Abstract
Background
Ichthyosis linearis circumflexa is a rare form of ichthyosis characterized by polycyclic and annular lesions which are bordered by a double-edged scale. Netherton syndrome is a genodermatosis in which ichthyosis linearis circumflexa is accompanied by characteristic hair shaft abnormalities and atopic diathesis. Different treatment modalities such as emmolients, keratolytics, calcipotriene, topical corticosteroids, topical calcineurin inhibitors, systemic retinoids, phototherapy and photochemotherapy have been used with variable results. Topical therapies may result in considerable absorption because of the defective barrier function in ichthyosis linearis circumflexa/Netherton syndrome.
Main observation
A 12-year-old patient diagnosed as ichthyosis linearis circumflexa demonstrated considerable improvement with narrowband UVB phototherapy at the end of 30 sessions.
Conclusion
Short-term narrowband-UVB may an effective treatment option in patients with ichthyosis linearis circumflexa/Netherton syndrome.
Keywords: ichthyosis, Netherton syndrome, phototherapy, treatment, trichorrhexis invaginata, UV
Introduction
Ichthyosis linearis circumflexa is a rare, autosomal recessive disorder of keratinization characterized by annular and polycyclic lesions with double-edged scales. Netherton syndrome is characterized by a triad of ichthyosis, hair shaft abnormalities and atopic diathesis.[1] Different treatment modalities have been tried with variable results in the management of this genodermatosis.[2] Here, we describe a case of ichthyosis linearis circumflexa which showed significant improvement with narrowband (NB) UVB treatment.
Case Report
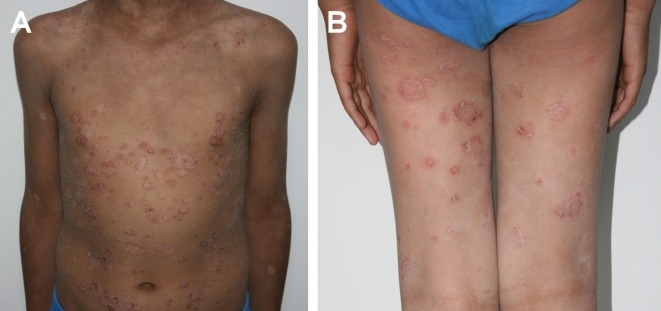
A 12-year-old Caucasian male presented for evaluation of a long standing skin condition characterized by dry, red and scaling skin. The eruption had appeared on the face as erythema and scaling at the age of one month and it had spread to the trunk and extremities during the following year. The patient had not benefited from emollients and topical corticosteroids. His brother was healthy, the parents were nonconsanguineous and there was no personal or family history of atopy. On dermatological examination, widespread erythematous, annular, polycyclic and double-edged papulosquamous plaques were detected on the trunk and extremities [Fig. 1A,B]. On the face, there was a mild, diffuse erythema with slight scaling. Oral mucosa, hair, nails, and other systemic examination were normal. Microscopic examination of the hair was normal. Biopsy revealed parakeratosis, hypogranulosis, psoriasiform acanthosis, vacuolar changes in the basal layer as well as intraepidermal neutrophilic infiltrates; mild perivascular inflammatory cell infiltration was also present in the dermis. Serum biochemistries, IgE levels and complete blood count were within reference intervals.
Figure 1.
(A,B) Widespread, erythematous, polycyclic, scaly eruption with double-edged scales.
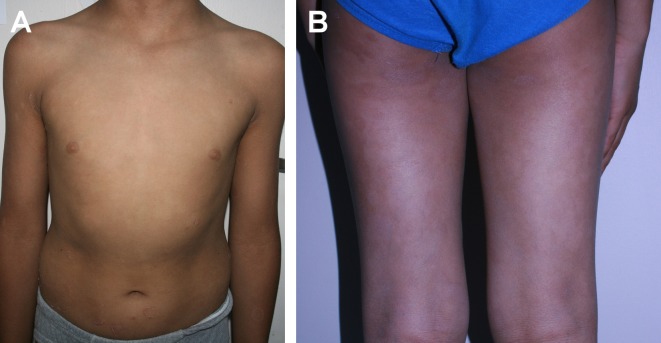
A diagnosis of ichthyosis linearis circumflexa was established based on the clinical and histopathological findings. A trial of NB UVB three times a week was initiated at 0,50 J/cm2 after obtaining consent from his parents. Significant improvement was observed after amild flare-up which ocurred at the 20th session [Fig. 2A,B]. The majority of lesions cleared after 30 sessions with a cumulative dose of 54.7 J/cm2. The treatment was well tolerated and the patient remained in remission for five months after discontinuation of phototherapy.
Figure 2.
(A,B) Clinical improvement of skin lesions after phototherapy.
Discussion
Netherton syndrome is an autosomal recessive disorder characterized by ichthyosis linearis circumflexa, atopic diathesis and hair shaft abnormalities such as trichorrhexis invaginata.[1] The disease develops as a result of a mutation in the SPINK5, the gene that encodes lymphoepithelial Kazaltype- related inhibitor (LEKTI), located to chromosome 5q32. LEKTI is a new type of serine protease inhibitor with antitrypsin activity. Mutations in SPINK5 result in a loss of LEKTI activity and, thus, to premature and uncontrolled proteolytic activity of serine proteases, leading to skin barier dysfunction.[1,3]
Various treatment modalities such as emmolients, keratolytics, calcipotriene, topical corticosteroids, topical calcineurin inhibitors, systemic retinoids, phototherapy and photochemotherapy have been used in the management of this disorder.[1,2] Because of the defective barrier function, topical therapies may result in considerable absorption in Netherton syndrome. Cushing syndrome has been reported as a consequence of widespead application of topical corticosteroids.[1,2,4] Significant absorption of tacrolimus was also reported; therefore blood tacrolimus levels should be monitored in patients with Netherton syndrome.[5] Systemic retinoids have exhibited variable responses in this disorder; some patients have demonstrated improvement whereas flares have been noted in others.[1,2]
PUVA, UVA1 and balneophototherapy have been reported to be effective in the management of the disorder.[6-9] We could find two case reports of Netherton syndrome treated with NB UVB: One of these patients had received phototherapy for eight months while the other patient had been treated for more than four years and both had demonstrated complete response.[2,4] Given our patient’s age and the potential carcinogenicity of NB UVB, we administered 30 sessions and observed significant improvement in the lesions. The exact mechanism of action of phototherapy in this condition is unknown, but it has been proposed that phototherapy may enhance the synthesis of other serine protease inhibitors that compensate the activity of the defective LEKTI function. Additionally, phototherapy may be effective through its immunomodulatory and apoptosis inducing effects on keratinocytes, dendritic cells, mast cells and T-lymphocytes.[8,9]
Conclusion
NB UVB is an effective and well-tolerated treatment option in the management of ILC/Netherton syndrome. NB UVB phototherapy can be considered a rational approach with regard to the side effects of topical therapies and the variable results obtained from systemic retinoids in the management of this disorder.
References
- Richard G, Ringpfeil F. Ichthyoses, Erythrokeratodermas and Related Disorders. In: Dermatology (Jorizzo JL, Bolognia JL, Schaffer JV, eds), 3rd edn, Vol.1. Elsevier Saunders Company; 2012. pp. 837–870. [Google Scholar]
- Maatouk I, Moutran R, Tomb R. Narrowband ultraviolet B phototherapy associated with improvement in Netherton syndrome. Clin Exp Dermatol. 2012;37:364–366. doi: 10.1111/j.1365-2230.2011.04231.x. [DOI] [PubMed] [Google Scholar]
- Chavanas S, Bodemer C, Rochat A, Hamel-Teillac D, Ali M, Irvine AD, Bonafé JL, Wilkinson J, Taïeb A, Barrandon Y, Harper JI, de Prost Y, Hovnanian A. Mutations in SPINK5, encoding a serine protease inhibitor cause Netherton syndrome. Nat Genet. 2000;25:141–142. doi: 10.1038/75977. [DOI] [PubMed] [Google Scholar]
- Kaminska EC, Ortel B, Sharma V, Stein SL. Narrowband UVB phototherapy as a novel treatment for Netherton syndrome. Photodermatol Photoimmunol Photomed. 2012;28:162–164. doi: 10.1111/j.1600-0781.2012.00655.x. [DOI] [PubMed] [Google Scholar]
- Allen A, Siegfried E, Silverman R, Williams ML, Elias PM, Szabo SK, Korman NJ. Significant absorption of topical tacrolimus in 3 patients with Netherton syndrome. Arch Dermatol. 2001;137:747–750. [PubMed] [Google Scholar]
- Manabe M, Yoshiike T, Negi M, Ogawa H. Successful therapy of ichthyosis linearis circumflexa with PUVA. J Am Acad Dermatol. 1983;8:905–907. doi: 10.1016/s0190-9622(83)80032-2. [DOI] [PubMed] [Google Scholar]
- Gambichler T, Senger E, Altmeyer P, Hoffmann K. Clearence of ichthyosis linearis circumflexa with balneophototherapy. J Eur Acad Dermatol Venerol. 2000;14:397–399. doi: 10.1046/j.1468-3083.2000.00116.x. [DOI] [PubMed] [Google Scholar]
- Capezzera R, Venturini M, Bianchi D, Zane C, Calzavara-Pinton P. UVA1 phototherapy of Netherton syndrome. Acta Derm Venereol. 2004;84:69–70. doi: 10.1080/00015550310015437. [DOI] [PubMed] [Google Scholar]
- Osmola-Mankowska A, Silny W, Danczak-Pazdrovska A, Bowszyc-Dmochowska M, Olek-Hrab K, Sadowska-Przytocka A, Czarnecka-Operacz M. A case of a Comél-Netherton syndrome patient treated with UVA1 phototherapy. Post Dermatol Alergol. 2011;XXVIII, 5:418–421. [Google Scholar]