Abstract
Background:
The pneumatic tourniquet (PT) is routinely used in upper and lower limb operations by most orthopaedic surgeons. The silicone ring tourniquet (SRT) was introduced in clinical practice over the last decade. Clinical as well as comparative studies have been published in volunteers concerning its safety and efficacy. The aim of this study was to investigate the postoperative effect of the silicone ring tourniquet (SRT), primarily on the motor nerve conduction, and secondarily on the pain and grip strength, in comparison to the effect of the pneumatic tourniquet (PT) in healthy volunteers.
Methods:
Both tourniquets were applied in the forearm of the dominant arm in 20 healthy volunteers and were kept on for 10 minutes. Pain was measured using the visual analogue scale and grip strength was measured with a hand dynamometer. We evaluated the following parameters of median nerve conduction: motor conduction velocity (MCV), latency (LAT) and amplitude (AMP).
Results:
Pain score at the time of tourniquet application was higher in SRT group but the alteration in pain scores in PT group was higher, with statistical significance (P<0.05). The grip strength was reduced by the application of both tourniquets; however there was a significantly higher reduction in the SRT group (P<0.05). The conduction impairment of the median nerve was worse in the PT group than in the SRT one, according to the changes in MCV (P<0.05).
Conclusion:
Median nerve conduction was affected more after PT application as compared to the SRT. Nevertheless, the reduction of grip strength was higher after the SRT application.
Keywords: Cuff, Nerve conduction, Pain, Silicone ring tourniquet, Tourniquet
Introduction
The tourniquet is routinely used in upper and lower limb operations by most orthopaedic surgeons in order to achieve bloodless surgery, improve the identification of vital structures and expedite surgical procedures (1). Pneumatic tourniquet (PT) is the most commonly used device since its introduction by Harvey Cushing in 1904 and its use has become almost routine (1).
The mechanical pressure as well as ischemia-reperfusion injury are related to structural and functional changes to muscles and nerves as well as to skin and vessels. Apart from the amount of the applied pressure and the duration of application, the characteristics of the cuff (width and shape) are also important elements. Although lower arterial occlusion pressure is required using wider cuffs, human volunteer studies have shown that the wider cuffs resulted in more pain and were tolerated less than narrow cuffs (2-4). A more recent study found this to be true with higher pressures; however with lower pressures a wide tourniquet cuff is less painful than a narrow one (5). Nerve conduction studies in volunteers have recently shown that wider cuffs resulted in more severe changes of the nerve function than narrow cuffs, provided that they were inflated at the same pressure and for the same time (6).
The silicone ring tourniquet (SRT) was has been introduced in clinical practice during the last decade and both clinical and comparative studies in volunteers concerning its safety and efficacy have been published (7-15). The SRT is a narrow silicone ring applied at a predetermined pressure. This is determined by the selected tourniquet model, according to the patient’s arterial blood pressure.
Pain intensity and tolerance time after SRT application in comparison to PT have been studied in healthy volunteers (11-13). However, the effect of this tourniquet on muscle strength and nerve function has not been studied yet, according to our knowledge.
The aim of this study was to investigate the effect of the SRT on the motor nerve conduction in comparison to that of a standard PT, in healthy volunteers. Secondarily, we assessed tourniquet pain and the effect of both tourniquets on the grip strength.
Material and Methods
Volunteers
Twenty healthy volunteers, on no medication and without previous operations or fractures in the limbs, participated in this study [Table 1]. The study was approved by the Ethics Committee (UGHE 50/3-7-2013), the procedure was explained to each volunteer and a written consent was obtained from all volunteers.
Table 1.
Volunteers’ characteristics
| Number | 20 |
|---|---|
| Age (mean ± std) | 35.45 ± 10.308 |
| Gender (male) | 14 (70%) |
| Height (mean±std) | 1.735 ± 0.087 |
| Weight (mean±std) | 80.32 ± 15.576 |
| BMI (mean±std) | 26.612 ± 4.564 |
| R-L (Right arm) | 18 (90%) |
Tourniquets
Both tourniquets were applied on the dominant forearm, one after the other, with an at least 2-day interval. The SRT was studied firs in half of the volunteers and the PT on the other half (one alternating with the other). The volunteers were placed in a supine, comfortable position. The systolic blood pressure was measured in each one and was used as standard.
The appropriate model-size of the silicone ring tourniquet (HemaClear, OHK Medical Devices, Haifa, Israel) was used according to the standard systolic blood pressure. A standard PT with a 14-cm-wide cuff was also used and the cuff was applied over two layers of smoothly applied cast padding. The limb was elevated for 3 min before the tourniquet inflation, with the inflation pressure being 100 mmHg above the standard systolic blood pressure.
Grip strength and pain measurement
Grip strength was evaluated with the Jamar dynamometer (FEI, Irvington, NY, USA) according to the protocol of the American Society of Hand Therapists (16). Volunteers performed three maximum attempts for each measurement, each arm alternatively. The results of these trials were recorded and the average value was used for analysis.
The volunteers were instructed how to use the Visual Analogue Scale (VAS) for pain measurement (0 = no pain to 10 = the worst pain) and how to use the hand dynamometer (17).
Median nerve conduction studies
Volunteers were resting in a supine, comfortable position. Motor nerve conduction velocity (MCV) (in m/sec), amplitude (AMP) (in mVolt) and latency (LAT) (in msec) measurements of the median nerve for each subject were carried out prior to the application of tourniquet to the forearm and the results were recorded.
Stimulating and recording electrodes were placed on the forearm of the dominant upper extremity for each subject to stimulate the median nerve. The skin below the electrodes was slightly abraded before placement to reduce impedance. A ground electrode was fastened to the non-dominant arm’s forearm. The recording site was at the abductor policis brevis muscle. R1 and R2 electrodes were placed in such a way that R1 was placed over the muscle belly of the abductor brevis muscle and R2 over the first metacarpophalangeal joint. Stimulation sites were ante-cubital fossa proximally, and the wrist crease between the flexor carpi radialis and palmaris longus tendons distally.
The motor nerve conduction velocity before and following the application of the two cuffs was calculated by dividing the distance between the two stimulation sites by the difference in the onset latency proximal and distal to the cuff, i.e. CV (m/s) = distance (mm)/LATproxtocuff - LATdistaltocuff.
Procedure
Both tourniquets were applied in the forearm of the dominant arm and were kept on for 10 minutes.
The VAS score for pain was recorded (a) immediately after tourniquet application (initial pain score, T1), (b) 5 minutes after the tourniquet application (T5), and (c) just before the tourniquet removal (final pain score, T10). Grip strength was measured prior to tourniquet application (T0) and 5 minutes after the removal of the tourniquet (T+5).
Nerve conduction measurements were done just before the tourniquet application (T0), after 5 and 10 minutes (T5 and T10) of tourniquet application, and following the tourniquet removal at 5,10 and 15 minutes (T+5, T+10 and T+15).
Statistics
Statistical Package for Social Sciences (SPSS), version 20 was used for the analysis of data. The quantitative parameters were expressed as mean ± std and the qualitative as frequencies and percentages. At the beginning of our statistical analysis, we used the Kolmogorov-Smirnov test to evaluate the normality of each parameter. The results showed that all parameters followed the normal distribution. As a consequence, we utilized the parametric one way repeated measures ANOVA tests, with the assistance of post hoc analysis (Bonferroni correction) as well as the paired T-test. All tests were two-tailed and statistical significance was considered for values less than 0.05.
Results
Twenty volunteers with a mean age of 35.5 years (range 25 to 45 years) participated in this study; their demographics are shown in Table 1.
Pain
Pain scores and changes over time are shown it Table 2 and Figure 1. In this study, the pain at the time of tourniquet application (T1) was higher in the SRT group than in PT one. One way repeated measures ANOVA showed significantly different pain scores between the two different tourniquets only at T1 (P<0.001).
Table 2.
Pain scores of both tourniquets
| PT [mean (sd)] | SRT [mean (sd)] | P-Value | |
|---|---|---|---|
| T1 | 1.3 (1.2) | 4.1±2.1 | <0.001* |
| T5 | 3.0 (2.2) | 3.8±2.4 | 0.135 |
| T10 | 3.6 (2.7) | 4.5±2.5 | 0.138 |
| T1-T5 | 1.7 (1) ^P <0.001, COT: 130% | -0.3 (0.3) ^P =0.433, COT; (-7.3%) | 0.187 |
| T5-T10 | 0.6 (0.5) ^P =0.008, COT: 20% | 0.7 (0.1) ^P =0.024, COT: 18.4% | 0.258 |
| T1-T10 | 2.3 (1.5) ^P <0.001, COT: 176% | 0.4 (0.4) ^P =0.631, COT: 9.7% | 0.237 |
Significance over time.
COT: Change over time.
P <0.05.
Statistically significant difference. T: Time points described in the «procedure» section. PT: pneumatic tourniquet. SRT: Silicone ring tourniquet
Figure 1.

Pain scores.
The initial pain intensity during the SRT testing gradually subsided and increased again later, with a statistically significant difference identified only between T5 and T10 (F=4.142, P=0.024). On the contrary, the pain score changes during PT testing were significantly higher at all-time intervals, as it was shown by parametric statistics (from T1-T5, F=19.000, P<0.001, from T5 to T10, F=8.876, P=0.008, and from T1 to T10, F=21.891, P=<0.001). Two way mixed ANOVA have shown a statistically significant correlation between the type of the tourniquet and the change in pain scores over time (F=4.478, P=0.005), meaning that the changes in pain scores with PT were more pronounced.
Grip strength in Dominant and Non-Dominant Arm
A reduction of grip strength was observed after the application of both tourniquets for 10 minutes [Table 3]. Paired T-test showed that the difference in average values before tourniquet application (T0) and after tourniquet removal (T+5) was marginally significant for the SRT test (P=0.049). As far as the values for the non-dominant arm is concerned, a statistically significant difference was also found during the SRT test (P=0.002).
Table 3.
Grip strength values
| T0 | T+5 | Change | P-value | ||
|---|---|---|---|---|---|
| Dominant | PT [mean (std)] | 37.8 (9.6) | 36.7 (10.1) | -1.1 (0.5) [-2.96%] | P =0.183 |
| SRT [mean (std)] | 39.3 (10.3) | 37.0 (10.6) | -2.3 (0.3) [-5.7%] | P =0.049* | |
| Non-Dominant | PT [mean (std)] | 35.3 (8.3) | 36.0 (9.0) | 0.7 (0.7) [+0.83%] | P =0.405 |
| SRT [mean (std)] | 38.7 (10.2) | 36.3 (9.0) | -2.4 (1.2) [-3.88%] | P =0.002* |
T0: Time 0. Grip strength measurement before the tourniquet application.
T5: Time 5. Grip strength measurement five (5) minutes after the tourniquet removal.
P<0.05. Statistically significant difference
Nerve conduction studies
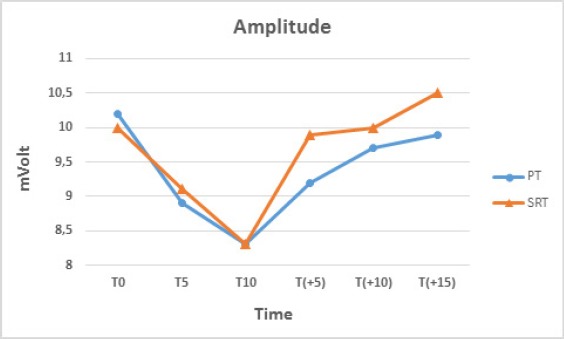
The application of both tourniquets resulted in an increase of the latency up to T10, while the removal of the tourniquets was followed by a decrease of the latency [Table 4; Figure 2]. On the other hand, the amplitude and MCV values decreased after the tourniquet application and subsequently gradually increased following its the removal [Table 4; Figure 3; 4].
Table 4.
Nerve conduction studies
| PT Mean (sd) | SRT Mean (sd) | RT versus SRT P-value | |
|---|---|---|---|
| Latency | |||
| Τ0 | 3.2 (0.5) | 3.2 (0.5) | 1.000 |
| T5 | 3.3 (0.4) | 3.3 (0.5) | 0.670 |
| T10 | 3.3 (0.4) | 3.4 (0.6) | 0.215 |
| T(+5) | 3.1 (0.5) | 3.2 (0.5) | 0.662 |
| T(+10) | 3.1 (0.5) | 3.2 (0.4) | 0.547 |
| T(+15) | 3.1 (0.4) | 3.1 (0.5) | 0.611 |
| Amplitude | |||
| Τ0 | 10.2 (3.6) | 10 (3.7) | 0.163 |
| T5 | 8.9 (2.8) | 9.1 (3.6) | 0.776 |
| T10 | 8.3 (2.8) | 8.3 (4.3) | 0.816 |
| T(+5) | 9.2 (2.6) | 9.9 (3) | 0.347 |
| T(+10) | 9.7 (2.6) | 10 (2.9) | 0.829 |
| T(+15) | 9.9 (2.4) | 10.5 (1.9) | 0.372 |
| Motor Nerve Conduction Velocity | |||
| Τ0 | 61.2 (5.4) | 61.2 (5.4) | 1.000 |
| T5 | 54.7 (4.8) | 56.7 (4.5) | 0.003* |
| T10 | 49.3 (4.7) | 52.6 (4) | 0.000* |
| T(+5) | 54 (4.7) | 56 (4.2) | 0.043* |
| T(+10) | 56.2 (4.5) | 58.1 (4.3) | 0.014* |
| T(+15) | 58.6 (4.7) | 60.6 (4.7) | 0.075 |
<0.05. Statistically significant difference. T: Time points described in the “procedure” section. PT: pneumatic tourniquet. SRT: Silicone ring tourniquet
Figure 2.

Changes in values of latency.
Figure 3.
Changes in values of amplitude.
Figure 4.

Changes in values of motor nerve conduction velocity.
Overall, the changes of the values for the nerve conduction studies were more pronounced in the PT test, as compared with the SRT test, particularly in MCV, where the differences were found to be statistically significant. Furthermore, a return to the T0 values (before the tourniquet application) was noticed during the SRT test in 4 volunteers at T+10, while in PT test only in 1 volunteer at T+10 and another at T+15.
Discussion
This study showed that nerve conduction was impaired more severely in the PT group than in the SRT group, according to the changes in nerve amplitude; nevertheless, pain scores and reduction of grip strength were higher in the SRT testing. To our knowledge, this is the first study that investigated the effect of the Silicone Ring Tourniquet on motor nerve conduction in comparison to standard Pneumatic Tourniquet in healthy volunteers.
Pain
Tourniquet pain is related to local phenomena –compression and ischaemia- and there is evidence that more central mechanisms may also be involved (18, 19).
It is not clear whether compression of the skin, muscles and nerves, or ischaemia play the most important role in the etiology of tourniquet pain (20-23).
In our study, the pain score at the time of tourniquet application was higher in SRT group than in PT group. This high initial pain level during the SRT testing gradually subsided and later increased slowly, while the change in pain scores in PT testing was higher and statistically significant. These findings are in accordance to the findings of previous studies (11).
It is likely that the initial high level of pain with the SRT originates locally in skin and muscle, as the narrow size of the silicone ring exerts pressure over a small surface area (13).
Grip strength
The reduction of grip strength may be related to muscle functional changes and is due to muscle injury as well as to nerve conduction impairment (24, 25).
For the SRT test, the reduction of the grip strength was higher (marginally significant; P=0.049). It is possible that the initial changes caused by muscle compression and therefore the functional strength impairment, are more pronounced using the SRT, because the narrow silicone ring exerts the given pressure over a small area of the muscle. In the case of PT test these changes may take more time to be apparent because the given pressure is applied in a wider area.
The reduction of the grip strength in the contralateral upper limb, as was found in the previous study, has been attributed to changes of the sensitivity of neurons, or to very rapid cortical synaptic remodeling, or fast re-organisation of the synaptic system due to short-term deprivation of sensory input by ischaemic nerve block (24, 26-28).
In our study, there was no reduction of the grip strength of the contralateral (non-dominant) hand in the PT test, while in the SRT test this reduction was significant, although nerve conduction was more severely impaired in the PT group than in SRT one.
It is possible that the structural and functional changes of the nerve may be different –at least initially- following the application of these two different tourniquets. If this is the case, the application of the SRT may result in a more rapid deprivation of sensory input. This hypothesis needs to be supported by future studies.
Nerve conduction studies
The findings of this study suggest that the SRT application caused less impairment of the nerve function as compared with the PT. A complete recovery within 15 minutes after the tourniquet removal was found more frequently in volunteers than in the PT group.
In a previously reported study, nerve conduction studies were performed in 20 healthy volunteers after the application of two different pneumatic cuffs – a narrow of 7 cm length and a wide one of 14 cm (6). It was found that the impairment of the motor nerve conduction was greater with the wider cuff as compared with that of the narrow one, despite the fact that the amount of pressure required for occluding the blood supply for the wider cuff was lower. The authors hypothesized that anoxia of the larger area of the nerve could be a possible causal factor for the greater impairment of nerve conduction with the wider 14 cm cuff. This hypothesis is based on the findings of previous studies suggesting that nerve anoxia is more important than mechanical deformation from compression (29, 30).
Furthermore, according to these experimental findings it is not clear whether the damage occurs only to the section of nerve directly under and near the edges of the cuff or it extents more distal to it, with stretching of the paranodal myelin on one side of the node and invagination of the paranodal myelin on the other (22, 23).
According to the results of this study, the reduction of grip strength was higher after the SRT application; nevertheless, nerve conduction was impaired more severely in the PT group than in the SRT group, as this was shown by the changes in nerve conduction studies.
References
- 1.Wakai A, Winter DC, Street JT, Redmond PH. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001;9(5):345–51. doi: 10.5435/00124635-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Moore MR, Garfin SR, Hargens AR. Wide tourniquets eliminate blood flow at low inflation pressures. J Hand Surg Am. 1987;12(6):1006–11. doi: 10.1016/s0363-5023(87)80098-9. [DOI] [PubMed] [Google Scholar]
- 3.Crenshaw AG, Hargens AR, Gershuni DH, Rydevik B. Wide tourniquet cuffs more effective at lower inflation pressures. Acta Orthop Scand. 1988;59(4):447–51. doi: 10.3109/17453678809149401. [DOI] [PubMed] [Google Scholar]
- 4.Hagenouw RR, Bridenbaugh PO, van Egmond J, Stuebing R. Tourniquet pain: a volunteer study. Anesth Analg. 1986;65(11):1175–80. [PubMed] [Google Scholar]
- 5.Estebe JP, Le Naoures A, Chemaly L, Ecoffey C. Tourniquet pain in a volunteer study: effect of changes in cuff width and pressure. Anaesthesia. 2000;55(1):21–6. doi: 10.1046/j.1365-2044.2000.01128.x. [DOI] [PubMed] [Google Scholar]
- 6.Mittal P, Shenoy S, Sandhu JS. Effect of different cuff widths on the motor nerve conduction of the median nerve: an experimental study. J Orthop Surg Res. 2008;3(1):1–6. doi: 10.1186/1749-799X-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boiko M, Roffman M. Evaluation of a novel tourniquet device for bloodless surgery of the hand. J Hand Surg Br. 2004;29(2):185–7. doi: 10.1016/j.jhsb.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Eidelman M, Katzman A, Bialik V. A novel elastic exsanguination tourniquet as an alternative to the pneumatic cuff in pediatric orthopedic limb surgery. J Pediatr Orthop B. 2006;15(5):379–84. doi: 10.1097/01202412-200609000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Orbay H, Unlu RE, Kerem M, Sensoz O. Clinical experiences with a new tourniquet device. Ann Plast Surg. 2006;56(6):618–21. doi: 10.1097/01.sap.0000203988.88955.bc. [DOI] [PubMed] [Google Scholar]
- 10.Norman D, Greenfield I, Ghrayeb N, Peled E, Dayan L. Use of a new exsanguination tourniquet in internal fixation of distal radius fractures. Tech Hand Up Extrem Surg. 2009;13(4):173–5. doi: 10.1097/BTH.0b013e3181b56187. [DOI] [PubMed] [Google Scholar]
- 11.Drosos GI, Stavropoulos NI, Kazakos K, Tripsianis G, Ververidis A, Verettas DA. Silicone ring versus pneumatic cuff tourniquet: a comparative quantitative study in healthy individuals. Arch Orthop Trauma Surg. 2011;131(4):447–54. doi: 10.1007/s00402-010-1144-x. [DOI] [PubMed] [Google Scholar]
- 12.Mohan A, Baskaradas A, Solan M, Magnussen P. Pain and paraesthesia produced by silicone ring and pneumatic tourniquets. J Hand Surg Eur Vol. 2011;36(3):215–8. doi: 10.1177/1753193410390845. [DOI] [PubMed] [Google Scholar]
- 13.Smith OJ, Heasley R, Eastwood G, Royle SG. Comparison of pain perceived when using pneumatic or silicone ring tourniquets for local anaesthetic procedures in the upper limb. J Hand Surg Eur Vol. 2012;37(9):842–7. doi: 10.1177/1753193412449116. [DOI] [PubMed] [Google Scholar]
- 14.Drosos GI, Ververidis A, Stavropoulos NI, Mavropoulos R, Tripsianis G, Kazakos K. Silicone ring tourniquet versus pneumatic cuff tourniquet in carpal tunnel release: a randomized comparative study. J Orthop Traumatol. 2013;14(2):131–5. doi: 10.1007/s10195-012-0223-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drosos GI, Ververidis A, Mavropoulos R, Vastardis G, Tsioros KI, Kazakos K. The silicone ring tourniquet in orthopaedic operations of the extremities. Surg Technol Int. 2013;23(2):251–7. [PubMed] [Google Scholar]
- 16.Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am. 1984;9(2):222–6. doi: 10.1016/s0363-5023(84)80146-x. [DOI] [PubMed] [Google Scholar]
- 17.Chapman CR, Casey KL, Dubner R, Foley KM, Gracely RH, Reading AE. Pain measurement: an overview. Pain. 1985;22(1):1–31. doi: 10.1016/0304-3959(85)90145-9. [DOI] [PubMed] [Google Scholar]
- 18.Crews JC, Cahall MA. An investigation of the neurophysiologic mechanisms of tourniquet-related pain: changes in spontaneous activity and receptive field size in spinal dorsal horn neurons. Reg Anesth Pain Med. 1999;24(2):102–9. doi: 10.1016/s1098-7339(99)90069-x. [DOI] [PubMed] [Google Scholar]
- 19.Cherng CH, Wong CS, Chang FL, Ho ST, Lee CH. Epidural morphine delays the onset of tourniquet pain during epidural lidocaine anesthesia. Anesth Analg. 2002;94(6):1614–6. doi: 10.1097/00000539-200206000-00046. [DOI] [PubMed] [Google Scholar]
- 20.Tsai YC, Lai YY, Chang CL. Comparison of the effect of EMLA cream, subcutaneous ring anaesthesia and a double cuff technique in the prevention of tourniquet pain. Br J Anaesth. 1993;70(4):394–6. doi: 10.1093/bja/70.4.394. [DOI] [PubMed] [Google Scholar]
- 21.Mense S. Nociception from skeletal muscle in relation to clinical muscle pain. Pain. 1993;54(3):241–89. doi: 10.1016/0304-3959(93)90027-M. [DOI] [PubMed] [Google Scholar]
- 22.Ochoa J, Fowler TJ, Gilliatt RW. Anatomical changes in peripheral nerves compressed by a pneumatic tourniquet. J Anat. 1972;113(Pt 3):433–55. [PMC free article] [PubMed] [Google Scholar]
- 23.Pedowitz RA. Tourniquet-induced neuromuscular injury. A recent review of rabbit and clinical experiments. Acta Orthop Scand Suppl. 1991;245(1):1–33. [PubMed] [Google Scholar]
- 24.Prodhomme G, Mouraux D, Dugailly PM, Chantelot C, Fontaine C, Schuind F. Tolerance of upper extremity pneumatic tourniquets and their effect on grip strength. J Hand Surg Eur Vol. 2008;33(3):266–71. doi: 10.1177/1753193408087093. [DOI] [PubMed] [Google Scholar]
- 25.Nitz AJ, Dobner JJ. Upper extremity tourniquet effects in carpal tunnel release. J Hand Surg Am. 1989;14(3):499–504. doi: 10.1016/s0363-5023(89)80011-5. [DOI] [PubMed] [Google Scholar]
- 26.Behbehani MM, Dollberg-Stolik O. Partial sciatic nerve ligation results in an enlargement of the receptive field and enhancement of the response of dorsal horn neurons to noxious stimulation by an adenosine agonist. Pain. 1994;58(3):421–8. doi: 10.1016/0304-3959(94)90137-6. [DOI] [PubMed] [Google Scholar]
- 27.Lundborg G, Richard P. Bunge memorial lecture. Nerve injury and repair--a challenge to the plastic brain. J Peripher Nerv Syst. 2003;8(4):209–26. doi: 10.1111/j.1085-9489.2003.03027.x. [DOI] [PubMed] [Google Scholar]
- 28.Werhahn KJ, Mortensen J, Kaelin-Lang A, Boroojerdi B, Cohen LG. Cortical excitability changes induced by deafferentation of the contralateral hemisphere. Brain. 2002;125(Pt 6):1402–13. doi: 10.1093/brain/awf140. [DOI] [PubMed] [Google Scholar]
- 29.Bostock H, Baker M, Grafe P, Reid G. Changes in excitability and accommodation of human motor axons following brief periods of ischaemia. J Physiol. 1991;441(17):513–35. doi: 10.1113/jphysiol.1991.sp018765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ikemoto T, Tani T, Taniguchi S, Ikeuchi M, Kimura J. Effects of experimental focal compression on excitability of human median motor axons. Clin Neurophysiol. 2009;120(2):342–7. doi: 10.1016/j.clinph.2008.09.082. [DOI] [PubMed] [Google Scholar]


