Abstract
Using a cohort of African American women enrolled in a physical activity program, the purpose of the paper is to examine how well individual characteristics, neighborhood characteristics and intervention participation predict study retention and staff level of effort needed for retention. Secondary data analysis was conducted from a randomized clinical trial. Participants were 40–65 years without major signs/symptoms of cardiovascular disease. Assessments were conducted at community sites in/bordering African American communities. Study retention was 90%. Of those retained, 24% required moderate/high level of staff effort for retention. Retention was predicted by being older, having lower perceived neighborhood walkability, living in neighborhoods with greater disadvantage and crime, and having greater program participation. More staff effort was predicted by participants being younger, having more economic hardships, poorer health, or lower intervention participation. We may be able to identify people at baseline likely to require more staff effort to retain.
Keywords: retention, intervention, physical activity, African American, women
African American women report lower physical activity (PA) levels than White American women, and this contributes to health disparities in cardiovascular health, diabetes, and depressive symptoms (National Center for Health Statistics, 2013). To address this, researchers must develop proven effective PA interventions. However, retaining minority participants for post-baseline outcome assessments in behavior change studies is challenging (Carroll et al., 2011). Completion of post-baseline assessments is an issue of missing data. Low levels of completion of post-baseline assessments lead to reduced analytic samples. Reducing the size of the analytic sample introduces potential bias in the sample and limits generalizability. In addition, missing data reduces statistical power.
Factors Influencing Study Retention and Staff Effort for Study Retention
Three important factors that influence study retention include participant characteristics, neighborhood characteristics and intervention participation. Participant characteristics associated with lower study retention rates among African American women in PA interventions have been identified in previous studies. Employment (Parra-Medina et al., 2011; Yanek, Becker, Moy, Gittelsohn, & Koffman, 2001) and younger age (Parra-Medina et al., 2011; Resnicow et al., 2005; Yanek et al., 2001; Young & Stewart, 2006) have been associated with lower retention in several studies of PA interventions for African American women. Associations with income have been inconsistent, with one study reporting a negative association (lower income related to higher study retention; Yanek et al., 2001) and another reporting positive associations (Wilbur et al., 2008). Several PA studies reported African American women’s reasons for low retention, including health problems and factors that can contribute to stress such as family issues, and lack of time (Hornbuckle et al., 2012; Wilbur et al., 2008). Neighborhood characteristics such as living in high-poverty areas have been shown to decrease the odds of enrolling in a PA program (Wilbur et al., 2006) and, for those individuals who do enroll, may reduce study retention. Finally, intervention participation has also been shown to be associated with study retention. Not surprisingly, Yanek et al. (2001) found that African American women who had higher intervention participation were more likely to have higher study retention (complete post-baseline assessments) than those with lower intervention participation.
Participant characteristics, neighborhood characteristics and intervention participation are related to study retention. In order to offset bias created by low study retention, it has been noted that research staff effort must be expended to retain participants for post-baseline assessments in non-physical activity interventions (Barnett, Aguilar, Brittner, & Bonuck, 2012; Senturia et al., 1998). However for PA interventions, staff level of effort in regards to retention is a little studied factor (Carroll et al., 2011; Whitt-Glover et al., 2014). By understanding the characteristics that are associated with PA study retention, we may be able to identify participants at baseline that are most likely to require greater staff effort to retain.
Purpose
Using a cohort of community-based, inactive, midlife African American women who were enrolled in the Women’s Lifestyle Physical Activity program, the purpose of the paper is to examine how well baseline individual characteristics (demographics, stress, and health), neighborhood characteristics (neighborhood walkability, poverty, and crime) and intervention participation predict: (1) study retention and (2) staff level of effort needed for study retention.
Methods
Design
This is a secondary analysis of data collected from a previously conducted randomized clinical trial, the Women’s Lifestyle PA Program (Wilbur et al., 2015). Post-baseline assessments were conducted at 24- and 48-weeks.
Sample and Setting
As described elsewhere in detail, participants in the Women’s Lifestyle PA Program were sedentary (not involved in routine exercise two or more times per week in the past six months), urban-dwelling, midlife African American women aged 40 to 65 years (Wilbur et al., 2015; Wilbur et al., 2013). Exclusion criteria included only risks for exercise-related adverse events: (1) major signs or symptoms of pulmonary disease or cardiovascular disease; (2) history of myocardial infarction or stroke; and (3) blood pressure ≥ 160 mmHg systolic or ≥ 100 mmHg diastolic (American College of Sports Medicine, 2010). Women with diabetes had to have a HbA1c less than 9% (American Diabetes Association, 2004). All women signed an informed consent, and the study was approved by the Institutional Review Board at two universities.
Recruitment was concentrated within the six Chicago communities where the study healthcare sites were located, including three community hospitals and three health centers. The sites were in or bordering low-income communities that were predominantly African American (> 90%; United States Census Bureau, 2014b).
Briefly, as reported elsewhere (Wilbur et al., 2013), of the 514 women who completed an initial telephone screening, 105 were ineligible and 409 were scheduled for a health assessment screening for cardiovascular risk at their respective community site with a study nurse practitioner. Of the 337 women (72 women did not come to the health assessment) who completed the screening health assessment, 40 were ineligible. The remaining 297 were not at risk for exercise-related adverse events and therefore found safe to increase their PA without close monitoring. A total of 288 women began the Women’s Lifestyle Physical Activity Program. Twenty-four and 48-week post-baseline follow up assessments took place at the original community sites, unless participants were unable to reach the original sites. In those cases, assessments were completed at locations of the participants’ convenience.
Intervention
The Women’s Lifestyle PA Program was a randomized clinical trial testing three lifestyle PA conditions (Wilbur et al., 2015). All women in the study were invited to participate in six group meetings (held at the same community healthcare sites as the assessments) that consisted of brief individual time with a program nurse, followed by a group discussion led predominately by a nurse facilitator. Social cognitive strategies were applied throughout including behavioral capability, self-regulation (self-monitoring, goal setting, problem-solving), behavioral rehearsal, and vicarious experience (Bandura, 1997). The first five group meetings were held every five weeks during the more intensive 24-week adoption period, with a sixth “booster” group meeting held during the subsequent 24-week maintenance period. Between meetings, the first condition received 11 person-administered motivational phone calls, the second condition received 11 automated computer-generated motivational tips, and the third condition received no motivational phone calls. All three conditions had significant improvements in PA and weight maintenance and there were no significant differences between conditions (Wilbur et al., 2015).
Measures
Individual characteristics
Demographics included age, marital status, family income, number of children under age 18, education, and employment. Nine questions from the Hardship Measure used in the U.S. Census Bureau Survey of Income and Program Participation (Bauman, 1998) assessed ability (yes/no) to meet expenses for housing, utility, telephone, medical needs, and food adequacy. The “yes” responses were summed for a score ranging from 0 to 9.
Stress was measured with the 14-item global Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983). Participants are asked how often they felt or thought a certain way during the last month: 0 = never to 4 = very often. Items are summed for a total of 0 to 56, with a high score indicating higher stress. A recent review showed that internal consistency was acceptable across multiple trials (α’s ≥ .78; Al Kalaldeh & Shosha, 2012). Construct validity was demonstrated by correlating the measure with other measures with established validity (Cohen et al., 1983).
General health was measured with a single item from the Behavioral Risk Factor Surveillance System (2010). Participants are asked to rate their overall health status from 5 = excellent to 1 = poor.
Neighborhood characteristics
Perceived attributes of the neighborhood were assessed with five subscales (28 items) from the Neighborhood Environment Walkability Scale, including neighborhood surroundings, safety from crime, safety from traffic, access to services, and sidewalk infrastructure (Saelens, Sallis, Black, & Chen, 2003). All items are measured on a Likert scale from 1 = strongly disagree to 4 = strongly agree with higher scores indicating better walkability. Test-retest reliability has been supported (Brownson et al., 2004; Saelens et al., 2003), and construct validity was demonstrated by significant differences in the subscales between neighborhoods that differed on walkability (Saelens et al., 2003).
Two objective measures of neighborhood characteristics were obtained based on geocoded residential addresses. Using U.S. Census Bureau 2010 data, neighborhood-level concentrated disadvantage (Tolan, Gorman-Smith, & Henry, 2003) was determined for each participant: a linear combination of four measures from the 2007–2011 estimates in the American Community Survey (United States Census Bureau, 2014a) aggregating (a) families below poverty, (b) renter-occupied housing, (c) unemployment, and (d) female-headed households. Next, rates (incidence per 100,000 residents) of index crime (murder, criminal sexual assault, robbery, aggravated assault/battery, burglary, theft, motor vehicle theft, and arson) for the 2009 calendar year were obtained from the Chicago Police Department and Illinois State Police (United States Department of Justice, 2013). Rates in the city of Chicago were calculated for each census tract, while suburban rates were calculated for the entire community.
Intervention participation
Intervention participation was measured by the number of the six group meetings the women attended over the intervention’s 48 weeks.
Study retention
Women who returned for their post-baseline 48-week assessment were identified as retained in the study, while those who did not were classified as not retained.
Staff effort for study retention
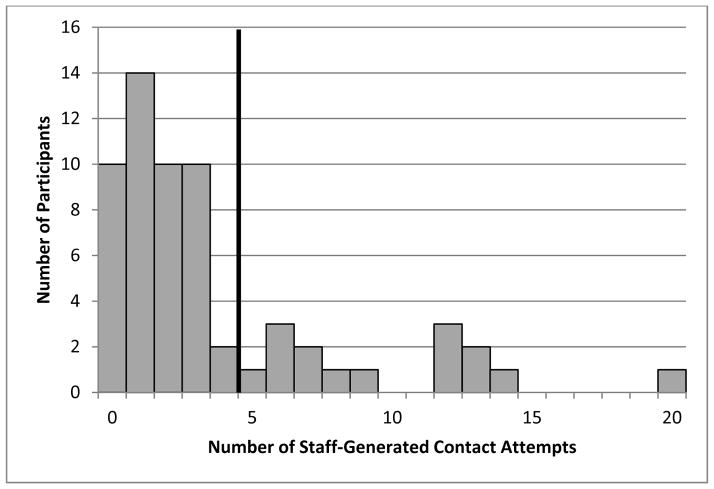
Staff effort for study retention was classified into three levels: standard, moderate, high. The retained participants who completed both the 24- and 48-week assessments on their original scheduled date were assigned to the standard staff effort group. The definition of moderate and high levels was based on visual inspection of the data. The contact attempts histogram (Figure 1) had a bimodal distribution, with a cutoff between four and five attempts. Therefore, the contact attempts were dichotomized into “moderate staff effort” (0–4 attempts) and “high staff effort” (5 or more), creating a three-level staff effort variable (standard, moderate, and high). As a second indicator of staff effort, the 13 participants in the moderate staff effort group whose assessments had to be completed away from the standard data collection sites were reassigned to the high staff effort group.
Figure 1.
Contact Attempts Histogram
Protocol
Baseline and follow-up assessment at 24 and 48 weeks after baseline each included a questionnaire, a health history, blood pressure, weight and a fitness test. These assessments occurred at the same community healthcare sites as the group visits and were scheduled two months in advance. Appointment times included weekday afternoons and select Saturday mornings with on-site childcare provided if needed. The research staff would provide a schedule of possible appointment times for the participants to choose from, at the group visit that occurred either prior to the 24- or 48-week assessment. Participants received a letter confirming the location, date, and time of each follow-up assessment one month prior to the appointment. In addition, each participant received up to three reminder telephone calls at their preferred number (home, cell or work) and preferred time of day (including evenings) the week of the scheduled assessment appointment. Once direct contact was made on these reminder calls, no further calls were made. If a woman was unable to come to the community healthcare sites at the scheduled times, arrangements were made for a staff member to go to the women’s home to complete the assessment. For women who missed their scheduled appointments, rescheduling contact attempts (telephone, text and/or e-mail) were made until they completed the assessment, withdrew from the study, or were lost to follow-up. Women were considered lost to follow-up when all attempts to contact them up to three months after they did not show up for their 48-week health assessment, were unsuccessful. During screening, participants provided a preferred number and time of day to be reached were obtained along with information on two alternative contact persons. A web-based system was used to track study appointments and contacts (either staff- or participant-generated), with participant information updated during each contact. Participants could leave voice messages, which were reviewed and calls were returned daily. The women were compensated $40 for their time at each assessment. In addition, women were given their own pedometer at the conclusion of the 48-week assessment.
Statistics
Bivariate analyses were done first to examine differences between study retention groups (retained, not retained) and between staff level of effort for study retention groups (standard, moderate, and high) on baseline individual characteristics, neighborhood characteristics and intervention participation. Using binary logistic regression, study retention was regressed on baseline individual characteristics, neighborhood characteristics and intervention participation. Staff level of effort was then regressed on baseline individual characteristics, neighborhood characteristics and intervention participation using multiple ordinal logistic regression.
Results
Descriptive findings
Descriptive statistics for study variables are presented in Table 1 (continuous variables) and Table 2 (categorical variables). The 288 participants ranged in age from 50 to 65 (M = 53 years). Just over one-third were married, and over one-third had at least one child under 18. Half of the participants had less than a college education, and a quarter was unemployed. The majority (60%) had a family income of less than $60,000, and 45% had experienced at least one economic hardship in the past year. On average, participants had mean stress in the middle range of possible stress scores (M = 20.60) and rated their general health as fair. Census-based measures of neighborhood concentrated disadvantage indicated that the neighborhoods averaged over one standard deviation above the mean concentrated disadvantage for the US (M = 1.23), placing the average study neighborhood at the 89th percentile of concentrated disadvantage. Average index crime rate in the communities in which participants resided was 6,192 incidents per 100,000 residents for the year 2012, nearly twice the national rate (3,246; United States Department of Justice, 2013). Despite these findings, participant perception of neighborhood walkability on average tended toward the positive end of the scale (M = 3.11).
Table 1.
Baseline characteristics and intervention participation by retention and staff level of effort for retention
| Total (N=288) M (SD) |
Retention (N=288) M (SD) |
Staff level of effort for retention (N=260) M (SD) |
||||||
|---|---|---|---|---|---|---|---|---|
| Retained (n=260) | Not retained (n=28) | p | Standard (n=199) | Moderate (n=33) | High (n=28) | p | ||
| Baseline characteristics | ||||||||
| Age | 53.07 (6.55) | 53.48 (6.50) | 49.29 (5.81) | .001 | 54.08 (6.27) | 50.55 (7.23) | 52.64 (6.45) | .011 |
| Stressa | 20.60 (6.75) | 20.65 (6.79) | 20.07 (6.53) | .673 | 20.32 (6.97) | 21.84 (6.33) | 21.61 (5.87) | .363 |
| General healtha | 3.23 (0.79) | 3.25 (0.80) | 3.07 (0.73) | .279 | 3.33 (0.82) | 3.04 (0.75) | 2.89 (0.57) | .009 |
| Neighborhood | ||||||||
| Concentrated disadvantage | 1.23 (1.16) | 1.31 (1.15) | 0.53 (1.07) | .001 | 1.29 (1.16) | 1.31 (0.97) | 1.50 (1.30) | .645 |
| Rates of index crime | 6192.12 (3476.22) | 6346.56 (3485.14) | 4774.63 (3103.54) | .023 | 6348.51 (3507.85) | 6231.40 (3807.09) | 6464.48 (3027.75) | .967 |
| Neighborhood walkabilitya | 3.11 (0.43) | 3.08 (0.42) | 3.45 (0.39) | <.001 | 3.09 (0.42) | 3.01 (0.42) | 3.05 (0.38) | .558 |
| Intervention participation | 4.56 (1.48) | 4.84 (1.23) | 2.00 (1.15) | <.001 | 5.02 (1.15) | 4.61 (1.25) | 3.85 (1.30) | <.001 |
Some cases had missing data for these variables.
Table 2.
Baseline characteristics and study condition by retention and staff level of effort for retention
| Total (N=288) N (%) |
Retention (N=288) N (%) |
Staff level of effort for retention (N=260) N (%) |
||||||
|---|---|---|---|---|---|---|---|---|
| Retained (n=260) | Not retained (n=28) | p | Standard (n=199) | Moderate (n=33) | High (n=28) | p | ||
| Baseline characteristics | ||||||||
| Marital or living with partnera | 110 (38.3%) | 101 (38.8%) | 9 (33.3%) | .575 | 78 (39.2%) | 15 (45.5%) | 8 (28.6%) | .394 |
| One or more children younger than 18 years of age | 106 (36.8%) | 95 (36.5%) | 11 (39.3%) | .775 | 67 (33.7%) | 14 (42.4%) | 14 (50.0%) | .184 |
| Education college or highera | 142 (49.5%) | 128 (49.2%) | 14 (51.9%) | .795 | 102 (51.3%) | 13 (39.4%) | 13 (46.4%) | .429 |
| Employed (full- or part-time)a | 213 (74.2%) | 193 (74.2%) | 20 (74.1%) | .986 | 151 (75.9%) | 23 (69.7%) | 19 (67.9%) | .540 |
| Incomea | .757 | .074 | ||||||
| <$20,000 | 32 (11.7%) | 30 (12.1%) | 2 (8.0%) | 21 (11.1%) | 5 (15.6%) | 4 (14.8%) | ||
| $20,000–$39,999 | 71 (26.0%) | 66 (26.6%) | 5 (20.0%) | 46 (24.3%) | 9 (28.1%) | 11 (40.7%) | ||
| $40,000–$59,999 | 62 (22.7%) | 55 (22.2%) | 7 (28.0%) | 45 (23.8%) | 5 (15.6%) | 5 (18.5%) | ||
| ≥$60,000 | 108 (39.6%) | 97 (39.1%) | 11 (44.0%) | 77 (40.7%) | 13 (40.6%) | 7 (25.9%) | ||
| Hardshipa | .684 | .001 | ||||||
| No hardship | 156 (55.3%) | 142 (55.7%) | 14 (51.9%) | 116 (59.5%) | 19 (57.6%) | 7 (25.9%) | ||
| One hardship | 65 (23.0%) | 57 (22.4%) | 8 (29.6%) | 42 (21.5%) | 8 (24.2%) | 7 (25.9%) | ||
| More than one hardship | 61 (21.6%) | 56 (22.0%) | 5 (18.5%) | 37 (19.0%) | 6 (18.2%) | 13 (48.1%) | ||
| Study Condition | .624 | .638 | ||||||
| Group Meeting | 95 (33.0%) | 88 (33.8%) | 7 (25.0%) | 66 (33.2%) | 12 (36.4%) | 10 (35.7%) | ||
| Group Meeting + Personal Calls | 96 (33.3%) | 86 (33.1%) | 10 (35.7%) | 70 (35.2%) | 10 (30.3%) | 6 (21.4%) | ||
| Group Meeting + Automated Calls | 97 (33.7%) | 86 (33.1%) | 11 (39.3%) | 63 (31.7%) | 11 (33.3%) | 12 (42.9%) | ||
Some cases had missing data for these variables.
Mean intervention participation for the women was 76% (4.56/6) of possible group meetings, and overall study retention at 48 weeks was 90% (260/288), including one woman who missed her 24-week post-baseline assessment. Of the 28 women who were not retained in the study, 23 withdrew from the study and 5 were lost to follow-up. As reported earlier, the primary reasons for withdrawal were family issues (n = 7), health problems (n =5), time constraints (n =5), other reasons (n = 6), (Wilbur et al., 2015).
Of the 260 women retained in the study, 76% (199/260) came to their 24- and 48-week assessments at the originally-scheduled time and location, thereby requiring only standard staff effort, while 13% (33/260) required moderate staff effort, and 11% (28/260) required high staff effort for study retention. Of the 28 women who required high staff effort, 21 (75%) required five or more extra contacts and 7 (25%) required fewer than five contacts but completed the assessment at a location other than the original community data collection site. Among those retained, the overall number of contacts ranged from 0 to 20. No significant differences were attributable to study condition in either the rate of study retention or staff level of effort for study retention.
For comparative purposes 15 of the 28 women not retained withdrew before the 24 week assessment and 8 women withdrew before the 48-week assessment. For women who were not retained the number of contacts therefore ranged from 0 to 21.
Baseline characteristics and intervention participation by study retention and staff level of effort for study retention
Bivariate analyses showed significant differences by study retention for age, neighborhood concentrated disadvantage, rate of index crime, perceived neighborhood walkability, and intervention participation (Table 1). Those who were retained were significantly older, had higher scores on both concentrated neighborhood disadvantage and index crime rates, and had lower perceived neighborhood walkability. In addition, they had significantly higher intervention participation. The point biserial correlation between intervention participation and study retention was .57. Using baseline characteristics and intervention participation as predictors, a binary logistic regression was conducted with study retention as the dependent variable. Age, perceived neighborhood walkability, and intervention participation, remained significant multivariate predictors of being retained in the study (see Table 3). Older age, lower perceived neighborhood walkability, and higher intervention participation all increased the odds of completing the post-baseline 48-week assessments (Cox and Snell R2 = .31; χ2 = 105.15, df = 3, p ≤ .001).
Table 3.
Results of Final Binary Logistic Regression Model for Study Retention on Baseline Characteristics and Intervention Participation.
| b | SE | p | OR | 95% CI | |
|---|---|---|---|---|---|
| Age | 0.17 | 0.06 | .002 | 1.19 | [1.06, 1.33] |
| Intervention Participation | 1.32 | 0.23 | <.001 | 3.73 | [2.39, 5.81] |
| Neighborhood Walkability | −3.43 | 0.92 | <.001 | 0.03 | [0.01, 0.20] |
| Constant | 0.29 | 3.25 | .928 | 1.34 |
Bivariate analyses showed significant differences by staff level of effort for study retention for age, number of hardships, self-rated general health, and intervention participation (Tables 1 and 2). Those who were younger, had more hardships, poorer health, or lower intervention participation required a higher level of staff effort for study retention. In a multiple ordinal logistic regression with level of staff effort for study retention as the dependent variable, age, number of hardships, self-rated general health, and level of intervention participation remained significant independent predictors of staff level of effort for study retention (see Table 4). Younger age, more hardships, poorer self-rated general health, and lower level of intervention participation were independently related to increased staff level of effort for study retention (Cox and Snell R2 = .15; χ2 = 42.17, df = 4, p ≤ .001).
Table 4.
Results of Final Ordinal Logistic Regression Model for Staff Level of Effort for Study Retention on Baseline Characteristics and Intervention Participation.
| b | SE | Wald | p | 95% CI | |
|---|---|---|---|---|---|
| Parameter 1 | −6.05 | 1.65 | 13.50 | <.001 | [−9.27, −2.82] |
| Parameter 2 | −4.93 | 1.63 | 9.17 | .002 | [−8.13, −1.74] |
| General Health | −0.66 | 0.21 | 9.55 | .002 | [−1.07, −0.24] |
| Age | −0.06 | 0.03 | 5.48 | .019 | [−0.11, −0.01] |
| Hardships | 0.35 | 0.12 | 7.78 | .005 | [0.10, 0.59] |
| Intervention Participation | −0.52 | 0.12 | 19.15 | <.001 | [−0.75, −0.28] |
Discussion
We analyzed the relationships of baseline individual characteristics, neighborhood characteristics and intervention participation to both study retention and staff level of effort needed for study retention in the Women’s Lifestyle PA Program. At the 48-week assessment, the program had a study retention rate of 90%, which is higher than the mean study retention rate of 70% in 12 recent PA intervention studies with greater than 75% African American females at 6 and 12 months (Bopp et al., 2009; Clark, Stump, & Damush, 2003; Fitzgibbon et al., 2010; Hornbuckle et al., 2012; Newton & Perri, 2004; Parra-Medina et al., 2011; Resnicow et al., 2005; Wilbur et al., 2008; Yancey et al., 2006; Yanek et al., 2001; Young & Stewart, 2006; Zoellner et al., 2010).
Similar to earlier studies with African American women, participants who were not retained were younger than women who were retained (Parra-Medina et al., 2011; Resnicow et al., 2005; Yanek et al., 2001; Young & Stewart, 2006). Despite the availability of childcare and scheduling assessments at a convenient time, younger women may have more time barriers than older women and may need innovative assessment strategies such as online questionnaires. Although we did not find differences in study retention based on individual socioeconomic factors, we were surprised to find that women who were not retained tended to have lower neighborhood poverty and crime as well as higher perceived neighborhood walkability. We speculate that women from impoverished neighborhoods, regardless of socioeconomic status, may have perceived more benefit from the support they received at the group meetings in overcoming neighborhood barriers to PA (Ingram, Wilbur, McDevitt, & Buchholz, 2011; Jaber, Braksmajer, & Trilling, 2006). This perceived benefit may have then translated to a greater willingness to complete follow-up assessments. These mechanisms should be explored in future studies.
Retention was not significantly related to baseline general health. In contrast, a modal reason for withdrawal in earlier studies was poor participant health (Newton & Perri, 2004; Wilbur et al., 2008; Young & Stewart, 2006). While the difference was not significant, it was in the same direction as in the other studies. Baseline general health may be of limited utility in predicting the impact of later health problems on study retention; however, monitoring health throughout a study can help decrease this impact.
Intervention participation was higher among women who were retained. As noted by Carroll and colleagues (2011), intervention participation influences but is distinct from study retention. Although there is a strong relationship between intervention participation and study retention, they only share about 33% of the variance in this sample. This demonstrates that, while they are related, intervention participation and study retention should be treated as distinct concepts.
In addition to examining the characteristics of women who were not retained in the study, we also examined the characteristics of those 61 women who took more staff effort to be successfully retained compared to the 199 women who required only standard effort. Without the additional staff effort, study retention may have been even lower with the younger women and those who had lower intervention participation. Although economic factors and health were not related to study retention, women with more hardships and women with poor health tended to require more staff effort to retain. The additional staff effort may have prevented the loss of these women, thus retaining a sample more representative of those who began the study.
The study has limitations. Generalizability is limited by the fact that the participants were volunteer, urban African American midlife women. The high rates of intervention participation and study retention may have been artifacts of self-selection into the study. In addition, future studies should provide estimates of costs incurred to enhance study retention.
In summary, 24% (61/260) of the women successfully retained in our study required additional staff efforts to arrange their post-baseline assessments. The high study retention rates even among those women with more hardships and poorer health may reflect the additional effort extended by staff to reach women who did not attend their original scheduled assessments. These efforts likely added to the study’s external validity by lessening the effects of hardships and health on study retention. In future studies, researchers could identify women at the start of the intervention likely to require more staff effort to retain and thus make expenditure of resources more efficient.
Acknowledgments
The authors gratefully acknowledge the study participants and research collaborators Phyllis Pelt, MSN, RN, Edith V. Ocampo, MS, Shannon Halloway, BSN, RN, and Judith McDevitt, PhD, RN.
Funding: The study was funded by Award Number R01NR004134, National Institute of Nursing Research.
Footnotes
Registered Clinical Trial: NCT01700894
Declaration of Conflicting Interests: The authors declare no potential conflicts of interest.
References
- Al Kalaldeh MT, Shosha GMA. Application of the perceived stress scale in health care studies: An analysis of literature. International Journal of Academic Research. 2012;4(4):45–50. [Google Scholar]
- American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 8. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- American Diabetes Association. Physical activity/exercise and diabetes. Diabetes Care. 2004;27:S58–S62. doi: 10.2337/diacare.27.2007.s58. Retrieved from http://care.diabetesjournals.org/content/27/suppl_1/s58.full. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W.H. Freeman and Company; 1997. [Google Scholar]
- Barnett J, Aguilar S, Brittner M, Bonuck K. Recruiting and retaining low-income, multi-ethnic women into randomized controlled trials: Successful strategies and staffing. Contemporary Clinical Trials. 2012;33(5):925–932. doi: 10.1016/j.cct.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman KJ. Direct measure of poverty as an indicator of economic need: Evidence from the survey of income and program participation. Washington, DC: U.S. Census Bureau, Population Division; 1998. [Google Scholar]
- Behavioral Risk Factor Surveillance System. Behavioral risk factor surveillance system questionnaire. 2010 Retrieved from http://www.cdc.gov/brfss/questionnaires/pdf-ques/2010brfss.pdf.
- Bopp M, Wilcox S, Laken M, Hooker SP, Parra-Medina D, Saunders R, McClorin L. 8 steps to fitness: A faith-based, behavior change physical activity intervention for African Americans. Journal of Physical Activity & Health. 2009;6(5):568–577. doi: 10.1123/jpah.6.5.568. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Chang JJ, Eyler AA, Ainsworth BE, Kirtland KA, Saelens BE, Sallis JF. Measuring the environment for friendliness toward physical activity: A comparison of the reliability of 3 questionnaires. American Journal of Public Health. 2004;94(3):473–483. doi: 10.2105/ajph.94.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JK, Yancey KY, Spring B, Figueroa-Moseley C, Mohr DC, Mustian KM, Fiscella K. What are successful recruitment and retention strategies for underserved populations? Examining physical activity interventions in primary care and community settings. Translational Behavioral Medicine. 2011;1(2):234–251. doi: 10.1007/s13142-011-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DO, Stump TE, Damush TM. Outcomes of an exercise program for older women recruited through primary care. Journal of Aging and Health. 2003;15(3):567–585. doi: 10.1177/0898264303253772. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sharp LK, Singh V, Dyer A. Obesity reduction black intervention trial (ORBIT): 18-month results. Obesity. 2010;18(12):2317–2325. doi: 10.1038/oby.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornbuckle LM, Liu PY, Ilich JZ, Kim JS, Arjmandi BH, Panton LB. Effects of resistance training and walking on cardiovascular disease risk in African American women. Medicine and Science in Sports and Exercise. 2012;44(3):525–533. doi: 10.1249/MSS.0b013e31822e5a12. [DOI] [PubMed] [Google Scholar]
- Ingram D, Wilbur J, McDevitt J, Buchholz S. Women’s walking program for African American women: Expectations and recommendations from participants as experts. Women & Health. 2011;51(6):566–582. doi: 10.1080/03630242.2011.606357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaber R, Braksmajer A, Trilling JS. Group visits: A qualitative review of current research. The Journal of the American Board of Family Medicine. 2006;19(3):276–290. doi: 10.3122/jabfm.19.3.276. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2012: With special feature on emergency care. Hyattsville, MD: Author; 2013. [PubMed] [Google Scholar]
- Newton RL, Perri MG. A randomized pilot trial of exercise promotion in sedentary African American adults. Ethnicity & Disease. 2004;14(4):548–557. [PubMed] [Google Scholar]
- Parra-Medina D, Wilcox S, Salinas J, Addy C, Fore E, Poston M, Wilson DK. Results of the heart healthy and ethnically relevant lifestyle trial: A cardiovascular risk reduction intervention for African American women attending community health centers. American Journal of Public Health. 2011;101(10):1914–1921. doi: 10.2105/AJPH.2011.300151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S, Periasamy S. Results of the healthy body healthy spirit trial. Health Psychology. 2005;24(4):339–348. doi: 10.1037/0278-6133.24.4.339. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: An environment scale evaluation. American Journal of Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senturia Y, Mortimer KM, Baker D, Gergen P, Mitchell H, Joseph C, Wedner HJ. Successful techniques for retention of study participants in an inner-city population. Controlled Clinical Trials. 1998;19:544–554. doi: 10.1016/s0197-2456(98)00032-4. [DOI] [PubMed] [Google Scholar]
- Tolan PH, Gorman-Smith D, Henry DB. The developmental ecology of urban males’ youth violence. Developmental Psychology. 2003;39(2):274–291. doi: 10.1037//0012-1649.39.2.274. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. Design and methodology: American community survey. Washington, D.C: U.S. Government Printing Office; 2014a. [Google Scholar]
- United States Census Bureau. State and county quick facts. 2014b Retrieved from http://quickfacts.census.gov/qfd/states/17/1714000.html.
- United States Department of Justice. Summary reporting system (SRS) user manual. Clarksburg, WV: Federal Bureau of Investigation; 2013. [Google Scholar]
- Whitt-Glover MC, Keith NR, Ceaser TG, Virgil K, Ledford L, Hasson RE. A systematic review of physical activity interventions among African American adults: Evidence from 2009 to 2013. Obesity Reviews. 2014;15(Suppl 4):125–145. doi: 10.1111/obr.12205. [DOI] [PubMed] [Google Scholar]
- Wilbur J, Miller AM, Fogg L, McDevitt J, Castro CM, Schoeny M, Dancy BL. Randomized clinical trial of the Women’s Lifestyle Physical Activity program for African American women: 24- and 48-week outcomes. American Journal of Health Promotion. 2015 doi: 10.4278/ajhp.140502-QUAN-181. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Wilbur J, Buchholz SW, Ingram DM, Braun LT, Johnson TJ, Fogg L, McDevitt J. Effectiveness, efficiency, duration, and costs of recruiting for an African American women’s lifestyle physical activity program. Research in Nursing & Health. 2013;36(5):487–499. doi: 10.1002/nur.21550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilbur J, McDevitt J, Wang E, Dancy B, Briller J, Ingram D, Zenk SN. Recruitment of African American women to a walking program: Eligibility, ineligibility and attrition during screening. Research in Nursing & Health. 2006;29(3):176–189. doi: 10.1002/nur.20136. [DOI] [PubMed] [Google Scholar]
- Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, Lee H. Outcomes of a home-based walking program for African American women. American Journal of Health Promotion. 2008;22(5):307–317. doi: 10.4278/ajhp.22.5.307. [DOI] [PubMed] [Google Scholar]
- Yancey A, McCarthy W, Harrison G, Wong W, Siegel J, Leslie J. Challenges in improving fitness: Results of a community-based, randomized, controlled lifestyle change intervention. Journal of Women’s Health. 2006;15:412–428. doi: 10.1089/jwh.2006.15.412. [DOI] [PubMed] [Google Scholar]
- Yanek LR, Becker DM, Moy TF, Gittelsohn J, Koffman DM. Project joy: Faith based cardiovascular health promotion for African American women. Public Health Reports. 2001;116(Suppl 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young DR, Stewart KJ. A church-based physical activity intervention for African American women. Family & Community Health. 2006;29(2):103–117. doi: 10.1097/00003727-200604000-00006. [DOI] [PubMed] [Google Scholar]
- Zoellner J, Connell C, Powers A, Avis-Williams A, Yadrick K, Bogle ML. Does a six-month pedometer intervention improve physical activity and health among vulnerable African Americans? A feasibility study. Journal of Physical Activity & Health. 2010;7(2):224–231. doi: 10.1123/jpah.7.2.224. [DOI] [PubMed] [Google Scholar]