Abstract
Background:
Intertrochanteric fracture is one of the most common fractures of the hip especially in the elderly with osteoporotic bones, usually due to low-energy trauma like simple falls. Dynamic Hip Screw (DHS) is still considered the gold standard for treating intertrochanteric fractures by many. Not many studies compare the DHS with Proximal femoral nail (PFN), in Type II intertrochanteric fractures (Boyd and Griffin classification). This study was done to compare the functional and radiological outcome of PFN with DHS in treatment of Type II intertrochanteric fractures.
Methods:
From October 2012 to March 2015, a prospective comparative study was done where 30 alternative cases of type II intertrochanteric fractures of hip were operated using PFN or DHS. Intraoperative complications were noted. Functional outcome was assessed using Harris Hip Score and radiological findings were compared at 3, 6, and 12 months postoperatively.
Results:
The average age of the patients was 60 years. In our series we found that patients with DHS had increased intraoperative blood loss (159ml), longer duration of surgery (105min), and required longer time for mobilization while patients who underwent PFN had lower intraoperative blood loss (73ml), shorter duration of surgery (91min), and allowed early mobilization. The average limb shortening in DHS group was 9.33 mm as compared with PFN group which was only 4.72 mm. The patients treated with PFN started early ambulation as they had better Harris Hip Score in the early post-op period. At the end of 12th month, there was not much difference in the functional outcome between the two groups.
Conclusion:
PFN is better than DHS in type II intertrochanteric fractures in terms of decreased blood loss, reduced duration of surgery, early weight bearing and mobilization, reduced hospital stay, decreased risk of infection and decreased complications.
Keywords: Dynamic Hip Screw (DHS), Intertrochanteric fractures, Harris Hip Score, Proximal Femoral Nail (PFN)
Introduction
Intertrochanteric fracture is one of the most common fractures of the hip especially in the elderly with osteoporotic bones, usually due to low-energy trauma like simple falls (1). The incidence of intertrochanteric femoral fractures has increased significantly during recent decades and this tendency will probably continue in the near future due to the rising geriatric population and increase in incidence of osteoporosis. The incidence of intertrochanteric fractures varies from country to country. Gulberg et al. has predicted that the total number of hip fractures will reach 2.6 million by 2025 and 4.5 million by 2050 (2). In 1990, 26% of all hip fractures that occurred in Asia were intertrochanteric fractures whereas this figure could rise to 37% in 2025 and 45% in 2050 (3). The goal of treatment of these fractures is stable fixation, which allows early mobilization of the patient. These fractures are associated with substantial morbidity and mortality. Associated co-morbid medical problem like diabetes, hypertension, pulmonary, renal and cardiac problems add to the insult of the fracture. Elderly patients are threatened with life-threatening complications such as hypostatic pneumonia, catheter sepsis, cardio respiratory failure and decubitus ulcer. All the circumstances mentioned above require using an urgent surgical solution for early rehabilitation and mobilization of the patient (4).
They are also one of the most common fractures encountered in today’s orthopaedic practice. Many treatment options are described aiming for stable fixation, which allows early mobilization of the patient as they are unable to even partially restrict weight bearing (5).
Dynamic Hip Screw (DHS) is still considered the gold standard for treating intertrochanteric fractures by many. The advantages and disadvantages of the DHS have been well established in several studies done in the past (5). Many studies compare the DHS with Gamma nail (6-8). Not many studies compare the DHS with Proximal femoral nail (PFN), which is being preferred by many. This study was conducted to compare the functional and radiological outcome of Proximal femoral nail (PFN) with Dynamic hip screw (DHS) in treatment of Type II intertrochanteric fractures (Boyd and Griffin classification).
Materials and Methods
This was a prospective comparative study conducted from October 2012 to March 2015. During this period 30 adult patients with type II Intertrochanteric fractures of femur were selected according to the inclusion criteria. Alternate patients who fulfilled the inclusion and exclusion criteria underwent PFN or DHS respectively.
Inclusion Criteria: Age more than18 years.
Sex: Both sexes.
Type 2 (Boyd and Griffin classification) intertrochanteric fracture.
Fractures less than 2 weeks of duration.
Exclusion Criteria: Pathological fractures.
Polytrauma.
Patients with co-morbid conditions like stroke that may hinder rehabilitation.
Standard pre-operative planning was done. Radiographs of the pelvis with both hips antero-posterior view and traction-internal rotation view was obtained to confirm the diagnosis.
The length of Richard’s screw was measured pre-operatively on radiographs subtracting magnification. Neck shaft angle was measured to determine the angle for barrel plate. Non-locking DHS plate (sharma surgicals) with minimum of 6 cortices were fixed to the shaft distal to the fracture. In case of PFN, a standard length of 250 mm and 135° angle nail was used in all our cases (sharma surgicals). The diameter was determined by measuring diameter of the femur at the level of isthmus on an AP X-ray. All cases were operated on a single standard fracture table under spinal anaesthesia using standard operating techniques. C-arm was used in all cases. As a standard protocol, intra-venous cefoperazone and sulbactum 1.5 gms was administered intravenously prior to the skin incision. The same combination was used for 48 hours postoperatively in standard doses. Intra-operatively the duration of surgery, the radiation exposure, intra-operative blood loss (method of Lee et al.), size of the incision and any associated complications were noted (9).
All patients in our study underwent a similar rehabilitation protocol involving mobilization from the second postoperative day depending upon the physical condition of the patient, static quadriceps, knee and ankle mobilisation exercises. All drains were removed by 48 hrs. The wounds were inspected on the 2nd post operative day. Stitches were removed between 10th-14th day. Functional outcome was assessed using Harris Hip Score and radiological findings were compared at 3months, 6months and 12 months post operatively. All patients were followed up for a minimum period of 1 year. There were no drop-outs in the study.
Statistical analysis was performed with the SPSS version 13.0 software for Windows and P<0.05 was chosen to indicate statistical significance.
Results
Out of the 30 patients, 16 patients (53%) were males and 14 patients (47%) females. In our study, the average age was 60 years with 85 years being the maximum and 28 years being the minimum. We found that intertrochanteric fractures due to trivial trauma (77%) was the most common mode of injury, followed by road traffic accidents (23%). Patients with road traffic accidents were younger while patients with trivial trauma were older. 50% of the fractures occurred on the left side and 50% on the right side showing no significant difference. As the surgical approach suggests, PFN requires a smaller incision (6.1 cm) to access the entry site into the medullary canal compared to DHS which was found to be more than twice the length (17cm). Since distal locking was done using percutaneous stab incisions in PFN, very minimal incisions were required to complete the procedure. The duration of surgery was calculated from the time of incision to skin closure. The average duration of surgery for PFN was 90.6 mins, which was shorter than the average time required for DHS (105.3 mins)(P=0.04). Following surgery, all swabs and mops with blood contamination from the surgical procedure were weighed to determine the amount of blood loss, similar to the method of Lee et al. (9). The average blood loss during PFN procedure was 73ml, which was significantly less than DHS procedure (159ml)(P=0.001). 5 out of 15 patients in DHS group required blood transfusion either intra or postoperatively. Since the incision was smaller and duration of surgery was shorter in PFN, there was less tissue damage and hence lesser blood loss.
The sliding of both groups was compared at the end of 1 year on the radiographs as described by Hardy et al. there was an average of 4.3 mm of sliding in the P.F.N group as compared to 6.9 mm in the DHS group (P=0.001) (10). The average limb shortening in DHS group was 9.33 mm as compared with PFN group which was only 4.72 mm (P=0.02). Even though there was more shortening in the D.H.S group it was not significant enough to cause any gait or functional impairment. The average hospital stay was 12.4 days (8 -14 days) in case of DHS while 7.8 days (4-12 days) in case of PFN (P=0.001). Return to pre-injury walking ability in DHS group was on an average of 12 weeks compared to PFN which was 8 weeks (P=0.03).
Out of 15 patients, 5 patients (33%) required opening of the fracture site in DHS group. Two patients had medial communition requiring additional bone grafting procedure from the ipsilateral iliac crest. Remaining three of them had soft tissue interposition in between the fracture fragments requiring open reduction. Two of these were underwent bone grafting. In PFN group, 3 patients had jig miss match (20%), 1 underwent open reduction (6.7%) and in 1 patient only one cephalic screw was placed (6.7%) as the other screw could not be accommodated. Patients with jig miss match underwent free-hand screw locking [Table 1]. The average Tip-Apex-Distance (TAD) in DHS group was 18.3 mm (range 12-24 mm).
Table 1.
Intra-operative complications in each group and additional Procedures carried out in each group
| DHS (n=15) | PFN (n=15) | |
|---|---|---|
| Intra-operative complications | Open reduction – 5 (33.3%) | Jig mismatch – 3 (20%) Open reduction – 1 (6.7%) Solitary cephalic Screw – 1 (6.7%) |
| Additional Procedures | Bone grafting - 4 (26.7%) Bone Marrow infiltration. – 3 (20%) |
Bone grafting – 2 (13.3%) Bone Marrow infiltration – 2 (13.3%) |
As PFN is an intra medullary load sharing device as compared to DHS which is a load bearing device, full and partial weight bearing was started at an early stage for PFN patients [Table 2].
Table 2.
showing the average number of days/weeks taken for post-operative patient mobilization in each group
| Patient Mobilization | DHS (n=15) | PFN(n=15) |
|---|---|---|
| Active hip and knee mobilization | 4.27 days | 2.33 days |
| Non-weight bearing crutch walk | 2.93 weeks | 1.53 weeks |
| Partial weight bearing walking | 7.87 weeks | 3.73 weeks |
| Full weight bearing walking | 11.80 weeks | 7.93 weeks |
Radiological outcome was assessed at 3months, 6months and 12th month post-op. At 3 months post-op, 11 patients in both groups showed attempted callus formation. Four patients in the DHS group were found to have attempted callus formation with a gap. While in the PFN group, 2 patients who underwent bone grafting showed good integration of the graft while the remaining two patients showed callus formation with minimal gap.
At 6 months post-op, we found few variations and complications in both the groups. In the PFN group, all the 15 patients showed good union of fracture while the other 2 patients who underwent bone grafting had good graft integration with union [Figure 1]. Two patients had backing out of the proximal cephalic screw in the PFN group but both of them united without any complications [Figure 2]. Implant exit for these cases were done at 13th and 15th month respectively. In the DHS group, 6 patients had collapse at fracture site and 8 patients showed solid union at the fracture site [Figure 3]. One patient had varus malunion of 120 degrees due to excessive collapse.
Figure 1.
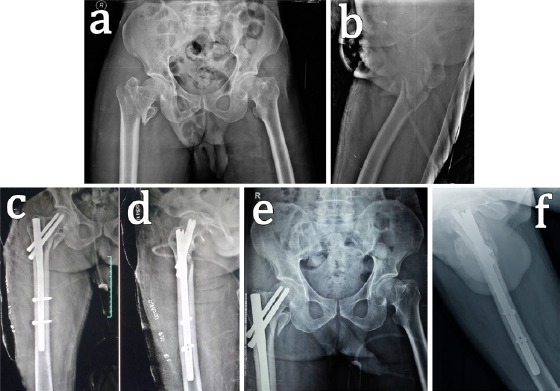
Radiographs of a 56-year-old male with right sided type-II intertrochanteric fracture operated with PFN. (a and b) Pre-operative antero-posterior and lateral view radiographs showing type II intertrochanteric fracture. (c and d) Immediate post operative radiographs showing good reduction of fracture with PFN in-situ. (e and f) Antero-posterior and lateral radiographs showing union at 12 weeks of follow up.
Figure 2.
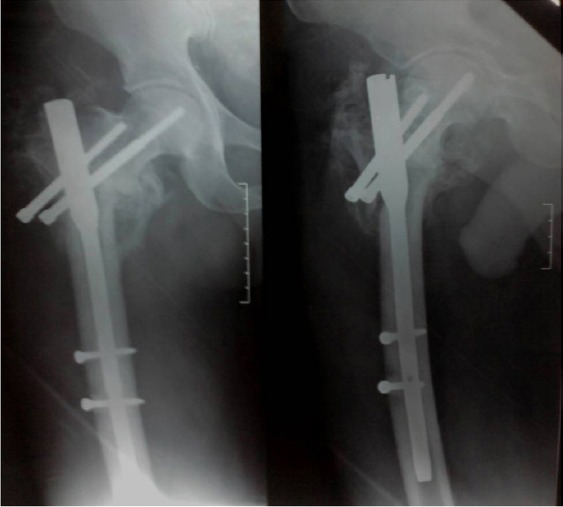
Radiographs showing backing out of proximal cephalic screw with exuberant callus at the fracture site in a 60 year old patient treated with PFN.
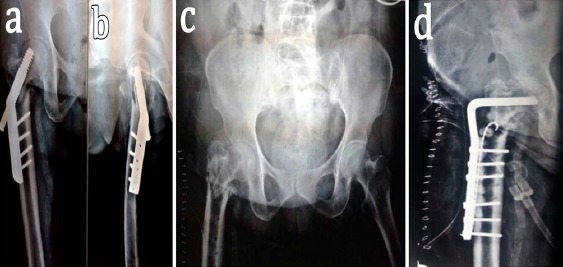
Figure 3.
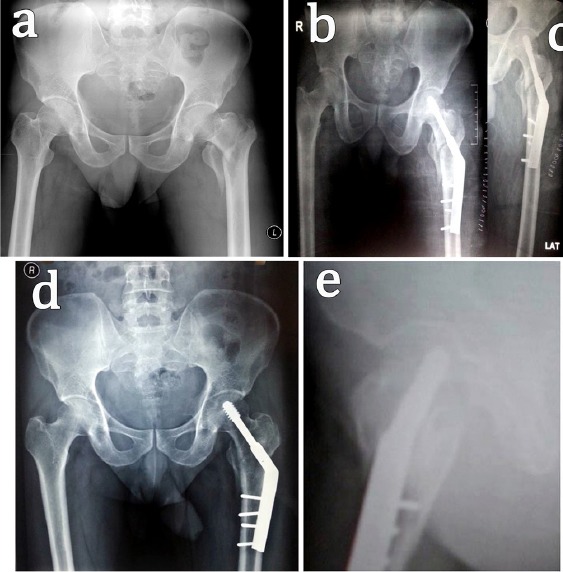
Radiographs of a 71-year-old male patient with left sided type-II intertrochanteric fracture fixed with DHS. (a) Pre-operative antero-posterior view of left sided type II intertrochanteric fracture. (b and c) Immediate radiographs showing good reduction of fracture fragments with DHS in-situ. (d and e) Antero-posterior and lateral view radiographs showing good union at 12 weeks follow up.
At 12 months post operative, we found 13 patients in the DHS group had complete union of the fracture site with one patient continuing to have union in 120 degree of varus which did not progress [Figure 4]. One patient sustained a peri-implant fracture just below the tip of the DHS plate following a road traffic accident at 7th month post-op. The fracture occurred through the last screw (stress raiser) for which the DHS plate was removed and the fracture was fixed with longer plate (10 holed). The plate alone was changed retaining the Richard screw. The patient was followed up till union [Figure 5]; which took about 4 months post re-surgery [Table 3]. No such complications were noted in the PFN group, all the 15 patients showed good union of fracture at 12 months post-op.
Figure 4.

Radiographs of a 70-year-old male who had varus malunion (120 degrees) due to excessive collapse at the fracture site. (a and b) Antero-posterior and lateral radiographs with varus collapse at 6 months post-op. (c and d) Radiographs showing the varus union persisting after implant removal.
Figure 5.
A 65-year-old male with peri-implant fracture at 7th month post-op. (a) Antero-posterior view showing the peri-implant fracture at the distal end of the plate. (b and c) Radiographs of the immediate post-op after plate exchange and fixation. (d and e) Antero-posterior and lateral view radiographs at 4 months post-re-surgery showing union of peri-implant fracture and intertrochanteric fracture.
Table 3.
Showing the radiological outcome of DHS and PFN groups
| Follow-up month | DHS(n=15) | PFN(n=15) |
|---|---|---|
| 3rd Month | ACF# + Gap – 4 (26.7%) ACF – 11 (73.3%) |
ACF – 11 (73.3%) ACF + ^ BG Integration – 2 (13.3%) ACF With Gap – 2 (13.3) |
| 6th Month | CAFS* – 6 (40%) CF – 8 (53.3%) United In Varus – 1 (6.67%) |
CF – 11 (73.3%) CF** + BG Integrated – 2 (13.3%) Z Effect – 2 (13.3%) |
| 12th Month | Complete Union – 12 (80%) United In Varus – 1 (6.67%) Re-fracture – 1 (6.67%) Infection – 1 (6.67%) |
Complete union – 13 (86.7%) Z Effect with Union– 2 (13.3%) |
ACF: attempted callous formation;
CAFS: callous at facture site;
BG: Bone Grafting,
CF: Callous Formation
There was one case of infection in DHS group. She was diagnosed to have infected non-union and she underwent implant removal. Deep cultures taken intra-op, showed no growth of organisms. She was initially managed with a upper tibial pin traction for two weeks and then later fixed with condylar blade plate fixation with bone grafting and antibiotic beads insertion near the fracture site [Figure 6]. On 5th day post operative, she had sero-sanguineous discharge from the operated site for which she underwent multiple wound washes and repeated cultures were taken. Cultures showed growth of Staphylococcus aureus. Intra venous antibiotics were prescribed according to the antibiotic sensitivity. She expired 2 months after the second procedure.
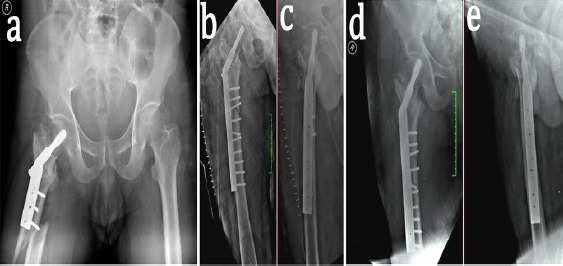
Figure 6.
Post-DHS infection in a 67-year-old female. (a and b) Antero-posterior and lateral view radiographs showing backing out of the Richard screw with non-union at the fracture site. (c) Radiograph of pelvis post implant exit showing non-union at the fracture site. (d) Antero-posterior radiograph showing condylar blade plate fixation of the infected non-union with bone grafts and antibiotic beads in-situ.
At the end of 3 months, we found that the functional results calculated using the Harris hip score in patients of DHS group scored an average of 32.67 compared to PFN group that showed 52.87 (P=0.001). Scores increased to 67.6 and 85.4 for DHS and PFN group respectively at the end of 6 months (P=0.001). But at the end of 12th month, the average functional scores in the DHS group increased to 89.08 as compared to PFN group which was 90.33 (P=0.31). There was not much significance between the two groups [Table 4].
Table 4.
Average Functional Score (Harris Hip Score)
| FUNCTIONAL SCORE (Follow-up) | DHS (n=15) | PFN (n=15) |
|---|---|---|
| 3 MONTHS | 32.67 | 53.87 |
| 6 MONTHS | 67.60 | 85.40 |
| 12 MONTHS | 89.08 | 90.33 |
Discussion
In the last few decades treatment of intertrochanteric fractures has evolved significantly. Various methods of fixation devices have come and gone. The treatment still merits the type of fracture and quality of bone. DHS has been the considered the gold standard of intertrochanteric fracture fixation for a long time.
Historically, Smith Peterson nail and Jewet nail were introduced in the 1930’s. In the 1950’s and 60’s Pugh and Massie modified sliding devices and dynamic hip screw (DHS) were developed. Kuntscher, Zickle, Grosse, Kempf and Russel and Taylor developed intramedullary nail (IMN) with sliding hip screw (SHS) (11-13). In the early 90s intramedullary devices were developed for fixation of Intertrochanteric fractures. These devices had numerous biomechanical and biological advantages over the conventional dynamic hip screw. The advantages and disadvantages of the original design of the Gamma nail have been well established in several studies done in the past, usually by comparing the results with the dynamic hip screw (DHS) (10,14,15).
Recent data suggests intra-medullary devices have been very good with union rates up to 100% compared with other extra-medullary devices which show union up to 80% only (14,15).
Kyle et al. has noted that increased forces are required to initiate sliding in intra medullary devices as compared to sliding hip screw with plate (16). Amongst all intra medullary devices the Gamma nail requires the largest force. The explanation lies in the barrel of the side plate, the barrel provides a free passage for the screw to slide, thus the longer the barrel length the less the forces required to initiate sliding. The nail in the medullary canal provides a physical block to significant shortening of the head and neck segments in the fractures which explains the minimum shortening in the PFN group as compared to DHS group (11). Randomized post-op rehabilitation study by Pajarinen et al. comparing peritrochanteric femoral fracture treated with DHS or PFN suggested that the use of PFN may allow faster post operative restoration of walking ability when compared to DHS (17). In our study patients who underwent PFN returned to pre-injury walking status earlier than patients who underwent DHS. Proximal femoral nailing creates a shorter lever arm, which translates to a lower bending moment and a decreased rate of mechanical failure (10). PFN has shown to be more biomechanically stronger because they can withstand higher static and several fold higher cyclical loading than dynamic hip screw. The implant compensates for the function of the medial column. Proximal femoral nail also acts as a buttress in preventing the medialization of the shaft (18,19).
PFN is better than DHS in Type II intertrochanteric fractures of femur in terms of decreased blood loss, reduced duration of surgery, early weight bearing and mobilization, reduced hospital stay, decreased risk of infection and other complications (20). It is just a matter of time that PFN replaces DHS as the gold standard for Type II intertrochanteric fractures.
References
- 1.Dimon JH, Hughston JC. Unstable intertrochanteric fractures of the hip. J Bone Joint Surg Am. 1967;49(3):440–50. [PubMed] [Google Scholar]
- 2.Gulberg B, Johnell O, Kanis JA. World-wide projection for hip fractures. Osteoporos Int. 1997;7(5):407–13.3. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 3.Melton LJ, 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, et al. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20(5):687–94. doi: 10.1007/s00198-008-0742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kulkarni GS, Limaye R, Kulkarni M, Kulkarni S. Intertrochanteric fractures. Indian J Orthop. 2006;40(1):16–23. [Google Scholar]
- 5.Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949;31B(2):190–203. [PubMed] [Google Scholar]
- 6.Bridle SH, Patel AD, Bircher M. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73(2):330–4. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 7.Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993;75(5):789–93. doi: 10.1302/0301-620X.75B5.8376441. [DOI] [PubMed] [Google Scholar]
- 8.O’Brien PJ, Meek RN, Blachut PA, Broekhuyse HM, Sabharwal S. Fixation of intertrochanteric hip fractures: gamma nail versus dynamic hip screw: A randomized, prospective study. Can J Surg. 1995;38(6):516–20. [PubMed] [Google Scholar]
- 9.Lee MH, Ingvertsen BT, Kirpensteijn J, Jensen AL, Kristensen AT. Quantification of surgical blood loss. Vet Surg. 2006;35(4):388–93. doi: 10.1111/j.1532-950X.2006.00162.x. [DOI] [PubMed] [Google Scholar]
- 10.Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998;80(5):618–30. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Kuntscher G. A new method of treatment of pertrochanteric fractures. Proc R Soc Med. 1970;63(11 Part 1):1120–1. doi: 10.1177/003591577006311P118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grosse A, Kempf I, Lafforgue D. Treatment of fragments, loss of bony substance and pseudarthrosis of femur and tibia using screw fixation (40 cases)in French. Rev Chir Orthop Reparatrice Appar Mot. 1978;64(2):33–5. [PubMed] [Google Scholar]
- 13.Russell TA. Fractures of hip and pelvis. In: Crenshaw AH, Wenger Dr, editors. Campbell’s Operative Orthopaedics. 8th ed. St Louis: CV Mosby; 1992. pp. 895–7. [Google Scholar]
- 14.Spivak JM, Zuckerman JD, Kumme FJ. Fatigue failure of sliding hip screw in hip fracture fixation: a report of three cases. J Orthop Trauma. 1991;5(3):325–31. doi: 10.1097/00005131-199109000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Leung KS, So WS, Shen WY, Hui PW. Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomized prospective study in elderly patients. J Bone Joint Surg Br. 1992;74(3):345–51. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 16.Kyle RF, Wright TM, Burstein AH. Biomechanical analysis of the sliding characteristics of compression hip screws. J Bone Joint Surg Am. 1980;62(8):1308–14. [PubMed] [Google Scholar]
- 17.Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with dynamic hip screws or a proximal femoral nail: A randomized study comparing post-operative rehabilitation. J Bone Joint Surg Br. 2005;87(1):76–81. [PubMed] [Google Scholar]
- 18.Boldin C, Seibert FJ, Fankhauser F, Peicha G, Grechenig W, Szyszkowitz R. The proximal femoral nail (PFN)--a minimal invasive treatment of unstable proximal femoral fractures: a study of 55 patients with a follow-up of 15 months. Acta Orthop Scand. 2003;74(1):53–8. doi: 10.1080/00016470310013662. [DOI] [PubMed] [Google Scholar]
- 19.Nuber S, Schoweiss T, Ruter A. Stabilization of unstable trochanteric femoral fractures. Dynamic hip screw (DHS) with trochanteric stabilisation plate vs. proximal femur nail (PFN) Unfallchirurg. 2003;106(1):39–47. doi: 10.1007/s00113-002-0476-6. [DOI] [PubMed] [Google Scholar]
- 20.Peivandi MT, Kachooei AR, Nazemian Z. New method to remove a broken guide pin in the hip joint. Orthopedics. 2011;34(10):e685–7. doi: 10.3928/01477447-20110826-25. [DOI] [PubMed] [Google Scholar]


