Abstract
Background: The DASH (Dietary Approaches to Stop Hypertension) dietary pattern, which is high in fruit, vegetables, and low-fat dairy foods, significantly lowers blood pressure as well as low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
Objective: The study was designed to test the effects of substituting full-fat for low-fat dairy foods in the DASH diet, with a corresponding increase in fat and a reduction in sugar intake, on blood pressure and plasma lipids and lipoproteins.
Design: This was a 3-period randomized crossover trial in free-living healthy individuals who consumed in random order a control diet, a standard DASH diet, and a higher-fat, lower-carbohydrate modification of the DASH diet (HF-DASH diet) for 3 wk each, separated by 2-wk washout periods. Laboratory measurements, which included lipoprotein particle concentrations determined by ion mobility, were made at the end of each experimental diet.
Results: Thirty-six participants completed all 3 dietary periods. Blood pressure was reduced similarly with the DASH and HF-DASH diets compared with the control diet. The HF-DASH diet significantly reduced triglycerides and large and medium very-low-density lipoprotein (VLDL) particle concentrations and increased LDL peak particle diameter compared with the DASH diet. The DASH diet, but not the HF-DASH diet, significantly reduced LDL cholesterol, HDL cholesterol, apolipoprotein A-I, intermediate-density lipoprotein and large LDL particles, and LDL peak diameter compared with the control diet.
Conclusions: The HF-DASH diet lowered blood pressure to the same extent as the DASH diet but also reduced plasma triglyceride and VLDL concentrations without significantly increasing LDL cholesterol. This trial was registered at clinicaltrials.gov as NCT01404897.
Keywords: DASH diet, lipoproteins, saturated fat, triglyceride, blood pressure, dairy
INTRODUCTION
The Dietary Approaches to Stop Hypertension (DASH)6 dietary eating pattern, which emphasizes fruit and vegetables, low-fat dairy foods, and whole grains (1, 2), is one of the most widely prescribed dietary modifications for reducing blood pressure (BP) and cardiovascular disease risk. Notably, in the Nurses’ Health Study, self-reported greater adherence to a DASH-style diet was associated with a lower risk of coronary artery disease and stroke (3). Because LDL cholesterol is lower with the consumption of the DASH diet than with a typical Western diet due in part to its limitation of saturated fatty acids, it is believed that its lower saturated fat content may contribute to reduced risk of cardiovascular disease (4, 5).
The degree of dietary adherence strongly determines the efficacy of dietary interventions (6). A recent review of 9 trials of the DASH diet with objective measures of compliance reported poorer adherence when dietary advice rather than foods was provided (7). A common reason for low adherence or high attrition is the difficulty of following prescribed diets (8). In the original DASH trial, lack of menu variety was a primary reason for lapses in dietary adherence (9). This suggests the potential value of providing options for the DASH diet that permit variation in macronutrient composition while preserving benefits on BP and lipid risk factors.
One such variation is the substitution of fat for carbohydrate. Appel et al. (10) reported that the replacement of 10% of energy from carbohydrate with unsaturated fat (primarily monounsaturated) in a DASH-like diet resulted in a reduction in triglycerides and an increase in HDL cholesterol, with no change in LDL cholesterol, and a further reduction in the Framingham risk score. There is evidence that long-term compliance to diets with reduced saturated fat is poor (11), even with intensive counseling, and that moderate-fat diets may yield better dietary adherence than low-fat diets (12). Furthermore, the mean intake of individuals who consumed the DASH diet in the ENCORE (Exercise and Nutrition Interventions for Cardiovascular Health) study failed to meet the low total fat and saturated fat targets (13).
The effects on lipids and BP of replacing carbohydrates with saturated fats within a DASH-like diet have not been reported, to our knowledge. In the present study we tested the effects of substituting full-fat dairy products for nonfat and low-fat dairy foods (thereby increasing saturated fat from 8% to 14% of energy) in conjunction with a reduction of 12% of energy in carbohydrate, primarily from sugars.
METHODS
Study design and diets
A 3-period randomized crossover study in free-living participants was conducted between August 2011 and December 2013 at our clinical research center in Berkeley, California. The participants consumed a 1-wk run-in diet, consisting of a mixture of 2 or 3 d of each experimental diet, and then consumed in random order a control diet, a standard DASH diet, and a higher-fat, lower-carbohydrate modification of the DASH diet (HF-DASH diet) for 3 wk each. Each experimental diet was separated by a 2-wk washout period, during which participants ate their own foods but continued to abstain from alcohol. Participants were assigned their diet sequence in randomly determined blocks of 3, 6, 9, or 12 individuals by using a uniform random-number generator. Diet sequences were kept in sealed envelopes and assigned to the participant by the study nutritionist 1–2 d before starting the first experimental diet. Participants were blinded to diet order, but because of the nature of the diets they were likely able to identify each diet. Clinic personnel were not blinded to diet order. Laboratory personnel and investigators were blinded to diet order, and unblinding was performed after data collection before analysis. Participants met with study staff weekly for counseling, to receive study foods, and to be weighed. At the end of each experimental diet, participants visited the clinic on 2 consecutive days for clinical and laboratory measurements. In addition, a fasting blood sample was taken after each washout period to document a return to baseline for standard lipid and BP measurements.
Study population
Participants included generally healthy men and women >21 y of age with an average diastolic BP between 80 and 95 mm Hg and systolic BP <160 mm Hg for 2 screening visits. Exclusion criteria included the following: use of nicotine products or recreational drugs; history of coronary artery disease, diabetes, or other chronic disease; use of hormones or medications known to affect lipid metabolism or BP; use of dietary supplements within the past 3 mo; unwillingness to refrain from alcoholic beverages during the study; BMI (in kg/m2) ≥35; total and LDL cholesterol >95th percentile for sex and age; fasting triglycerides >500 mg/dL; fasting glucose ≥126 mg/dL; and abnormal thyroid-stimulating hormone concentration. Participants were recruited primarily through our database of previous study participants, Internet advertisements, and community health events. The protocol was reviewed and approved by the Institutional Review Board of Children’s Hospital and Research Center Oakland. All participants provided written informed consent. Their characteristics at screening are shown in Table 1.
TABLE 1.
Participant characteristics at screening1
| Women (n = 15) | Men (n = 21 ) | P | |
| Age, y | 50 ± 12 | 45 ± 14 | 0.28 |
| BMI, kg/m2 | 26.8 ± 3.8 | 28.2 ± 3.5 | 0.26 |
| Body fat, % | 35.5 ± 6.3 | 26.2 ± 7.7 | 0.0003 |
| Waist circumference, cm | 92 ± 10 | 99 ± 11 | 0.04 |
| Systolic blood pressure, mm Hg | 136 ± 13 | 133 ± 10 | 0.51 |
| Diastolic blood pressure, mm Hg | 85 ± 5 | 84 ± 4 | 0.37 |
| Triglycerides, mmol/L | 1.08 ± 0.47 | 1.32 ± 0.86 | 0.30 |
| Cholesterol, mmol/L | |||
| Total | 5.13 ± 0.91 | 4.30 ± 0.80 | 0.008 |
| LDL | 2.90 ± 0.67 | 2.46 ± 0.60 | 0.05 |
| HDL | 1.74 ± 0.34 | 1.17 ± 0.31 | <0.0001 |
| Glucose, mmol/L | 5.44 ± 0.39 | 5.44 ± 0.44 | 0.89 |
Values are means ± SDs. P values were determined by unpaired t test.
Dietary provision
The Bionutrition Core of the University of California, San Francisco, Clinical and Translational Science Institute developed and prepared diets for a 3-d cycle menu at 5 levels of energy intake (1800, 2100, 2600, 3100, and 3600 kcal). Participants whose energy needs were between main-menu calorie levels received unit foods (100 kcal) that matched the macronutrient and mineral content of the experimental diets. The control and DASH diets were designed to match the characteristics of the diets used in the original DASH trial (1, 14–16). The higher-fat and lower-carbohydrate content of the HF-DASH diet was achieved by replacing nonfat and low-fat dairy with full-fat dairy products, mostly in the form of whole milk, cheese, and yogurt, and by reducing sugars, mostly from fruit juices, which constituted 59% of total fruit intake in the DASH diet (14). The DASH and HF-DASH patterns were otherwise developed by using similar recipes and foods, provided in different amounts to meet each diet specification. As in the original trial design, emphasis was placed on an abundance of fruit and vegetables; increased whole grains and dairy products; limited servings of meat, poultry, and fish; and inclusion of nuts, seeds, and legumes several times weekly (Table 2). The nutrient composition of the diets was initially assessed by using Nutrition Data System for Research Software (NDSR 2010; Nutrition Coordinating Center, University of Minnesota) and validated by compositional analysis of the 3-d cycle menus (Covance Laboratories) (Table 2). The sodium, potassium, magnesium, calcium, and fiber contents of the DASH and HF-DASH patterns were similar; the diets differed only in the amount of total fat, saturated fat, cholesterol, and carbohydrate they provided (Table 2). A sample 1-d menu is shown in Supplemental Table 1.
TABLE 2.
Diet composition1
| Control | DASH | HF-DASH | |
| Carbohydrate, % of energy | 47 | 55 | 43 |
| Protein, % of energy | 14 | 17 | 18 |
| Fat, % of energy | 38 | 27 | 40 |
| SFAs | 16 | 8 | 14 |
| MUFAs | 14 | 12 | 18 |
| PUFAs | 8 | 7 | 8 |
| Cholesterol, mg | 253 | 160 | 221 |
| Sodium, mg | 3052 | 2752 | 2720 |
| Potassium, mg | 1906 | 4575 | 4631 |
| Magnesium, mg | 193 | 469 | 465 |
| Calcium, mg | 429 | 1278 | 1324 |
| Fiber, g | 19 | 48 | 42 |
| Total sugar,2 g | 141 | 158 | 93 |
| Food groups3 | |||
| Grains,4 servings/d | 5.8 | 5.0 | 5.2 |
| Fruit and juices, cups/d | 0.9 | 3.3 | 1.4 |
| Vegetables, cups/d | 1.9 | 3.7 | 5.0 |
| Beef, oz/d | 2.3 | 1.6 | 1.9 |
| Poultry, oz/d | 3.5 | 2.0 | 2.1 |
| Fish, oz/d | 0.7 | 0.9 | 0.7 |
| Nuts and legumes, oz/d | 0 | 1.9 | 2.4 |
| Low-fat dairy, cups/d | 0 | 2.6 | 0 |
| Full-fat dairy, cups/d | 0.7 | 0 | 2.5 |
| Sugar from sweets and sugar-sweetened drinks, tsp/d | 20.4 | 2.4 | 0.4 |
| Fats, tsp/d | 10.1 | 6.7 | 11.9 |
Values are shown for a 1-wk 2100-kcal menu and are based on compositional analysis (Covance Laboratories) unless otherwise stated. DASH, Dietary Approaches to Stop Hypertension diet; HF-DASH, high-fat, low-carbohydrate DASH diet; oz, ounces; tsp, teaspoons.
Calculated values (Nutrition Data System for Research Software 2010; Nutrition Coordinating Center, University of Minnesota).
Food group servings based on choosemyplate.org. Equivalencies in metric units are as follows: 1 oz = 28 g; 1 cup = 250 mL; 1 tsp = 5 mL.
Based on 1-oz equivalents.
Dietary control was achieved by providing participants with 2 standardized entrées and accompanying side dishes daily (lunch, dinner, and some snacks), representing ∼50% of total energy. Detailed menus, shopping lists, and food preparation instructions were provided for the remaining food items (mostly dairy, produce, and cereal products) to be purchased and prepared at home. Participants were required to come to the clinic weekly to pick up study foods, submit receipts documenting study food purchases, and to meet with the nutritionist to assess compliance with the dietary protocol and adjust energy intake to maintain a stable weight (within 3% of baseline, ±10 pounds maximum). They were also required to maintain their usual physical activity levels during the study and to monitor daily steps by pedometer. Compliance was assessed by measuring 24-h urinary potassium at the end of the second week of each experimental diet. Twenty-four-hour urinary sodium was measured as an indicator of sodium intake.
Experimental measurements
After each 3-wk dietary period, body weight and waist and hip circumference were measured and the percentage of body fat was assessed by bioimpedance (TBF 551 body-weight scale; Tanita). BP was measured at the clinic by using a Dinamap monitor (GE Pro 100 or Critikon Pro 300) after the second week of each diet and on 2 consecutive days at the end of each experimental diet, and the 3 values were averaged. At each instance, BP was measured in a sitting position after 5 min rest 3 times, and the last 2 measurements were averaged. Participants were also provided with a portable BP cuff (Model BP791IT, Omron Healthcare, Inc) and were instructed to self-measure BP twice in the morning and twice in the evening for the last 7 d of each experimental dietary period. Data were automatically recorded on the BP instrument and downloaded for analyses. Urinary potassium and sodium were measured in 24-h urine collections by an outside clinical laboratory (Quest Diagnostics).
Fasting plasma samples collected on 2 consecutive days at the end of each experimental dietary period were analyzed for plasma lipids and lipoproteins, glucose, and insulin. Total cholesterol, HDL cholesterol, triglycerides, and glucose were measured by enzymatic end-point measurements with the use of enzyme reagent kits (Ciba-Corning Diagnostics Corporation) on an AMS Liasys 330 Clinical Chemistry Analyzer. LDL cholesterol was calculated by using the Friedewald equation (17). Total cholesterol, HDL cholesterol, and triglyceride concentrations were monitored throughout by the CDC-National Heart, Lung, and Blood Institute Lipid Standardization Program. Apolipoprotein B (apoB) and apolipoprotein A-I (apo A-I) were measured by immunoturbidimetric assays (Bacton Assay Systems; AMS Liasys 330 analyzer) (18, 19).
Lipoprotein particle concentrations and LDL peak diameter were measured by gas-phase electrophoresis (ion mobility), as previously described (20), with a modified procedure for initially separating the lipoproteins from other plasma proteins (21). Lipoprotein intervals were defined as previously described (22).
Statistical analysis
The primary objective was to compare the DASH and HF-DASH diets for lipid and lipoprotein measurements. At 80% power, an n of 36 would yield a minimum detectable difference between diets of 0.14 mmol/L for LDL cholesterol (SD of response = 0.30 mmol/L), 0.04 g/L for apoB (SD of response = 0.09 g/L), 0.03 mmol/L for HDL cholesterol (SD of response = 0.07 mmol/L), 4.1 mm Hg for systolic BP (SD of response = 8.6 mm Hg), and 2.2 mm Hg for diastolic BP (SD of response = 5.3 mm Hg). The detectable changes in BP were sufficient to confirm the differences observed in the original DASH trial (1). Treatment differences were determined by ANOVA for a 3-treatment crossover design (Stata version 11). Pairwise comparisons between diets were adjusted by the Bonferroni method for 3 group comparisons (HF-DASH diet compared with control diet, HF-DASH diet compared with DASH diet, and DASH diet compared with control diet), and P < 0.017 corresponding to an overall 2-tailed P < 0.05 was considered significant. ANOVA and paired t tests were used to compare triglycerides and total, LDL, and HDL cholesterol after each of the 2 washout periods with baseline to test for the effectiveness of the washout period for normalizing plasma lipids. The analyses were restricted to those subjects who completed all 3 diets.
RESULTS
Study participants
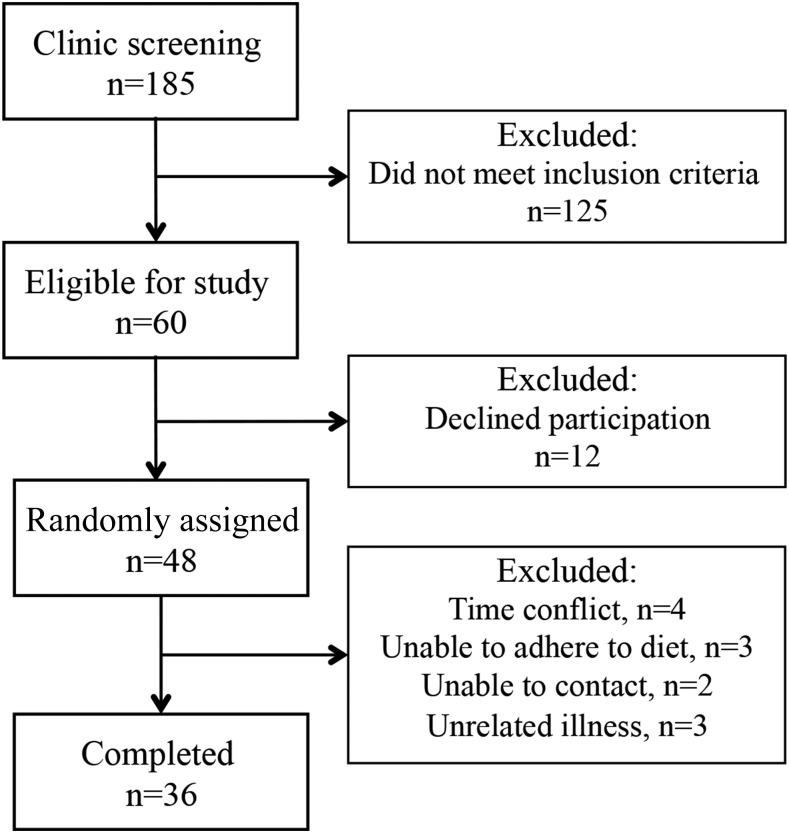
Figure 1 shows the participant flow. Thirty-six participants completed all 3 experimental diets and are included in analyses. Table 1 presents their baseline characteristics. Fasting plasma triglycerides and total, LDL, and HDL cholesterol measured after each of the 2 washout periods showed no significant differences between screening values and their values after the first or second washout period (analyses not shown), indicative of their return to baseline concentrations.
FIGURE 1.
Participant recruitment flow.
As expected, 24-h urinary potassium excretion was significantly higher with the DASH and HF-DASH diets than with the control diet (P < 0.0001 for both, adjusted for period) and did not differ between the DASH and HF-DASH diets (mean ± SE: HF-DASH diet, 81.5 ± 3.5; DASH diet, 83.5 ± 3.5; and control diet, 50.5 ± 3.5 mmol), consistent with good dietary compliance. Urinary sodium excretion did not differ between diets (mean ± SE: HF-DASH diets, 116.6 ± 7.8; DASH diet, 119.3 ± 7.8; and control diet, 129.0 ± 7.8 mmol; P = 0.49, adjusted for period). Body weight remained stable throughout the study and there were no differences by diet (mean ± SE: HF-DASH diet, 79.7 ± 0.1; DASH diet, 79.6 ± 0.1; and control diet, 79.8 ± 0.1 kg; P-treatment = 0.62).
Effects of diets on BP
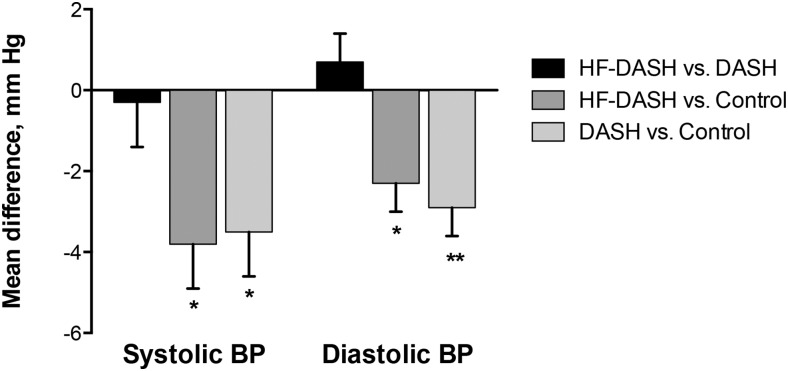
Table 3 presents the statistical evaluation of the crossover design’s treatment, period, and sequence effects along with the adjusted treatment means and their SEs. Significant treatment effects were observed for systolic and diastolic BP, such that the DASH and HF-DASH diets produced significant and comparable reductions relative to the control diet (Figure 2), with no differences between the DASH and HF-DASH diets.
TABLE 3.
Crossover analyses of the effects of diet on BP, lipids, and lipoproteins1
| Group |
P |
||||||
| HF-DASH | DASH | Control | Treatment | Carry-forward | Period | Sequence | |
| Systolic BP, mm Hg | 125.0 ± 0.8a | 125.4 ± 0.8a | 128.8 ± 0.8b | 0.0001 | 0.0001 | 0.004 | 0.91 |
| Diastolic BP, mm Hg | 79.0 ± 0.5a | 78.3 ± 0.5a | 81.2 ± 0.5b | 0.0001 | 0.0001 | 0.09 | 0.63 |
| Triglycerides, mmol/L | 1.15 ± 0.04a | 1.32 ± 0.04b | 1.20 ± 0.04a,b | 0.03 | 0.99 | 0.18 | 0.25 |
| Total cholesterol, mmol/L | 4.53 ± 0.06a | 4.51 ± 0.06a | 4.76 ± 0.06b | 0.02 | 0.65 | 0.11 | 0.86 |
| LDL cholesterol, mmol/L | 2.65 ± 0.05a,b | 2.60 ± 0.05a | 2.81 ± 0.05b | 0.04 | 0.29 | 0.09 | 0.79 |
| HDL cholesterol, mmol/L | 1.36 ± 0.02a,b | 1.32 ± 0.02a | 1.40 ± 0.02b | 0.03 | 0.29 | 0.14 | 0.47 |
| Non–HDL cholesterol, mmol/L | 3.16 ± 0.06 | 3.19 ± 0.06 | 3.36 ± 0.06 | 0.10 | 0.32 | 0.12 | 0.44 |
| apo A-I, g/L | 1.35 ± 0.01a,b | 1.32 ± 0.01a | 1.38 ± 0.01b | 0.02 | 0.17 | 0.63 | 0.42 |
| apoB, g/L | 0.76 ± 0.01 | 0.76 ± 0.01 | 0.80 ± 0.01 | 0.22 | 0.28 | 0.02 | 0.43 |
| LDL peak diameter, nm | 22.3 ± 0.0a | 22.1 ± 0.0b | 22.2 ± 0.0a | 0.004 | 0.81 | 0.42 | 0.23 |
| Lipoprotein particle concentrations, nmol/L | |||||||
| VLDL | |||||||
| Total | 97.8 ± 2.5 | 105.0 ± 2.5 | 104.4 ± 2.5 | 0.15 | 0.85 | 0.35 | 0.71 |
| Large | 12.9 ± 0.4a | 14.8 ± 0.4b | 14.0 ± 0.4a,b | 0.02 | 0.97 | 0.25 | 0.45 |
| Medium | 39.2 ± 1.1a | 43.2 ± 1.1b | 42.2 ± 1.1a,b | 0.04 | 0.84 | 0.37 | 0.61 |
| Small | 45.8 ± 1.2 | 47.0 ± 1.2 | 48.2 ± 1.2 | 0.39 | 0.64 | 0.51 | 0.90 |
| IDL | 243 ± 5a,b | 237 ± 5a | 259 ± 5b | 0.02 | 0.51 | 0.85 | 0.94 |
| LDL | |||||||
| Total | 702 ± 14 | 716 ± 14 | 744 ± 14 | 0.44 | 0.10 | 0.06 | 0.46 |
| Large | 433 ± 11a,b | 414 ± 11a | 468 ± 11b | 0.004 | 0.10 | 0.16 | 0.92 |
| Medium | 119 ± 4 | 123 ± 4 | 130 ± 4 | 0.78 | 0.01 | 0.003 | 0.42 |
| Small | 101 ± 4 | 106 ± 4 | 104 ± 4 | 0.77 | 0.69 | 0.34 | 0.17 |
| Very small | 185 ± 5 | 201 ± 5 | 185 ± 5 | 0.12 | 0.72 | 0.61 | 0.36 |
| HDL | |||||||
| Total | 15,191 ± 184 | 15,066 ± 183 | 15,467 ± 183 | 0.32 | 0.94 | 0.67 | 0.80 |
| Large | 3960 ± 70 | 3893 ± 70 | 4038 ± 69 | 0.20 | 0.25 | 0.33 | 0.77 |
| Small | 11,231 ± 130 | 11,173 ± 130 | 11,429 ± 129 | 0.45 | 0.60 | 0.27 | 0.75 |
Values are means ± SEs; n = 36. Data were analyzed by ANOVA for a 3-treatment crossover design. Values in the same row not sharing a superscript letter differ from each other, P < 0.017 (Bonferroni adjustment for 3 pairwise comparisons). apo A-I, apolipoprotein A-I; apoB, apolipoprotein B; BP, blood pressure; DASH, Dietary Approaches to Stop Hypertension diet; HF-DASH, high-fat, low-carbohydrate DASH diet; IDL, intermediate-density lipoprotein.
FIGURE 2.
Differences between diets in systolic and diastolic BP. *P < 0.017, **P < 0.001. Values are means ± SEs, adjusted for dietary period; n = 36. Data were analyzed by ANOVA for a 3-treatment crossover design. BP, blood pressure; DASH, Dietary Approaches to Stop Hypertension diet; HF-DASH, high-fat, low-carbohydrate DASH diet.
There were no significant sequence effects (Table 3), but there were significant carry-forward effects for both systolic and diastolic BP and a significant period effect for systolic BP. The carry-forward effect appeared to be due to lower systolic and diastolic BP after the HF-DASH diet compared with the DASH, control, or no previous diet. Mean BPs were, in fact, lower at the end of the washout period after the HF-DASH diet than after the other diets for systolic (mean ± SE: −4.1 ± 1.7 mm Hg; P = 0.02) and diastolic (−0.9 ± 1.1 mm Hg; P = 0.40) BPs. The carry-forward effect did not appear to be the result of any individual participant.
Both morning and evening systolic and diastolic BPs measured by the participants at home were similarly reduced with the DASH and HF-DASH diets compared with the control diet (Supplemental Table 2), confirming the treatment effect of the DASH and HF-DASH diets on BP. There were no significant sequence, period, or carry-forward effects for home BP measurements.
Effects of diets on plasma lipids and lipoproteins
Significant treatment effects were observed for plasma concentrations of triglycerides, total cholesterol, LDL cholesterol, and HDL cholesterol, apo A-I, LDL peak diameter, large and medium VLDL, intermediate-density lipoprotein (IDL), and large LDL concentrations (Table 3).
Detailed pairwise comparisons between diets for all lipid and lipoprotein measurements are shown in Supplemental Table 3. For the primary comparison of the DASH and HF-DASH diets, the latter resulted in significantly lower plasma triglycerides, large and medium VLDL concentrations, and significantly higher LDL peak particle diameter (differences shown in Figure 3). There were no significant differences between the DASH and HF-DASH diets for any other lipid or lipoprotein measurement after Bonferroni correction.
FIGURE 3.
Differences between diets for plasma triglycerides (A), VLDL concentrations (large, medium, small) (B), and LDL peak diameter (C). *P < 0.017, **P < 0.001. Values are means ± SEs, adjusted for dietary period; n = 36. Data were analyzed by ANOVA for a 3-treatment crossover design. DASH, Dietary Approaches to Stop Hypertension diet; HF-DASH, high-fat, low-carbohydrate DASH diet.
Both the DASH and the HF-DASH diets significantly reduced total cholesterol compared with the control diet (Supplemental Table 3). The DASH diet also significantly decreased LDL cholesterol, HDL cholesterol, apo A-I, IDL concentrations, large LDL concentrations, and LDL peak diameter compared with the control diet. Except for lower total cholesterol, none of the lipid and lipoprotein measurements differed significantly between the HF-DASH and control diets after Bonferroni correction (Supplemental Table 3).
There were no significant sequence effects for any of the lipid and lipoprotein variables examined (Table 3). None of the variables that showed a significant treatment effect exhibited significant carry-forward or period effects.
DISCUSSION
The DASH diet, which was developed and validated as a means for lowering BP, was formulated to include low-fat and nonfat dairy foods (1, 14). In this study, we tested whether the BP benefit, as well as a favorable lipid and lipoprotein profile, could be maintained by the HF-DASH diet that includes full-fat dairy foods, with a corresponding increase in total and saturated fat, and a reduction in carbohydrate achieved primarily by reducing fruit juices and sugars, because sugar intake is associated with detrimental effects on cardiovascular disease risk factors (23). The HF-DASH diet lowered both systolic and diastolic BP to an extent similar to the DASH diet, indicating that the diet components responsible for the BP reduction were retained in the HF-DASH diet. Although the sodium content of the control diet was slightly higher than that of the 2 experimental diets (Table 2), this difference was similar to that observed in the original DASH trial (1). Furthermore, 24-h urine sodium measurements were similar on all 3 diets, indicating that the BP reductions with the DASH and HF-DASH diets were not attributable to lower sodium intake.
When substituted for carbohydrates or unsaturated fats, saturated fats have been consistently shown to increase LDL cholesterol (24). We previously showed that with limitation of carbohydrate intake, the increase in LDL cholesterol induced by saturated fat is due primarily to large, cholesterol-rich LDL particles and not small, dense LDL particles (25). Indeed, in the present study, we found that the reduction in LDL cholesterol with the DASH diet compared with the control diet occurred in conjunction with lower concentrations of large LDL particles as well as of IDL particles, which both contribute cholesterol content to the standard LDL-cholesterol measurement (26). However, despite a 6% of energy higher saturated fat content in the HF-DASH diet compared with the DASH diet, there were no significant differences in LDL cholesterol or any of the LDL subclasses between these diets. There may be features of the DASH diet that mitigate the increase in LDL cholesterol that is typically observed with higher saturated fat intake.
It is of interest that there was a significantly higher LDL peak particle diameter with the HF-DASH diet compared with the DASH diet. Although this difference was of relatively small magnitude, it corresponded to a trend, albeit nonsignificant, for relatively higher concentrations of larger LDL particles and lower concentrations of smaller LDL particles with the HF-DASH diet with no net difference in total LDL particle concentrations. This change in the distribution of LDL particles may be more easily detected by the peak diameter than the individual subfractions. The shift toward larger LDL particles with the HF-DASH diet may be attributed at least in part to the lower carbohydrate content of this diet compared with the DASH diet, because a shift from smaller to larger LDL particles was previously shown to correlate with reductions in plasma triglyceride and VLDL concentrations resulting from reduced carbohydrate or sugar intake (23, 27). The reductions in triglycerides and VLDL particle concentrations with the HF-DASH diet compared with the DASH diet observed in the present study were relatively modest as might be expected from the moderate difference in carbohydrate content between the diets (43% compared with 55% of energy). It is possible that these differences were not of sufficient magnitude to elicit the significant reductions in small, dense LDL particles as well as in apoB (an index of LDL particle number) that have been observed previously with more substantial reductions in carbohydrate intake (25, 28).
The present study confirmed previous observations that the DASH diet lowers HDL cholesterol (5), which is consistent with a significant reduction in apo A-I compared with the control diet. These changes were not observed with the HF-DASH diet, although the differences between the effects of the HF-DASH and DASH diets did not reach significance. The basis for the reduction in HDL cholesterol with the DASH diet is not known, although it is noteworthy that this effect was not associated with a change in HDL particle concentrations, suggesting that it may represent a change in HDL composition.
Other investigators have also tested modifications of the DASH diet on BP or lipid risk factors. The OmniHeart trial tested the replacement of 10% of energy from carbohydrate in a DASH diet with 10% of energy from unsaturated, primarily monounsaturated, fat or 10% of energy from protein (10). The protein and monounsaturated fat diets yielded similar or greater reductions in BP compared with the standard, high-carbohydrate DASH diet. Replacing carbohydrate with monounsaturated fat reduced total cholesterol and triglycerides and increased HDL cholesterol without affecting LDL cholesterol. Replacing carbohydrate with protein reduced total, LDL, and HDL cholesterol and triglycerides (10). The Beef in an Optimal Lean Diet Study found that the inclusion of lean beef in a low-saturated-fat DASH-like diet resulted in comparable effects on lipid and lipoprotein measures compared with a standard DASH diet (29). Sayer et al. (30) recently showed that a DASH-style diet containing either lean pork or chicken and fish similarly reduced BP. Together with results from the present study, the above findings provide evidence that aspects of the DASH diet can be modified without compromising its benefits on BP or LDL-cholesterol lowering, offering flexibility in food choices for individuals following the DASH diet.
The crossover design of this trial was largely successful in that lipids and lipoprotein returned to baseline concentrations and there were no significant sequence effects and no carry-forward effects for most of the variables. The exceptions were the clinic measurements of systolic and diastolic BPs, whose reductions showed significant carry-forward on the HF-DASH diet, an unexpected and unexplained effect because there was no such carry-forward effect for the home BP measurements.
Strengths of our study include high dietary compliance as measured by urinary biomarkers and lack of weight change as a potential confounder. Limitations include a relatively small sample size and a short intervention duration.
In conclusion, the results of this study indicate that modification of the DASH diet to allow for more liberal total and saturated fat intake in conjunction with moderate limitation of carbohydrate intake, primarily from fruit juices and sugars, results in lower concentrations of triglycerides and VLDL particles, with no increases in total or LDL cholesterol and no attenuation of the favorable BP response to the standard DASH diet. Therefore the modified HF-DASH diet studied here presents an effective alternative to this widely recommended dietary pattern, with less-stringent dietary fat constraints, which may promote even broader implementation.
Acknowledgments
We thank Sarah King for technical assistance, Megan Bennett and Anna Doheny for administering clinical protocols, and Joyce Gray of the Ethnic Health Institute for assisting with participant recruitment.
The authors’ responsibilities were as follows—SC, NB, and RMK: designed the research; SC, NB, BS, and RMK: conducted the research; SC, PTW, and RMK: analyzed the data; SC, NB, PTW, GAB, and RMK: wrote the manuscript; SC had primary responsibility for the final content; and all authors: read and approved the final manuscript. RMK has previously received and is currently receiving research funding from Dairy Management Inc. for this and other projects. None of the other authors reported a conflict of interest. This was an investigator-initiated study, and its financial supporters had no role in the study design, implementation, data analysis, or data interpretation.
Footnotes
Abbreviations used: apo A-I, apolipoprotein AI; apoB, apolipoprotein B; BP, blood pressure; DASH, Dietary Approaches to Stop Hypertension; HF-DASH, higher-fat, lower-carbohydrate Dietary Approaches to Stop Hypertension; IDL, intermediate-density lipoprotein.
REFERENCES
- 1.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. ; DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 2.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER III, Simons-Morton DG, et al. ; DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 3.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 2008;168:713–20. [DOI] [PubMed] [Google Scholar]
- 4.Harsha DW, Sacks FM, Obarzanek E, Svetkey LP, Lin PH, Bray GA, Aickin M, Conlin PR, Miller ER III, Appel LJ. Effect of dietary sodium intake on blood lipids: results from the DASH-sodium trial. Hypertension 2004;43(2):393–8. [DOI] [PubMed] [Google Scholar]
- 5.Obarzanek E, Sacks FM, Vollmer WM, Bray GA, Miller ER III, Lin PH, Karanja NM, Most-Windhauser MM, Moore TJ, Swain JF, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr 2001;74:80–9. [DOI] [PubMed] [Google Scholar]
- 6.Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: results from the A to Z weight loss study. Int J Obes (Lond) 2008;32:985–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwan MW, Wong MC, Wang HH, Liu KQ, Lee CL, Yan BP, Yu CM, Griffiths SM. Compliance with the Dietary Approaches to Stop Hypertension (DASH) diet: a systematic review. PLoS One 2013;8:e78412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 2005;293:43–53. [DOI] [PubMed] [Google Scholar]
- 9.Windhauser MM, Evans MA, McCullough ML, Swain JF, Lin PH, Hoben KP, Plaisted CS, Karanja NM, Vollmer WM; DASH Collaborative Research Group. Dietary adherence in the Dietary Approaches to Stop Hypertension trial. J Am Diet Assoc 1999;99(8 Suppl):S76–83. [DOI] [PubMed] [Google Scholar]
- 10.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER III, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, et al. . Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 2005;294(19):2455–64. [DOI] [PubMed] [Google Scholar]
- 11.Henkin Y, Garber DW, Osterlund LC, Darnell BE. Saturated fats, cholesterol, and dietary compliance. Arch Intern Med 1992;152:1167–74. [PubMed] [Google Scholar]
- 12.Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Better dietary adherence and weight maintenance achieved by a long-term moderate-fat diet. Br J Nutr 2007;97:399–404. [DOI] [PubMed] [Google Scholar]
- 13.Epstein DE, Sherwood A, Smith PJ, Craighead L, Caccia C, Lin PH, Babyak MA, Johnson JJ, Hinderliter A, Blumenthal JA. Determinants and consequences of adherence to the dietary approaches to stop hypertension diet in African-American and white adults with high blood pressure: results from the ENCORE trial. J Acad Nutr Diet 2012;112:1763–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karanja NM, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, Champagne CM, Hoben KP; DASH Collaborative Research Group. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. J Am Diet Assoc 1999;99(8 Suppl):S19–27. [DOI] [PubMed] [Google Scholar]
- 15.Lin PH, Aickin M, Champagne C, Craddick S, Sacks FM, McCarron P, Most-Windhauser MM, Rukenbrod F, Haworth L; Dash-Sodium Collaborative Research Group. Food group sources of nutrients in the dietary patterns of the DASH-Sodium trial. J Am Diet Assoc 2003;103:488–96. [DOI] [PubMed] [Google Scholar]
- 16.Vogt TM, Appel LJ, Obarzanek E, Moore TJ, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Cutler JA, Windhauser MM, et al. ; DASH Collaborative Research Group. Dietary Approaches to Stop Hypertension: rationale, design, and methods. J Am Diet Assoc 1999;99(8 Suppl):S12–8. [DOI] [PubMed] [Google Scholar]
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502. [PubMed] [Google Scholar]
- 18.Rifai N, King ME. Immunoturbidimetric assays of apolipoproteins A, AI, AII, and B in serum. Clin Chem 1986;32:957–61. [PubMed] [Google Scholar]
- 19.Smith SJ, Cooper GR, Henderson LO, Hannon WH. An international collaborative study on standardization of apolipoproteins A-I and B. Part I. Evaluation of a lyophilized candidate reference and calibration material. Clin Chem 1987;33:2240–9. [PubMed] [Google Scholar]
- 20.Caulfield MP, Li S, Lee G, Blanche PJ, Salameh WA, Benner WH, Reitz RE, Krauss RM. Direct determination of lipoprotein particle sizes and concentrations by ion mobility analysis. Clin Chem 2008;54(8):1307–16. [DOI] [PubMed] [Google Scholar]
- 21.Mora S, Caulfield MP, Wohlgemuth J, Chen Z, Superko HR, Rowland CM, Glynn RJ, Ridker PM, Krauss RM. Atherogenic lipoprotein subfractions determined by ion mobility and first cardiovascular events after random allocation to high-intensity statin or placebo: the JUPITER trial. Circulation 2015;132(23):2220–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Musunuru K, Orho-Melander M, Caulfield MP, Li S, Salameh WA, Reitz RE, Berglund G, Hedblad B, Engstrom G, Williams PT, et al. Ion mobility analysis of lipoprotein subfractions identifies three independent axes of cardiovascular risk. Arterioscler Thromb Vasc Biol 2009;29(11):1975–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Te Morenga LA, Howatson AJ, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr 2014;100(1):65–79. [DOI] [PubMed] [Google Scholar]
- 24.Siri-Tarino PW, Chiu S, Bergeron N, Krauss RM. Saturated fats versus polyunsaturated fats versus carbohydrates for cardiovascular disease prevention and treatment. Annu Rev Nutr 2015;35:517–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krauss RM, Blanche PJ, Rawlings RS, Fernstrom HS, Williams PT. Separate effects of reduced carbohydrate intake and weight loss on atherogenic dyslipidemia. Am J Clin Nutr 2006;83(5):1025–31; quiz: 205. [DOI] [PubMed] [Google Scholar]
- 26.Havel RJ, Rapaport E. Management of primary hyperlipidemia. N Engl J Med 1995;332:1491–8. [DOI] [PubMed] [Google Scholar]
- 27.Krauss RM, Williams PT, Lindgren FT, Wood PD. Coordinate changes in levels of human serum low and high density lipoprotein subclasses in healthy men. Arteriosclerosis 1988;8:155–62. [DOI] [PubMed] [Google Scholar]
- 28.Dreon DM, Fernstrom HA, Williams PT, Krauss RM. A very low-fat diet is not associated with improved lipoprotein profiles in men with a predominance of large, low-density lipoproteins. Am J Clin Nutr 1999;69:411–8. [DOI] [PubMed] [Google Scholar]
- 29.Roussell MA, Hill AM, Gaugler TL, West SG, Heuvel JP, Alaupovic P, Gillies PJ, Kris-Etherton PM. Beef in an Optimal Lean Diet Study: effects on lipids, lipoproteins, and apolipoproteins. Am J Clin Nutr 2012;95:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sayer RD, Wright AJ, Chen N, Campbell WW. Dietary Approaches to Stop Hypertension diet retains effectiveness to reduce blood pressure when lean pork is substituted for chicken and fish as the predominant source of protein. Am J Clin Nutr 2015;102(2):302–8. [DOI] [PMC free article] [PubMed] [Google Scholar]