Abstract
Acute esophageal necrosis, also known as “black esophagus syndrome”, is a rare acute esophageal disease that is often associated with vomiting and upper gastrointestinal haemorrhage. At present, little is known regarding the pathogenesis of this disease. We present the case of a 50-year-old white male patient with diabetic ketoacidosis suffering from acute esophageal necrosis with nausea and vomiting but without any clinical signs of upper gastrointestinal bleeding.
Keywords: Diabetic ketoacidosis, Acute esophageal necrosis, Black esophagus syndrome
Core tip: The aetiology and pathogenesis of the so-called black esophagus syndrome are unclear. This case report supports a possible link between the occurrence of diabetic ketoacidosis and the black esophagus syndrome.
INTRODUCTION
Acute esophageal necrosis (AEN), also known as “black esophagus syndrome”, is a rare pathological condition typically characterized by a circumferential black-appearing esophageal mucosa, which mostly affects the distal portion of the esophagus and stops abruptly at the gastro-esophageal junction[1,2]. Although the aetiology of AEN is still unclear, it is likely to be multifactorial, arising from an ischaemic insult to the esophagus, an impaired local defence of the mucosal barrier systems and injury from backflow of gastric contents. Major complications of AEN include stenosis or stricture formation in the middle-distal esophagus, perforation, mediastinitis, and mortality. The overall mortality is approximately 30% and is largely related to the underlying medical conditions[1,2].
In this report, we present the case of an adult patient with AEN associated with diabetic ketoacidosis.
CASE REPORT
A 50-year-old white male patient with type 2 diabetes mellitus (treated with metformin 2 g/d) and hypertension (treated with doxazosine 4 mg/d) recently was admitted to the Emergency Department of our university hospital. He presented dysphagia, vomiting (without any clinical signs of acute upper gastrointestinal bleeding), polyuria, polydipsia and low-grade fever. These symptoms had started about two days earlier with epigastric/abdominal pain, nausea and vomiting. The patient strongly denied the ingestion of caustic substances or alcohol abuse. Twelve years earlier, he had undergone an exeresis of a superficial nasal melanoma.
Laboratory analyses revealed severe hyperglycemia (40 mmol/L), hyponatremia (121 mmol/L), hypokalemia (2.71 mmol/L), severe metabolic acidosis with glycosuria and ketonuria. Laboratory analyses also revealed increased serum creatinine levels, hypoalbuminemia, moderate leukocytosis and elevated plasma C-reactive protein concentrations. Upon physical examination, the patient appeared dehydrated, was hypotensive at 90/60 mmHg, tachycardic at 120 beats/min, and had a soft and non-tender abdomen. Chest X-rays and abdominal ultrasonography were normal.
The patient was admitted to our Endocrinology Division with a diagnosis of diabetic ketoacidosis (DKA). An appropriate treatment with intravenous hydration, potassium supplementation and insulin infusion was promptly started. Intravenous piperacillin/tazobactan was also administered intravenously every 8 h. After approximately 36 h of insulin infusion, the daily plasma glucose profile improved, the serum creatinine and electrolyte levels normalized, the ketoacidosis resolved, and the gastro-intestinal symptoms also improved. Thus, we shifted the patient’s insulin therapy to multiple daily injections.
The patient underwent upper gastrointestinal endoscopy for persistent dysphagia, which showed a circumferential necrosis of the middle and distal portions of the esophagus (starting from 24 to 40 cm from the incisors) with an abrupt transition at the gastro-esophageal junction (Figure 1A-C). No endoscopic findings of suspected esophageal metaplasia and gastro-duodenal pathology were observed. A chest computed tomography revealed a thickened distal esophagus but excluded the presence of esophageal perforation or mediastinal infection/abscess. The patient was then treated with high-dose intravenous proton-pump inhibitors and albumin infusion and was kept initially nil-per-os (a total parenteral nutrition was maintained for approximately 15 d). Then, he was treated with a semi-liquid diet for the subsequent 5-6 d.
Figure 1.
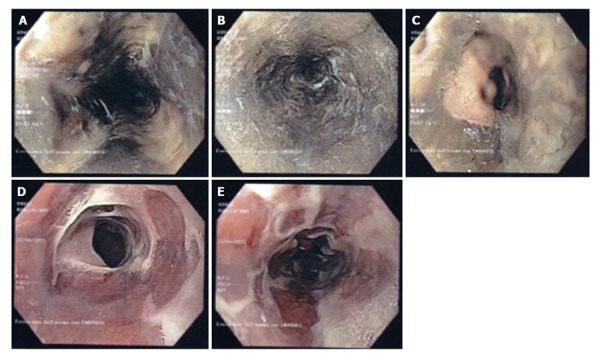
Upper gastrointestinal endoscopy findings. A-C: First upper gastrointestinal endoscopy: Typical endoscopic findings of AEN; D and E: Third upper gastrointestinal endoscopy: Improvement/resolution of AEN after treatment. Complete disappearance of the black mucosa with whitish membranes covering the subepithelial surface of the esophagus. AEN: Acute esophageal necrosis.
A second gastrointestinal endoscopy, performed approximately 1 wk after diagnosis, was essentially unchanged. Another gastrointestinal endoscopy, performed approximately 15 d after diagnosis, showed a marked reduction in the esophageal necrosis and a loss of the superficial epithelial lining (Figure 1D and E). An esophageal biopsy revealed the presence of tissue necrosis, granulated tissue and marked leukocyte infiltration with hemosiderosis.
After 4 wk, the patient was discharged from the hospital without any clinical gastro-intestinal symptoms and was prescribed lansoprazole 60 mg/d and metformin 2 g/d. Approximately three weeks after the hospital discharge, the patient underwent esophageal X-rays, owing to the appearance of dysphagia, which revealed the presence of a stenosis (with a length of about 10 cm) in the middle and distal third of the esophagus with a luminal diameter of about 1 cm. The patient underwent three consecutive sessions of esophageal endoscopic dilation with through-the-scope (TTS) balloons (maximum TTS-balloon diameter of 15 mm) over a period of three months with a complete resolution of dysphagia. An esophageal biopsy performed during the procedures was normal and excluded the presence of dysplasia and Barrett’s esophagus.
DISCUSSION
AEN or black esophagus syndrome is a rare acute medical condition. Overall, fewer than 90 cases of AEN have been reported in the literature until 2007[1], making the diagnosis of this esophageal disorder very uncommon. Diagnosis of AEN is made endoscopically in an appropriate clinical setting by observing a striking diffuse circumferential black appearance of the esophageal mucosa, almost universally affecting the distal portion of the esophagus and stopping at the Z-line[1,2]. The aetiology of AEN is multifactorial, resulting from a combination of tissue hypoperfusion, massive reflux of gastric secretions, and diminished mucosal defences in the esophagus. Generally, AEN is more common in elderly male patients with multiple serious co-morbidities, and it characteristically presents with signs of upper gastrointestinal haemorrhage (occurring in up to 90% of cases). Major risk factors for AEN include male sex, older age, alcohol abuse, hypertension, chronic kidney disease, malnourishment, and vascular diseases[1,2]. Differential diagnosis includes malignant melanoma, melanocytosis, coal dust deposition, acanthosis nigricans of the esophagus, and caustic ingestion. The overall prognosis of AEN is poor, and nearly one third of patients succumb to the underlying critical illness[1,2]. Although the therapeutic modalities are not currently standardized, the aggressive treatment of the underlying medical conditions with haemodynamic resuscitation, total parenteral nutrition and acid suppression with high-dose intravenous proton-pump inhibitors should be immediately instituted in all patients with suspected or established AEN. The most common complications of AEN are esophageal stenosis and stricture formation; these complications occur in up to 15% of patients and usually appear as early as 1 to 3 wk after the diagnosis[1,2].
In the largest multicentre series of reviewed cases of AEN, Gurvits et al[3] have recently found that nearly 90% of the patients are moderately hyperglycaemic. However, although some previous case reports had also shown a possible association between AEN and DKA[4,5], none of the patients included in this recent multicentre case series showed any evidence of DKA at the time of hospital admission[3].
We believe that our case report is clinically relevant because it further supports the possibility that DKA may be associated with the occurrence of AEN. Notably, our case report also shows that AEN can occur in a middle-aged male patient with DKA without any clinical signs of hematemesis, coffee ground emesis or melena and the coexistence of important co-morbidities (except for the presence of hypertension).
Thus, although to date DKA has been rarely reported as a possible cause of AEN, it is essential to diagnose AEN in patients with DKA as a potential cause of mortality or morbidity. Indeed, the early recognition and management of AEN will result in improved clinical outcomes as the medical world gets more familiar with this rarely diagnosed and important clinical syndrome.
COMMENTS
Case characteristics
A 50-year-old white man with type 2 diabetes and hypertension was admitted to the Emergency Department with dysphagia, vomiting, polyuria, polydipsia and low-grade fever.
Clinical diagnosis
The diagnosis of black esophagus syndrome, also known as acute esophageal necrosis, is made endoscopically by observing a striking diffuse circumferential black appearance of the esophageal mucosa, almost universally affecting the distal portion of the esophagus and stopping at the Z-line.
Differential diagnosis
Differential diagnosis includes malignant melanoma, melanocytosis, coal dust deposition, acanthosis nigricans of the esophagus, and caustic ingestion.
Laboratory diagnosis
Most laboratory data are normal, except for moderate leukocytosis, hypoalbuminemia and anemia (especially if upper gastrointestinal haemorrhage is also present).
Imaging diagnosis
The diagnosis of black esophagus syndrome is made endoscopically and is typically characterized by a circumferential black-appearing esophageal mucosa, which mostly affects the distal portion of the esophagus and stops abruptly at the gastro-esophageal junction.
Pathological diagnosis
Esophageal biopsy shows the presence of tissue necrosis, granulation tissue and marked leukocyte infiltration with hemosiderosis.
Treatment
Although, to date, therapeutic modalities are not standardized, the aggressive treatment of the underlying medical conditions with haemodynamic resuscitation, total parenteral nutrition and acid suppression with high-dose intravenous proton-pump inhibitors should be immediately started in all patients with suspected or established black esophagus syndrome.
Related reports
Black esophagus syndrome is a rare acute medical condition. Very few studies have reported an association between black esophagus syndrome and diabetic ketoacidosis.
Term explanation
The black esophagus syndrome is a rare pathologic condition typically characterized by circumferential black-appearing esophageal mucosa, which mostly affects the distal portion of the esophagus and stops abruptly at the gastro-esophageal junction.
Experiences and lessons
The black esophagus syndrome is an under-recognized disease and there is need of increased attention to the presence of this acute esophageal disorder.
Peer-review
This is an interesting case report of a rare esophageal acute disease.
Footnotes
Institutional review board statement: The study was reviewed and approved by the local Institutional Review Board (Comitato etico per la sperimentazione clinica delle Province di Verona e Rovigo).
Informed consent statement: The patient involved in this study gave his informed written consent prior to study enrollment, authorizing the use and disclosure of his protected health information.
Conflict-of-interest statement: All the authors of the article have no conflicts of interest to disclose.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 31, 2015
First decision: October 14, 2015
Article in press: December 4, 2015
P- Reviewer: Campo SMA, Goral V, Kozarek R, Worrell SG S- Editor: Qi Y L- Editor: A E- Editor: Liu SQ
References
- 1.Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29–38. doi: 10.1007/s00535-006-1974-z. [DOI] [PubMed] [Google Scholar]
- 2.Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol. 2010;16:3219–3225. doi: 10.3748/wjg.v16.i26.3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gurvits GE, Cherian K, Shami MN, Korabathina R, El-Nader EM, Rayapudi K, Gandolfo FJ, Alshumrany M, Patel H, Chowdhury DN, et al. Black esophagus: new insights and multicenter international experience in 2014. Dig Dis Sci. 2015;60:444–453. doi: 10.1007/s10620-014-3382-1. [DOI] [PubMed] [Google Scholar]
- 4.Kim YH, Choi SY. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol. 2007;13:5662–5663. doi: 10.3748/wjg.v13.i42.5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Talebi-Bakhshayesh M, Samiee-Rad F, Zohrenia H, Zargar A. Acute Esophageal Necrosis: A Case of Black Esophagus with DKA. Arch Iran Med. 2015;18:384–385. [PubMed] [Google Scholar]


