Abstract
Background: It is well established that low birth weight and accelerated postnatal growth increase the risk of liver dysfunction in later life. However, molecular mechanisms underlying such developmental programming are not well characterized, and potential intervention strategies are poorly defined.
Objectives: We tested the hypotheses that poor maternal nutrition and accelerated postnatal growth would lead to increased hepatic fibrosis (a pathological marker of liver dysfunction) and that postnatal supplementation with the antioxidant coenzyme Q10 (CoQ10) would prevent this programmed phenotype.
Design: A rat model of maternal protein restriction was used to generate low-birth-weight offspring that underwent accelerated postnatal growth (termed “recuperated”). These were compared with control rats. Offspring were weaned onto standard feed pellets with or without dietary CoQ10 (1 mg/kg body weight per day) supplementation. At 12 mo, hepatic fibrosis, indexes of inflammation, oxidative stress, and insulin signaling were measured by histology, Western blot, ELISA, and reverse transcriptase–polymerase chain reaction.
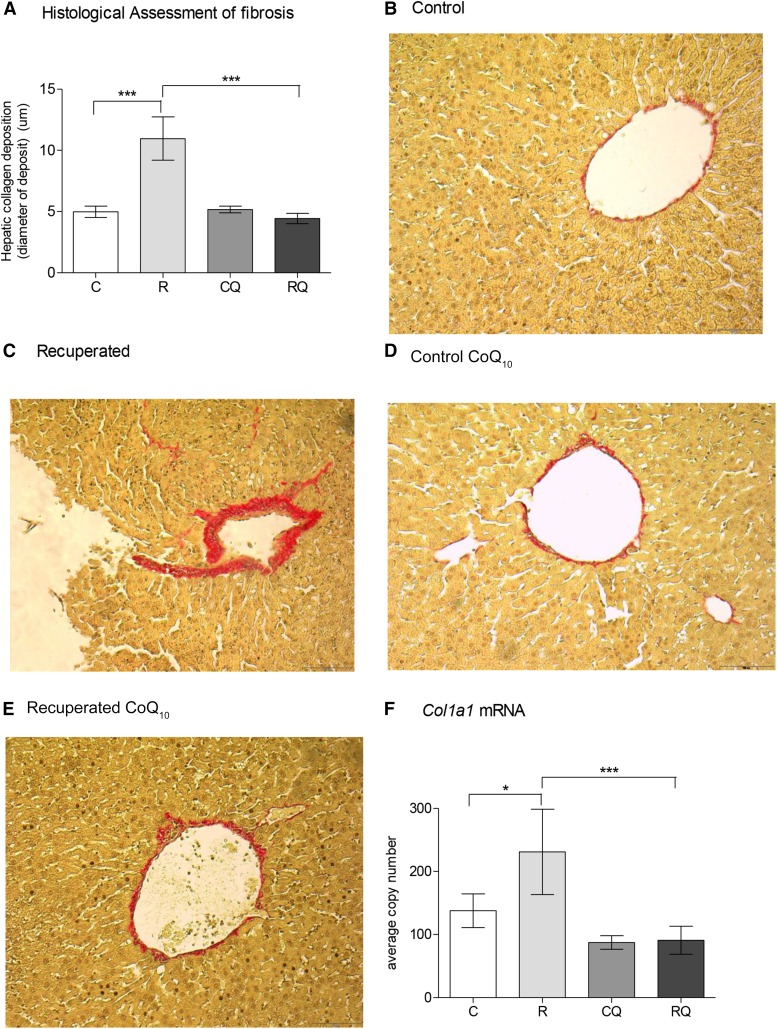
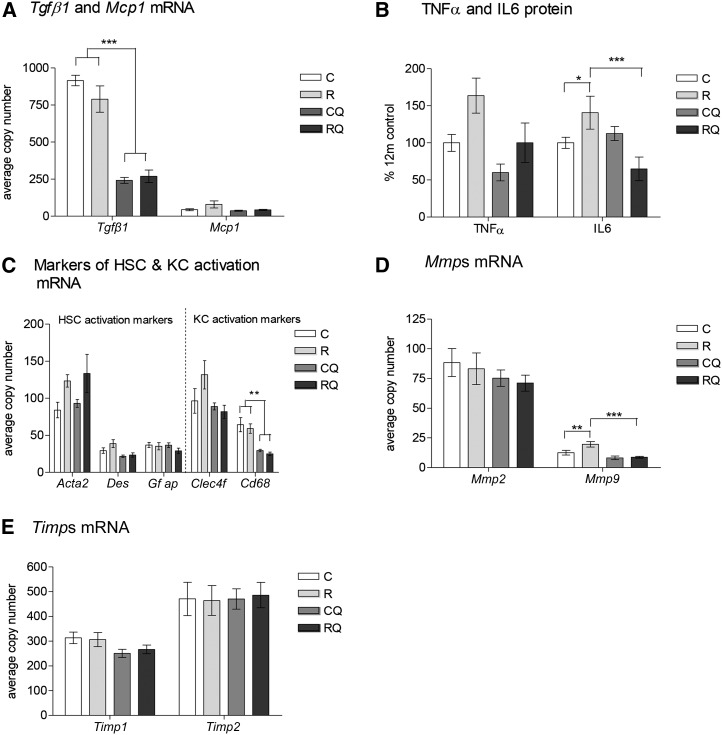
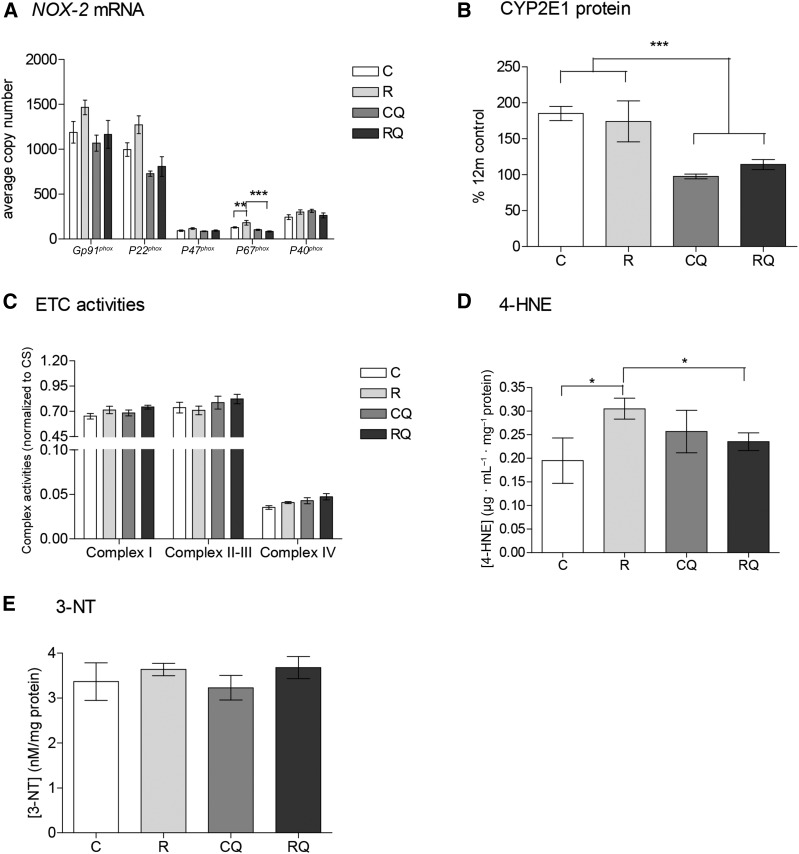
Results: Hepatic collagen deposition (diameter of deposit) was greater in recuperated offspring (mean ± SEM: 12 ± 2 μm) than in controls (5 ± 0.5 μm) (P < 0.001). This was associated with greater inflammation (interleukin 6: 38% ± 24% increase; P < 0.05; tumor necrosis factor α: 64% ± 24% increase; P < 0.05), lipid peroxidation (4-hydroxynonenal, measured by ELISA: 0.30 ± 0.02 compared with 0.19 ± 0.05 μg/mL per μg protein; P < 0.05), and hyperinsulinemia (P < 0.05). CoQ10 supplementation increased (P < 0.01) hepatic CoQ10 concentrations and ameliorated liver fibrosis (P < 0.001), inflammation (P < 0.001), some measures of oxidative stress (P < 0.001), and hyperinsulinemia (P < 0.01).
Conclusions: Suboptimal in utero nutrition combined with accelerated postnatal catch-up growth caused more hepatic fibrosis in adulthood, which was associated with higher indexes of oxidative stress and inflammation and hyperinsulinemia. CoQ10 supplementation prevented liver fibrosis accompanied by downregulation of oxidative stress, inflammation, and hyperinsulinemia.
Keywords: developmental programming, liver disease, coenzyme Q, low birth weight, accelerated postnatal growth
INTRODUCTION
In 1992, Hales and Barker (1) proposed the “thrifty phenotype hypothesis,” which postulated that in response to suboptimal in utero nutrition, the fetus alters its organ structure and adapts its metabolism to ensure immediate survival. This occurs through the sparing of vital organs (e.g., the brain) at the expense of others, such as the liver, thus increasing the risk of metabolic disease such as liver dysfunction in later life (2–4). This risk is exacerbated if a suboptimal uterine environment is followed by rapid postnatal growth (5, 6).
Nonalcoholic fatty liver disease (NAFLD)4 is the hepatic manifestation of the metabolic syndrome. Aspects of the metabolic syndrome, including NAFLD, have been linked to exposure to suboptimal early-life environments (7, 8). Although the incidence of NAFLD is high (9), the associated morbidity is low if there is no progression to hepatic fibrosis. Progression to fibrosis is indicative of the clinically important subtype of patients with NAFLD who have a high chance (20%) of developing frank liver cirrhosis and subsequent liver failure (10). At present, it is unknown why this progression occurs only in a subset of individuals. The development of an intervention that prevents these changes from accumulating could improve the prognosis of patients who develop NAFLD later in life.
Increased oxidative stress is a common consequence of developmental programming (11). Increased reactive oxygen species (ROS) have been strongly implicated in the etiology of hepatic fibrosis. Several animal studies have focused on antioxidant therapies to prevent the deleterious phenotypes of developmental programming (12–14); however, the doses used are not recommended for use in humans. In practice, a suboptimal intrauterine environment is often recognized retrospectively (i.e., after delivery). Thus, it is important to address potential beneficial effects of targeted postnatal interventions.
Coenzyme Q (CoQ10) is a benzoquinone ring linked to an isoprenoid side-chain. The isoform containing 9 isoprenoid units (CoQ9) is most abundant in rodents, whereas CoQ10 (10 isoprenoid units) is the most common in humans. When oxidized, CoQ10 shuttles electrons between mitochondrial complexes I and III and complexes II and III. Reduced CoQ10 is the most abundant endogenous cellular antioxidant (15) and is a safe and effective therapeutic antioxidant (16, 17). We have also shown that postnatal CoQ10 supplementation prevents developmentally programmed accelerated aging in rat aortas (18) and hearts (19).
Liver is one of a few tissues to take up dietary CoQ10 (20), and CoQ10 supplementation has been previously investigated as a potential therapy to prevent the progression of NAFLD in humans (21). In this study, we aimed to 1) investigate the effects of poor maternal nutrition and rapid postnatal catch-up growth on hepatic CoQ9 concentrations and molecular pathways leading to proinflammatory changes and development of fibrosis and 2) determine whether a clinically relevant dose of dietary CoQ10 could correct any observed hepatic fibrosis.
METHODS
Animal experimentation
All procedures involving animals were conducted under the British Animals (Scientific Procedures) Act (1986) and underwent ethical review by the University of Cambridge Animal Welfare and Ethical Review Board. Stock animals were purchased from Charles River, and dams were produced from in-house breeding from stock animals.
Pregnant Wistar rats were maintained at room temperature in specific-pathogen-free housing with the use of individually ventilated cages with environmental enrichment. The dams were maintained on a 20% protein diet (control) or an isocaloric low-protein (8%) diet, as previously described (22). Access to diets and water was provided ad libitum. All rats used in this study were specific-pathogen-free housed individually at 22°C on a controlled 12:12-h light-dark cycle. Diets were purchased from Arie Blok.
The day of birth was recorded as day 1 of postnatal life. Pups born to low-protein-diet–fed dams were cross-fostered to control-fed mothers on postnatal day 3 to create a recuperated litter. Each recuperated litter was standardized to 4 male pups at random to maximize their plane of nutrition. The control group consisted of the offspring of dams fed the 20%-protein diet and suckled by 20% protein–fed dams. Each control litter was culled to 8 pups as a standard. To minimize stress to the pups when cross-fostered, they were transferred with some of their own bedding. Body weights were recorded at postnatal days 3 and 21 and at 12 mo. At 21 d, 2 males per litter were weaned onto standard laboratory feed pellets (Special Diet Services) and the other 2 were weaned onto the same diet supplemented with CoQ10 to give a dose of 1 mg/kg body weight per day. Diets were given in the home cage. Rat pups were fed these diets until 12 mo of age, at which time all rats were killed by carbon dioxide asphyxiation at ∼1000. Post mortem, liver tissue was removed, weighed, and snap-frozen in liquid nitrogen and then stored at −80°C until analysis. A further portion of liver tissue (the same area for each sample) was removed and fixed in formalin for histologic assessment.
For all measurements, 1 pup per litter was used, thus “n” represents number of litters. Ten litters per group were used in this study based on power calculation with the use of previous data from our studies of RNA expression in postnatal tissues from programmed animals. Rat numbers were calculated to give 80% power to detect a 20% difference between groups at the P < 0.05 level. Only male rats were used in this study.
CoQ10 diet preparation
A dose of 1 mg CoQ10/kg body weight per day was used in this study, which was administered via the diet (18). This was achieved by appropriate CoQ10 supplementation of laboratory feed pellets, as we described previously (18, 19). Diet was prepared twice a week throughout the study.
CoQ10, lipid profile, glucose, and insulin analysis
Total liver ubiquinone (CoQ9 and CoQ10) was quantified by reverse-phase HPLC with UV detection at 275 nm, as described previously (18, 19). Serum was obtained as detailed previously (18), and blood from the tail vein collected into EDTA tubes and centrifuged for 3 min at 3000 rpm at 4° Celsius to isolate plasma. Fasted blood glucose measurements were obtained by using a glucose analyzer (Hemocue). The serum lipid profile and fasted plasma insulin analyses were performed by using an auto-analyzer (the Wellcome Trust–supported Cambridge Mouse Laboratory). Liver triglyceride concentrations were determined by using the Folch assay (23). Briefly, liver samples were homogenized in a 2:1 ratio of chloroform:methanol. The distinct lipid phase was removed after centrifugation, and lipid weight was quantified after the solvent was removed by evaporation.
Histologic assessment
Liver samples were fixed in formalin, paraffin-embedded, and sectioned to a 6-μm thickness by using a microtome. Picro Sirius Red staining was used to stain for fibrosis. Cell-D software (Olympus Soft Imaging Solutions) was used to quantify the thickness of fibrosis around all visible hepatic vessels (including all arteries and veins) from 1 section per sample. This sample was taken at the same point (20 sections for each sample) by using a nonbiased grid sampling method. All analyses were performed at 10× magnification by using an Olympus microscope (Olympus Soft Imaging Solutions). All analyses were performed blinded.
Mitochondrial electron transport chain complex activities
Activities of complex I [NAD(H): ubiquinone reductase; Enzyme Commission (EC) 1.6.5.3], complexes II–III (succinate: cytochrome c reductase; EC 1.3.5.1 + EC 1.10.2.2), and complex IV (cytochrome oxidase; EC 1.9.3.1) as well as citrate synthase (EC 1.1.1.27) were assayed as described previously (18, 19).
Protein analysis
Protein was extracted and assayed as described previously (18). Protein (20 μg) was loaded onto 10%, 12%, or 15% polyacrylamide gels, dependent on the molecular weight of the protein to be measured. The samples were electrophoresed and transferred to polyvinylidene fluoride membranes (18) and detected with the use of the following dilutions of primary antibody: insulin receptor substrate 1 (IRS-1; 1:1000; Millipore); phosphoinositide-3-kinase, p110-β (p110-β); insulin receptor β (IR-β); protein kinase-ζ (1:200; Santa-Cruz); Akt-1 and Akt-2 (1:1000; New England Biolabs); phosphoinositide-3-kinase, p85-α (p85-α 1:5000; Upstate); cytochrome P450-2E1 (CYP2E1) and Il-6 (1:1000; Abcam); Tnf-α (1:1000; Cell Signaling Technology); and anti-rabbit IgG secondary antibodies (1:20,000; Jackson Immunoresearch Laboratories). Equal protein loading was confirmed by staining electrophoresed gels with Coomassie Blue (Bio-Rad) to visualize total protein.
Gene expression
RNA was extracted by using a miReasy mini kit (Qiagen) following the manufacturer’s instructions, as detailed previously (19). A DNase digestion step was performed to ensure no genetic DNA contamination. RNA (1 μg) was used to synthesize complementary DNA by using oligo-dT-adaptor primers and Moloney murine leukemia virus reverse transcriptase (Promega). Gene expression was determined by using custom-designed primers (Sigma) and SYBR Green reagents (Applied Biosystems). Primer sequences are presented in Table 1. Quantification of gene expression was performed with the use of a Step One Plus reverse transcriptase–polymerase chain reaction machine (Applied Biosystems). Equal efficiency of the reverse transcription of RNA from all groups was confirmed through quantification of expression of the housekeeping gene β-actin (Actb). The expression of Actb did not differ between groups (effect of maternal diet, P = 0.9; effect of CoQ10 supplementation, P = 0.8; control: 153 ± 32; recuperated: 144 ± 24; control CoQ10: 143 ± 12; and recuperated CoQ10: 157 ± 21 average copy numbers).
TABLE 1.
Primers1
| Sequence |
|||
| Primer | F | R | Product size, bp |
| Col1a1 | GCCTCCCAGAACATCACCTA | GCAGGGACTTCTTGAGGTTG | 82 |
| Tgfb | TGCCCTCTACAACCAACACA | CTTGCGACCCACGTAGTAGA | 100 |
| Mcp1 | TGGACCAGAACCAAGTGAGA | TGCTGAAGTCCTTAGGGTTGA | 71 |
| Acta2 | GACATCAGGAAGGATCTCTATGC | TCTCCTTCTGCATCCTGTCA | 88 |
| Des | GGAGGAGATCCGACACCTAA | ACATCCAAGGCCATCTTCAC | 87 |
| Gfap | GAGTTACCAGGAGGCACTCG | GGGCCATCTCCTCCTTGAG | 65 |
| Clec4f | ACGGAGAGCGTGAAGACTGT | CTTGCACACCCAGTTGTAGG | 83 |
| Cd68 | AAAGCTTCTGTTGCGGAAAT | GAGCAGGTCCAGGTGAATTG | 62 |
| Mmp2 | GGAAAGAGGATACCCCAAGC | TCCAGTTAAAGGCAGCGTCT | 80 |
| Mmp9 | TTGGGTCTAGGCTCAGAGGT | AGATACGTTCCCGGCTGAT | 88 |
| Timp1 | CTGAGAAGGGCTACCAGAGC | TATTGCCAGGTGCACAAATC | 70 |
| Timp2 | GGATGGACTGGGTCACAGAG | GCGCAAGAACCATCACTTCT | 85 |
| Gp91phox | CGAAGCCTTGGCTAAAACTCT | TCCTTGTTGAAGATGAAGTGGA | 87 |
| P22phox | GTGAGCAGTGGACTCCCATT | GTAGGTGGCTGCTTGATGGT | 76 |
| P47phox | TGTGACACCCTCTCACAGACA | GTCGCATTTTCCCTCCTTTA | 96 |
| P67phox | CCGATAACCGGACAACAGAG | CAGGTCTTCTGGCTGGGTAG | 72 |
| P40phox | GATGTGGGACTCATGGTGAA | AATTGTCCTTCTGGGTGACG | 91 |
| Nrf2 | AGCAAGACTTGGGCCACTTA | GATGGAGGTTTCTGTCGTTTTC | 78 |
| Hmox1 | TAACCAGGATCTCCCCAAGA | TTAGAGTGCTGTGGCAGGTG | 73 |
| Gpx1 | CACCCGCTCTTTACCTTCCT | CGGGGACCAAATGATGTACT | 75 |
| Gst | TCTTGTTGGCAACCAACTCA | AGTCAGACAGCACAGGAGCA | 92 |
| Nqo1 | TGGAGACTGTCTGGGAGGAG | TCCTGCCTGGAAGTTTAGGT | 74 |
| Actb | ATGCTGCGTCTGGACTG | CTCCAGTGTGGTGAA | 85 |
Acta2, α-smooth muscle actin 2; Actb, β-actin; Cd68, cluster of differentiation 68; Clec4f, C-type lectin-domain family 4; Col1a1, collagen type 1, α1; Des, desmin; F, forward; Gfap, glial fibrillary acidic protein; Gpx1, glutathione peroxidase 1; Gst, glutathione synthetase; Hmox1, heme oxygenase 1; Mcp1, monocyte chemoattractant protein 1; Mmp, matrix metalloproteinase; Nqo1, NAD(P)H dehydrogenase, quinone 1; Nrf2, nuclear factor, erythroid 2–like 2; R, reverse; Tgfb, transforming growth factor β Timp, tissue inhibitor of matrix metalloproteinases.
Mitochondrial DNA copy number
Total DNA was extracted using a phenol/chloroform extraction protocol (24). Mitochondrial DNA copy number analysis was performed as described previously (25).
4-Hydroxynonenal and 3-nitrotyrosine analysis
Protein nitrotyrosination was assayed by using a Nitrotyrosine ELISA kit (MitoSciences), according to the manufacturer’s instructions. Lipid peroxidation was analyzed by using an OxiSelect HNE Adduct ELISA kit (Cambridge Biosciences), according to the manufacturer’s instructions.
Statistical analysis
Data were analyzed by using a 2-factor ANOVA with maternal diet and CoQ10 supplementation as the independent variables. Post hoc testing was carried out when appropriate and is indicated in the text accordingly. Data are represented as means ± SEMs. All statistical analyses were performed with the use of Statistica 7 software (Statsoft), and for all tests, P values <0.05 were considered significant. Data were checked for normal distribution. In all cases, “n” refers to the number of litters (with 1 rat used from each litter).
RESULTS
Anthropometric measurements
Recuperated offspring were born smaller than control rats (6.3 ± 0.2 compared with 7.4 ± 0.2 g; P < 0.001) and underwent rapid postnatal catch-up growth so that their weights were similar to those of the control offspring at postnatal day 21 (52.2 ± 0.9 compared with 50.7 ± 1.2 g). At 12 mo of age, there was no effect of maternal diet or CoQ10 supplementation on body weights or absolute liver weights (Table 2).
TABLE 2.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on rat pup body and liver weights1
| Control | Recuperated | Control CoQ10 | Recuperated CoQ10 | |
| Body weight at 12 mo, g | 956.3 ± 25.2 | 920.3 ± 28.8 | 979.6 ± 35.1 | 935.7 ± 29.9 |
| Absolute liver weight at 12 mo, g | 27.5 ± 1.4 | 28.4 ± 1.2 | 28.1 ± 1.2 | 29.5 ± 1.3 |
Values are means ± SEMs; n = 10/group. Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. No significant differences between groups were reported. CoQ10, coenzyme Q.
Dietary CoQ10 supplementation leads to greater hepatic CoQ9 and CoQ10 concentrations
Recuperated hepatic CoQ9 and CoQ10 concentrations were unaltered compared with those in control rats (Table 3). However, CoQ9 and CoQ10 concentrations were greater (P < 0.01) when supplemented with CoQ10 (Table 3).
TABLE 3.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on serum and plasma measurements1
| Control | Recuperated | Control CoQ10 | Recuperated CoQ10 | Effect of CoQ10 | |
| Hepatic CoQ9, pmol/mg protein | 494 ± 28 | 497 ± 24 | 872.4 ± 79** | 1071 ± 266** | 0.003 |
| Hepatic CoQ10, pmol/mg protein | 80 ± 7 | 78 ± 6 | 146 ± 17** | 102 ± 11** | 0.002 |
| Fasting plasma glucose, mmol/L | 5.6 ± 0.2 | 5.3 ± 0.1 | 5.4 ± 0.3 | 5.24 ± 0.2 | 0.9 |
| Serum cholesterol, mmol/L | 4.8 ± 0.5 | 4.9 ± 0.4 | 6.1 ± 0.7* | 5.9 ± 0.6* | 0.04 |
| Serum trigyclerides, mmol/L | 3.8 ± 0.05 | 3.8 ± 0.4 | 4.2 ± 0.6* | 5.7 ± 0.7* | 0.02 |
| Hepatic triglyceride content, g | 2.0 ± 0.2 | 2.3 ± 0.2 | 2.0 ± 0.1 | 2.0 ± 0.2 | 0.3 |
Values are means ± SEMs; n = 10/group. Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. The overall effects of maternal diet and interaction between maternal diet and CoQ10 supplementation were not significant for any of the variables reported in the table. *,**Effect of CoQ10: *P < 0.05, **P < 0.01. CoQ10, coenzyme Q.
CoQ10 supplementation ameliorates hepatic fibrosis and inflammation induced by poor maternal nutrition
Recuperated offspring showed greater (P < 0.001) collagen deposition (Figure 1A) than did control offspring (Figure 1B, C). CoQ10 supplementation prevented this effect of maternal diet (P < 0.001; interaction between maternal diet and CoQ10 supplementation, P = 0.001) (Figure 1A, D, E). Collagen type 1, α1 (Col1a1), mRNA expression was also greater (P < 0.05) in recuperated offspring (Figure 1F) and was reduced (P < 0.05) by CoQ10 supplementation (interaction between maternal diet and CoQ10 supplementation, P = 0.001) (Figure 1F).
FIGURE 1.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on hepatic fibrosis, quantified by measurement of collagen (A), in 12-mo-old male rat livers (B–E). (F) mRNA expression of Col1a1. Values are as means ± SEMs; n = 10/group; 10/10 rats used. *,***C compared with R and R compared with RQ: *P < 0.05, ***P < 0.001. Interaction between in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation (statistical interaction): P = 0.001 (A and F). Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. C, control; Col1a1 = collagen type 1, α1; CoQ10, coenzyme Q; CQ, control CoQ10; R, recuperated; RQ, recuperated CoQ10.
Recuperated and control offspring had similar expression of the profibrotic cytokine transforming growth factor β1 (Tgfb1), and a trend for greater expression of monocyte chemoattractant protein 1 (Mcp1; effect of maternal diet, P = 0.06) was observed in recuperated offspring (Figure 2A). CoQ10 supplementation reduced the concentrations of Tgfb1 (effect of CoQ10 supplementation, P < 0.001) and Mcp1 (effect of CoQ10 supplementation, P = 0.07) (Figure 2A). The cytokine Tnf-α was greater in recuperated offspring than in controls (effect of maternal diet, P < 0.05) and concentrations were reduced by CoQ10 supplementation (effect of CoQ10 supplementation, P < 0.05). Concentrations of Il-6 were greater (P < 0.05) in recuperated offspring than in controls and this effect was prevented by CoQ10 supplementation (P < 0.001; interaction between maternal diet and CoQ10 supplementation, P < 0.001) (Figure 2B). The gene expression of markers of hepatic stellate cell (HSC) and Kupffer cell (KC) activation [α-smooth muscle actin 2 (Acta2), desmin (Des), and C-type lectin-domain family 4 (Clec4f)] was greater in recuperated offspring than in controls (effects of maternal diet, P < 0.05 for all listed variables) (Figure 2C). CoQ10 supplementation reduced Des (P < 0.001), Clec4f (P < 0.05), and cluster of differientation 68 (Cd68) (P < 0.01; all were effects of CoQ10 supplementation) (Figure 2C). Acta2 was unchanged by CoQ10 supplementation (Figure 2C). Glial fibrillary acidic protein (Gfap) mRNA expression was not significantly different between groups (Figure 2C). Gene expression of matrix metalloproteinase (Mmp) 9 (Mmp9) was greater (P < 0.01) in recuperated offspring than in controls, and CoQ10 supplementation reduced (P < 0.001) recuperated Mmp9 mRNA to control levels (interaction between maternal diet and CoQ10 supplementation, P < 0.05) (Figure 2D). The gene expression of Mmp2 remained unaltered between groups (Figure 2D). Tissue inhibitors of Mmps (Timps) were also not significantly different between groups (Figure 2E).
FIGURE 2.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on inflammatory markers Tgfb1 and Mcp1 mRNA (A), Tnf-α and Il-6 protein (B), mRNA expression of markers of HSC activation (Acta2, Des, Gfap) and KC activation (Clec4f, Cd68) (C), and Mmp (D) and Timp (E) mRNA in 12-mo-old male rat livers. Values are means ± SEMs; n = 10/group; 10/10 rats used. **,***C and R compared with CQ and RQ: **P < 0.01, ***P < 0.001. *,**C compared with R: *P < 0.05, **P < 0.01. ***R compared with RQ, P < 0.001. Statistical interactions: Tgfb1, P = 0.1; Mcp1, P = 0.3; Tnf-α, P = 0.5; Il-6, P = 0.002; Acta2, P = 0.5; Des, P = 0.3; Gfap, P = 0.5; Clec4f, P = 0.1; Cd68, P = 0.9; Mmp2, P = 0.9; Mmp9, P = 0.04; Timp1, P = 0.6; Timp2, P = 0.8. Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. Acta2, α-smooth muscle actin 2; C, control; Cd68, cluster of differentiation 68; Clec4f, C-type lectin-domain family 4; Col1a1, collagen type 1, α1; CoQ10, coenzyme Q; CQ, control CoQ10; Des, desmin; Gfap, glial fibrillary acidic protein; Mcp1, monocyte chemoattractant protein 1; Mmp, matrix metalloproteinase; R, recuperated; RQ, recuperated CoQ10; Tgfb1, transforming growth factor β1; Timp, tissue inhibitor of matrix metalloproteinase.
CoQ10 supplementation attenuates ROS induced by poor maternal nutrition
Components of the NAD(P)H oxidase 2 (NOX-2) protein complex—Gp91phox (P < 0.05), P22phox (P < 0.05), and P47phox (P = 0.05)—were greater in recuperated offspring than in controls. P67phox was greater (P < 0.01) in recuperated offspring than in controls, and this effect was reduced (P < 0.001) by CoQ10 supplementation (interaction between maternal diet and CoQ10 supplementation, P < 0.01) (Figure 3A). Levels of Gp91phox (P = 0.08), P22phox (P < 0.001), and P47phox (P = 0.05) were reduced by CoQ10 supplementation (Figure 3A). CYP2E1 was not significantly different between control and recuperated offspring; however, CoQ10 supplementation reduced this concentration by 50% (effect of CoQ10 supplementation, P < 0.01) (Figure 3B). Complex I and complex IV electron transport chain activities were greater in recuperated offspring (effect of maternal diet, P = 0.05); however, complex II–III activity was unaffected. CoQ10 supplementation caused an increase in complex IV activity (effect of CoQ10 supplementation, P < 0.05) (Figure 3C). Mitochondrial DNA copy number was not significantly different between groups (control: 36 ± 4 copy numbers; recuperated: 36 ± 5 copy numbers) or by CoQ10 supplementation (control CoQ10: 41 ± 4 copy numbers; recuperated CoQ10: 35 ± 3 copy numbers). Concentrations of 4-hydroxynonenal (4-HNE) adducts were greater (P < 0.05) in recuperated offspring. There was a significant interaction between maternal diet and CoQ10 supplementation on 4-HNE concentrations (P < 0.05), reflecting the fact that CoQ10 supplementation reduced 4-HNE concentrations in recuperated offspring but had no effect in control offspring (Figure 3D). 3-nitrotyrosine concentrations were not significantly different between groups (Figure 3E).
FIGURE 3.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on indexes of oxidative stress: components of the NOX-2 complex (A), CYP2E1 (B), ETC activities (C), 4-HNE (D), and 3-NT adducts (E) in 12-mo-old male rat livers. Values are means ± SEMs; n = 10/group; 10/10 rats used. D: *Comparison of C with R and comparison of R with RQ, P < 0.05. A and B: **Comparison of C with R, P < 0.01; ***Comparison of R with RQ and comparison of C and R with CQ and RQ, P < 0.001. Statistical interactions: NOX-2 (Gp91phox, P = 0.5; P22phox, P = 0.3; P47phox, P = 0.4; P67phox, P = 0.01; P40phox, P = 0.3), CYP2E1 (P = 0.5), ETC activities (complex I, P = 0.9; complexes II–III, P = 0.6; complex IV, P = 0.9), 4-HNE (P = 0.04), and 3-NT (P = 0.8). Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. C, control; CoQ10, coenzyme Q; CQ, control CoQ10; CS, citrate synthase; CYP2E1, cytochrome P450-2E1; ETC, electron transport chain; NOX-2, NAD(P)H oxidase 2; R, recuperated; RQ, recuperated CoQ10; 3-NT, 3-nitrotyrosine; 4-HNE, 4-hydroxynonenal.
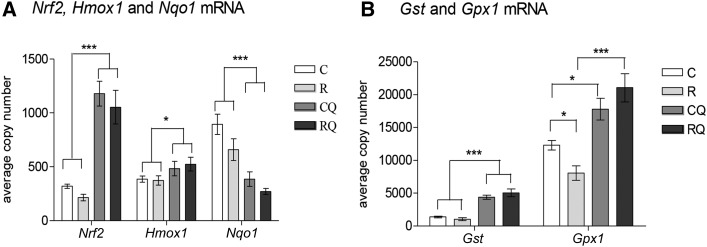
CoQ10 supplementation alters hepatic antioxidant defense capacity
Nuclear factor erythroid 2–like 2 (Nrf2), heme oxygenase 1 (Hmox1), and glutathione synthetase (Gst) expression were not significantly different between control and recuperated offspring (Figure 4A, B). Glutathione peroxidase 1 (Gpx1) was reduced in recuperated offspring compared with controls, and this effect was prevented by CoQ10 supplementation (interaction between maternal diet and CoQ10 supplementation, P < 0.05). NAD(P)H dehydrogenase, quinone 1 (Nqo1), was reduced in recuperated offspring (effect of maternal diet, P < 0.05) (Figure 4A, B). CoQ10 supplementation increased Nrf2 (P < 0.001), Hmox1 (P < 0.05), and Gst (P < 0.001) (Figure 4A, B); however Nqo1 expression was reduced by CoQ10 supplementation (effect of CoQ10 supplementation, P < 0.001) (Figure 4A).
FIGURE 4.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on mRNA expression of molecules involved in the NRF antioxidant defense pathway in 12-mo-old male rat livers. (A) Nrf2, Hmox1, and Nqo1 and (B) Gst and Gpx1. Values are means ± SEMs; n = 10/group; 10/10 rats used. *,***C and R compared with CQ and RQ: *P < 0.05, ***P < 0.001. *C compared with R and C compared with CQ, P < 0.05. ***R compared with RQ, P < 0.001. Statistical interactions: Nrf2, P = 0.9; Hmox1, P = 0.6; Nqo1, P = 0.4; Gst, P = 0.1; Gpx1, P = 0.01. Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. C, control; CoQ10, coenzyme Q; CQ, control CoQ10; Gpx1, glutathione peroxidase 1; Gst, glutathione synthetase; Hmox1, heme oxygenase 1; Nqo1, NAD(P)H dehydrogenase, quinone 1; NRF, nuclear erythroid 2-related factor; Nrf2, nuclear factor, erythroid 2–like 2; R, recuperated; RQ, recuperated CoQ10.
CoQ10 supplementation alters expression of molecules involved in insulin and lipid metabolism
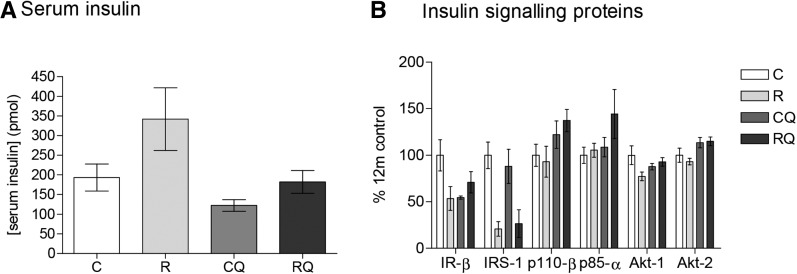
Greater serum insulin concentrations were observed in recuperated offspring than in controls (overall effect of maternal diet, P < 0.05) (Figure 5A). Concentrations were reduced by CoQ10 supplementation (effect of CoQ10 supplementation, P < 0.01) (Figure 5A). Protein expression of IR-β (P < 0.001), IRS-1 (P < 0.001), and Akt-1 (P < 0.05) was reduced in recuperated offspring compared with controls (all effects of maternal diet). Phosphoinositide-3-kinase-p110-β (p110-β), phosphoinositide-3-kinase-p85α (p85-α), and Akt-2 were not influenced by maternal diet (Figure 5B). CoQ10 supplementation increased p110-β (P < 0.05) and Akt-2 (P < 0.01) protein expression (Figure 5B). Fasting plasma glucose concentrations were not significantly different between groups (Table 3). Serum and hepatic triglyceride concentrations and serum cholesterol concentrations were not significantly different between control and recuperated offspring (Table 3). CoQ10 supplementation increased serum triglyceride and cholesterol concentrations (effects of CoQ10 supplementation, P < 0.05); however, hepatic triglyceride concentrations were unchanged (Table 3).
FIGURE 5.
Effect of in utero protein restriction, accelerated postnatal growth, and CoQ10 supplementation on serum insulin (A) and insulin signaling protein expression (B) in 12-mo-old male rat livers. Values are means ± SEMs; n = 10/group; 10/10 rats used. Statistical interactions: insulin, P = 0.3; insulin signaling proteins (IR-β, P = 0.12; IRS-1, P = 0.5; p110β, P = 0.4; p85α, P = 0.3; Akt-1, P = 0.05; Akt-2, P = 0.5). Data were analyzed by using 2-factor ANOVA and Duncan’s post hoc testing, where appropriate. C, control; CoQ10, coenzyme Q; CQ, control CoQ10; IR-β, insulin receptor β IRS-1, insulin receptor substrate 1; p85α, phosphoinositide-3-kinase, p85-α p110-β, phosphoinositide-3-kinase, p110-β R, recuperated; RQ, recuperated CoQ10.
DISCUSSION
Our findings that a maternal low-protein diet in utero followed by accelerated postnatal growth (recuperated) confers a higher risk of oxidative damage, proinflammatory changes, and liver fibrosis suggest that the early environment is an important determinant of an individual’s risk of developing complications of fatty liver disease. The potential for progression from NAFLD to nonalcoholic steatohepatitis and finally to hepatitis, fibrosis, and cirrhosis is well described. However, it has not previously been possible to identify patients who are at high risk of these changes. Our finding that recuperated rats developed more hepatic fibrosis than did controls indicates that the early environment plays a central role in the risk of liver disease in later life. Identifying the early environment as influential in the propensity to hepatic inflammation and fibrosis provides valuable new insight into predetermining individuals at increased risk from hepatic manifestations of the metabolic syndrome.
HSCs are the main source of extracellular matrix formation during hepatic fibrosis (26). The key step in inducing fibrosis during liver injury is the transformation of quiescent HSCs to activated HSCs, which differentiate into myofibroblasts (26). We found increased expression of Acta2 and Des in recuperated offspring. Acta2 is expressed in myofibroblasts of damaged liver (27) and hence is a good marker of HSC activation. In rats, HSC activation and proliferation correlate with a high expression of Des and are found in HSCs of acutely injured liver (27). KC infiltration and activation play a prominent role in HSC activation. Increased KC infiltration coincides with the activation of HSC markers such as Acta2 (28). Cle4f (a unique KC receptor for glycoproteins and therefore a good marker of KC activation) was increased in livers of recuperated offspring.
Increased concentrations of proinflammatory cytokines are also crucial in initiating HSC activation. Hepatic protein expression of Tnf-α and Il-6 was greater in recuperated offspring, suggesting that inflammation plays a role in the HSC activation and consequent hepatic fibrosis observed in our model. Tgfb1 mRNA levels were not changed in recuperated offspring; however, we cannot discount the possibility that Tgfb1 is upregulated at the protein level. Mcp1 (a chemokine that acts as a chemoattractant for HSCs) was also upregulated in recuperated livers. Mmps are also associated with hepatic fibrosis (29). Mmp9 expression was upregulated in recuperated livers. Mmp9 is prominent in scar areas of active fibrosis, and treatment with a profibrotic agent can increase its expression, with peak expression coinciding with induction of inflammatory cytokines (29). Mmp2 expression was unaltered between groups. Because Mmp expression is an early event in wound healing, the time window for Mmp2 elevation may have been missed and that difference would be observed only in younger animals.
A further driving factor in HSC activation and fibrosis is increased ROS, which can be generated by Tnf-α, Il-6 (30), KCs (28), and the mitochondrial electron transport chain. We found increased ROS in the context of increased lipid peroxidation [which is known to increase in liver disease (31)] and greater expression of the NOX-2 components (Gp91phox, P22phox, P47phox, and P67phox), a major source of hepatic ROS production, which have been observed in hepatic fibrosis (32, 33). Complex I activity, a predominant generator of ROS (34), was greater in recuperated livers. Decreased antioxidant defense capacity was evidenced by a reduction in Gpx1, a peroxidase responsible for the conversion of H2O2 into H2O and O2. Increased concentrations of cellular H2O2, due to Gpx1 depletion, could cause accumulation of the hydroxyl anion, a free radical that can directly increase lipid peroxidation.
Accumulation of hepatic triglycerides also plays a role in hepatic fibrosis (35); however, neither liver nor plasma triglycerides were altered in recuperated rats. This may be explained by the fact that recuperated offspring are fed a feed pellet diet and do not display an obesogenic phenotype. This in itself is interesting, because it shows that the observed deleterious liver phenotypes develop in a physiologic environment that had been influenced only by developmental programming per se, and not by obesity.
Insulin resistance and hyperinsulinemia are also major contributors to liver fibrosis (36) and are inherently linked to increased oxidative stress. Recuperated offspring had whole-body insulin resistance as indicated by hyperinsulinemia. The hyperinsulinemia was associated with hepatic insulin signaling protein dysregulation, as shown by the downregulation of IR-β, IRS-1, and Akt-1.
Importantly, we identified an effective means of arresting the pathologic progression of NAFLD, by postnatal supplementation with CoQ10. In recuperated offspring, CoQ10 supplementation reduced markers of HSC and KC activation, the accumulation of ROS, and the deposition of collagen around the hepatic vessels. This agrees with a study in which high-fat diet fed mice administered 1% CoQ10 supplementation led to reduced hepatic NOX expression (37). CoQ10 supplementation also increased activity of complex IV, in keeping with in vitro studies (38). CoQ10 supplementation decreased Tnf-α, Il-6, Tgfb1, and Mcp1, suggesting that CoQ10 also can reduce inflammatory changes in liver, which is consistent with studies in mouse liver (37) and human blood (39). Our data therefore recapitulate CoQ10’s function, both as a potent antioxidant (15) and as an anti-inflammatory agent.
CoQ10 supplementation also prevented hyperinsulinemia in recuperated rats; however, hepatic insulin signaling protein dysregulation was not normalized by CoQ10 supplementation. The whole-body insulin sensitivity may therefore be improved through other mechanisms such as improvements in muscle and/or adipose tissue insulin sensitivity. CoQ10 may exert antifibrotic effects through the activation of the Nrf2/antioxidant response element (Nrf2/ARE) pathway. Nrf2 is a transcription factor that responds to oxidative status and regulates transcription of genes involved in antioxidant defense. CoQ10 treatment in a model of hepatic fibrosis ameliorates liver damage via suppression of Tgfb1 and upregulation of Nrf-ARE-associated genes (40). Although Nrf2 expression was not affected by maternal diet, CoQ10 supplementation increased Nrf2 by 4-fold. The antioxidant genes involved in the Nrf2/ARE pathway—Hmox1, Gst, and Gpx1—were increased by CoQ10 supplementation. This suggests that CoQ10 supplementation upregulates the Nrf2/ARE pathway via suppression of Tgfb1 (40). These observations support a role for CoQ10 supplementation in increasing antioxidant defenses to a protective level in animals that have experienced detrimental catch-up growth (18, 19). Because Nqo1 activity is known to prevent 1 electron reduction in quinones, it is plausible that because hepatic CoQ10 concentrations are elevated by CoQ10 supplementation, Nqo1 expression is not required and thus suppressed.
In conclusion, a suboptimal early-life environment combined with a mismatched postnatal milieu predisposes offspring to increased hepatic ROS, inflammation, and hyperinsulinemia, leading to hepatic fibrosis. This recapitulates changes seen in patients in whom benign NAFLD progresses to cirrhosis and ultimately liver failure. We suggest that the early environment life is crucial in identifying the subgroup of patients at highest risk of such progression; however, this should be tested in humans. A clinically relevant dose of CoQ10 reversed liver fibrosis via downregulation of ROS, inflammation, and hyperinsulinemia and upregulation of the Nrf2/ARE antioxidant pathway. Because fibrosis contributes to up to 45% of deaths in the industrial world (41), CoQ10 supplementation may be a cost-effective and safe way of reducing this global burden in at-risk individuals, before the development of an NAFLD phenotype.
Acknowledgments
We thank K Phillips for technical expertise.
The authors’ responsibilities were as follows—JLT-A: conducted research, analyzed data; DSF-T: provided essential materials; IPH and VN: conducted research; CEA: wrote the manuscript; MSM-G: provided essential materials; JMM: designed the research; SEO: designed the research; JLT-A and SEO wrote the manuscript and had primary responsibility for final content; and all authors: read and approved the final manuscript. None of the authors declared a conflict of interest.
Footnotes
Abbreviations used: Acta2, α-smooth muscle actin 2; Actb, β-actin; ARE, antioxidant response element; Cd68, cluster of differentiation 68; Clec4f, C-type lectin-domain family 4; Col1a1, collagen type 1, α1; CoQ9, coenzyme Q isoform containing 9 isoprenoid units; CoQ10, coenzyme Q; CYP2E1, cytochrome P450-2E1; Des, desmin; EC, Enzyme Commission; Gfap, glial fibrillary acidic protein; Gpx1, glutathione peroxidase 1; Gst, glutathione synthetase; Hmox1, heme oxygenase 1; HSC, hepatic stellate cell; IR-β, insulin receptor β IRS-1, insulin receptor substrate 1; KC, Kupffer cell; Mcp1, monocyte chemoattractant protein 1; Mmp, matrix metalloproteinase; NAFLD, nonalcoholic fatty liver disease; NOX-2, NAD(P)H oxidase 2; Nqo1, NAD(P)H dehydrogenase, quinone 1; Nrf2, nuclear factor, erythroid 2–like 2; p85-α, phosphoinositide-3-kinase, p85-α p110-β, phosphoinositide-3-kinase, p110-β ROS, reactive oxygen species; Tgfb1, transforming growth factor β1; Timp, tissue inhibitor of matrix metalloproteinases; 4-HNE, 4-hydroxynonenal.
REFERENCES
- 1.Hales CN, Barker DJ. The thrifty phenotype hypothesis. Br Med Bull 2001;60:5–20. [DOI] [PubMed] [Google Scholar]
- 2.Tarry-Adkins JL, Ozanne SE. Mechanisms of early life programming: current knowledge and future directions. Am J Clin Nutr 2011;94(6 Suppl):1765S–71S. [DOI] [PubMed] [Google Scholar]
- 3.Zhou D, Pan XY. Pathophysiological basis for compromised health beyond generations: role of maternal high-fat diet and low-grade chronic inflammation. J Nutr Biochem 2015;26:1–8. [DOI] [PubMed] [Google Scholar]
- 4.Moraes C, Rebelato HJ, Amaral MEC, Resende TM, Silva EVC, Esquisatto MAM, Catisti R. Effect of maternal protein restriction on liver metabolism in rat offspring. J Physiol Sci 2014;64:347–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Breij LM, Kerkhof GF, Hokken-Koelenga AC. Accelerated infant weight gain and risk for non-alcoholic liver disease in early adulthood. J Clin Endocrinol Metab 2014;99:1189–95. [DOI] [PubMed] [Google Scholar]
- 6.Faienza MF, Brunetti G, Ventura A, D’Anniello M, Pepe T, Giordano P, Monteduro M, Cavallo L. Nonalcoholic fatty liver disease in prepubertal children born small for gestational age: influence of rapid weight catch-up growth. Horm Res Paediatr 2013;79:103–9. [DOI] [PubMed] [Google Scholar]
- 7.Carr SK, Chen JH, Cooper WN, Constancia M, Yeo GSH, Ozanne SE. Maternal diet amplifies hepatic aging trajectory of Cidae in male mice and leads to the development of fatty liver. FASEB J 2014;28:2191–201. [DOI] [PubMed] [Google Scholar]
- 8.Nobili V, Alisi A, Panare N, Agostoni C. Low birth weight and catch-up growth associated with metabolic syndrome: a ten year systemic review. Pediatr Endocrinol Rev 2008;6:241–7. [PubMed] [Google Scholar]
- 9.Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt Harrison SA. Prevalence of nonalcoholic fatty liver disease and non-alcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 2011;140:124–31. [DOI] [PubMed] [Google Scholar]
- 10.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Lui YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 1999;116:1413–9. [DOI] [PubMed] [Google Scholar]
- 11.Tarry-Adkins JL, Ozanne SE. The impact of early nutrition on the ageing trajectory. Proc Nutr Soc 2014;73:289–301. [DOI] [PubMed] [Google Scholar]
- 12.Sen S, Simmons RA. Maternal antioxidant supplementation prevents adiposity in Western diet fed rats. Diabetes 2010;59:3058–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giussani DA, Camm EJ, Nui Y, Richter HG, Blanco CE, Gottschalk R, Blake EZ, Horder KA, Thakor AS, Hansell JA, et al. Developmental programming of cardiovascular dysfunction by prenatal hypoxia and oxidative stress. PLoS One 2012;7:e31017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cambonie G, Comte B, Yzdorczyk C, Ntimbane T, Germaine N, Le NL, Pladys P, Gauthier C, Lahaie I, Abran D, et al. Antenatal oxidant prevents adult hypertension, vascular dysfunction, and microvascular rarefaction associated with in utero exposure to a low-protein diet. Am J Physiol Regul Integr Comp Physiol 2007;292:R1236–45. [DOI] [PubMed] [Google Scholar]
- 15.Turunen M, Olssen J, Dallner JG. Metabolism and function of coenzyme Q. Biochim Biophys Acta 2004;1660:171–99. [DOI] [PubMed] [Google Scholar]
- 16.Hidaka T, Fuji K, Funahashi I, Fukutomi N, Hoseo K. Safety assessment of coenzyme Q10 (CoQ10). Biofactors 2008;32:199–208. [DOI] [PubMed] [Google Scholar]
- 17.Ikematsu H, Nakamura K, Harashima S, Fujii K, Fukutomi N. Safety assessment of coenzyme Q10 (Kaneka Q10) in healthy subjects: a double-blind, randomized placebo-controlled trial. Regul Toxicol Pharmacol 2006;44:212–8. [DOI] [PubMed] [Google Scholar]
- 18.Tarry-Adkins JL, Fernandez-Twinn DS, Chen JH, Hargreaves IP, Martin-Gronert MS, McConnell JC, Ozanne SE. Nutritional programming of coenzyme Q: potential for prevention and intervention? FASEB J 2014;28:5398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tarry-Adkins JL, Blackmore HL, Martin-Gronert MS, Fernandex-Twinn DS, McConnell JM, Hargreaves IP, Giussani DA, Ozanne SE. Coenzyme Q prevents accelerated cardiac aging in a rat model of poor maternal nutrition and accelerated postnatal growth. Mol Metab 2013;2:480–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lönnrot K, Holm P, Lagerstedt A, Huhtala H, Alho H. The effects of lifelong ubiquinone supplementation on the Q9 and Q10 tissue concentrations and life span of male rats and mice. Biochem Mol Biol Int 1998;44:727–37. [DOI] [PubMed] [Google Scholar]
- 21.Farhangi MA, Alipour B, Jafarvand E, Khoshbaten M. Oral coenzyme q10 supplementation in patients with nonalcoholic liver disease: effects on serum vaspin, chemerin, pentraxin 3, insulin resistance and oxidative stress. Arch Med Res 2014;45:589–95. [DOI] [PubMed] [Google Scholar]
- 22.Snoeck A, Remacle C, Reusens B, Hoett JJ. Effect of low protein diet during pregnancy on the fetal rat endocrine pancreas. Biol Neonate 1990;57:107–18. [DOI] [PubMed] [Google Scholar]
- 23.Folch J, Lees M, Sloane Stanley GH. A simple method for the isolation and purification of total lipides from animal tissues. Long Island (NY): J Biol Chem 1957;226:497–509. [PubMed] [Google Scholar]
- 24.Green MR, Sambrook J. Molecular cloning: a laboratory manual. 4th ed. C; old Spring Harbor Laboratory Press; 1989. [Google Scholar]
- 25.Aiken CE, Tarry-Adkins JL, Ozanne SE. Suboptimal nutrition in-utero gives rise to DNA damage and accelerated aging of the female reproductive tract. FASEB J 2013;27:3959–65. [DOI] [PubMed] [Google Scholar]
- 26.Geerts A. History, heterogeneity, developmental biology and functions of quiescent hepatic stellate cells. Semin Liver Dis 2001;21:311–35. [DOI] [PubMed] [Google Scholar]
- 27.Ballardini G, Fallini M, Biagini G, Bianchi FB, Pisi E. Desmin and actin in the identification of Ito cells and in monitoring their evolution to myofibroblasts in experimental fibrosis. Virchows Arch B Cell Pathol Incl Mol Pathol 1988;56:45–9. [DOI] [PubMed] [Google Scholar]
- 28.Li JT, Liao ZX, Ping J, Xu D, Wang HJ. Molecular mechanisms of hepatic stellate cell activation and anti-fibrotic therapeutic strategies. J Gastroenterol 2008;43:419–28. [DOI] [PubMed] [Google Scholar]
- 29.Han YP. Matrix metalloproteinases, the pros and cons, in liver fibrosis. J Gastroenterol Hepatol 2006;21:S88–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woo CH, Eom YW, Yoo MH, You HJ, Han HJ, Song WK, Yoo YJ, Chun JS, Kin JH. Tumor necrosis factor-alpha generates reactive oxygen species via a cytosolic phospholipase A2-linked cascade. J Biol Chem 2000;275:32357–62. [DOI] [PubMed] [Google Scholar]
- 31.George J, Pera N, Phung N, Leclerqc I, Yun-Hou J, Farrell G. Lipid peroxidation, stellate cell activation and hepatic fibrogenesis in a rat model of chronic steatohepatitis. J Hepatol 2003;39:756–64. [DOI] [PubMed] [Google Scholar]
- 32.Paik YH, Iwaisako K, Seki E, Inokuchi S, Schnabl B, Osterreicher CH, Kisseleva T, Brenner DA. The nicotinamide adenine dinucleotide phosphate oxidase (NOX) homologues NOX1 and NOX2/gp91(phox) mediate hepatic fibrosis in mice. Hepatology 2011;53:1730–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jiang JX, Venugopal S, Serizawa N, Chen X, Scott F, Li Y, Adamson R, Devaraj S, Shah V, Gershwin ME, et al. Reduced nicotinamide adenine dinucleotide phosphate oxidase 2 plays a key role in stellate cell activation and liver fibrogenesis in vivo. Gastroenterology 2010;139:1375–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu Y, Fiskum G, Schubert D. Generation of reactive oxygen species by the mitochondrial electron transport chain. J Neurochem 2002;80:780–7. [DOI] [PubMed] [Google Scholar]
- 35.Berlanga A, Guiu-Jurado E, Porras JA, Auquet T. Molecular pathways in non-alcoholic liver disease. Clin Exp Gastroenterol 2014;7:221–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.García-Monzón C,Lo lacona O, Mayoral R, Gonzalez-Rodriguez A, Miguilena-Colina ME, Lozano-Rodriguez T, Garcia-Pozo L, Vargas-Castrillon J, Casado M, Bosca L, et al. Hepatic insulin resistance is associated with increased apoptosis and fibrogenesis in nonalcoholic steatohepatitis and chronic hepatitis C. J Hepatol 2011;54:142–52. [DOI] [PubMed] [Google Scholar]
- 37.Sohet FM, Neyrinck AM, Pachikian BD, de Backer FC, Bindels LB, Niklowitz P, Menke T, Cani PD, Delzenne NM. Coenzyme Q10 supplementation lowers hepatic oxidative stress and inflammation associated with diet-induced obesity in mice. Biochem Pharmacol 2009;78:1391–400. [DOI] [PubMed] [Google Scholar]
- 38.Duberley KE, Heales SRJ, Abramov AY, Chalasani A, Land JM, Rahman S, Hargreaves IP. Effect of CoQ10 supplementation on mitochondrial electron transport chain activity and mitochondrial oxidative stress in CoenzymeQ10 deficient human neuronal cells. Int J Biochem Cell Biol 2014;50:60–3. [DOI] [PubMed] [Google Scholar]
- 39.Sanoobar M, Eghtesadi S, Azimi A, Khalili M, Khodadi B, Jazayeri S, Gohari MR, Aryaeian N. Coenzyme Q10 supplementation ameliorates inflammatory markers in patients with multiple sclerosis: a double blind, placebo, controlled randomised clinical trial. Nutr Neurosci 2015;18:169–76. [DOI] [PubMed] [Google Scholar]
- 40.Choi HK, Pokharel YR, Lim SC, Han HK, Ryu CS, Kim SK, Kwak MK, Kang KW. Inhibition of liver fibrosis by solubilized coenzyme Q10: Role of NRF2 activation in inhibiting transforming growth factor-beta-1 expression. Toxicol Appl Pharmacol 2009;240:377–84. [DOI] [PubMed] [Google Scholar]
- 41.Friedman SL, Sheppard D, Duffield JS, Violette S. Therapy for fibrotic diseases: nearing the starting line. Sci Transl Med 2013;5:167sr1. [DOI] [PubMed] [Google Scholar]