Abstract
Background:
The aim of this study was to determine the treatment outcome of humeral shaft fractures with a locked rigid intramedullary nail in patients indicated for surgical treatment.
Methods:
In this descriptive-cross sectional study, all patients were followed up for one, six, and 18 months post operatively. The Short Form Questionnaire (SF-36) and Constant Shoulder Score were applied.
Results:
Of 78 included patients (mean age: 35), one patient had a soft tissue infection, one had secondary radial nerve palsy, eight had non-union, one had elbow limited range of motion in extension, and three patients had decreased shoulder range of motion. The Constant Shoulder Score and Short Form Questionnaire Score (SF-36) increased in all patients, although aged women showed lower improvement.
Conclusion:
Intramedullary nail fixation in the humeral shaft fracture may be associated with high rates of non-union.
Keywords: Humeral shaft fractures, Nailing, Orthopedic procedures, Treatment outcome
Introduction
Humerus fractures comprise 1-7% of all fractures and are the third most common fractures in the elderly, after hip and wrist fractures (1-3). Isolated humeral shaft fracture counts for 1-3% of all fractures and in many patients is due to closed trauma (3,4).
Fortunately, non-operative methods are effective in treating the majority of humeral shaft fractures. In patients with surgical indication two different models are available: compression plate and intramedullary nailing (with open and closed approaches) and each one has its advantages and disadvantages (3,4). With plate and screw fixation, we may achieve more rigid fixation; however, in intramedullary nailing, fracture site soft tissue manipulation is much less (3,4). Closed locked nailing is a successful alternative for femoral, tibial, and humeral shaft fracture treatment (5,6). Also, segmental fracture, pathological fracture, obesity, burn injuries and multiple fractures are indications for intramedullary nailing and contraindications are chronic shoulder pain, wheel chair bound patients, radial nerve palsy and humeral canal size less than nine millimeters (7).
Because of the significant morbidity that has been reported following the operative treatment of humeral shaft fractures, we reviewed our experience with a series of such fractures that were treated by intramedullary fixation at our hospital. In this study we present surgical outcomes, technical errors and complications.
Materials and methods
This descriptive cross-sectional study (2008-2012) comprised of 274 patients with humeral shaft fractures over 16 years old who were referred to our academic tertiary referral hospital. Seventy-eight of the patients had indications for intramedullary nailing with a 7-8 mm diameter steel nail, and all were treated by the senior author. The study protocol was approved by the institutional review board and ethical committee. All these patients were initially treated the first 48 hours after admission. Only three patients with multiple traumas was treated dilatory within a maximum of one week after injury. Open Gustilo type III fractures, proximal fractures within four centimeters of the surgical neck, distal fractures within three centimeters of diaphysis-metaphysis junction, and shaft fractures extending into the greater tubercle were excluded.
The indications for operative treatment were patients with multiple fractures (n=51), pathologic fractures (n=3), segmental fractures (n=19), a burn patient (n=1), and patients with BMI>30 (n=4). Seventy-three patients had closed fractures and five patients had open fractures. Fifty-nine fractures were treated with the closed approach and 19 were treated with the open approach.
Before beginning the treatment, therapeutic protocols, and their advantages and disadvantages were completely explained to all patients orally and informed consent was obtained.
Pre-operation planning
High quality anteroposterior and lateral radiographs of the injured extremity were obtained to learn about the fracture pattern, presence of comminution, medullary canal dimensions, and bowing of the humerus. The length of the nail was measured as the distance between two centimeters over the olecranon fossa and lower edge of greater tuberosity on the uninjured extremity radiograph after correcting for magnification.
Surgery technique
The fracture was reduced with gentle longitudinal traction and manipulation. If the reduction procedure failed three times, or if there were any neurovascular injuries, the open technique was selected. After reduction, the entry point for the nail was the greater tuberosity, just lateral to the articular margin. We broached the canal with a reamer and the nail was passed across the fracture site. In case of nonunion, nail removal plating and bone grafting were performed. Postoperative external support consisted of a sling and an elastic bandage. Physiotherapy was initiated gently the first day after surgery, followed by gradually active range of motion exercises when the Codman exercises (5) ceased to be painful.
All patients dismissed in 48 hours after surgery. All patients demographic features, including age, sex and mechanism of trauma were recorded before the follow up begin. Times of follow up visits in all patients were month one, sixth, and 18th after surgery.
Post-op evaluation
In the month one (Visit A), sixth (Visit B), and 18th (Visit C) after surgery, each patient was examined by another surgeon. Complications were recorded and shoulder subjective outcome was evaluated using a combination of the Constant Shoulder Score, Short Form Questionnaire (SF-36).
Union was defined as the absence of motion at the fracture site with manual manipulation and the consolidation of visible callus as seen on radiographs. A nonunion was present if the fracture did not reach the union by six months after injury. Other complications in this study were: mal-union, secondary radial nerve palsy, soft tissue infection, and limited range of motion in the elbow or shoulder joints.
Constant score is a valid tool to evaluate the function of the shoulder. This scoring system (range: 0-100) consists of four variables (pain, daily living activities, range of motion, power) that are used to assess the range of motion and limb strength. Range of motion was measured by the Goniometer and the favorable score for this tool is between 60-70 points (8-9).
The Short Form Questionnaire (SF-36) is a valid tool to evaluate the health of patients. It is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of treatment. This tool consists of eight different scaled scores that grade each patient with points from 0-100. The reliability and validity of this evaluation form was confirmed by Montazeri et al. (10).
Demographic characteristics (age and gender) and the above mentioned criteria were recorded and were statistically analyzed using the SPSS software package for Windows version 19 (SPSS Inc., Chicago, IL, USA). All quantitative numeric values are expressed as mean± standard deviation. The chi-square test was used to compare differences in the qualitative parameters. Analysis of variance (ANOVA) was used to compare parametric continuous data among several groups, and the t test was employed to analyze parametric continuous data. In all statistical tests, the alpha level was set at 0.05.
Results
Of the 78 included patients (mean age: 35), 63 patients (81%) were male and 15 patients (19%) were female. Five patients (6%) had open fractures and 73 patients (94%) had closed fractures. In 75 patients, fractures occurred following an acute trauma and in three other patients pathological fractures occurred because of bony tumors. The most common mechanism of trauma among these patients was car to car accidents (33%) followed by motorcycle to car accidents (28%).
The open approach used in 53 patients (68%) and the closed approach in 25 patients (32%). The mean time of the procedure in the close method was 30 minutes versus 40 minutes in the open method. There were no significant differences between the approaches (P=0.135). Three patients with primary radial nerve palsy improved after surgery. Complications recorded during the follow-up visits were: one patient with malunion, one with secondary radial nerve palsy (a 29-year-old female with a segmental humeral fracture; radial function returned itself after 4 months), three patients with nail protrusion from the humeral head that caused decrease shoulder range of motion [Figure 1], one patient with elbow limited range of motion caused by entering the nail into the olecranon fossa [Figure 2], and eight patients with nonunion after six months. One was a 47-year-old male with a segmental fracture during a motorcycle collision with an automobile [Figure 3a]. Another patient was a 52-year-old female with multiple fractures and BMI>30 injured as a pedestrian an automobile accident [Figure 3b]. The third patient was a 40-year-old female with multiple fractures and diabetes type I, who was injured as a pedestrian in an automobile accident [Figure 3c]. All of the nonunion patients were treated with nail removal and bone plating with autogenic bone graft.
Figure 1.

Decreased shoulder range of motion caused by nail protrusion out of the humeral head.
Figure 2.

Elbow limited range of motion caused by nail protrusion into the olecranon fossa.
Figure 3a.
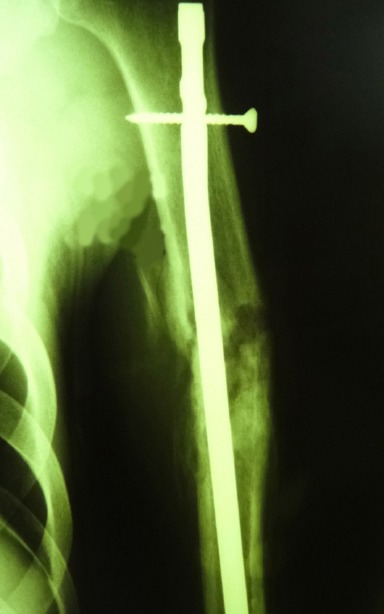
Nonunion in a 47-year-old man with a segmental fracture during a motorcycle collision with an automobile.
Figure 3b.

Nonunion in a 52-year-old female with multiple fractures.
Figure 3c.

Nonunion in a 40-year old woman with multiple fractures.
In visits A, B and C, the Constant shoulder score and SF-36 were used to evaluate all patients. The mean Constant shoulder score in visit A was 73, in visit B was 81, and in visit C was 89 among all patients. There was significant differences between the groups (P=0.016). Also, the mean SF-36 score in visit A was 77, in visit B was 82, and in visit C was 91 (P=0.017). Our findings showed that with the increase of age, shoulder subjective performance (SF-36 and constant shoulder scores) severely decreased and there was a reverse significant correlation (r SF-36, age=-0.417, P=0.005 r constant scores, age= -0.365, P=0.014).
In both the SF-36 and constant shoulder scores, the lowest score obtained in those in the over 50 age group (P<0.001) and scores in female patients was lower than males (P<0.001). The results showed that the mean time of union in the closed approach was 85 days versus 102 days in the open method (P=0.03).
Discussion
The choice of operative treatment in the humeral shaft fracture depends on multiple factors: fracture indications, associated injuries, and patient indications (11, 12). The goal of the operative treatment of humeral shaft fractures is to reestablish length, alignment, and rotation with stable fixation that allows early motion and ideally early weight bearing on the fractured extremity (13-15).
In our study the constant shoulder score and average time for union was better than Firat et al.’s study (score of 82 versus score of 74 and 85-102 days versus 100 days respectively) (16). Moreover, Firat et al. reported that due to possible self-rotation of the nail, displacement of the nail or screw and hypoperfusion in the area of entering the nail happened in intramedullary nailing of the humerus. Also, the high risk of shoulder impingement syndrome and restriction of shoulder and elbow joints was observed, but in our study such complications were observed minimally or not at all. The reason for these differences is that in our study, proper length of the nail was determined before surgery on the basis of intact limb radiograph (pre-operation planning) and physiotherapy initiated immediately after surgery. On the other hand, we applied screws to stabilize and prevention nail rotation or nail displacement. Our good results were similar to several other studies (17-24).
Preoperative planning provides numerous benefits to a surgeon. Formal planning increases surgical efficiency and decreases stress in the operating room (25, 26). The length of the nail is carefully chosen and if too long of a nail is selected, one risk is distracting the fracture site as the nail impacts the tapered end of the humeral canal as it is advanced in an attempt to seat it below the tuberosity proximally. Leaving the nail proud proximally will result in an increased incidence of impingement. So we used this method of measuring to improve our results and decrease patient complications.
As time passed, this study showed a progression in the SF-36 scores and constant shoulder score, indicating fractures and surgery complications progressively decreased. Infection incidence was reduced by medical treatment, radial nerve damage diminished and nerve function progressively returned to normal status. Also, by physiotherapy and limb muscle empowering, arm function improved as well.
The most common cause of shoulder movement restriction is the excess length of the nail that brings the risk of ejection from the humeral head. Therefore, selection of the precise length of the nail is very important to avoid such a disorder. It is recommended to hide the proximal head of the nail completely under the humeral head cartilage. Moreover, fluoroscope should be used carefully to control the point of nail insertion.
Taking a detailed history of shoulder pain, doing a thorough physical examination for range of shoulder movement, and performing the required radiography to assess previous pathology in the shoulder joint are recommended. Furthermore, physiotherapy immediately after the operation to obtain proper elbow and shoulder joint motion is necessary. Inserting the distal screw, conducting fluoroscopy for fracture site assessment and reduction are also mandatory.
The limitations of our study are that it is a descriptive one and there is no control group to compare the results. The present study had other limitations that might have influenced the outcomes as well, such as the sample size of 78 patients might not have been adequate for conclusive evidence of statistically significant differences between the scores. Our study was not a multi-centric one and it may weaken the generalizability of the study. Finally, we did not undertake any explanatory analyses. Instead, we suggested that the results of the present investigation could be useful in the development of further investigations.
Intramedullary nail fixation in the humeral shaft fracture may be associated with high rates of non-union. A clinical trial on this method is recommended.
References
- 1.Ekholm R, Tidermark J, Tornkvist H, Adami J, Ponzer S. Outcome after Closed Functional Treatment of Humeral Shaft Fractures. J Orthop Trauma. 2006;20(9):591–6. doi: 10.1097/01.bot.0000246466.01287.04. [DOI] [PubMed] [Google Scholar]
- 2.Dağlar B, Delialioğlu OM, Taşbaş BA, Bayrakçi K, Ağar M, Günel U. Comparison of plate-screw fixation and intramedullary fixation with inflatable nails in the treatment of acute humeral shaft fractures. Acta Orthop Traumatol Turc. 2007;41(1):7–14. [PubMed] [Google Scholar]
- 3.Saka G, Saglam N, Kurtulmus T, Özer C, Uqurlar M, Akpinar F. Interlocking intramedullary ulna nails in isolated ulna diaphyseal fractures: a retrospective study. Acta Orthop Traumatol Turc. 2013;47(4):236–43. doi: 10.3944/aott.2013.3021. [DOI] [PubMed] [Google Scholar]
- 4.Oztürk I, Ertürer E, Uzun M, Akman S, Seçkin F. The effectiveness of functional bracing in the conservative treatment of humeral diaphyseal fractures. Acta Orthop Traumatol Turc. 2006;40(4):269–73. [PubMed] [Google Scholar]
- 5.Canale TS, Beaty JH. Campbell’s operative orthopedics. 12th ed. Hardcover; 2013. [Google Scholar]
- 6.Hall Rf, Pankovich Am. Ender nailing of acute fracture of humerus. A study of closed fixation by intramedullary nailing without reaming. J Bone joint surg AM. 1987;69(4):558–67. [PubMed] [Google Scholar]
- 7.Bucholz RW, Green DV, Rockwood CA. Rockwood and Green’s fractures in adult. 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 8.Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14(3):279–85. doi: 10.1016/j.jse.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–4. [PubMed] [Google Scholar]
- 10.Montzeri A, Gohoshtasbi A, Vahdaninia M, Gandek B. The short form health survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14(3):875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 11.Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. Injury. 2010;41(7):e21–27. doi: 10.1016/j.injury.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Robinson CM, Bell KM, Court-Brown CM, McQueen MM. Locked nailing of humeral shaft fractures. Experience in Edinburgh over a two-year period. J Bone Joint Surg Br. 1992;74(4):558–62. doi: 10.1302/0301-620X.74B4.1624516. [DOI] [PubMed] [Google Scholar]
- 13.Stern PJ, Mattingly DA, Pomeroy DL, Zenni EJ, Jr, Kreig JK. Intramedullary fixation of humeral shaft fracture. J Bone Joint Surg Am. 1984;66(5):639–46. [PubMed] [Google Scholar]
- 14.Chapman JR, Henley MB, Agel J, Benca PJ. Randomized perspective study of humeral shaftfractures fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14(3):162–6. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Kesemenli CC, Subasi M, Arslan H, Necmioglu S, Kapukaya A. Comparison between the results of intramedullary nailing and compression plate fixation in the treatment of humerus fractures. Acta Orthop Traumatol Turc. 2003;37(2):120–5. [PubMed] [Google Scholar]
- 16.Firat A, Deveci A, Güler F, Ögüder A, Oǧuz T, Bozkurt M. Evaluation of shoulder and elbow functions after treatment of humeral shaft fractures: a 20-132-month follow-up study. Acta Orthop Traumatol Turc. 2012;46(4):229–36. doi: 10.3944/aott.2012.2486. [DOI] [PubMed] [Google Scholar]
- 17.Lin J. Treatment of humeral shaft fracture with humeral locked nail and comparison with plate fixation. J Trauma. 1998;44(5):859–64. doi: 10.1097/00005373-199805000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Lin J, Hou SM. Antegrade locked nailing for humeral shaft fractures. Clin Orthop Relar Res. 1999;(365):201–10. doi: 10.1097/00003086-199908000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Stannard JP, Harris HW, McGwin G, Jr, Volgas DA, Alonso JE. Intramedullary nailing of humeral shaft fractures with a locking flexible nail. J Bone Joint Surg AM. 2003;85(11):2103–10. doi: 10.2106/00004623-200311000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Brumback RJ, Bosse MJ, Poka A, Burgess AR. Intramedullary stabilization of humeral shaft fractures in patients with multiple trauma. J Bone Joint Surg Am. 1986;68(7):960–70. [PubMed] [Google Scholar]
- 21.Diaza SM, Ramíreza M, Marquésa F, Gines A, Monllau JC, Martinez-Gomez X, et al. Rigid intramedullary nailing of humeral shaft fractures in patients older than 60. Rev Ortop Traumatol. 2006;50(1):8–13. [Google Scholar]
- 22.Farahini H, Noruzi M, Naderi MN. Surgical treatment of humeral shaft fractures by interlocking nailing. KAUMS J (FEYZ) 2005;8(4):52–7. [Google Scholar]
- 23.Heineman DJ, Poolman RW, Nork SE, Ponsen KJ, Bhandari M. Plate fixation or intramedullary fixation of humeral shaft fractures. Acta Orthop. 2010;81(2):216–23. doi: 10.3109/17453671003635884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhandari M, Devereaux PJ, Mckee MD, Schemitsch EH. Compression plating versus intramedullary nailing of humeral shaft fractures–a meta-analysis. Acta Orthop. 2006;77(2):279–84. doi: 10.1080/17453670610046037. [DOI] [PubMed] [Google Scholar]
- 25.Hak DJ, Rose J, Stahel PF. Preoperative planning in orthopedic trauma: benefits and contemporary uses. Orthopedics. 2010;33(8):581–4. doi: 10.3928/01477447-20100625-21. [DOI] [PubMed] [Google Scholar]
- 26.Ebrahimzadeh MH, Kachooei AR, Soroush MR, Hasankhani EG, Razi S, Birjandinejad A. Long-term clinical outcomes of war-related hip disarticulation and transpelvic amputation. J Bone Joint Surg Am. 2013;95(16):e114(1-6). doi: 10.2106/JBJS.L.01160. [DOI] [PubMed] [Google Scholar]


