Abstract
Disaster exposure during pregnancy has received limited attention. This study examined the impact of the 2008 Iowa Floods on perinatal maternal depression and well-being, and the role of peritraumatic distress as a possible mechanism explaining this link. Perinatal women (N = 171) completed measures of depressive symptoms and general well-being at 5 timepoints from pregnancy to 30 months postpartum. Objectively assessed prenatal flood exposure was associated with greater depression (r = .15). Further, flood-related peritraumatic distress was uniquely associated with greater depression (r = .23), and was a key mechanism through which flood exposure led to depression. Prenatal flood exposure was also associated with general well-being (r = .18); however, a mechanism other than peritraumatic distress appears to have been responsible for the effect of flood exposure on well-being. We discuss the implications of these findings for informing etiological models and enhancing the efficacy of interventions for maternal psychopathology.
Maternal depression during pregnancy and the months following childbirth (i.e., perinatal depression) is a serious mental health concern, with prevalence rates ranging from 7% to 19% (Gavin et al., 2005; O’Hara & McCabe, 2013). Perinatal depression occurs in the context of childbearing when exceptional demands are placed on the psychological and physiological resources of women (O’Hara & McCabe, 2013). Maternal depression can have profound and lasting effects on child development, predicting higher rates of child psychopathology (Goodman et al., 2011), impaired cognitive development (Grace, Evindar, & Stewart, 2003), and poor physical health (e.g., Gump et al., 2009). Prenatal maternal stress (i.e., acute or chronic stress experienced during pregnancy) is one of the most robust risk factors for perinatal depression (Beck, 2001; O’Hara & Swain, 1996); however, the mechanisms explaining how prenatal stress ultimately contributes to maternal depression have been neglected (O’Hara & McCabe, 2013). Further, exposure to traumatic forms of stress during pregnancy has received limited attention.
The impact of traumatic stress on depression is well documented (e.g., Young, Abelson, Curtis, & Nesse, 1997); however, its role in depression experienced by women during the perinatal period has been relatively overlooked, with a few notable exceptions (Almeida, Cunha, Pires, & Sá, 2013; Delahaije, Dirksen, Peeters, & Smits, 2013; Howard, Oram, Galley, Trevillion, & Feder, 2013; Qu et al., 2012). Research on the link between trauma and perinatal depression has been inconclusive, perhaps because it has been focused on whether women have been exposed to an event that is objectively defined as traumatic (e.g., exposure to domestic violence) without considering subjective reactions in response to those exposures.
Peritraumatic distress (i.e., distress experienced during and in the minutes and hours following a potentially traumatic event) is associated with a range of mental health outcomes (e.g., Brunet et al., 2001, 2013; Guardia et al., 2013; Thomas, Saumier, & Brunet, 2012). Indeed, peritraumatic distress demonstrates incremental predictive utility beyond other characteristics of traumatic events (e.g., posttraumatic supports), having a notable effect on the development of posttraumatic stress symptoms and disorder (PTSD; Ozer, Best, Lipsey, & Weiss, 2003). Peritraumatic distress is not only associated with PTSD, but also with complicated grief symptoms (Hargrave, Leathem, & Long, 2012) and disordered eating (Rodgers, Franko, Brunet, Herbert, & Bui, 2012). Nonetheless, the role of peritraumatic distress in the development of depression is unclear. As is the case in PTSD, peritraumatic distress may represent a key mechanism linking certain forms of stress exposure to depression, including maternal depression experienced during the perinatal period.
Natural disasters provide a scientifically important context for examining peritraumatic distress as a process contributing to depression because they generate a diverse range of stressors of varying degrees of intensity (Norris, 2006), and often lead to high levels of subjective distress (Norris et al., 2002). Further, there are few opportunities, outside of laboratory experiments, to quasirandomly assign stress to participants. Because psychopathology is associated with subsequent exposure to traumatic events (e.g., Cougle, Resnick, & Kilpatrick, 2009), it is difficult to disentangle temporal relations between these variables; however, natural disasters have a sporadic, sudden onset, and are relatively independent of individual influence (unlike many other psychosocial stressors), helping to reduce confounds such as shared vulnerabilities for both stress and psychopathology.
In June 2008, the U.S. Midwest experienced its worst flooding in more than 50 years, and 85 of Iowa’s 99 counties were declared disaster areas. The total cost of recovery has been estimated to be as high as $10 billion. More than 38,000 people were driven from their homes. A primary goal of the present study was to examine whether exposure to the Iowa floods during pregnancy initiated a cascade effect, leading to greater maternal depression via peritraumatic distress. We examined the long-term impact of flood exposure on depression assessed at five timepoints from pregnancy to 30 months postpartum. Multiwave longitudinal designs that span multiple years provide numerous advantages relative to cross-sectional or two-wave designs. Symptom trajectories can be modeled over time, providing a more sensitive analysis of the developmental course of depression from pregnancy throughout several years following childbirth.
A focus on perinatal women was especially important given that women are already at increased risk for depression during pregnancy and the months following childbirth due to the numerous changes and adjustments inherent to this transition. Further, understanding the role of traumatic stress in long-term trajectories of maternal depression is of critical importance given the implications of maternal psychopathology for child development, including emotional and physical well-being (Goodman et al., 2011).
Another goal of the study was to examine the sequence leading from flood exposure to well-being and quality of life of mothers. Healthy maternal psychological functioning—a dimension of maternal mental health that is inversely related to depression, yet also distinct (Watson et al., 2007)—is often overlooked. This is problematic because positive affect has important implications for clinical treatment outcomes independent from negative affect (Frisch, Cornell, Villanueva, & Retzlaff, 1992). Further, mothers who are low in positive affect tend to be less socially engaged, and display less responsiveness, warmth, and support during interactions with their children (Lovejoy, Graczyk, O’Hare, & Neuman, 2000) which in turn is associated with maladaptive child outcomes (e.g., Kochanska, Aksan, Prisco, & Adams, 2008). Accordingly, we also examined the extent to which women experienced changes in energy level, positive affect, and optimism (i.e., well-being) over the perinatal period, as a function of traumatic stress from the floods.
We predicted that greater severity of flood exposure would be associated with greater maternal depression and lower levels of well-being over the perinatal period, up to 30 months postpartum. Further, we predicted that peritraumatic distress would represent a primary mechanism linking flood exposure to maternal outcomes.
Method
Participants and Procedure
A study of psychological functioning during pregnancy was underway at the time of the Iowa floods: the Emotional Experiences of Women During Pregnancy Study (Nylen, O’Hara, & Engeldinger, 2012). Participants in the emotional experiences study were invited to enroll in a new project designed to assess the impact of the floods—The Iowa Flood Study. Further, additional women were recruited for the flood study, and were invited to complete the emotional experiences protocol. Women were eligible to participate if they met the following criteria: (a) 18 years of age or older, (b) pregnant on (or prior to) June 10, 2008 (the onset of the floods), (c) singleton pregnancy, and (d) English speaking. Women were recruited via brochures, press releases, or in person at obstetric clinics and women, infants, and children clinics located in areas affected by the flood. Please see Brock et al. (2014) for a detailed description of the study protocols. A total of 269 participants completed procedures from both the emotional experiences and flood study protocols. All procedures were approved by the University of Iowa Institutional Review Board, and signed consent was obtained from all study participants.
A subsample of 171 women were included in the present report, consisting of women who were exposed to the flood during pregnancy and completed measures of depression at least once during pregnancy. Of these women, 86.6% were in a committed relationship (of whom 94.6% were married), 93.0% identified as White, and 73.7% were employed. The majority of participants were upper middle class (44.4%; Hollingshead socioeconomic status [SES]), and modal income was > $70,001 (35.1%). On average, women were 28.82 years of age at the time of enrollment (SD = 5.12). Approximately one fourth (26.3%) of participants had withdrawn from the study by the fifth wave of data collection (30-months postchildbirth).
The majority of women were exposed to the peak of flooding during the second trimester of pregnancy (45.0%), 29.2% of women were exposed to the flood during the first trimester, and 25.7% during the third trimester. All women completed the emotional experiences protocol (including measures of depression and well-being, as described below) at least once during pregnancy. Approximately one fifth of participants (21.1% n = 36) completed their initial emotional experiences assessment prior to the peak of flooding (M = 2.56 months, SD = 1.74) because they had already been enrolled in the study prior to the onset of the floods. The remaining women were recruited after the flooding began. Measures of prenatal flood exposure and peritraumatic distress were administered immediately after women consented to participate in the flood study protocol (M = 3.47 months after peak of the floods, SD = 4.90, range = 0.95 to 24.67 months postflood).
Measures
Maternal depression and well-being were measured with the Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007). Participants were asked to indicate the degree to which they had experienced a list of symptoms over the past 2 weeks using a 5-point Likert scale ranging from 1 = not at all to 5 = extremely. IDAS scores were obtained at five time points: (1) during pregnancy (M = 3.81 months prior to childbirth, SD = 2.17, range = 7.56 to 0.03 months prior to childbirth), (2) around the time of childbirth (M = 1.86 months prior to childbirth, SD = 0.69, range = 2.96 months prior to childbirth to 0.56-months postchildbirth), (3) 16-months postchildbirth (M = 16.17 months, SD = 1.08, range = 15.11-to 21.36-months postchildbirth), (4) 18-months postchildbirth (M = 17.59 months, SD = 2.63, range = 12.65 to 24.74-months postchildbirth), and (5) 30-months postchildbirth (M = 30.80 months, SD = 1.38, range = 29.14 to 34.66-months postchild-birth). The General Depression Scale (20 items; possible range 20 to 100) includes items capturing a broad range of depressive symptoms whereas the Well-Being Scale (8 items; possible range 8 to 40) includes items of high energy and positive affect (e.g., feelings of optimism and hope, sense of accomplishment, looking forward to the future).
Based on the Storm32 questionnaire (Laplante, Zelazo, Brunet, & King, 2007), the Iowa Flood 100 (IF100) was developed specifically for this study to measure each woman’s degree of objective hardship resulting from the Iowa floods. The measure simply instructed subjects to answer questions about the hardships they experienced during the flood. Items were either yes or no, or scaled with 3–6 response options. Items were written to collect factual information rather than subjective experience. Items assessed four key dimensions of natural disasters: threat to life or physical integrity (13 items; e.g., “Were you physically hurt?”), loss (9 items; e.g., “Was your home damaged?”), scope of each woman’s experience (4 items; e.g., “To what extent was your neighborhood affected?”), and change (13 items; e.g., “How many times were you required to change residence because of the flood?”). A committee of three researchers and a statistician constructed the scoring scheme by examining the distribution of each item, attributing an initial scoring scheme to each item, and adjusting the weights of individual items. This was done over many iterations until consensus was reached about the face validity within and across subscales. Each category was scored such that the sum of the items could range from 0 = no impact to a maximum of 25 points = high impact. A total stress score was calculated by summing the four categories (possible range = 0 to 100). The scales were weighted equally, as was done by McFarlane (1988) because there was no a priori knowledge about which category would have the greatest predictive power. See Brock et al. (2014) for the complete measure and scoring procedures.
The Peritraumatic Distress Inventory (PDI; Brunet et al., 2001) was administered to assess peritraumatic responses that people have during and immediately after a potentially traumatic event. Participants were asked to read a series of statements and “choose the response that best describes your reactions and experiences during the 2008 flood and immediately after.” Participants responded retrospectively to 13 items involving emotional distress and panic-like physical reactions that they had experienced at the time of the flood (e.g., “I was horrified,” “I had physical reactions like sweating, shaking, and my heart pounding,” “I felt sadness and grief, “I thought I might die”) with a 5-point Likert scale ranging from 0 = not at all true to 4 = extremely true. The possible range of scores was 0 to 52.
Data Analysis
Preliminary analyses (e.g., descriptive statistics, correlations, missing data patterns) were conducted for all study variables. Growth curve modeling techniques (GCM) in HLM 7 (Raudenbush, 2001; Raudenbush & Bryk, 2002) were used to test the study hypotheses. GCM estimates a trajectory of change described by two parameters: intercept and slope (rate of change over time). Time was measured in months and was centered at 30-months postpartum. Missing data were addressed via GCM.
To examine average trajectories of IDAS General Depression and Well-Being scores over time, we initially tested linear models of change, separately for each outcome variable, using five waves of data:
where Yij represents one’s score at time i for subject j, β0j is the intercept for subject j, β1j is the rate of linear change in scores over time for subject j, and rij is the residual variance in repeated measures for individual j. We compared the fit of a linear model to that of intercept only model (excluding the time parameter). If a linear model provided superior fit, the linear model was retained.
To examine the link between severity of prenatal flood exposure (IF100) and (a) trajectories of depressive symptoms (IDAS) and (b) trajectories of well-being (IDAS), IF100 scores were added at Level 2. Next, procedures outlined by Zhang, Zyphur, and Preacher (2008) for testing a 2–2–1 multilevel mediation model were followed to examine peritraumatic distress (PDI) as a mediator of the link between prenatal flood exposure (IF100) and trajectories of depressive symptoms and maternal well-being (IDAS). First, we conducted a regression analysis to estimate the univariate association between the predictor (IF100) and the mediator (PDI). Next, we examined the simultaneous effects of the predictor and mediator on each outcome. Finally, we used a Monte Carlo Method for Assessing Mediation (MCMAM; Mackinnon, Lockwood, & Williams, 2004), using 20,000 repetitions for the simulation (Selig & Preacher, 2008) to estimate indirect effects.
Results
Descriptive statistics and correlations are reported in Table 1. Objective flood exposure and peritraumatic distress were positively correlated with each other, and with maternal depressive symptoms during pregnancy and the first 18 months postpartum (but not at 30-months postpartum), and with maternal well-being at 4 months prior to birth.
Table 1.
Descriptive Statistics and Correlations of Prenatal Flood Exposure, Peritraumatic Distress, Depression, and Well-Being at Five Time Points
| Variable | n | M | SD | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. IF100 | 171 | 8.53 | 11.02 | – | – | ||||||||||
| 2. PDI | 171 | 10.82 | 8.30 | .88 | .49** | – | |||||||||
| IDAS Depression | |||||||||||||||
| 3. 4-Months ante | 170 | 39.08 | 11.05 | .90 | .37** | .42** | – | ||||||||
| 4. 2-Months ante | 116 | 37.75 | 9.83 | .89 | .22* | .39** | .76** | – | |||||||
| 5. 16-Months post | 115 | 36.36 | 9.87 | .89 | .29** | .27** | .66** | .67** | – | ||||||
| 6. 18-Months post | 120 | 34.74 | 11.00 | .92 | .26** | .40** | .60** | .68** | .78** | – | |||||
| 7. 30-Months post | 98 | 33.44 | 8.83 | .91 | .19 | .17 | 44** | 51** | .66** | .62** | – | ||||
| IDAS Well-Being | |||||||||||||||
| 8. 4-Months ante | 169 | 23.94 | 6.34 | .90 | −.25** | −.20** | −.64** | −.54** | −.54** | −.62** | −.32** | – | |||
| 9. 2-Months ante | 117 | 24.38 | 6.29 | .91 | −.03 | −.21* | −.51** | −.64** | −.44** | −.62** | −.44** | .70** | – | ||
| 10. 16-Months post | 116 | 25.20 | 6.48 | .85 | −.14 | −.12 | −.53** | −.59** | −.66** | −.65** | −.50** | .70** | .70** | – | |
| 11. 18-Months post | 120 | 24.14 | 6.80 | .91 | −.05 | −.01 | −.28** | −.32** | −.43** | −.54** | −.36** | .61** | .61** | .68** | – |
| 12. 30-Months post | 98 | 25.06 | 6.00 | .90 | .01 | −.01 | −.26** | −.40** | −.48** | −.48** | −.58** | .52** | .66** | .69** | .59** |
Note. IF100 = Iowa Flood 100—prenatal flood exposure; PDI = Peritraumatic Distress Inventory; IDAS = Inventory of Depression and Anxiety Symptoms; ante = prior to childbirth; post = after childbirth.
p < .05.
p < .01.
Depressive symptoms decreased, on average, over time, t(170) = −5.06, p < .001. There was significant between-subject variability in the intercept parameter, χ2(134) = 549.06, p < .001, and the slope parameter, χ2(137) = 286.05, p < .001. A quadratic model did not provide a superior fit to the data, χ2(3) = 2.10, p > .500.
On average, there was no systematic linear increase or decrease in well-being over time, t(170) = 1.56, p = .121. Further, a nested model comparison revealed that adding the linear parameter to the model did not improve the fit, χ2(2) = 3.47, p = .174. Consequently, a more parsimonious intercept-only model was retained that modeled well-being as fluctuating (waxing and waning) over time.
A linear model best represented the nature of change in depressive symptoms over time. Accordingly, the following model was tested to examine the link between severity of prenatal flood exposure (IF100) and (a) rates of change in depressive symptoms over time (β1j) and (b) levels of symptoms at 30-months postpartum (β0j):
Greater flood exposure was associated with higher levels of depressive symptoms, t(169) = 2.03, p = .044, but not with rates of change in symptoms over time, t(169) = −1.71, p = .089. The overall linear trajectory was higher (i.e., symptoms were higher at any point in time up to 30-months postpartum) to the extent that flood exposure was greater. See Table 2 for detailed results.
Table 2.
Results of Models Linking Prenatal Flood Exposure to Depression and Well-Being
| Variable | γ | SE | t | ES (r) |
|---|---|---|---|---|
| Flood exposure predicts | ||||
| depressive symptoms | ||||
| β0j (Intercept) | ||||
| Intercept, γ00 | 34.12 | 0.87 | 39.29**** | |
| IF100, γ01 | 0.16 | 0.08 | 2.03* | .15 |
| β1j (Time) | ||||
| Intercept, γ10 | −0.13 | 0.03 | −5.13**** | |
| IF100, γ11 | 0.00 | 0.00 | −1.71 | .13 |
| Peritraumatic distress mediates effect of flood exposure on depression |
||||
| β0j (Intercept) | ||||
| Intercept, γ00 | 34.14 | 0.87 | 39.39**** | |
| IF100, γ01 | 0.13 | 0.07 | 1.76 | .13 |
| PDI, γ02 | 0.34 | 0.11 | 3.07*** | .23 |
| β1j (Time) | ||||
| Intercept, γ10 | −0.13 | 0.03 | −5.03**** | |
| Flood exposure predicts maternal well-being |
||||
| β0j (Intercept) | ||||
| Intercept, γ00 | 24.39 | 0.43 | 57.16**** | |
| IF100, γ01 | −0.07 | 0.03 | −2.42* | .18 |
Note. N = 171. IF100 = Iowa Flood 100—prenatal flood exposure; PDI = Peritraumatic Distress Inventory; ES (r) = effect size r = √[t2 / (t2 + df)].
p < .05.
p < .005.
p < .001.
We predicted that the effect of flood exposure on depression would be mediated by peritraumatic distress in response to the flood. First, we demonstrated a significant univariate association between the predictor (IF100) and the mediator (PDI), b = 0.37, SE = 0.05, p < .001.
Next, we examined the simultaneous effects of the predictor and mediator on the outcome. Given that the link between flood exposure and the slope parameter (β1j) was not significant in the prior analysis, we tested the following model:
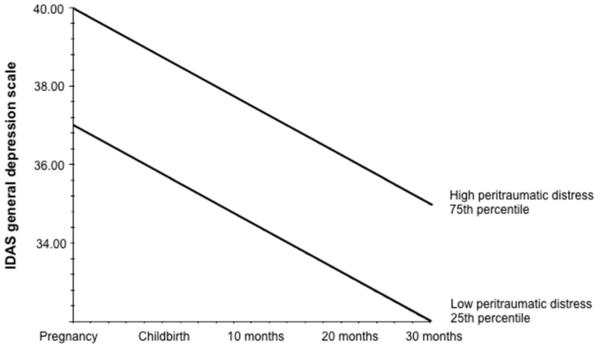
Peritraumatic distress was associated with symptom levels, t(168) = 3.07, p = .002, when adjusting for flood exposure. Notably, the effect of flood exposure on symptoms was no longer significant when adjusting for peritraumatic distress, t(168) = 1.76, p = .080. See Table 2 for detailed model results and Figure 1 for a graphical depiction of the results: Trajectories of depressive symptoms over time are graphed at high (75th percentile) versus low (25th percentile) levels of peritraumatic distress, adjusting for flood exposure. The 95% confidence interval [0.04, 0.22] suggested an indirect effect of flood exposure on depressive symptoms via peritraumatic distress.
Figure 1.
N = 171. Trajectories of depressive symptoms from pregnancy to 30 months postpartum for women reporting high (75th percentile) versus low (25th percentile) levels of pentraumatic distress (PDI scores), adjusting for objective scores of flood exposure. Depressive symptoms decline at a significant rate over time regardless of peritraumatic distress level. IDAS = Inventory of Depression and Anxiety Symptoms.
As previously reported, an intercept only model was the best fit for IDAS Well-Being scores; therefore, the following model was specified to examine the association between flood exposure (IF100) and overall levels of maternal well-being:
Greater flood exposure was associated with lower overall levels of maternal well-being across the perinatal period, t(169) = −2.42, p = .017 (Table 2). Peritraumatic distress (PDI) was added to the model: β0j = γ00 + γ01 (IF100) + γ 02 (PDI) + μ0j; however, peritraumatic distress was not associated with levels of well-being, t(168) = −0.90, p = .369, when adjusting for degree of flood exposure. Accordingly, an indirect effect was not estimated.
As previously reported, approximately one fifth of participants completed the IDAS prior to the peak of flooding because they had already been enrolled in the study before the onset of the floods. Timing of the initial IDAS assessment (i.e., before or after the floods) did not moderate any of the effects in the present report, ts ranged from −1.44 to 1.54, ps > .05.
Discussion
Perinatal depression is a serious mental health concern that not only causes disability in women, but also contributes to maladaptive developmental outcomes in their offspring (Goodman et al., 2011; Grace et al., 2003; Gump et al., 2009). Research has established that stress during pregnancy is a prominent risk factor for perinatal depression (O’Hara & McCabe, 2013), and results of the present study demonstrated that severe, objective hardship as the function of an independent, external stressor had long-term implications for the mental health of women: More severe flood exposure was associated with greater depression during the perinatal period. On the other hand, maternal depressive symptoms decreased, on average, from pregnancy to 30-months postpartum, although this overall linear trajectory was higher or lower depending on levels of prenatal flood exposure. To the extent that women were exposed to greater hardships from flood exposure during pregnancy, they not only had higher levels of depressive symptoms, but also lower levels of well-being up to 2½ years later. Further, peritraumatic distress (i.e., transient reactions to trauma exposure such as intrusive thoughts and hyperarousal) was identified as a significant mediator of the link between severity of flood exposure and depression. That is, the internal psychological reactions that some women recalled experiencing—directly in response to exposures to highly stressful circumstances during pregnancy—were largely responsible for elevated depressive symptoms during the perinatal period.
The results of the present study were consistent with findings observed in a subsample of women who had enrolled in the Iowa Flood Study and were in committed, intimate relationships (Brock et al., 2014). Stress from the flood was associated with greater depression for partnered women; however, this effect was minimized to the extent that these women reported more frequent support from their partners. In the present study, we showed the detrimental impact of flood exposure on maternal mental health in a larger, more generalizable sample of women, and identified a potential mechanism explaining the link between objective levels of flood exposure and maternal depression: peritraumatic distress.
In addition to depressive symptoms, we examined the impact of flood exposure on maternal well-being, a related dimension of maternal mental health that should be routinely considered along with perinatal depression. Results suggest that prenatal flood exposure not only puts perinatal women at risk for higher levels of depression, but also diminished well-being. Whereas peritraumatic distress explained the link between flood exposure and depression, it was not associated with well-being (i.e., bivariate correlations were small in magnitude and only significant during pregnancy). This finding highlights that although depression is associated with low levels of positive affect and vitality (Watson, Clark, & Stasik, 2011), unique mechanisms appear to contribute to these related, yet distinct dimensions of maternal mental health. Other aspects of natural disaster exposure, aspects not related to subjective distress, may contribute to well-being (e.g., restricted access to naturally reinforcing and rewarding aspects of one’s environment), and should be explored in future research.
The present study had limitations. First, the sample consisted primarily of White, high SES women, who reported relatively low levels of prior trauma, limiting the generalizability of our findings. Nonetheless, we expect more vulnerable populations to demonstrate stronger associations among flood exposure, peritraumatic distress, and mental health outcomes. Second, causal conclusions cannot be drawn due to the correlational nature of the study; however, testing our hypotheses in the context of a natural disaster was a strength of the present study. Because of the sporadic onset of natural disasters, their independence from individual influence, and the lack of correlation between psychosocial variables and severity of exposure (r < .20), prenatal stress was quasirandomly assigned to women during pregnancy reducing potential confounds. Further, we were able to capture multiple types and varying degrees of stress, including forms of stress that are likely to elicit traumatic responses. Third, although there are multiple advantages to using dimensional measures of psychopathology (e.g., they are ideally suited for community samples with low rates of diagnosable psychopathology), diagnostic measures would have provided additional, clinically relevant information.
Finally, although women were sent the IF100 and PDI immediately after they enrolled in the flood study, women varied with regard to when they completed those measures relative to the peak of flooding; this may have contributed to reporter bias (e.g., less accurate reports by women who reported on hardships and distress after a prolonged interval). Nonetheless, degree of delay in responding, following the peak of flooding, was not associated with IF100 (r = −.02) or PDI (r = .05) scores. Further, when including timing of those assessments as a control variable in the analyses, the same pattern of results emerged. It is also noteworthy that women with higher levels of depression may have retrospectively reported greater hardship and peritraumatic distress, potentially inflating associations among the study variables.
Results of the present study suggested that exposure to a natural disaster during pregnancy has pervasive and enduring effects on the mental health of women, not only increasing risk for depression, but also diminished positive affect and well-being for several years after childbirth. To the extent that women were exposed to greater degrees of flood hardship during pregnancy, a cascade was triggered such that women were also more likely to experience peritraumatic distress, which in turn increased the risk for depression across the perinatal period. For the first time of which we are aware, our finding demonstrates the unique role of peritraumatic distress in depression, and high-lights the importance of considering subjective reactions to prenatal stress in research aimed at explaining the developmental course of maternal depression. Further, the enduring impact of flood exposure on maternal depression and well-being—up to 30 months after childbirth—is particularly notable given that children are especially susceptible to the effects of maternal depression during toddlerhood (e.g., Davies & Sturge-Apple, 2007).
The present study also had implications for informing interventions aimed at preventing and treating perinatal depression by identifying potential treatment targets and priorities. Results identified a mechanism that could be targeted in interventions implemented immediately after exposure to traumatic stress. For example, interventions might include psychoeducation about the nature of traumatic stress (to detect early signs of trauma), training in coping skills, and guidance about how to best solicit external coping resources such as social support. Additionally, closely monitoring women’s psychological reactions to stress may be important. Indeed, the PDI—used to assess peritraumatic distress in the present study—is a useful screening tool for identifying at-risk individuals following exposure to traumatic events (Guardia et al., 2013). Guardia et al. (2013) suggest that individuals with PDI scores exceeding 28 (≈ 5% of this sample) should receive immediate care and follow-up, and those with scores between 7 and 28 (60% of this sample) should be monitored over time. Future research is needed to clarify what mitigates the deleterious effects of peritraumatic distress on psychopathology (e.g., by testing comprehensive moderated mediation models) to identify treatment targets and priorities.
Acknowledgments
This research was supported by grants from NIMH (MH086150) to Michael W. O’Hara and the Canadian Institutes of Health Research (MOP-93660) to Suzanne King. Although data from this sample have been published elsewhere (e.g., Brock et al., 2014; Nylen, O’Hara, & Engeldinger, 2012), this is the first publication to include an examination of the mechanisms linking flood exposure to multiple dimensions of maternal mental health.
Footnotes
Rebecca L. Brock is now at the Department of Psychology, University of Nebraska-Lincoln. Kimberly J. Hart is now at the Department of Psychiatry, University of Iowa. Chunbo Yu is now at Government of Alberta, Canada.
References
- Almeida CP, Cunha FF, Pires EP, Sá E. Common mental disorders in pregnancy in the context of interpartner violence. Journal of Psychiatric and Mental Health Nursing. 2013;20:419–425. doi: 10.1111/j.1365-2850.2012.01937.x. doi:10.1111/j.1365-2850.2012.01937.x. [DOI] [PubMed] [Google Scholar]
- Beck CT. Predictors of postpartum depression. Nursing Research. 2001;50:275–285. doi: 10.1097/00006199-200109000-00004. doi:10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Brock RL, Hara MW, Hart KJ, McCabe JE, Williamson JA, Laplante DP, King S, et al. Partner support and maternal depression in the context of the Iowa floods. Journal of Family Psychology. 2014;28:832–843. doi: 10.1037/fam0000027. doi:10.1037/fam0000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet A, Sanche S, Manetti A, Aouizerate B, Ribeéreau-Gayon R, Charpentier S, Arbus C, et al. Peritraumatic distress but not dissociation predicts posttraumatic stress disorder in the elderly. International Psychogeriatrics. 2013;25:1007–1012. doi: 10.1017/S1041610213000069. doi:10.1017/S1041610213000069. [DOI] [PubMed] [Google Scholar]
- Brunet A, Weiss DS, Metzler TJ, Best SR, Neylan TC, Rogers C, Marmar CR, et al. The peritraumatic distress inventory: A proposed measure of PTSD criterion A2. The American Journal of Psychiatry. 2001;158:1480–1485. doi: 10.1176/appi.ajp.158.9.1480. doi:10.1176/appi.ajp.158.9.1480. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. Journal of Abnormal Psychology. 2009;118:405–411. doi: 10.1037/a0015370. doi:10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple M. Advances in the formulation of emotional security theory: An ethologically based perspective. Advances in Child Development and Behavior. 2007;35:87–137. doi: 10.1016/b978-0-12-009735-7.50008-6. doi:10.1016/B978-0-12-009735-7.50008-6. [DOI] [PubMed] [Google Scholar]
- Delahaije D, Dirksen CD, Peeters LL, Smits LJ. Anxiety and depression following preeclampsia or hemolysis, elevated liver enzymes, and low platelets syndrome. A systematic review. Acta Obstetricia et Gynecologica. 2013;92:746–761. doi: 10.1111/aogs.12175. doi:10.1111/aogs.12175. [DOI] [PubMed] [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the quality of life inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. doi:10.1037//1040-3590.4.1.92. [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. doi:10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. doi:10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Archives of Women’s Mental Health. 2003;6:263–274. doi: 10.1007/s00737-003-0024-6. doi:10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- Guardia D, Brunet A, Duhamel A, Ducrocq F, Demarty A, Vaiva G. Prediction of trauma-related disorders: A proposed cutoff score for the Peritraumatic Distress Inventory. The Primary Care Companion to CNS Disorders. 2013;15 doi: 10.4088/PCC.12l01406. doi:10.4088/PCC.12l01406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gump BB, Reihman J, Stewart P, Lonky E, Darvill T, Granger DA, Matthews KA. Trajectories of maternal depressive symptoms over her child’s life span: Relation to adrenocortical, cardiovascular, and emotional functioning in children. Development and Psychopathology. 2009;21:207–225. doi: 10.1017/S0954579409000133. doi:10.1017/S0954579409000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargrave PA, Leathem JM, Long NR. Peritraumatic distress: Its relationship to posttraumatic stress and complicated grief symptoms in sudden death survivors. Journal of Traumatic Stress. 2012;25:344–347. doi: 10.1002/jts.21703. doi:10.1002/jts.21703. [DOI] [PubMed] [Google Scholar]
- Howard L, Oram S, Galley H, Trevillion K, Feder G. Domestic violence and perinatal mental disorders: A systematic review and meta-analysis. PLOS Medicine. 2013;10:1–16. doi: 10.1371/journal.pmed.1001452. doi:10.1371/journal.pmed. 1001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, Aksan N, Prisco TR, Adams EE. Mother–child and father–child mutually responsive orientation in the first 2 years and children’s outcomes at preschool age: Mechanisms of influence. Child Development. 2008;79:30–44. doi: 10.1111/j.1467-8624.2007.01109.x. doi:10.1111/j.1467-8624.2007.01109.x. [DOI] [PubMed] [Google Scholar]
- Laplante DP, Zelazo PR, Brunet A, King S. Functional play at 2 years of age: Effects of prenatal maternal stress. Infancy. 2007;12:69–93. doi: 10.1111/j.1532-7078.2007.tb00234.x. doi:10.1111/j.1532-7078.2007.tb00234.x. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. doi:10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. doi:10.1207/s15327906mbr3901 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane A. Relationship between psychiatric impairment and a natural disaster: The role of distress. Psychological Medicine. 1988;18:129–139. doi: 10.1017/s0033291700001963. doi:10.1017/S0033291700001963. [DOI] [PubMed] [Google Scholar]
- Norris FH. Disaster research methods: Past progress and future directions. Journal of Traumatic Stress. 2006;19:173–184. doi: 10.1002/jts.20109. doi:10.1002/jts.20109. [DOI] [PubMed] [Google Scholar]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. 2002;65:207–239. doi: 10.1521/psyc.65.3.207.20173. doi:10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- Nylen KJ, Hara MW, Engeldinger J. Perceived social support interacts with prenatal depression to predict birth outcomes. Journal of Behavioral Medicine. 2012;36:427–440. doi: 10.1007/s10865-012-9436-y. doi:10.1007/s10865-012-9436-y. [DOI] [PubMed] [Google Scholar]
- Hara MW, McCabe JE. Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. doi:10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Swain A. Rates and risk of postpartum depression-a meta-analysis. International Review of Psychiatry. 1996;8:37–54. doi:10.3109/09540269609037816. [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. doi:10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Qu Z, Wang X, Tian D, Zhao Y, Zhang Q, He H, Guo S. Posttraumatic stress disorder and depression among new mothers at 8 months later of the 2008 Sichuan earthquake in China. Archives of Women’s Mental Health. 2012;15:49–55. doi: 10.1007/s00737-011-0255-x. doi:10.1007/s00737-011-0255-x. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, et al. Comparing personal trajectories and drawing causal inferences from longitudinal data. Annual Review of Psychology. 2001;52:501–525. doi: 10.1146/annurev.psych.52.1.501. doi:10.1146/annurev.psych.52.1.501. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Rodgers RF, Franko DL, Brunet A, Herbert CF, Bui E. Disordered eating following exposure to television and Internet coverage of the March 2011 Japan earthquake. International Journal of Eating Disorders. 2012;45:845–849. doi: 10.1002/eat.22031. doi:10.1002/eat.22031. [DOI] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects. 2008 [Computer Software]. Available from http://quantpsy.org/ [Google Scholar]
- Thomas É, Saumier D, Brunet A. Peritraumatic distress and the course of posttraumatic stress disorder symptoms: A meta-analysis. Canadian Journal of Psychiatry. 2012;57:122–129. doi: 10.1177/070674371205700209. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Stasik SM. Emotions and the emotional disorders: A quantitative hierarchical perspective. International Journal of Clinical and Health Psychology. 2011;11:429–442. [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Stuart S, et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19:253–268. doi: 10.1037/1040-3590.19.3.253. doi:10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Young E, Abelson J, Curtis G, Nesse R. Childhood adversity and vulnerability to mood and anxiety disorders. Depression and Anxiety. 1997;72:66–72. doi:10.1002/(SICI)1520-6394(1997)5:2<66::AID-DA2>3.0.CO;2-3. [PubMed] [Google Scholar]
- Zhang Z, Zyphur MJ, Preacher KJ. Testing multilevel mediation using hierarchical linear models: Problems and solutions. Organizational Research Methods. 2008;12:695–719. doi:10.1177/1094428108327450. [Google Scholar]