Abstract
Objective
Studying physiologic underpinnings of loss-of-control (LOC) eating may inform its etiology and contribute to intervention efforts. We therefore examined temporal relationships between autonomic indices (heart rate (HR), heart rate variability (HRV)) and LOC-eating in the natural environment.
Method
For two days, adolescents (n=17, 14.77±1.55 years, BMI-Z 2.17±0.48) with LOC-eating reported on LOC using an electronic device while HR and HRV were assessed continuously using Holter monitoring.
Results
Higher HR and lower HRV in the 30-minutes before eating were significantly associated with LOC-eating overall (p’s < 0.001) and at the within-subjects level (p’s < 0.001), but not at the between-subjects level (p’s > 0.44). Examined categorically, HR was significantly higher, and HRV significantly lower, prior to high-LOC compared to low-LOC episodes (p’s < 0.001).
Discussion
This pilot study suggests that LOC-eating may involve physiologic underpinnings. Additional research with larger samples is needed to further investigate this phenomenon.
Keywords: LOC-eating, adolescence, heart rate, heart rate variability
Loss-of-control (LOC) eating, defined as the subjective feeling of being unable to stop eating or control what or how much one is eating, is commonly reported by community youth, with estimates ranging from 6 – 40% (1), and the highest rates observed among overweight adolescent girls (2). Predictive of excess weight gain, partial or full-syndrome binge eating disorder (BED), and depressive and anxiety symptoms (3–6), LOC-eating warrants investigation and requires intervention efforts. In particular, identifying triggers of LOC-eating in the natural environment has potential for improving LOC interventions.
Key existing LOC etiologic models hypothesize that stress and negative emotions play a role in LOC-eating (7–9). Although emotions are thought to reflect an interplay between cognitive processes (e.g. self-reported “feelings”), physiologic changes, and behavior (10), most existing investigations of predictors of LOC-eating have focused on self-report constructs (11–13). Because investigating self-reported affective states is limited by participants’ ability to know and report emotions, studying physiologic indices is warranted.
Prior investigations of physiologic indices and disordered eating have examined associations at the trait-level and in response to food cues. Women with binge eating (14) and bulimia nervosa (15) experience greater heart rate increases in response to food cues. Among obese women with BED, greater cardiovascular reactivity to a psychological stressor was associated with post-stress hunger ratings (16), suggesting that physiologic stress may play a role in subsequent eating behavior.
To date, no study has examined momentary associations between cardiovascular indices (heart rate (HR) and heart rate variability (HRV)), thought to be indicative of stress (17–19), and LOC-eating. Therefore, we aimed to collect pilot data examining associations between pre-meal HR and HRV and subsequent LOC-eating. We hypothesized that HR would be positively associated, and HRV inversely associated, with LOC.
METHOD
Participants
Seventeen adolescents participating in a pilot study of the utility of ecological momentary assessment (EMA) for examining interpersonal, affective, and physiologic predictors of LOC-eating were studied. Outcome data pertaining to self-report predictors of LOC-eating are published (13). Participants were English-speaking, adolescent (12-17 y) females with a body mass index (BMI; kg/m2) at or above the 85th percentile (20) who reported at least two LOC episodes during the month prior to assessment, determined using the Eating Disorder Examination (EDE) version 14.0-Interview (21). Exclusion criteria were major medical (e.g. diabetes) or psychiatric illness (e.g. major depressive disorder), use of medications affecting eating/body weight (e.g. antipsychotic class), and pregnancy. The study was approved by the Uniformed Services University of the Health Sciences (USUHS) institutional review board. Parents/guardians and adolescents provided written consent and assent, respectively.
Procedure
Participants attended a baseline screening visit during which height, fasting weight and body composition, and eating-related and general psychopathology were assessed. Adolescents practiced completing EMA recordings for one day to ensure familiarity with procedures and subsequently engaged in EMA for two weeks. Except during school, girls completed signal-contingent recordings distributed around target times of 11:10, 13:50, 16:30, 19:10, and 23:50 and event-contingent recordings before and after eating. Four items pertaining to LOC (e.g. “Did you feel a sense of loss of control?”), adapted from the EDE (21), were rated on a 5-point Likert-type scale after eating. Posture (“reclining;” “sitting;” “standing still;” “walking”) was queried at each recording.
For two days, adolescents wore a 12-lead, 9-channel Mortara H12 Holter monitor to measure HR and HRV. Data were sampled at a frequency of 1000 Hz (22). Generated ECG recordings were manually screened for clinically-relevant abnormalities and analyzed using a MATLAB-based program (23). High-frequency HRV was derived as power amplitude in the spectrum between 0.15-0.40 Hz generated by a fast-Fourier transformation. RMSSD (root mean square of successive differences), pNN50 (proportion of beat-to-beat intervals differing by >50 milliseconds), and HF HRV (high-frequency HRV) constituted indices of parasympathetically-mediated HRV as recommended (10, 22).
Data Analyses
Consistent with prior studies of HRV and eating (24, 25), physiologic indices were evaluated in the 30-minute period preceding the eating episode start time (before-meal recording). Loss-of-control was assessed after the eating episode. For after-meal LOC ratings with absent (5/40) or implausible (≤ 2 minutes before the after-meal recording, 8/40) before-meal recordings, the eating episode start time was considered to occur 28:37 minutes before the after-meal recording, based upon mean replacement with the average latency between corresponding before and after-meal recordings. Findings did not differ when analyses were restricted to episodes with a valid before-meal recording. To reduce confounding, episodes occurring within three hours of the previous episode were excluded. To evaluate LOC, a composite score comprising the average rating on three LOC items was calculated. One item (“Did it feel like you were able to stop eating?”) was excluded to improve internal reliability (13).
Three sets of analyses were performed. First, separate linear mixed models (LMM) predicting LOC from HR and HRV were conducted. Second, to parse between- versus within- subjects variability, LMM including participants’ mean (mean-centered) for each independent variable, as well as the difference between the participant’s mean and each observation, were conducted. Third, exploratory LMM were used to categorically examine the association between episode type (high-LOC versus low-LOC based on median split) and physiologic variables. All models included a random (subject-specific) intercept and a variance components correlation structure. Covariates tested included age and adiposity at the between-subjects level and before-meal posture and time of day (00:00-5:59; 6:00-11:59; 12:00-17:59; 18:00-23:59) at the within-subjects level. Posture was considered missing for eating episodes with absent/implausible before-meal recordings; when analyses were restricted to episodes with available before-meal recordings, findings were unchanged.
RESULTS
Sample and response rate
Adolescents’ baseline characteristics are reported in supplementary table 1. Out of 49 eating episodes, 40 were included in analyses. Six were excluded because the episode occurred within three hours of a previous episode; three were excluded due to noisy/missing physiologic data. Slightly less than half (40-42%) of physiologic data were collected on weekends. Eighty percent of episodes occurred between 12:00 – 23:59.
Heart rate
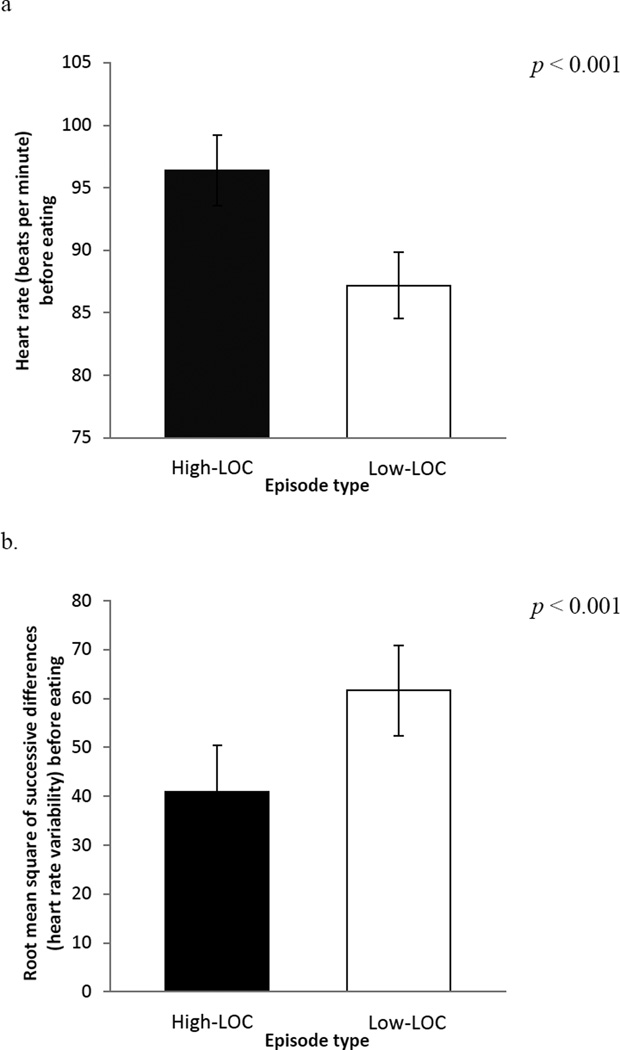
Controlling for posture, greater HR predicted increased LOC (estimate = 0.019, SE = 0.004, p < 0.001, ΔR2 = 0.12, Table 1a). The within (estimate = 0.019, SE = 0.004, p < 0.001), but not between (p = 0.44), -subjects level effect was also significant. Examined categorically, HR was higher prior to high-LOC (96.40±2.84 beats per minute (bpm)) compared to low-LOC (87.20±2.63 bpm, p < 0.001, Figure 1a) episodes.
Table 1.
Results from linear mixed models predicting level of LOC-eating from (a) heart rate (b) root mean square of successive differences (RMSSD), controlling for posture category
| (a) | ||||
|---|---|---|---|---|
| Estimate | Standard Error | t Statistic | significance | |
| Intercept | −0.487 | 0.424 | −1.149 | 0.253 |
| Heart rate | 0.019 | 0.004 | 4.608 | <0.001 |
| Posture | ||||
| missing* | 1.037 | 0.216 | 4.807 | <0.001 |
| walking | 0.140 | 0.225 | 0.620 | 0.536 |
| standing still | 0.913 | 0.247 | 3.699 | <0.001 |
| sitting | 0.437 | 0.181 | 2.409 | 0.017 |
| reclining | reference | - | - | - |
| (b) | ||||
|---|---|---|---|---|
| Estimate | Standard Error | t Statistic | significance | |
| Intercept | 1.679 | 0.251 | 6.693 | <0.001 |
| RMSSD | −0.009 | 0.002 | −4.860 | <0.001 |
| Posture | ||||
| missing* | 1.137 | 0.214 | 5.315 | <0.001 |
| walking | 0.112 | 0.224 | 0.499 | 0.618 |
| standing still | 0.852 | 0.246 | 3.471 | 0.001 |
| sitting | 0.434 | 0.180 | 2.412 | 0.017 |
| reclining | reference | - | - | - |
Posture rating was coded “missing” for eating episodes that did not have a valid “before meal” recording and results did not differ when these episodes (k = 13) were excluded
Figure 1.
Mean measured (a) heart rate and (b) root mean square of successive differences (heart rate variability) prior to eating for high- and low- loss-of-control (LOC) episodes
Heart rate variability
Findings were similar for RMSSD, pNN50 and HF HRV and therefore RMSSD is presented. Controlling for posture, lower HRV was associated with higher LOC (estimate = -0.009, SE = 0.002, p < 0.001, ΔR2 = 0.14, Table 1b). The within-subjects level effect for RMSSD was significant (estimate = -0.010, SE = 0.002, p < 0.001), and the between-subjects level effect was not (p = 0.36). Examined categorically, RMSSD was significantly lower prior to high- (41.04±9.40) compared to low- (61.66±9.21, p < 0.001) LOC episodes (Figure 1b).
DISCUSSION
In an initial investigation of physiological underpinnings of LOC-eating, we analyzed the associations between HR and HRV and LOC-eating in the natural environment in adolescent girls with recurrent LOC. Preliminary findings revealed significant associations between physiologic parameters and LOC overall and at the within-subjects level.
Stress and LOC-eating
Within-subjects level associations suggest that an individual is more susceptible to LOC-eating when HR is higher, and HRV is lower, than average. Since elevated HR and lower HRV can indicate stress (17), these findings suggest that LOC may be more likely to occur following stress. This finding dovetails with a naturalistic self-report study of adults in which a positive relationship between daily stress and snack intake among high-stress responders was found (26). Notably, conclusions that can be drawn from the current study are limited by the small sample size and insufficient examination of potential confounding or moderating variables, including factors varying at the person-level (e.g. pubertal status, LOC frequency/severity) and the state-level (e.g. environmental factors, physical activity, phase of menstrual cycle). In spite of this, findings set the stage for a larger investigation with more rigorous control of confounders, and provide promising data to support investigation of the mediation hypothesis that stressors predict physiologic indices, which in turn predict LOC-eating.
Potential mechanisms
From a psychological perspective, LOC-eating may be used to cope with or alleviate negative emotions, consistent with affect theories (7, 8). From a physiologic perspective, stress-induced glucoregulatory processes may contribute to LOC-eating via the production of insulin during the recovery phase of the stress response (27), which may in turn promote hunger (27, 28). Differentiating whether glucoregulatory processes specifically promote LOC, as compared to non-LOC, episodes may further elucidate this potential mechanism. It is possible that physiologic (homeostatic) and non-homeostatic factors interact to promote LOC-eating in stressful situations.
Conclusion
In conclusion, among adolescent girls, markers of physiological stress may predict LOC-eating. These findings are consistent with models of LOC as a coping strategy (7, 8). If replicated, findings point to the potential utility of physiologic indices for assessing momentary susceptibility to LOC and/or as a biofeedback tool. Especially among youth or others with difficulty self-reporting psychological constructs, physiologic indices may serve as a salient cue for LOC-eating. Future research accounting for additional influences on HR and HRV may more definitively elucidate the relation between physiologic stress and LOC-eating.
Supplementary Material
Acknowledgments
Research support: by NIMH 5F31MH095348 (to LMR), NIDDK grant 1R01DK080906-01A1 (to MTK), USUHS grant R072IC (to MTK).
Footnotes
Disclaimer: The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of USUHS or the U.S. Department of Defense.
Contributor Information
Lisa M. Ranzenhofer, Email: lisa_ranzenhofer@brown.edu.
Scott G. Engel, Email: sengel@nrifargo.com.
Ross D. Crosby, Email: rcrosby@nrifargo.com.
Mark Haigney, Email: mark.haigney@usuhs.edu.
Micheline Anderson, Email: micheline.anderson@gmail.com.
Jeanne M. McCaffery, Email: jeanne_mccaffery@brown.edu.
Marian Tanofsky-Kraff, Email: marian.tanofsky-kraff@usuhs.edu.
References
- 1.Tanofsky-Kraff M. Binge eating among children and adolescents. In: Jelalian E, Steele R, editors. Handbook of Child and Adolescent Obesity. New York: Springer Publishers; 2008. pp. 41–57. [Google Scholar]
- 2.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: implications for preventing weight-related disorders. Archives of pediatrics & adolescent medicine. 2002;156(2):171–178. doi: 10.1001/archpedi.156.2.171. Epub 2002/02/12. doi: poa10194 [pii]. PubMed PMID: 11814380. [DOI] [PubMed] [Google Scholar]
- 3.Hilbert A, Hartmann AS, Czaja J, Schoebi D. Natural course of preadolescent loss of control eating. Journal of abnormal psychology. 2013;122(3):684–693. doi: 10.1037/a0033330. Epub 2013/09/11. doi: 10.1037/a0033330. PubMed PMID: 24016009. [DOI] [PubMed] [Google Scholar]
- 4.Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, et al. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr. 2013;167(2):149–155. doi: 10.1001/2013.jamapediatrics.12. Epub 2012/12/12. doi: 10.1001/2013.jamapediatrics.12. PubMed PMID: 23229786; PubMed Central PMCID: PMC3654655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, et al. A prospective study of pediatric loss of control eating and psychological outcomes. Journal of abnormal psychology. 2011;120(1):108–118. doi: 10.1037/a0021406. Epub 2010/12/01. doi: 10.1037/a0021406. PubMed PMID: 21114355; PubMed Central PMCID: PMC3051193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. The International journal of eating disorders. 2009;42(1):26–30. doi: 10.1002/eat.20580. Epub 2008/08/23. doi: 10.1002/eat.20580. PubMed PMID: 18720473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawkins RC, Clement PF. Binge eating: Measurement problems and a conceptual model. In: Hawkins RC, Fremouw WJ, Clement PF, editors. The binge purge syndrome: Diagnosis, treatment, and research. New York, NY: Springer; 1984. pp. 229–251. [Google Scholar]
- 8.Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. Epub 1991/07/01. PubMed PMID: 1891520. [DOI] [PubMed] [Google Scholar]
- 9.Wilfley DE, Pike KM, Striegel-Moore RH. Toward an integrated model of risk for binge eating disorder. Journal of Gender Culture and Health. 1997;2(1):1–32. [Google Scholar]
- 10.Appelhans BM, Luecken LJ. Heart rate variability as an index of regulated emotional responding. Journal of General Psychology. 2006;10(3):229–240. [Google Scholar]
- 11.Hilbert A, Rief W, Tuschen-Caffier B, de Zwaan M, Czaja J. Loss of control eating and psychological maintenance in children: an ecological momentary assessment study. Behav Res Ther. 2009;47(1):26–33. doi: 10.1016/j.brat.2008.10.003. Epub 2008/11/18. doi: S0005-7967(08)00208-8 [pii] 10.1016/j.brat.2008.10.003. PubMed PMID: 19010458. [DOI] [PubMed] [Google Scholar]
- 12.Tanofsky-Kraff M, Goossens L, Eddy KT, Ringham R, Goldschmidt A, Yanovski SZ, et al. A multisite investigation of binge eating behaviors in children and adolescents. Journal of consulting and clinical psychology. 2007;75(6):901–913. doi: 10.1037/0022-006X.75.6.901. Epub 2007/12/19. doi: 2007-19013-007 [pii] 10.1037/0022-006X.75.6.901. PubMed PMID: 18085907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ranzenhofer LM, Engel SG, Crosby RD, Anderson M, Vannucci A, Cohen LA, et al. Using ecological momentary assessment to examine interpersonal and affective predictors of loss of control eating in adolescent girls. The International journal of eating disorders. 2014 doi: 10.1002/eat.22333. Epub 2014/07/22. doi: 10.1002/eat.22333. PubMed PMID: 25046850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vogele C, Florin I. Psychophysiological responses to food exposure: an experimental study in binge eaters. The International journal of eating disorders. 1997;21(2):147–157. doi: 10.1002/(sici)1098-108x(199703)21:2<147::aid-eat5>3.0.co;2-l. Epub 1997/03/01. PubMed PMID: 9062838. [DOI] [PubMed] [Google Scholar]
- 15.Legenbauer T, Vogele C, Ruddel H. Anticipatory effects of food exposure in women diagnosed with bulimia nervosa. Appetite. 2004;42(1):33–40. doi: 10.1016/S0195-6663(03)00114-4. Epub 2004/03/24. doi: 10.1016/S0195-6663(03)00114-4. PubMed PMID: 15036781. [DOI] [PubMed] [Google Scholar]
- 16.Klatzkin RR, Gaffney S, Cyrus K, Bigus E, Brownley KA. Binge eating disorder and obesity: Preliminary evidence for distinct cardiovascular and psychological phenotypes. Physiology & behavior. 2015 doi: 10.1016/j.physbeh.2015.01.018. Epub 2015/01/21. doi: 10.1016/j.physbeh.2015.01.018. PubMed PMID: 25600469. [DOI] [PubMed] [Google Scholar]
- 17.Porges SW. Cardiac vagal tone: a physiological index of stress. Neuroscience and biobehavioral reviews. 1995;19(2):225–233. doi: 10.1016/0149-7634(94)00066-a. Epub 1995/01/01. doi: 014976349400066A [pii]. PubMed PMID: 7630578. [DOI] [PubMed] [Google Scholar]
- 18.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–216. doi: 10.1016/s0165-0327(00)00338-4. Epub 2001/02/13. PubMed PMID: 11163422. [DOI] [PubMed] [Google Scholar]
- 19.Thayer JF, Lane RD. Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neuroscience and biobehavioral reviews. 2009;33(2):81–88. doi: 10.1016/j.neubiorev.2008.08.004. Epub 2008/09/06. doi: 10.1016/j.neubiorev.2008.08.004. PubMed PMID: 18771686. [DOI] [PubMed] [Google Scholar]
- 20.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999 – 2010. JAMA : the journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. Epub 2012/01/19. doi: 10.1001/jama.2012.40. PubMed PMID: 22253364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fairburn CG, Cooper Z, editors. The Eating Disorder Examination (12th ed.) 12 ed. New York: Guilford Press; 1993. [Google Scholar]
- 22.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart Rate Variability: Standards of Measurement, Physiological Interpretation, and Clinical Use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 23.Dobson C, Olsen C, T LM, M B, M V, P M, et al. QT Variability Index on 24-Hour Holter Independently Predicts Mortality in Patients with Heart Failure: Analysis of GISSI-HF Trial Data. Heart Rhythm. 2011;8(8):1237–1242. doi: 10.1016/j.hrthm.2011.03.055. [DOI] [PubMed] [Google Scholar]
- 24.Friesen CA, Lin Z, Schurman JV, Andre L, Mc Callum RW. Autonomic nervous system response to a solid meal and water loading in healthy children: its relation to gastric myoelectrical activity. Neurogastroenterol Motil. 2007;19(5):376–382. doi: 10.1111/j.1365-2982.2007.00906.x. Epub 2007/05/19. doi: NMO906 [pii] 10.1111/j.1365-2982.2007.00906.x. PubMed PMID: 17509019. [DOI] [PubMed] [Google Scholar]
- 25.Harthoorn LF, Dransfield E. Periprandial changes of the sympathetic-parasympathetic balance related to perceived satiety in humans. Eur J Appl Physiol. 2008;102(5):601–608. doi: 10.1007/s00421-007-0622-5. Epub 2007/12/20. doi: 10.1007/s00421-007-0622-5. PubMed PMID: 18092177; PubMed Central PMCID: PMC2225999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newman E, O'Connor DB, Conner M. Daily hassles and eating behaviour: the role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32(2):125–132. doi: 10.1016/j.psyneuen.2006.11.006. Epub 2007/01/03. doi: 10.1016/j.psyneuen.2006.11.006. PubMed PMID: 17198744. [DOI] [PubMed] [Google Scholar]
- 27.Sominsky L, Spencer SJ. Eating behavior and stress: a pathway to obesity. Frontiers in psychology. 2014;5:434. doi: 10.3389/fpsyg.2014.00434. Epub 2014/05/27. doi: 10.3389/fpsyg.2014.00434. PubMed PMID: 24860541; PubMed Central PMCID: PMC4026680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dunn-Meynell AA, Sanders NM, Compton D, Becker TC, Eiki J, Zhang BB, et al. Relationship among brain and blood glucose levels and spontaneous and glucoprivic feeding. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009;29(21):7015–7022. doi: 10.1523/JNEUROSCI.0334-09.2009. Epub 2009/05/29. doi: 10.1523/JNEUROSCI.0334-09.2009. PubMed PMID: 19474328; PubMed Central PMCID: PMC2728115. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.