoperative deep venous thrombosis, pulmonary embolism, postoperative hemorrhage), surgical infection, surgical revision, the Elixhauser comorbidity measure24 as implemented by the Agency for Healthcare Research and Quality,25 any intensive care unit use, hospital length of stay (LOS), time to surgery from hospital admission, and indicators of whether the participant underwent surgery during his or her first hospitalization or was transferred to another hospital for surgery. Hospital annual volume of first hip fractures was also included to capture hospitals’ experience treating and discharging individuals with hip fracture. SNF admission MDS covariates included physical function as measured according to activity of daily living (ADL) ability, cognition, body mass index (BMI), comorbid diagnoses that affect function, care planning, selected medication use, marital status, and whether the person lived alone before SNF admission.
Statistical Analysis
The unadjusted (raw) outcomes of participants treated in SNFs with different annual hip fracture volume were first compared. Multivariable logistic regression models controlled for observable differences in participant and facility characteristics. All continuous variables (age, hospital LOS, BMI, ADL scale, SNF volume, SNF staffing) were modeled using natural cubic splines to allow for nonlinear associations. Year indicators were included to capture secular trends. Because cubic spline coefficients of continuous variables are hard to interpret clinically, adjusted odd ratios and risk ratios for facility volume are reported graphically. The inverse probability of censoring weights approach was used to account for the possibility that censoring due to death is correlated with SNF volume of hip fracture admissions.26 Robust standard errors were used to adjust for clustering of participants within SNF providers.
Two additional logistic regression approaches were used to account for potential selection bias: the Inverse Probability of Treatment Weighting, which creates propensity score–based weights to estimate a weighted logistic regression that adjusts for selective referral on observed participant characteristics,26 and the instrumental variable (IV) logistic regression method, which has the potential to account for selective referral due to observed and unobserved participant characteristics. The literature guided the choice of IV. Independent of case severity or local market conditions, nonclinical factors such as convenience because of proximity and availability have been shown to affect the selection of PAC sites.27,28 Distance to the nearest facility of a given type is often used as an IV to remove the effect of treatment site choice.8,29 In the case of selection of PAC setting, it has been recently argued that convenience because of proximity strongly affects the selection of PAC sites.28 These distance-based IVs are expected to be correlated with choice of SNF facility but uncorrelated with participant clinical condition because proximity or availability of specific PAC options is not thought to influence place of residence. The IV model was implemented using the two-stage residual inclusion method30 and to control for two potential sources of selection: discharge to alternative PAC sites (SNF, inpatient rehabilitation facility, community) after the index hospitalization and referral to a SNF facility with a specific volume of those referred to SNFs. Because of space limitations and because results were similar, only results for the preferred IV model are presented. Further methodological details are available upon request. All analyses were conducted in Stata version 13 (Stata Corp., College Station, TX). The Brown University institutional review board approved this study, which relied upon Data Use Agreement 19085 with the Centers for Medicare and Medicaid Services to access the identifiable health data.
Sensitivity Analyses
In addition to correcting for selection bias using regression methods, sensitivity analyses were conducted after stratifying the SNF cohort into two groups based on their risk of remaining institutionalized in the SNF to examine whether a volume effect was still observed even in the lowest-risk participants. Determination of the relative important of each factor was established by performing a likelihood ratio test for exclusion of each factor from the full-factor regression outcome model. The magnitude in the drop in the likelihood function when excluding each factor (relative to the full-factor model) provides a measure of the relative size of the outcome variance that that single factor explains. The higher the likelihood ratio test is, the greater the relative importance of that factor.
The low-risk stratum consisted of participants with four risk factors most likely associated with successful 30-day discharge to the community: no cognitive impairment and no Alzheimer’s or other dementia diagnosis, a femoral neck fracture (vs pertrochanteric fracture), not living alone at the time of the hip fracture, and having an index hospital stay of less than 7 days. These factors have also been strongly associated with better PAC discharge outcomes.27,31,32
RESULTS
Participant Characteristics
Between 2000 and 2007, 512,967 individuals with a firsttime hip fracture discharged to 15,439 SNF providers for PAC were identified. Average participant age was 85.1 ± 5.7, 78.6% were female, and 94.6% were white. Table 1 contrasts participant characteristics for the four SNF volume quartiles, revealing small differences overall according to volume group. Those entering low-volume SNFs were slightly more likely than those entering high-volume SNFs to be older (85.5 vs 84.7), nonwhite (7.5% vs 4.3%), and not currently married (25% vs 30%) and to have had a longer hospital stay (6.9 vs 6.3 days) and somewhat higher levels of physical impairment (ADL score 19.0 vs 17.2), cognitive impairment (CPS score 1.9 vs 1.3), do-not-resuscitate orders (37.7% vs 17.8%), Alzheimer’s disease or dementia (25.1% vs 13.6%), incontinence (25.1% vs 14.6%), and comorbidities. Participants discharged to SNFs in the high-volume quartile were discharged from hospitals with a higher annual volume of hip fractures (99.6 vs 76.3).
Table 1.
Characteristics of Community-Dwelling Individuals with First-Time Hip Fracture Living in a Skilled Nursing Facility (SNF), 2000–2007, and Characteristics of SNFs According to Annual SNF Provider Volume of Hip Fracture Admissions (N = 15,439 SNFs)
| Annual Volume of Hip Fracture Admissions a |
|||||
|---|---|---|---|---|---|
| Characteristic | 0–6, n = 120,465 (23.5%) |
7–13, n = 130,914 (25.5%) |
14–24, n = 128,456 (25.1%) |
≥25, n = 133,132 (25.9%) |
Total, N = 512,967 |
| Successful discharge to community, % | 18.8 | 24.9 | 34.3 | 43.7 | 30.8 |
|
| |||||
| Censored (died within 60 days of discharge from hospital), % |
9.0 | 8.3 | 7.0 | 6.1 | 7.6 |
|
| |||||
| Participant characteristics b | |||||
|
| |||||
| Age, mean ± SD | 85.5 ± 5.7 | 85.3 ± 5.7 | 85.0 ± 5.6 | 84.7 ± 5.6 | 85.1 ± 5.7 |
|
| |||||
| Female, % | 78.1 | 78.9 | 78.7 | 78.7 | 78.6 |
|
| |||||
| Race, % | |||||
|
| |||||
| White | 92.5 | 94.9 | 95.2 | 95.7 | 94.6 |
|
| |||||
| Black | 4.4 | 2.7 | 2.5 | 2.1 | 2.9 |
|
| |||||
| Hispanic | 1.1 | 0.8 | 0.9 | 0.8 | 0.9 |
|
| |||||
| Otherc | 1.6 | 1.2 | 1.1 | 1.1 | 1.2 |
|
| |||||
| Marital status, % | |||||
|
| |||||
| Never married | 6.2 | 5.6 | 5.2 | 5.0 | 5.5 |
|
| |||||
| Currently married | 25.1 | 26.1 | 28.0 | 30.0 | 27.4 |
|
| |||||
| Widowed, divorced | 68.7 | 68.3 | 66.8 | 65.0 | 67.1 |
|
| |||||
| Femoral neck fracture, % | 47.5 | 48.1 | 2.4 ± 1.3 | 2.4 ± 1.3 | 48.6 |
|
| |||||
| Number of Elixhauser comorbidities, mean ± SD | 2.4 ± 1.3 | 2.4 ± 1.3 | 2.4 ± 1.3 | 2.4 ± 1.3 | 2.4 ± 1.3 |
|
| |||||
| Hospital length of stay, days, mean ± SD | 6.9 ± 4.4 | 6.6 ± 4.0 | 6.3 ± 3.8 | 6.3 ± 3.7 | 6.5 ± 4.0 |
|
| |||||
| Body mass index, kg/m2, mean±SD | 23.6 ± 4.9 | 23.7 ± 4.8 | 23.8 ± 4.7 | 23.8 ± 4.7 | 23.7 ± 4.8 |
|
| |||||
| Activity of daily living score (range 0–28), mean ± SD | 19.0 ± 4.7 | 18.5 ± 4.5 | 17.8 ± 4.5 | 17.2 ± 4.3 | 18.1 ± 4.5 |
|
| |||||
| Comorbidities, % | |||||
|
| |||||
| Osteoporosis | 17.6 | 18.4 | 17.0 | 15.1 | 17.0 |
|
| |||||
| Congestive heart failure | 16.4 | 16.0 | 14.7 | 13.4 | 15.1 |
|
| |||||
| Cardiovascular disease | 15.0 | 14.8 | 13.3 | 12.1 | 13.8 |
|
| |||||
| Cerebrovascular accident | 9.5 | 8.9 | 7.7 | 6.8 | 8.2 |
|
| |||||
| Diabetes mellitus | 18.1 | 17.9 | 17.4 | 16.8 | 17.5 |
|
| |||||
| Depression | 20.5 | 20.9 | 19.2 | 17.4 | 19.5 |
|
| |||||
| Cognitive Performance Scale score, mean ± SD (range 0–6) |
1.9 ± 1.7 | 1.7 ± 1.6 | 1.5 ± 1.6 | 1.3 ± 1.5 | 1.6 ± 1.6 |
|
| |||||
| Alzheimer’s disease or dementia, % | 25.1 | 22.7 | 18.2 | 13.6 | 19.8 |
|
| |||||
| Bladder or bowel incontinence, % | 25.1 | 21.5 | 17.9 | 14.6 | 19.7 |
|
| |||||
| Lived alone, % | 36.0 | 36.7 | 37.8 | 39.5 | 37.5 |
|
| |||||
| Do-not-resuscitate order, % | 37.7 | 33.5 | 26.2 | 17.8 | 28.6 |
|
| |||||
| Hospital hip fracture volume, mean ± SD | 76.3 ± 52.9 | 79.6 ± 54.3 | 82.3 ± 53.7 | 99.6 ± 53.5 | 84.7 ± 54.4 |
|
| |||||
| SNF characteristicsd | |||||
|
| |||||
| Based in a hospital, % | 6.6 | 12.5 | 26.7 | 42.9 | 22.5 |
|
| |||||
| Not for profit, % | 27.6 | 32.3 | 40.1 | 51.3 | 38.1 |
|
| |||||
| Multisite (part of a chain), % | 59.4 | 58.0 | 53.7 | 46.0 | 54.1 |
|
| |||||
| Number of beds, mean ± SD | 104.2 ± 55.2 | 119.0 ± 67.0 | 117.2 ± 83.9 | 122.3 ± 108.3 | 115.9 ± 81.9 |
|
| |||||
| Dedicated rehabilitation unit, % | 2.1 | 4.2 | 6.6 | 9.4 | 5.6 |
|
| |||||
| FTE registered nurses per 10 residents | 0.9 | 1.2 | 1.8 | 2.5 | 1.6 |
|
| |||||
| FTE licensed practical nurses per 10 residents | 1.7 | 1.8 | 2.0 | 2.2 | 1.9 |
|
| |||||
| FTE PTs per 10 residents receiving therapy | 1.9 | 1.8 | 2.0 | 2.5 | 2.0 |
|
| |||||
| ≥80% of FTE PTs on staff (not contracted), % | 41.1 | 54.1 | 65.0 | 74.0 | 59.1 |
|
| |||||
| FTE occupational therapists per 10 residents receiving therapy |
1.5 | 1.4 | 1.5 | 1.7 | 1.5 |
SD = standard deviation; FTE = Full-time equivalent; PT = physical therapist.
Volume in the 12 months before participant’s discharge from the hospital for hip fracture.
Participant characteristics included in the models but not reported in Table 1 included postoperative pulmonary failure, pulmonary embolism, postoperative acute renal failure, time to surgery from hospital admission, intensive care unit use, hypertension, hypotension, arteriosclerotic heart disease, cardiac dysrhythmias, peripheral vascular disease, arthritis, hemiplegia or hemiparesis, multiple sclerosis, paraplegia, Parkinson’s disease, seizure disorder, transient ischemic attack, traumatic brain injury, anxiety disorder, bipolar, schizophrenia, asthma, anemia, cancer, renal insufficiency, clostridium difficile, antibiotic resistant infection, septicemia, pressure ulcers, urinary tract infection, daily pain, and problem swallowing.
Race was unknown for 0.4% of participants, so race percentages do not add up to 100%.
SNF characteristics also included facility average resource utilization group case-mix classification index, calculated from all admissions (mostly SNF residents) in a given year and from all residents on a given day (to account for severity of non-SNF residents) to adjust the facility staffing levels for facility resident severity.39
Mortality differed slightly according to SNF volume category, primarily in the non-low risk cohort (9.0% in low volume vs 6.1% in high volume), so all analyses were performed using inverse probability of censoring weights to adjust for potential differential mortality according to SNF volume.
Facility Characteristics
On average, there were 10,622 SNF providers annually admitting individuals with hip fracture; 22.5% of the participants received their care in a hospital-based SNF and 38.1% in a nonprofit SNF. The average RN full-time equivalent (FTE) per 10 residents was 1.6, and the average LPN FTE was 1.9, and there were 2 FTE PTs on average per 10 residents receiving therapy (Table 1). Facilities with a larger volume of residents with hip fracture were also likely to have higher numbers of residents with other conditions, so it is not surprising to have found large differences in facility staffing between hip fracture volume groups (Table 1).
SNF Volume Effect on Successful Return to the Community
The rate of 30-day successful discharge to the community was 30.8%, with interquartile range variation between the 15,439 facilities from 0% (25th percentile) to 36% (75th percentile). An important determinant of this variation rate was facility volume. Successful discharge from high-volume facilities (>24 admissions/year) was 43.7%, vs 18.8% from low-volume facilities (1–6 admissions/year) (Table 1).
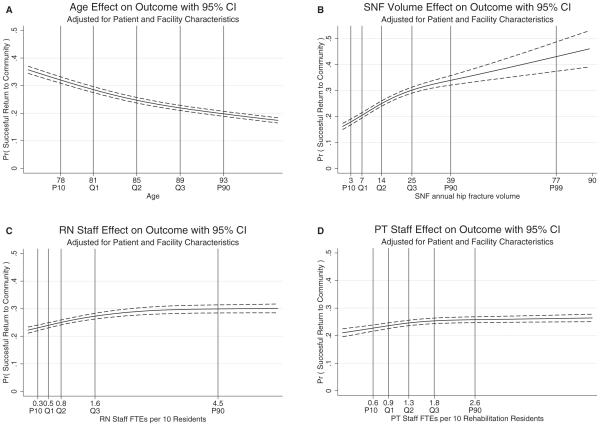
Figure 1 provides participant and facility risk-adjusted estimates of the association between the probability of successful discharge to the community and age, SNF volume, and two staffing facility characteristics, evaluated at the average value of the other covariates. These four factors had nonlinear relationships with the outcome. Age had a negative effect on the probability of successful discharge to the community but became marginally less influential at older ages. Of facility characteristics, an initial beneficial effect from higher staffing levels (per resident) was observed, particularly for RN staffing, but no noticeable benefits beyond a certain staffing level. Finally, there appeared to be a strong volume effect that differences in participant and facility characteristics in the model did not explain, particularly for individuals admitted to facilities with zero to 24 individuals with hip fracture the previous year. Because of the presence of nonlinearities, the adjusted odds ratios (AORs) and relative risk ratios (RRRs) from this model vary with the values used for the comparison. Because the coefficients of the cubic spline are hard to interpret clinically, the cubic splines of the continuous covariates were replaced with a 10-level categorization of the covariates based on deciles (for age, ADL scores, and facility volume) or with linear splines (for BMI, hospital LOS, hospital volume, and facility staffing factors). Table 2 provides estimates of the AORs for the most-relevant risk factors in this model. Compared to individuals in a facility in the lowest decile with 0–2 hip fracture admissions in the previous 12 months, individuals admitted to facilities in the top decile with 39 or more hip fracture admissions in the previous 12 months were more than twice as likely to experience a successful community discharge (AOR = 2.27, 95% CI = 1.92–2.69).
Figure 1.
Effect of participant and facility characteristics on probability of returning to community within 30 days of skilled nursing facility (SNF) admission and remaining at least 30 days at home without institutionalization: (A) age, (B) SNF hip fracture volume, (C) registered nurse (RN) staffing, (D) physical therapist (PT) staffing. Estimates from the independent variable model. Evaluated at age 85, ADL 16, BMI 24.0 kg/m2, hospital LOS 6 days, hospital annual volume of hip fractures 85, and cohort mean of all covariates (other than volume). Vertical lines (for reference) at values 3, 7, 14, 25, 39, and 77, which correspond to the 10th percentile (P10), 25th percentile (Q1), 50th percentile (Q2), 75th percentile (Q3), 90th percentile (P90), and 99th percentile (P99) of SNF facility annual volume, respectively. Dashed lines represent the 95% confidence interval (CI around the estimated probability of the outcome. FTE = full-time equivalent; ADL = activity of daily living; BMI = body mass index; LOS = length of stay.
Table 2.
Odds of Returning to the Community within 30 Days of Skilled Nursing Facility (SNF) Admission and Remaining at Least 30 Days at Home without Institutionalization
| Characteristic | Adjusted Odds Ratio (95% Confidence Interval) |
P-Value |
|---|---|---|
| Participant | ||
|
| ||
| Age decile (reference 75–77) | ||
|
| ||
| 78–79 | 0.89 (0.86–0.92) | .001 |
|
| ||
| 80–81 | 0.83 (0.80–0.85) | .001 |
|
| ||
| 82–82 | 0.75 (0.72–0.78) | .001 |
|
| ||
| 83–84 | 0.71 (0.69–0.73) | .001 |
|
| ||
| 85–86 | 0.66 (0.64–0.68) | .001 |
|
| ||
| 87–87 | 0.60 (0.58–0.63) | .001 |
|
| ||
| 88–89 | 0.58 (0.55–0.60) | .001 |
|
| ||
| 90–92 | 0.53 (0.51–0.55) | .001 |
|
| ||
| ≥93 | 0.50 (0.48–0.52) | .001 |
|
| ||
| Female | 1.08 (1.06–1.11) | .001 |
|
| ||
| Race and ethnicity (reference white) | ||
|
| ||
| Black | 1.15 (1.09–1.22) | .001 |
|
| ||
| Hispanic | 1.12 (0.98–1.27) | .09 |
|
| ||
| Other | 1.11 (1.01–1.22) | .03 |
|
| ||
| Marital status (reference widowed or divorced) | ||
|
| ||
| Never married | 0.80 (0.77–0.83) | .001 |
|
| ||
| Currently married | 1.29 (1.26–1.31) | .001 |
|
| ||
| Activity of daily living score decile (range 0–28) (reference 0–11) | ||
|
| ||
| 12–13 | 0.70 (0.67–0.73) | .001 |
|
| ||
| 14–15 | 0.50 (0.48–0.52) | .001 |
|
| ||
| 16–17 | 0.38 (0.36–0.39) | .001 |
|
| ||
| 18–18 | 0.30 (0.28–0.31) | .001 |
|
| ||
| 19–19 | 0.24 (0.23–0.25) | .001 |
|
| ||
| 20–21 | 0.21 (0.20–0.22) | .001 |
|
| ||
| 22–23 | 0.18 (0.17–0.19) | .001 |
|
| ||
| 24–28 | 0.18 (0.17–0.19) | .001 |
|
| ||
| Osteoporosis | 0.95 (0.93–0.97) | .001 |
|
| ||
| Femoral neck fracture | 1.65 (1.62–1.68) | .001 |
|
| ||
| Elixhauser comorbidity | 0.96 (0.95–0.97) | .001 |
|
| ||
| Body mass index (per unit) | ||
|
| ||
| For < 24 units | 1.001 (0.997–1.005) | .48 |
|
| ||
| For ≥24 units | 0.977 (0.974–0.980) | .001 |
|
| ||
| Congestive heart failure | 0.91 (0.88–0.93) | .001 |
|
| ||
| Cardiovascular disease | 1.01 (0.99–1.04) | .29 |
|
| ||
| Cerebrovascular accident | 0.88 (0.85–0.91) | .001 |
|
| ||
| Diabetes mellitus | 0.90 (0.88–0.92) | .001 |
|
| ||
| Depression | 0.82 (0.81–0.84) | .001 |
|
| ||
| Cognitive Performance Scale score (reference 0) (range 0–6) |
0.655 (0.640–0.673) | .001 |
|
| ||
| 1 | 0.74 (0.72–0.76) | .001 |
|
| ||
| 2–3 | 0.58 (0.57–0.60) | .001 |
|
| ||
| 4–6 | 0.65 (0.62–0.67) | .001 |
|
| ||
| Alzheimer’s disease or other dementia |
0.88 (0.86–0.91) | .001 |
|
| ||
| Bladder or bowel incontinence |
0.81 (0.78–0.83) | .001 |
|
| ||
| Lived alone at time of fracture |
0.74 (0.73–0.76) | .001 |
|
| ||
| Do-not-resuscitate order | 0.85 (0.83–0.88) | .001 |
|
| ||
| Hospital LOS per day | ||
|
| ||
| For 1–5 days | 0.94 (0.92–0.95) | .001 |
|
| ||
| For ≥ 6 days | 0.96 (0.95–0.96) | .001 |
|
| ||
| Hospital hip fracture volume per participant | ||
|
| ||
| For < 80 participants | 0.997 (0.996–0.998) | .001 |
|
| ||
| For ≥ 80 participants | 0.999 (0.998–0.999) | .001 |
|
| ||
| SNFa | ||
|
| ||
| Hip fracture volume decile (reference 0–2) | ||
|
| ||
| 3–5 | 1.10 (1.05–1.15) | .001 |
|
| ||
| 6–7 | 1.22 (1.16–1.29) | .001 |
|
| ||
| 8–10 | 1.32 (1.24–1.39) | .001 |
|
| ||
| 11–13 | 1.47 (1.38–1.56) | .001 |
|
| ||
| 14–17 | 1.57 (1.47–1.69) | .001 |
|
| ||
| 18–21 | 1.74 (1.61–1.89) | .001 |
|
| ||
| 22–28 | 1.89 (1.72–2.07) | .001 |
|
| ||
| 29–38 | 2.09 (1.85–2.36) | .001 |
|
| ||
| 39–138 | 2.27 (1.92–2.69) | .001 |
|
| ||
| SNF based in a hospital | 1.57 (1.46–1.69) | .001 |
|
| ||
| Not for profit | 1.06 (1.01–1.11) | .02 |
|
| ||
| Multisite (part of a chain) | 0.94 (0.90–0.98) | .003 |
|
| ||
| Dedicated rehabilitation unit | 1.19 (1.10–1.28) | .001 |
|
| ||
| FTE RN per 10 residents | ||
|
| ||
| For < 2.0 units | 1.16 (1.11–1.21) | .001 |
|
| ||
| For ≥ 2.0 units | 1.01 (0.996–1.021) | .20 |
|
| ||
| FTE PT per 10 residents receiving therapy | ||
|
| ||
| For < 1.3 units | 1.11 (1.058–1.19) | .001 |
|
| ||
| For ≥ 1.3 units | 1.02 (1.01–1.04) | .001 |
The regression model used for this table replaced the cubic splines for age, activities of daily living (ADLs), and facility hip fracture volume, with 10-level categories based on deciles of variables to help interpretation. Similarly, the cubic splines for hospital length of stay (LOS); hospital hip fractures volume; and SNF registered nurse (RN), licensed practical nurse (LPN), and physical therapist (PT) staffing were replaced with linear splines to obtain adjusted odd ratios (aORs) that are easier to interpret. In addition to the covariates listed in the table, the regression model included 67 additional covariates not shown for brevity.
Full-time equivalent (FTE) LPNs per 10 residents, FTE occupational therapists (OTs) per 10 residents receiving therapy, and having ≥ 0% of FTE PT and OT on staff (not contracted) were not statistically significant facility characteristics.
The regression model used for this table replaced the cubic splines for age, activities of daily living (ADLs), and facility hip fracture volume, with 10-level categories based on deciles of variables to help interpretation. Similarly, the cubic splines for hospital length of stay (LOS); hospital hip fractures volume; and SNF registered nurse (RN), licensed practical nurse (LPN), and physical therapist (PT) staffing were replaced with linear splines to obtain adjusted odd ratios (aORs) that are easier to interpret. In addition to the covariates listed in the table, the regression model included 67 additional covariates not shown for brevity.
To gain some perspective on what these variations in outcomes with SNF volume mean, of the roughly 75% (379,835) of participants who received care in a facility with zero to 24 hip fracture admissions and could have received their care in a facility with higher volume than the facility they were in, 10% (N = 37,810) had a facility with higher volume closer than the SNF they chose. If these individuals had been willing to travel up to 5 extra miles, 59.4% of them could have received their care at a higher-volume SNF, and 70.5% could have done so if they had been willing to travel up to 10 extra miles.
Sensitivity Analyses
The analysis was stratified according to the presence of four risk factors—no cognition problems, femoral neck fracture, living alone, shorter hospital stay—associated with better discharge outcomes shows that the volume effect was present even in this low-risk group (see Figure 2). The low-risk group appeared to experience a large increase in the probability of successful discharge when moving from a low-volume facility to a medium-volume facility, but not much difference when moving from a medium-volume facility to a high-volume facility. The non-low-risk group experienced nontrivial improvements in their probability of successful discharge at all volume levels and should therefore try to be admitted to the facility with the highest volume available to them.
Figure 2.
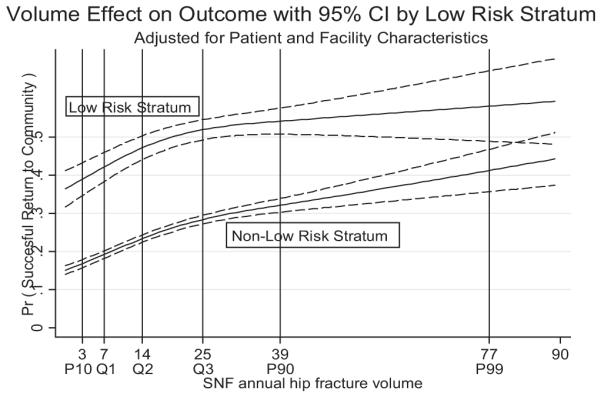
Skilled nursing facility (SNF) volume effect on probability of successful 30-day discharge to the community stratified according to outcome risk. The low-risk stratum consists of participants with the four risk factors most associated with successful 30-day discharge to the community: no diagnosis of cognitive impairment or Alzheimer’s or other dementia, having a femoral neck fracture, not living alone at the time of the hip fracture, and having an index hospital stay of less than 7 days. The non-low-risk stratum includes the remaining participants, who had one or more of these four risk factors at SNF admission.
A comparison of the estimation results using different regression models (basic logistic, propensity-score IPT-weighted logistic, or the preferred IV logistic model) that controlled for increasing amounts of confounding showed that the estimated association between volume and outcome was similar with different regression methods, indicating that the association was fairly robust regardless of the adjustment methodology used. For this reason, the results shown in the tables and figures were based on the IV regression model. The main appreciable difference between methods was for the highest-volume facilities (in the top decile), in which the IV results had a higher volume effect than the basic logit model, indicating that these facilities may be admitting some individuals not living near the facility who may be sicker than what their observed characteristics suggest. To validate the distance instruments, it was verified that participants tended to be admitted to facilities close to their residence, which shows that the instrument was correlated with the volume of the admitting facility, as the IV method required, and a t-test of the coefficient of the selection model residual in the outcome regression model (which provided a valid test of dependence between the SNF volume treatment variables and unmeasured confounders) showed that the coefficient of the selection model residual was significant at the 5% level (P = .002). Further technical details are available from the authors upon request.
DISCUSSION
Hip fractures are a significant cause of morbidity and mortality for frail older adults. An important goal of rehabilitation is successful discharge to the community. Only 31% of SNF residents with a first hip fracture achieved successful discharge to the community within 30 days of discharge from the hospital, although wide variation between the 15,439 facilities was found, with an interquartile range variation from 0% (25th percentile) to 36% (75th percentile). The results show that, after adjusting for many participant risk factors and for potential selection bias, facility characteristics (e.g., being hospital based, RN and PT staffing) are important determinants in this variation, and participants discharged to high-volume SNFs (all else equal) were approximately twice as likely to achieve successful discharge to the community. Nearly one in 10 participants could have gone to a higher-volume facility closer to their home than the one they went to, and 70.5% could have accessed a higher-volume facility had they traveled up to 10 extra miles.
The relationship between higher volume and better clinical outcomes has generated a large body of research33 over the last 3 decades, particularly for hospital and surgical outcomes.10,14,15,33–35 The present work extends this research to the postacute SNF setting. One recent study found that higher SNF volume (for any condition) was associated with fewer SNF resident 30- and 90-day rehospitalizations,16 but that study, unlike the current one, was based on all clinical diagnoses combined and did not control for selection bias.
There are some limitations to this study. The MDS assessment provides a long list of risk-adjustment factors, including nonclinical factors such as whether the person lived alone, that have been found to influence successful discharge from PAC,36 and further attempt was made to control for selection bias using instrumental variable regression methods and stratified sensitivity analyses that provide correction for unobserved confounders, but it is not certain that all selection bias was corrected for. For this reason, the analysis reports an association and cannot be interpreted as a causal analysis. Second, the care needs of all their residents, not only of those with hip fracture, determine staffing and other facility characteristics. Although facility average case-mix indices were included, this may not properly adjust for the measured facility staffing characteristics. In addition, the staffing measure does not account for the quality or efficiency differences of the staff members. Third, there was no reliable information on the amount, timing, or quality of the therapy delivered. Finally, other than through marital status and information on living alone at the time of the fracture, no information was available on other sources of informal care or whether the person resided in an assisted living facility after discharge to the community.
Despite these limitations, the results provide evidence that facility characteristics are important in explaining PAC outcome variations and that, after adjusting for these organizational and staffing characteristics, a strong positive relationship persists between volume and outcome. Further research is needed to better understand which SNF processes of care are behind the observed importance of the effect of volume on PAC outcomes.37 These volume findings provide a helpful taxonomy for guiding that research.
There is a growing interest in ensuring that consumers, policymakers, and payers have access to information about a provider’s quality of care. There are only five quality measures available to individuals and their caregivers on the publicly available Nursing Home Compare website, which reports NH quality measures and focuses specifically on this short-stay population: pain, pressure ulcers, influenza and pneumococcal vaccination, and antipsychotic medication. None provide adequate insight into the best place of care for an individual seeking therapeutic PAC, such as individuals with hip fracture. The fact that one in 10 persons could have gone to a SNF closer to home with better outcomes, together with the fact that few SNF facilities are at full capacity,38 indicates a lack of adequate information for individuals and hospital discharge staff at the time of SNF selection. This study introduces a new outcome measure, successful discharge to the community, which is more directly related to the goals of care for these individuals. Making public the (risk adjusted) facility rates of successful discharge to the community could provide valuable additional information to individuals and those helping them when faced with choosing a SNF for rehabilitation after hip fracture. Furthermore, policymakers and hospital discharge planners should consider the implications of these findings to achieve access to the best PAC.
ACKNOWLEDGMENTS
Primary support was received from the Shaping Long Term Care in America Project, funded by the National Institute on Aging (P01 AG027296). Additional support (N.E. Leland and T.J. Christian) was received from the Agency for Healthcare Research and Quality National Research Services Awards (5T32HS000011–24) (N.E. Leland), the Rehabilitation Research Career Development Program, National Center for Medical Rehabilitation Research, National Institutes of Health (K12 HD05 5929).
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper. Dr. Mor is a founder and on the board of directors of PointRight, Inc., an information services company that provides quality and improvement measurements to NHs. Dr. Mor receives no research funding, data, or consultation fees for his research from PointRight.
Author Contributions: All authors contributed in the study concept and design, acquisition of data, analysis and interpretation of data, and preparation of manuscript.
Sponsor’s Role: The funding sources had no role in the design of the study; data collection, management, analysis, or interpretation; or preparation, review, or approval of the manuscript.
REFERENCES
- 1.Chandra A, Dalton MA, Holmes J. Large increases in spending on postacute care in Medicare point to the potential for cost savings in these settings. Health Aff (Millwood. 2013;32:864–872. doi: 10.1377/hlthaff.2012.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grabowski DC, Huckfeldt PJ, Sood N, et al. Medicare postacute care payment reforms have potential to improve efficiency of care, but may need changes to cut costs. Health Aff (Millwood. 2012;31:1941–1950. doi: 10.1377/hlthaff.2012.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Report to the Congress—Medicare Payment Policy . Medicare Payment Advisory Committee; Washington, DC: 2003. [Google Scholar]
- 4.Report to the Congress—Medicare Payment Policy. Medicare Payment Advisory Committee; Washington, DC: 2013. [Google Scholar]
- 5.Joseph PN, Alan MG, Robin PG, et al. National Academies Press; Washington, DC: 2013. Variation in Health Care Spending: Target Decision Making, Not Geography. [PubMed] [Google Scholar]
- 6.Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- 7.Boudourakis LD, Wang TS, Roman SA, et al. Evolution of the surgeon-volume, patient-outcome relationship. Ann Surg. 2009;250:159–165. doi: 10.1097/SLA.0b013e3181a77cb3. [DOI] [PubMed] [Google Scholar]
- 8.McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis Using Instrumental Variables. JAMA. 1994;272:859–866. [PubMed] [Google Scholar]
- 9.Hannan EL, Siu AL, Kumar D, et al. The decline in coronary artery bypass graft surgery mortality in New York State. The Role of Surgeon Volume. JAMA. 1995;273:209–213. [PubMed] [Google Scholar]
- 10.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med. 1979;301:1364–1369. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- 11.Luft HS, Hunt SS, Maerki SC. The volume-outcome relationship: Practice-makes-perfect or selective-referral patterns? Health Serv Res. 1987;22:157–182. [PMC free article] [PubMed] [Google Scholar]
- 12.Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 13.Kahn JM, Ten Have TR, Iwashyna TJ. The relationship between hospital volume and mortality in mechanical ventilation: An instrumental variable analysis. Health Serv Res. 2009;44:862–879. doi: 10.1111/j.1475-6773.2009.00959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 15.Hernandez-Boussard T, Downey JR, McDonald K, et al. Relationship between patient safety and hospital surgical volume. Health Serv Res. 2012;47:756–769. doi: 10.1111/j.1475-6773.2011.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Cai X, Yin J, et al. Is higher volume of postacute care patients associated with a lower rehospitalization rate in skilled nursing facilities? Med Care Res Rev. 2012;69:103–118. doi: 10.1177/1077558711414274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Report to the Congress—Medicare Payment Policy . Medicare Payment Advisory Committee; Washington, DC: 2007. [Google Scholar]
- 18.Neuman MD, Fleisher LA, Even-Shoshan O, et al. Nonoperative care for hip fracture in the elderly: The influence of race, income, and comorbidities. Med Care. 2010;48:314–320. doi: 10.1097/mlr.0b013e3181ca4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Intrator O, Hiris J, Berg K, et al. The residential history file: Studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Long Term Care: Facts on care in the US. [on-line] Available at www.LTCFocUS.org Accessed December 2013.
- 21.Kim H, Harrington C, Greene WH. Registered nurse staffing mix and quality of care in nursing homes: A longitudinal analysis. Gerontologist. 2009;49:81–90. doi: 10.1093/geront/gnp014. [DOI] [PubMed] [Google Scholar]
- 22.Grabowski DC, Stewart KA, Broderick SM, et al. Predictors of nursing home hospitalization: A review of the literature. Med Care Res Rev. 2008;65:3–39. doi: 10.1177/1077558707308754. [DOI] [PubMed] [Google Scholar]
- 23.Castle NG, Engberg JB. The influence of agency staffing on quality of care in nursing homes. J Aging Soc Policy. 2008;20:437–457. doi: 10.1080/08959420802070130. [DOI] [PubMed] [Google Scholar]
- 24.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 25.HCUP) HCaUP . 3.4. Agency for Healthcare Research and Quality (AHRQ; Rockville, MD: 2009. Elixhauser Comorbidity Software. [Google Scholar]
- 26.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Buntin MB, Garten AD, Paddock S, et al. How much is postacute care use affected by its availability? Health Serv Res. 2005;40:413–434. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buntin MB, Colla CH, Deb P, et al. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Geweke J, Gowrisankaran G, Town RJ. Bayesian inference for hospital quality in a selection model. Econometrica. 2003;71:1215–1238. [Google Scholar]
- 30.Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. J Health Econ. 2008;27:531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu K, Wissoker D, Rimes C. Determinants and costs of Medicare postacute care provided by SNFs and HHAs. Inquiry. 1998;35:49–61. [PubMed] [Google Scholar]
- 32.Kane RL, Finch M, Blewett L, et al. Use of post-hospital care by Medicare patients. J Am Geriatr Soc. 1996;44:242–250. doi: 10.1111/j.1532-5415.1996.tb00909.x. [DOI] [PubMed] [Google Scholar]
- 33.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 34.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for highrisk surgical procedures: Potential benefits of the Leapfrog initiative. Surgery. 2001;130:415–422. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 35.Thiemann DR, Coresh J, Oetgen WJ, et al. The association between hospital volume and survival after acute myocardial infarction in elderly patients. N Engl J Med. 1999;340:1640–1648. doi: 10.1056/NEJM199905273402106. [DOI] [PubMed] [Google Scholar]
- 36.Kane RL. Assessing the effectiveness of postacute care rehabilitation. Arch Phys Med Rehabil. 2007;88:1500–1504. doi: 10.1016/j.apmr.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 37.Livingston EH, Cao J. Procedure volume as a predictor of surgical outcomes. JAMA. 2010;304:95–97. doi: 10.1001/jama.2010.905. [DOI] [PubMed] [Google Scholar]
- 38.Castle NG, Engberg J, Lave J, et al. Factors associated with increasing nursing home closures. Health Serv Res. 2009;44:1088–1109. doi: 10.1111/j.1475-6773.2009.00954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fries BE, Schneider DP, Foley WJ, et al. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III) Med Care. 1994;32:668–685. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]