Abstract
Objective
Prior research has suggested that competing neurobehavioral decision-making processes might affect health outcomes among traumatized populations. Regulatory imbalances to impulsive and executive decision systems are affected by high levels of stress, including stress resulting from traumatic events. Such regulatory imbalances have been associated with addictive behaviors. However, it is not well known whether addictive behavior increases or decreases the likelihood of utilization of behavioral health services among traumatized populations. The aim of this study is to systematically review mental health utilization studies targeting traumatized populations to determine the direction of association between substance use and behavioral health utilization.
Method
Databases of literature were searched in a systematic manner, and 37 relevant studies were recovered and analyzed.
Findings
Out of the 37 relevant studies that included addictive behaviors as a predictor of utilization, 16 showed a positive significant relationship and 6 showed a negative significant relationship. Studies showing a negative significant relationship used younger samples with more recent trauma exposure.
Conclusions
Studies have shown that for the most part, substance abuse increases the likelihood of utilization, except among younger populations with more recent trauma. Longitudinal studies that access how utilization evolves over time among traumatized populations and interacts with posttraumatic stress disorder (PTSD) and substance abuse severity are necessary to better understand how decision-making processes of traumatized individuals may increase the likelihood of chronic PTSD.
Keywords: mental health utilization, systematic review, substance use, trauma
Approximately 61% of men and 51% of women are exposed to a traumatic event at least once during their lifetimes (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Meanwhile, a number of empirically supported treatments are available for traumatized populations (Kearns, Ressler, Zatzick, & Rothbaum, 2012); however, only around 49% actually access treatment (Wang et al., 2005). Some scholars have suggested that areas of the brain that control executive activities may be exhausted by the stress of traumatic events, which can lead to problems with decision making, irritability, impulsivity, and apathy (Manuck, Flory, Muldoon, & Ferrell, 2014). This might explain why many traumatized individuals either do not seek mental health services, delay services for long periods of time, or engage in high levels of substance use and abuse during mental health service utilization (Stewart, Pihl, Conrad, & Dougier, 1998).
Recent studies have shown that cognitive-behavioral interventions administered within 9 months of exposure may provide a window of opportunity that can prevent the development of chronic posttraumatic stress disorder (PTSD; Kearns et al., 2012). Such interventions are effective because they reduce pathological anxiety by activating fear memory and providing corrective information. However, studies have also suggested that when individuals engage in addictive behaviors after exposure to trauma, they will discount at much higher rates (i.e., assign greater value to short-term rewards even if long-term rewards are substantially larger) and thus will be more likely to delay behaviors that could require some effort to improve long-term rewards (such as help seeking; MacKillop et al., 2011). In addition, addictive behavior can increase anxiety and arousal and reduce traumatized individuals' ability to manage emotions or process traumatic material (Kaysen et al., 2011; Stewart et al., 1998). Therefore, it is necessary to better understand the role of substance use, abuse, and dependence when it comes to behavioral health care utilization among traumatized populations. In this study, we conduct a systematic review of studies of help seeking by traumatized populations to better understand whether substance use, abuse, and dependence increase or decrease the likelihood of behavioral health care utilization and follow-up.
Studies of behavioral health utilization commonly use some variation of Andersen's (1995) help seeking model. This model is commonly used to conceptualize factors leading to behavioral healthcare utilization and includes individual or predisposing factors (e.g., demographics, attitudes), need characteristics (e.g., perceived need or health status), and structured factors or enabling characteristics (e.g., ability to pay, availability of providers). Substance use and dependence is typically regarded as a need variable in these studies (Gelberg, Anderson, & Leake, 2000). This is likely because substance use co-occurs with a variety of different mental health disorders.
However, research related to the relationship between substance use and the development of PTSD has suggested alternative explanations for understanding behavioral health utilization (Jacobsen, Southwick, & Kosten, 2001). Although studies generally show high levels of co-morbidity between PTSD and substance use, they also show that there are different pathways leading to both PTSD and substance use. The first pathway starts with substance abuse and ends later in PTSD. This pattern has been observed mostly among users of illicit substances, such as cocaine, because they repeatedly place themselves in dangerous situations (Brady, Dansky, Sonne, & Saladen, 1998). Chronic substance abuse also can lead to higher levels of arousal, anxiety, and sensitization of neurobiological stress symptoms (Piazza & Aiozerate, 2002), which can also increase risk for PTSD. In the second pathway, PTSD precedes substance abuse. This pathway is often explained using the self-medication hypothesis, which states that individuals use substances as a way to treat symptoms of mental disorders (Khantzian, 1997). Studies have shown that traumatized individuals have used alcohol, cannabis, opioids, and benzodiazepine to both deal with traumatic experiences and to alleviate symptoms of PTSD (Carter & Capone, 2011). These traumatized individuals report that the escalation of substance abuse and PTSD were entwined (Jacobsen et al., 2001). As these individuals attempt to withdrawal from substance use, physiological arousal prompts them to relapse back into patterns of self-medication.
Increased use of substances has also been explained by what have been referred to as competing neurobehavioral decision systems (i.e., competing regions of the brain that control decision making; Bickel, Jarmolowicz, Mueller, Gatchalian, & McClure, 2012). These regions can become dysregulated by stressors like trauma. When these regions are dysregulated, individuals have lowered capacity to inhibit impulses and thus are more likely to discount more readily. Thus, when given a choice between addictive substances (which will make them feel good in the short term) and mental health utilization (which will make them feel good in the long term), they are more likely to choose the former, especially when the trauma stressor is more recent.
Studies show that the second pathway to PTSD is much more common (i.e. PTSD leads to higher substance use; Jacobsen et al., 2001; Carter & Capone, 2011), and thus models of help seeking that incorporate aspects of behavioral economics, such as the health belief model (which examines how individuals calculate costs vs. benefits of help seeking; Wolinsky, 2014) and the culturally specific choice-making model (which examines the effect of alternative [or substitute] treatments on the utilization of mainstream treatments; Young, 1981), may help fill this gap. However, it still remains poorly understood whether traumatized individuals are choosing substance use over utilization or if substance use motivates utilization. It is also unclear how recency of trauma exposure could affect substance use and utilization patterns. The aim of this review is to identify whether, and under what circumstances, individuals choose substance use over utilization or whether, and under what circumstances, substance use motivates utilization.
Methods
Search Strategy
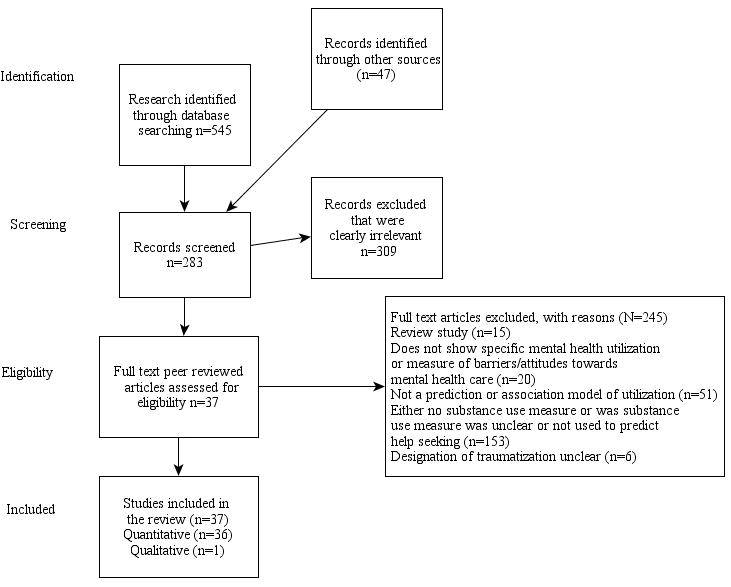
A four-step search strategy was used to obtain peer-reviewed papers. First, we searched databases (Academic Search Premier, Article First, JSTOR, Project Muse, Scopus, Web of Science, Psychinfo, Cinahl, Social Science Research Network, Socindex, Applied Social Sciences Index and Abstract, Social Work Abstracts, Social Service Abstracts, International Bibliography of Social Sciences, Academic Search Complete, PubMed, PILOTS, and Psychiatry Online) using the following keywords: “help seeking,” “utilization,” “Post Traumatic Stress Disorder” or “PTSD,” “trauma,” “violence,” “victim,” “crime,” “combat,” “rape,” and “war.” In addition, when available, we also filtered for “behavioral health” or “mental health.” Review studies were located through database searches and were also reviewed to identify articles that may have been missed through electronic databases (Brewin, Andrews, & Valentine, 2000; Gavrilovic, Schutzwohl, Fazel, & Priebe, 2005; Gourash, 1978; McCart, Smith, & Sawyer, 2011; Norris, Kaniasty, & Scheer, 1990; Sabrina & Tindale, 2008; Selkirk, Quayle, & Rothwell, 2014; Suffoletta-Maierle, Grubaugh, Magruder, Monnier, & Frueh, 2003; Ullman, 2007). As Figure 1 shows, after removing duplicate studies, we analyzed abstracts of all studies identified and excluded papers that did not satisfy the first tier of our search criteria (whether studies specifically examined help seeking behavior or utilized traumatized populations). Third, we analyzed the full-text versions of all remaining studies, excluding those that (a) did not provide a specific measure of mental health service utilization, attitudes, or perceived barriers to utilization; (b) did not either provide a measure predicting utilization or the association between utilization and other variables; (c) contained no substance use measure or contained a substance use measure that was either unclear or that was not used to predict help seeking; and (d) had an unclear stratification of the traumatized population. Out of 592 articles identified through search databases and review studies as potentially relevant, 283 were given full-text reviews, 37 of which fulfilled inclusion criteria.
Figure 1. Search approach.
Results
Overall, 20 studies showed a positive relationship between substance use and utilization, 11 studies showed a negative relationship between substance use and utilization, and 6 studies showed mixed results. Twenty-two of the 37 studies showed a statistically significant relationship between substance use and utilization.
All but three studies used U.S. populations. In total, the 37 studies employed 922,196 participants, and an average of 57% per study utilized mental health services (4 studies did not provide prevalence rates of utilization), whereas 29% per study reported some type of substance use issue (including hazardous alcohol use, substance abuse, and substance dependence; 8 studies did not provide prevalence rates on substance use problems). The majority of studies utilized male populations (87% overall; 63% per study). Of the 29 studies utilizing military populations, 904,147 participants experienced possible combat (approximately 88% of this group was male overall).1 There were 162,200 participants in the five studies on natural disaster and war (89% male overall) and 10,295 participants in the five studies on female physical/sexual assault victims (including domestic and sexual violence). One remaining study, which used a more general trauma history screen, included 100 participants who were recently incarcerated.
Recruitment Methods and Study Designs
About half (n = 18) of the studies relied on a clinical sample supplied by the Veterans Administration (VA). These studies either utilized a survey which was administered during intake at a VA service provider (n=7) or utilized Veteran Health Administration (VHA) patient registries (n=11). The rest used a mixture of random sampling methodology (n = 12), administrative rosters or registration lists (n = 3), and convenience samples (n = 4). For studies using random sampling methodologies or administrative rosters, response rates varied from 27% to 77% (mean 55%). Studies utilizing randomized designs generally involved about 60% military and 40% civilian populations and included the following methods to improve external validity: use of stratified probability sampling by geographic location, demographics, military characteristics, etc. (n=5); random digit dialing or random selection from an administrative roster (n=5); face-to-face interviews (n=2); and sampling weights (n=7). Studies utilizing administrative rosters only included military populations. These studies examined differences between responders and nonresponders when random sampling was not used. Differences were found between these groups in terms of age and level of education. Studies utilizing convenience samples typically recruited participants via flyer, newspaper ads and via staff. Twenty-three of the 38 studies utilized cross-sectional designs and the rest utilized longitudinal designs occurring over 6 months or more. In all cases where a longitudinal design was utilized, researchers accessed patient registries via the VA.
Measure of Mental Health Utilization
The majority of studies focused on whether individuals utilized mental health services (25 studies). Mental health services included professional and nonprofessional mental health services offered by community-based providers (including religious organizations), hospitals, and military providers (VA, Department of Defense). Other studies focused on treatment engagement (n = 4), treatment preference (n = 1), treatment delay (n = 2), perceived need for services (n = 2), and barriers to care (including unmet need and stigma; n = 3).
Measure of Substance Use
Studies typically either measured substance abuse as a whole or alcohol use, with two studies excepted: one that focused on drug abuse and alcoholism (Owens, Rogers, & Whitesell, 2011) and the other that used Diagnostic and Statistical Manual of Mental Disorders (DSM–IV; American Psychiatric Association, 2000) measures of substance abuse and binge drinking (Amstadter, McCauley, Ruggiero, Resnick, & Kilpatrick, 2008). Otherwise, studies varied significantly when it came to measures of substance use. Because so many studies utilized VA data, the most commonly used measure was a VA administrative ICD code that essentially combines all levels of substance use problems into one category (11 studies). A DSM–IV measure of substance abuse or dependence (5 studies) and the Cut down, Annoyed, Guilty, and Eye-opener (CAGE) score (to identify alcoholism in six studies; Kitchens, 1994) were the next most commonly used measures, followed by the Alcohol Use Disorders Identification Test (AUDIT), (4 studies; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), then measures of increased drinking (n = 4) and other types of measures Addiction Severity Index (ASI), Short Michigan Alcohol Screening Test (SMAST), Drug Abuse Screening Test (DAST), and (ASI, SMAST, DAST, and the World Mental Health Composite International Diagnostic Interview (WMH-CIDI), n = 5. No study differentiated between individuals according to trajectories of use, abuse, and dependence. As expected, clinical samples did, however, have a slightly higher prevalence of substance use issues (31%, using either International Classification of Diseases ICD code or CAGE score, compared to 27%, using a variety of measures, including increased drinking) in convenience, random, and roster samples.
Length of Time of Traumatization
About half of the studies (n = 13) either did not assess the amount of time in which the person was traumatized (e.g., used a lifetime measure) or utilized a sample where time of trauma exposure could not be determined. For some populations, the start of events (e.g., the conflicts in Iraq and Afghanistan) did provide information about the timing of traumatization, as studies were typically conducted within 5 years of the start of conflicts in Iraq and Afghanistan. Studies of Vietnam veterans took place 8 or more years after the Vietnam War (1975). Studies using natural disaster/exposure, such as 9/11 or hurricane exposure, typically took place within 3 years of the event. Although rates of utilization were similar regardless of recency of trauma, prevalence rates of substance use issues were slightly lower for those with more recent trauma (within past 5 years; 25%) than for those with less recent trauma (lifetime measure or more than 5 years ago; 31%).
Statistics
Twenty-two of the studies shown in Table 1 (in order by sample size) identified substance abuse as significantly associated with treatment seeking. We also include studies that do not show significant findings to give the reader a more balanced picture of the evidence. Studies applied bivariate, multivariate, or both methods to determine the relationship between substance use issues and help seeking.
Table 1. Studies That Met Inclusion Criteria (n = 37) and Whether Substance Use Had a Positive or Negative Relationship With Mental Health Utilization, Engagement, or Attitudes.
| Study name | Sample size | % Male | Trauma type | Recruitment | Prevalence help seekingb | Relationshipa |
|---|---|---|---|---|---|---|
| Maguen et al. (2012) | 314,717 | 88% | Combat | Clinical | 86% | P |
| Rotem and Rosenheck (2011) | 204,184 | 93% | Combat | Clinical | 88% | M |
| Frahm et al. (2013) | 153,511 | 92% | Disaster/war | Clinical | NA | N |
| Hundt et al. (2014) | 130,331 | 88% | Combat | Clinical | 100% | P |
| Chermack et al. (2008) | 41,412 | 91% | Combat | Clinical | 75% | P |
| Ilgen et al. (2012) | 16,892 | 97% | Combat | Clinical | 100% | P |
| Iversen et al. (2011) | 10,272 | NA | Combat | Clinical | NA | N |
| Sareen et al. (2010) | 8,441 | 85% | Combat | Random | 23% | P |
| Lipsky and Caetano (2007) | 7,924 | 0% | Domestic violence | Random | 19% | N |
| Ford et al. (2006) | 4,640 | 47% | Disaster/war | Random | 32% | M |
| Rosenheck and Fontana (2003) | 4,000 | NA | Disaster/war | Clinical | 36% | N |
| Washington et al. (2013) | 3,598 | 0% | Combat | Random | 49% | M |
| Elbogen et al. (2013) | 2,937 | 67% | Combat | Random | 26% | N |
| Tsan et al. (2012) | 2,470 | 86% | Combat | Clinical | 42% | P |
| Boscarino et al. (2004) | 2,368 | 47% | Disaster/war | Random | 12% | P |
| Hoff and Rosenheck (1998) | 2,348 | 69% | Combat | Random | 63% | P |
| Kulka et al. (1990) | 2,330 | 69% | Combat | Random | 63% | P |
| Fortuna et al. (2008) | 1,630 | 52% | Political violence | Random | 29% | P |
| Hankin et al. (1999) | 1,061 | 100% | Combat | Clinical | 68% | P |
| DiLeone et al. (2013) | 1,040 | 49% | Combat | Roster | 56% | N |
| Lu et al. (2011) | 869 | 89% | Combat | Clinical | 100% | P |
| Starzynkski et al. (2007) | 780 | 0% | Sexual violence | Clinical | 53% | N |
| Naragon-Gainey et al. (2012) | 618 | 91% | Combat | Clinical | 100% | N |
| Amstadter et al. (2008) | 556 | 0% | Sexual violence | Random | 60% | P |
| Bosworth et al. (2000) | 526 | 0% | Sexual violence | Clinical | 60% | P |
| Erbes et al. (2007) | 521 | 86% | Combat | Clinical | 62% | N |
| Decker et al. (2013) | 509 | 0% | Sexual violence | Clinical | NA | P |
| Wenzel et al. (1995) | 429 | 100% | Combat | Clinical | 37% | P |
| Pietrzak et al. (2009) | 272 | NA | Combat | Roster | 26% | N |
| Whealin et al. (2014) | 233 | 89% | Combat | Random | 36% | P |
| DeViva (2014) | 200 | 92% | Combat | Clinical | 38% | M |
| Harpaz-Rotem et al. (2014) | 167 | 96% | Combat | Clinical | 100% | P |
| Erbes et al. (2009) | 161 | 98% | Combat | Clinical | 100% | N |
| Owens et al. (2011) | 100 | 52% | Mixed | Convenience | 54% | P |
| Tucker et al. (2002) | 51 | 69% | Disaster/war | Roster | 14% | P |
| Owens et al. (2009) | 50 | 0% | Combat | Convenience | 58% | M |
| Gibbs et al. (2011) | 48 | NA | Combat | Convenience | NA | M |
Note. Studies are organized in order by sample size. NA = data not available. Italics indicate significant at p < .05.
Help seeking includes all forms of utilization of formal behavioral health services. Prevalence of 100% indicates that the dependent variable was treatment engagement.
P = positive; N = negative; M = mixed/unclear.
Positive versus negative versus mixed associations between substances use issues and help seeking
Of the 37 studies, 20 studies showed a positive relationship, 11 studies showed a negative relationship, and 6 studies showed mixed results. All but one of the studies showing a negative relationship between substance use and help seeking, utilized populations who had been traumatized within the past 5 years (7 of which experienced trauma recently or within the past year). Meanwhile, only 8 of the 20 studies showing a positive relationship utilized participants with trauma exposure within the past 5 years (see Table 2). Studies showed similar use of either substance or alcohol use disorders and virtually equal prevalence of males and females; and substance use issues (when these data were available). Studies also equally depended on clinical data, regardless of positive or negative relationship among studies reporting this item. Among samples who potentially were exposed to combat, 13 studies showed a positive relationship, 7 studies showed a negative relationship and 5 studies showed a mixed relationship. Four of the 6 studies focused on disaster, war and political violence showed a negative relationship (the remaining 2 showed a positive relationship. All studies of sexual violence (100% female samples) showed a positive relationship between substance use and mental health utilization. Random sampling was also used equally, regardless of negative or positive relationship. However, studies showing a negative relationship were slightly more likely to use younger samples (median age = 33 years vs. 44 years) and more likely to use bivariate statistical methods (54% vs. 30%), have a lower median sample size (median = 1,040 vs. 1,345), and have a lower average response rate (52% vs. 58%).
Table 2. Qualities of the Studies Showing Positive and Negative Relationships Between Substance Use and Measures of Mental Health Utilization (n=31).
| Positive relationship shown | Negative relationship shown | |
|---|---|---|
| Studies | Maguen et al. (2012); Hundt et al. (2014), Chermack et al. (2008), Ilgen et al. (2012); Sareen et al. (2010); Tsan et al. (2012); Hoff et al. (1998); Kulka et al. (1990); Hanken et al. (1999); Lu et al. (2011); Amstadter et al. (2008); Bosworth et al. (2006); Decker et al. (2013); Wenzel et al. (1995); Whealin et al. (2014); Owens et al. (2010); Tucker et al. (2010); Rotem et al. (2014); Boscarino et al. (2004); Fortuna et al. (2008) | Frahm et al. (2013); Iverson et al. (2011); Lipsky and Caetano (2007); Rosenheck and Fontana (2003); Elbogen et al. (2013); Erbes et al. (2009); Pietzak et al. (2009); DiLeone et al. (2013); Starzinsky et al. (2007); Gainey et al. (2012); Erbes et al. (2007) |
| Substance use, n | ||
| ICD code mixed substance abuse/dependence | 8 | 3 |
| DSM criteria: abuse | 1 | |
| DSM criteria: dependence/CAGE | 5 | 3 |
| AUDIT/increased drinking | 2 | 4 |
| Other measure (CIDI, Assist, alcohol to intoxication) | 4 | 1 |
| Average prevalence substance use/abuse/dependence,a % | 26 | 30 |
| Age,b years | ||
| Mean | 42 | 35 |
| Median | 44 | 33 |
| Length of time from traumatic event | ||
| Lifetime/ever | 9 | 1 |
| More than 5 years | 3 | |
| Within 5 years | 8 | 9 |
Missing: positive, 2; negative, 4.
Missing: positive; 2, negative, 2.
Studies showing mixed results are described in Table 3. Studies in this category typically showed that substance use increased the likelihood of utilization in some areas (such as the number of mental health visits) but not in others (such as treatment completion; DeViva, 2014; Harpaz-Rotem & Rosenheck, 2011). There were also differences depending on how substance use was measured (Ford, Adams, & Dailey, 2006), and sometimes differences between those engaging in substance use and those not were just too small to be considered either positive or negative (e.g., when p < .95). The qualitative study by Gibbs, Rae Olmsted, Brown, and Clinton-Sherrod (2011) was also considered under this category because there was no way of definitively assessing how alcohol use affected mental health utilization. However, the study did show how alcohol was used during early stages of trauma; that is, when members of the military have trouble accessing care (most often because of waiting lists and stigma), they substitute with use of alcohol. When alcohol use reaches a certain level of severity, these members often are forced into treatment, which thereby increases utilization rates.
Table 3. Studies Showing Mixed Findings in Regard to the Role of Substance Use (n=6).
| Study | Type of trauma | Recruitment | Sample size | Details |
|---|---|---|---|---|
| Rotem et al. (2011) | Combat | Clinical | 204,184 | Proportional hazard assessing risk of dropping out for an alcohol or drug use disorder in first year is significant at .004 and .001, respectively. However, respondents with alcohol or drug disorders were also significantly more likely to have more mental health visits in the first year after diagnosis. |
| Ford et al. (2006) | Disaster/war | Random | 4,640 | Bivariate: Individuals who were current drinkers were significantly less likely to utilize behavioral health services. However, individuals who increased either smoking or drinking were significantly more likely to utilize behavioral health services. Multivariate: Positive relationship (nonsignificant) between current drinker or smoker or increase in alcohol or tobacco use. |
| Washington et al. (2012) | Combat | Random | 3,598 | Bivariate difference too slight, p = .97. |
| DeViva et al. (2014) | Combat | Clinical | 200 | Those with comorbid substance abuse were likely to be seen but less likely to complete treatment; results were nonsignificant. |
| Owens et al. (2009) | Combat | Convenience | 50 | Bivariate differences too small; mean SMAST score = 3.12 (SD = 2.39) vs. mean SMAST score = 3.05 (SD = 1.39). |
| Gibbs et al. (2011) | Combat | Convenience | 48 | (Qualitative study) Reported use of “self-medication” after returning from deployment and as a way of coping with general conditions of military life and separation from family and friends. For some participants, alcohol was used as “self-medication” when there were too many barriers to care—wait times, stigma, career problems. However, when alcohol use went out of control, individuals usually were sanctioned by the military and forced to seek treatment. |
Findings from subgroups of studies with statistically significant results
Twenty-two out of the 37 studies showed a significant relationship between substance use issues and help seeking. Almost three times as many studies (n = 16 of 37) showed a positive significant relationship than a negative significant relationship (n = 6 of 37). However, studies showing a negative significant relationship were more likely to utilize samples with more recent trauma (within the past 5 years) than studies showing a positive significant relationship. Although studies showing negative results relied on younger samples (median age = 33 years vs. 44 years), studies showing a positive significant relationship showed higher rates of mental health service utilization (59% vs. 29%). Rates of substance use issues and use of substance use measures (alcohol vs. substance as a group) as well as use of clinical versus other types of samples were the same or similar regardless of direction of association. Median sample size was also slightly higher among studies showing a negative significant relationship (median = 4,320 vs. 1,696), as was average response rate (66% vs. 56%).
Discussion
The search yielded only 37 studies (out of a total of 283 where either utilization or other measures of mental health services utilization or utilization propensity were assessed), which would suggest that there is enough evidence is available to establish rigorous conclusions on the role of substance use in help seeking among traumatized populations. However, several methodological problems, including stratification by group, by time and type of trauma, different measurements of substance use, differences in substance use severity by population, and low response rates among nonclinical populations, made it difficult to compare findings from different studies. Furthermore, many studies utilized clinical samples that may have contained more severely symptomatic participants than general populations. Those studies utilizing clinical samples were the only studies to track mental health utilization over time. Nevertheless, some interesting inferences about the role of substance use on help seeking may be drawn from this review.
It appears that, for the most part, substance use issues increase the likelihood that traumatized populations will utilize mental health services, will not delay mental health services, and will feel that they have more of a need for mental health services. However, it appears that this can depend heavily on the age of the sample, the gender of the sample and the type of trauma endured and the time in which trauma occurs: Recently traumatized males (of all trauma types) and females experiencing trauma that is not interpersonal seem to be less likely to utilize services (or delay service use or have more negative attitudes about service utilization) if they are engaging in a higher level of substance use. Meanwhile, both females who experience interpersonal trauma and individuals who experienced trauma after the 5-year threshold appear to be more likely to utilize mental health services if they also have a substance use issue. Studies examining the onset of PTSD and drug use outcomes have also shown conflicting findings likely because of different measures of drug use (e.g., drug use vs. drug abuse/dependence),differences in age (e.g., early adulthood vs. late adulthood; Chilcoat & Breslau, 1998), differences in types and amount of trauma exposure (Tolin & Foa, 2006) and gender differences (Olff, et al., 2007).
Becker and Murphy's (1988) theory of rational addiction may help explain these findings. According to this model, limited resources, such as time, emotional energy, and money, are governed by individual choice processes where individuals seek to maximize lifetime utility function (a function measuring future well-being). Individuals are rational in that they consider future effects of current consumption. Younger populations may have less experience with the consequences of substance use and also do not have the knowledge about whether they have a tendency to develop a substance use problem (Leigh, 2002). Women, on the other hand, might be more likely to experiences consequences of substance use after a short period of time (See Greenfield et al., 2007) while individuals in the military might be encouraged to use alcohol to cope with the stresses of combat and PTSD as part of military culture (See Ames & Cunradi, 2004). A type of contrasting effect may occur under these circumstances (i.e., traumatized individuals' perceptions and judgments of behavioral health services or substances are based on earlier experiences; Simonsohn, 2006).
Taking into account the preferences of traumatized “consumers” of mental health services from a menu of other commodities available to improve their well-being under differing constraints would significantly improve prevention efforts. These preferences may include preference for substance use over mental health utilization. Some of the constraints may be more obvious, such as those posed on military populations, for example, military culture, accessibility of alcohol, and systematic barriers such as waiting lists (Ames & Cunradi, 2004). Under the current VA system, the majority of resources are allocated to individuals with severe problems (through service-connected disability status; Department of Veteran Affairs, 2013), which might create enough constraints to influence decision-making processes of traumatized veterans. Among civilian populations, mental health resources are also disproportionately consumed by those with severe mental health problems via emergency department use and hospitalization (Culhane & Metraux, 2008).
More systematic resources need to be available to support increased early utilization besides just traditional social norms campaigns. Behavioral economic approaches such as working memory training (training to improve individual decision-making processes by improving the ability to manipulate accurate representations of the contextual environment to achieve current goals) and episodic future thinking (training that teaches individuals to project representations of self into plausible future scenarios), along with already existing motivational interviewing techniques, may be useful approaches during this short window. These approaches are cost effective and help improve individuals' ability to make better long term decisions and decrease substance use (Bickel, Quisenberry, Moody, & Wilson, 2014).
Studies by Frahm et al. (2013) and Rosenheck and Fontana (2003) also showed how traumatic events can trigger help seeking among individuals with past-trauma exposure, except when those individuals have ongoing substance use problems. For such individuals, easily accessible mutual aid self-help groups need to be made available over long periods of time so that they can engage them easily as they move through different periods of increased and decreased risk. Such interventions should also focus on clients' post-treatment environment and how this environment can trigger substance abuse (Vuchinich & Heather, 2003). The challenge is therefore how to make services more appealing and accessible when traumatized individuals have just experienced trauma. Although a large number of studies have examined traumatized consumers' attitudes about treatment, one limitation of these studies is that they do not assess attitudes of trauma services among populations who were actively engaging in addictive behaviors.
This study is one of a few that systematically reviews the role of trauma and addictive behavior on behavioral health care utilization. The study is limited, however, for several reasons. First, our findings, drawn heavily from U.S. military and veteran samples, may not be generalizable to nonmilitary traumatized populations or individuals outside the United States. Studies utilizing military populations were often longitudinal but also relied heavily on VA patient registries, which typically contain patients with higher levels of mental illness and comorbidity than community samples, because the VA prioritizes veterans who have been injured through combat-related activities (Department of Veteran Affairs, 2013). Thus, substance use more likely reflects need in these populations, according to Anderson's model, because substance abuse typically is correlated with severe mental illness (Jacobson, et al., 2001). These individuals are also overwhelmingly male and have access to very different service delivery systems and types of services than civilian females who are more likely to experience sexual or domestic violence (Tolin & Foa, 2006). Many of the studies that relied on random samples, also, had low response rates (average 55%), which might have also biased results. Studies utilizing surveys also rarely showed whether there were differences between responders and nonresponders and when they did, significant differences were found in gender and education, factors that are highly correlated with help seeking (Gavrilovic, et al., 2005). Third, studies were also limited when it came to measurement, that is, they did not distinguish present substance use from past substance abuse or dependence. This made it difficult to make clear conclusions about the role of present substance use on utilization. Last, we cannot definitively conclude that a negative association between substance use and mental health utilization necessarily implies impulsive decision making; additional tests that assess whether individuals discount delayed benefits when they have been exposed to recent trauma are needed to make more solid conclusions.
Future studies using longitudinal models with large nationally representative samples that contain a diverse mix of traumatized populations as well as precise information about current substance use patterns, impulsivity, and likelihood of discounting long-term health outcomes are necessary to confirm the role of substance use, abuse, and dependence in behavioral health care utilization patterns. Such studies have the potential to apply behavioral economic principles to service utilization and therefore more effectively define and clarify how addiction changes at various points of contact with service providers.
Acknowledgments
Funding. This study was funded by the National Institutes of Drug Abuse research training grant T32DA007313. Funding sources had no further role in study design, collection, analysis and interpretation of data, writing of this manuscript, or the decision to submit the manuscript for publication.
Footnotes
There is likely overlap among observations in VA administrative data. However, the extent of overlap is unknown because studies accessed VA data from differing regions and populations. This number represents the total number of participants stated by these studies.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington DC: Author; 2000. [Google Scholar]
- Ames G, Cunradi C. Alcohol use and preventing alcohol-related problems among young adults in the military. Alcohol Research & Health. 2004;28:252–257. [Google Scholar]
- Amstadter AB, McCauley JL, Ruggiero KJ, Resnick HS, Kilpatrick DG. Service utilization and help seeking in a national sample of female rape victims. Psychriatric Services. 2008;59:1450–1457. doi: 10.1176/appi.ps.59.12.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Babor T, Higgins-Biddle J, Saunders J, Monteiro M. AUDIT: The alcohol use disorders identification test: guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- Becker G, Murphy K. A theory of rational addiction. Journal of Political Economy. 1988;96:675–700. [Google Scholar]
- Bickel W, Jarmolowicz D, Mueller E, Gatchalian K, McClure S. Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology. 2012;221:361–387. doi: 10.1007/s00213-012-2689-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel W, Quisenberry A, Moody L, Wilson A. Therapuetic opportunities for self-control repair in addiction and related disorders: Change and the limits of change in trans-disease processes. Clinical Psychological Science. 2014:1–14. doi: 10.1177/2167702614541260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick HS, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatric Services. 2004;55:274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- Bosworth H, Parsey K, Butterfield M. Racial variations kin wanting and needing mental health services among women veterans in a primary care clinic. Journal of National Medical Association. 2000;92:231–236. [PMC free article] [PubMed] [Google Scholar]
- Brady K, Dansky B, Sonne S, Saladen M. PTSD and cocaine dependence. American Journal of Addiction. 1998;7:128–135. [PubMed] [Google Scholar]
- Brewin C, Andrews B, Valentine J. Meta-analysis of risk factors for post-traumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Carter A, Capone C. Co-occuring PTSD and alcohol use disorder in the Veteran population. Journal of Dual Diagnosis. 2011;7:285–299. doi: 10.1080/15504263.2011.620453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Zivin K, Valenstein MM, Ilgen MA, Austin KL, Wryobeck J, et al. The prevalence and predictors of mental health treatment services in a national sample of depressed veterans. Medical Care. 2008;46:813–820. doi: 10.1097/MLR.0b013e318178eb08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat H, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addictive Behaviors. 1998;23:827–840. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Culhane DP, Metraux S. Rearranging the deck chairs or reallocating the lifeboats? Homelessness assistance and its alternatives. Journal of the American Planning Association. 2008;74(1):111–121. [Google Scholar]
- Decker SE, Rosenheck RA, Tsai J, Hoff R, Harpaz-Rotem I. Military sexual assault and homeless women veterans: Clinical correlates and treatment preferences. Women's Health Issues. 2013;23:373–380. doi: 10.1016/j.whi.2013.09.002. [DOI] [PubMed] [Google Scholar]
- Department of Veteran Affairs. Federal benefits for veterans. Washington DC: Author; 2013. [Google Scholar]
- DeViva J. Treatment utilization among OEF/OIF veterans referred for psychotherapy for PTSD. Psychological Services. 2014;11:179–185. doi: 10.1037/a0035077. [DOI] [PubMed] [Google Scholar]
- DiLeone B, Gradus J, Giasson H, Vogt D, Street A, Resick P. Predictors of mental health care use among male and female veterans deployed in support of the wars in Afghanistan and Iraq. Psychological Services. 2013;10:145–151. doi: 10.1037/a0032088. [DOI] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, et al. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatric Services. 2013;64:134–141. doi: 10.1176/appi.ps.004792011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbes C, Curry KT, Leskela J. Treatment presentation and adherence of Iraq/Afghanistan era veterans in outpatient care for PTSD. Psychological Services. 2009;6:175–183. [Google Scholar]
- Erbes C, Westmeyer J, Engdahl B, Johnson E. PTSD and service utilization in a sample of service members from Iraq and Afghanistan. Military Medicine. 2007;172:359–363. doi: 10.7205/milmed.172.4.359. [DOI] [PubMed] [Google Scholar]
- Ford J, Adams M, Dailey W. Factors associated with receiving help and risk factors for disaster-related distress among Connecticut adults 5–15 months after the September 11th terrorist incidents. Social Psychiatry Psychiatric Epidemiology. 2006;41:261–270. doi: 10.1007/s00127-006-0031-9. [DOI] [PubMed] [Google Scholar]
- Fortuna LR, Porche MV, Alegria M. Political violence, psychosocial trauma, and the context of mental health services use among immigrant Latinos in the United States. Ethnicity & Health. 2008;13:435–463. doi: 10.1080/13557850701837286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frahm KA, Barnett SD, Brown LM, Hickling EJ, Olney R, Campbell RR, et al. Posttraumatic stress disorder and use of psychiatric and alcohol related services: The effect of the 2004–2005 Florida hurricane seasons on veterans. Community Mental Health Journal. 2013;49:636–642. doi: 10.1007/s10597-012-9558-2. [DOI] [PubMed] [Google Scholar]
- Gavrilovic JJ, Schutzwohl M, Fazel M, Priebe S. Who seeks treatment after a traumatic event and who does not? A review of findings on mental health service utilization. Journal of Trauma and Stress. 2005;18:595–605. doi: 10.1002/jts.20068. [DOI] [PubMed] [Google Scholar]
- Gelberg L, Anderson R, Leake B. The behavioral model for vulnerable populations: Applications to medical care use and outcomes for homeless people. Health Services Research. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- Gibbs DA, Rae Olmsted KL, Brown JM, Clinton-Sherrod AM. Dynamics of stigma for alcohol and mental health treatment among army soldiers. Military Psychology. 2011;23:36–51. [Google Scholar]
- Gourash N. Help seeking: A review of the literature. Journal of Community Psychology. 1978;6:413–424. doi: 10.1007/BF00941418. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RR, Lincoln M, Hien D, Mielc GM. Treatment entry, retention and outcomes in women: A review of the literature. Drug and Alcohol Dependence. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin CS, Spiro A, Miller DR, Kazis LE. Mental disorders and mental health treatment among U.S. Department of Veterans Affairs outpatients: The Veterans Health Study. American Journal of Psychiatry. 1999;156:1924–1930. doi: 10.1176/ajp.156.12.1924. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Rosenheck RA. Serving those who served: Retention of newly returning veterans from Iraq and Afghanistan in mental health treatment. Psychiatric Services. 2011;62:22–27. doi: 10.1176/ps.62.1.pss6201_0022. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Rosenheck RA, Pietrzak RH, Southwick SM. Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan veterans. The Journal of Nervous and Mental Disease. 2014;202:97–104. doi: 10.1097/NMD.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Hoff R, Rosenheck R. The use of VA and non-VA mental health services by female veterans. Medical Care. 1998;36:1114–1119. doi: 10.1097/00005650-199811000-00002. [DOI] [PubMed] [Google Scholar]
- Hundt N, Barrera T, Mott J, Mignogna J, Hong-Jen Y, Shubhada S, et al. Predisposing, enabling, and need factors as predictors of low and high psychotherapy utilization in veterans. Psychological Services. 2014;3:1–9. doi: 10.1037/a0036907. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Conner KR, Roeder KM, Blow FC, Austin KL, Valenstein MM. Patterns of treatment utilization before suicide among male veterans with substance use disorders. American Journal of Public Health. 2012;102:88–92. doi: 10.2105/AJPH.2011.300392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen AC, Van Staden L, Hacker Hughes JG, Greenberg N, Hotopf M, Rona RJ, et al. The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Services Research. 2011;11:31. doi: 10.1186/1472-6963-11-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen I, Southwick S, Kosten T. Substance use disorders in patients with PTSD: A review of the literature. American Journal of Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Atkins D, Moore S, Lindgren K, Dillworth T, Simpson T. Alcohol use, problems and the course of PTSD: A prospective study of female crime victims. Journal of Dual Diagnosis. 2011;7:262–276. doi: 10.1080/15504263.2011.620449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearns M, Ressler K, Zatzick D, Rothbaum B. Early intervientions for PTSD: A review. Depression & Anxiety. 2012;29:833–842. doi: 10.1002/da.21997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Khantzian E. The self medication hypothesis of substance use disorders: A reconsideration and recent appliations. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kitchens J. Does this patient have an alcohol problem? JAMA. 1994;272:1782–1787. [PubMed] [Google Scholar]
- Kulka R, Schlenger W, Fairbank J, Hough R, Jordan B, Marmar C, et al. Trauma and the Vietnam War generation. New York, NY: Brunner/Mazel; 1990. [Google Scholar]
- Leigh B. Peril, chance, adventure: Concepts of risk, alcohol use and risky behavior in young adults. Addiction. 2002;94:371–383. doi: 10.1046/j.1360-0443.1999.9433717.x. [DOI] [PubMed] [Google Scholar]
- Lipsky S, Caetano R. Impact of intimate partner violence on unmet need for mental health care: Results from the NSDUH. Psychiatric Services. 2007;58:822–829. doi: 10.1176/ps.2007.58.6.822. [DOI] [PubMed] [Google Scholar]
- Lu MW, Duckart JP, O'Malley JP, Dobscha SK. Correlates of utilization of PTSD specialty treatment among recently diagnosed veterans at the VA. Psychiatric Services. 2011;62:943–949. doi: 10.1176/ps.62.8.pss6208_0943. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Amlung M, Few L, Ray L, Sweet L, Munafo M. Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology. 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguen S, Madden E, Cohen BE, Bertenthal D, Seal KH. Time to treatment among veterans of conflicts in Iraq and Afghanistan with psychiatric diagnoses. Psychiatric Services. 2012;63:1206–1212. doi: 10.1176/appi.ps.201200051. [DOI] [PubMed] [Google Scholar]
- Manuck S, Flory J, Muldoon M, Ferrell R. A neurobiology of intertemporal choice. In: Loewenstein G, Read D, Baumeister R, editors. Time and decision. New York, NY: Russell Sage Foundation; 2014. pp. 139–174. [Google Scholar]
- McCart M, Smith D, Sawyer G. Help seeking among victims of crime: A review of the empirical literature. Journal of Traumatic Stress. 2011;23:198–206. doi: 10.1002/jts.20509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K, Hoerster KD, Malte CA, Jakupcak M. Distress symptoms and high-risk behaviors prospectively associated with treatment use among returning veterans. Psychiatric Services. 2012;63:942–944. doi: 10.1176/appi.ps.201100349. [DOI] [PubMed] [Google Scholar]
- Norris FH, Kaniasty KZ, Scheer DA. Use of mental health services among victims of crime: Frequency, correlates, and subsequent recovery. Journal of Consulting and Clinical Psychology. 1990;58:538–547. doi: 10.1037//0022-006x.58.5.538. [DOI] [PubMed] [Google Scholar]
- Olff M, Draijer N, Langeland W, Gersons BP. Gender differences in PTSD. Psychological Bulletin. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Owens GP, Herrera CJ, Whitesell AA. A preliminary investigation of mental health needs and barriers to mental health care for female veterans of Iraq and Afghanistan. Traumatology. 2009;15:31–37. [Google Scholar]
- Owens GP, Rogers SM, Whitesell AA. Use of mental health services and barriers to care for individuals on probation or parole. Journal of Offender Rehabilitation. 2011;50:37–47. [Google Scholar]
- Piazza P, Aiozerate B. Endocrinology of drug dependence. In: D'Haenen H, den Boer J, editors. Biological Psychiatry. NY: Wiley Online Library; 2002. pp. 425–434. [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric Services. 2009;60:1118–1122. doi: 10.1176/ps.2009.60.8.1118. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Fontana A. Use of mental health services by veterans with PTSD after the terrorist attacks of September 11. American Journal of Psychiatry. 2003;160:1684–1690. doi: 10.1176/appi.ajp.160.9.1684. [DOI] [PubMed] [Google Scholar]
- Sabrina C, Tindale R. Abuse characteristics and coping resources as predictors of problem-focused coping strategies among battered women. Violence Against Women. 2008;14:437–456. doi: 10.1177/1077801208314831. [DOI] [PubMed] [Google Scholar]
- Sareen J, Belik SL, Stein MB, Asmundson GJG. Correlates of perceived need for mental health care among active military personnel. Psychiatric Services. 2010;61:50–57. doi: 10.1176/ps.2010.61.1.50. [DOI] [PubMed] [Google Scholar]
- Selkirk M, Quayle E, Rothwell N. A systematic review of factors affecting migrant attitudes toward seeking psychological help. Journal of Health Care for the Poor and Underserved. 2014;25:94–127. doi: 10.1353/hpu.2014.0026. [DOI] [PubMed] [Google Scholar]
- Simonsohn U. New Yorkers commute more everywhere: Contrast effects in the field. Review of Economics and Statistics. 2006;88:1–9. [Google Scholar]
- Starzynkski L, Ullman S, Townsend S, Long L, Long S. What factors predict women's disclosure of sexual assault to mental health professionals? Journal of Community Psychology. 2007;35:619–638. [Google Scholar]
- Stewart S, Pihl R, Conrad P, Dougier M. Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors. 1998;23:797–812. doi: 10.1016/s0306-4603(98)00070-7. [DOI] [PubMed] [Google Scholar]
- Suffoletta-Maierle S, Grubaugh AL, Magruder K, Monnier J, Frueh BC. Trauma-related mental health needs and service utilization among female veterans. Journal of Psychiatric Practice. 2003;9:367–375. doi: 10.1097/00131746-200309000-00005. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and PTSD: a quantitative review of 25 years of research. Psychological Bulletin. 2006;132(2):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Tsan JY, Zeber JE, Stock EM, Sun F, Copeland LA. Primary care mental health integration and treatment retention among Iraq and Afghanistan war veterans. Psychological Services. 2012;9:336–348. doi: 10.1037/a0028308. [DOI] [PubMed] [Google Scholar]
- Tucker P, Pfefferbaum B, Jordan F, Doughty D, Jones D, Nixon S. Body handlers after terrorism in Oklahoma City: Predictors of posttraumatic stress and other symptoms. Journal of Orthopsychiatry. 2002;72:469–475. doi: 10.1037/0002-9432.72.4.469. [DOI] [PubMed] [Google Scholar]
- Ullman SE. Mental health services seeking in sexual assault victims. Women and Therapy. 2007;30:61–84. [Google Scholar]
- Vuchinich R, Heather N. Choice behavioral economics and addiction. Oxford, England: Elsevier; 2003. [Google Scholar]
- Wang P, Lane M, Olfson M, Pincus H, Wells K, Kessler R. Twelve-month use of mental health services in the US. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Washington DL, Davis TD, Der-Martirosian C, Yano EM. PTSD risk and mental health care engagement in a multi-war era community sample of women veterans. Journal of Internal General Medicine. 2013;28:894–900. doi: 10.1007/s11606-012-2303-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel SL, Bakhtiar L, Caskey NH, Hardie E. Homeless veterans' utilization of medical, psychiatric, and substance abuse services. Medical Care. 1995;33:1132–1144. doi: 10.1097/00005650-199511000-00006. [DOI] [PubMed] [Google Scholar]
- Whealin JM, Stotzer RL, Pietrzak RH, Vogt D, Shore J, Morland L, et al. Deployment-related sequelae and treatment utilization in rural and urban war veterans in Hawaii. Psychological Services. 2014;11:114–123. doi: 10.1037/a0032782. [DOI] [PubMed] [Google Scholar]
- Wolinsky F. The sociology of health. Belmont, CA: Wadsworth; 2014. The sick role concept; pp. 101–116. [Google Scholar]
- Young J. Medical choice in a Mexican village. New Brunswick, NJ: Rutgers University Press; 1981. [Google Scholar]


