Abstract
Background:
Studies suggest that mindfulness-based interventions can improve anxiety, depression and stress in patients with multiple sclerosis (MS). However, no study investigated the effectiveness of this method in patients with a combination of problems such as depression, anxiety and stress simultaneously. However, comorbidities of depression and anxiety in MS are prevalent.
Objectives:
This study aimed to assess the effects of mindfulness-based stress reduction (MBRS) on anxiety, depression and stress in women with multiple sclerosis.
Patients and Methods:
This randomized controlled clinical trial was performed in 2013 in Ahvaz MS Society. Forty eight patients were selected by convenient sampling and randomly assigned in experimental and control groups. The patients in the two groups filled out depression, anxiety and stress scale (DASS-21) at initiation of study, 8 weeks later and 1 month after the end of intervention. The experimental group received 8 sessions of MBRS, while the control group treated as usual. Finally, data of 40 patients analyzed using t-test, chi square and repeated measures analysis of variance.
Results:
In the MBSR group, the mean depression, anxiety and stress were reduced significantly (P < 0.001). The mean depression score was 8.35 ± 1.78 before the intervention and reduced to 4.80 ± 0.83 and 4.45 ± 0.60 after the intervention and follow-up (P < 0.001). Also the mean anxiety score was 8.90 ± 1.97 before the intervention, which was significantly reduced to 4.70 ± 1.38 and 4.55 ± 0.99 after the intervention and follow-up (P < 0.001). The mean stress score was also 8.80 ± 2.35 before treatment and 4.80 ± 1.67 and 4.70 ± 1.34 after the intervention and follow-up (P < 0.001).
Conclusions:
This study showed that MBSR training can reduce mean depression, anxiety and stress scores in patients with MS. These findings suggest that MBSR is useful for psychological problems such as depression, anxiety and stress in patients with MS.
Keywords: Multiple Sclerosis, Mindfulness, Depression, Anxiety, Stress
1. Background
Multiple sclerosis (MS) is a neurologic illness in which the myelin covering the central nervous system is injured (1). Chronic and disabling diseases such as MS have numerous psychiatric consequences such as anxiety and depression (2). According to the Iranian Multiple Sclerosis Society, in 2013 there were about 70000 patients with MS in Iran (3). The progression of MS is accompanied with series of physical and psychological problems that affect all of daily activities such as dressing, taking a bath and self-care and eventually reduces individual’s autonomy, psychological wellbeing and quality of life (QOL) (4). Studies have shown high levels of anxiety, stress and mood disorders including depression in these patients. It is reported that more than a third of patients with MS have anxiety disorders (5, 6). Moreover, about 10% and 8.6% of them have panic disorder and obsessive compulsive disorder, respectively (5, 6). A recent study reported that lifetime prevalence of major depressive disorder in patients with MS is 22.8% to more than 50% (2). Another study reported that approximately 48% of patients with MS experience anxiety, stress and depression in the first year after the diagnosis (7). Individuals with anxiety disorder are more likely to be female, have a history of depression, drink excessively, have higher levels of social stress and contemplated suicide (8).
Presently no cure exists for MS. A combination of pharmacological and non-pharmacological managements is usually implemented in an individualized, organized, and rational program to delay the progression of the disease, manage chronic symptoms, and treat acute exacerbations (9). Considering the adverse effects of medications, non-pharmacological methods are suggested for reducing anxiety and stress in patients with MS. Non-pharmacological therapies such as exercise, hydrotherapy, nutritional therapy, medicinal plants, energy therapy, occupational therapy, acupuncture, acupressure, relaxation therapy and meditation are among the methods used to reduce physical and psychological symptoms of MS (9-11). One of the new treatments in the field of psychotherapy is mindfulness-based stress reduction (MBSR), which is under category of meditation. This approach was introduced by Kabat-Zinn (12) in the 1970s and since then, it was applied in many problems such as coping with stress, illness and pain in patients with heart disease, cancer, AIDS (acquired immune deficiency syndrome), chronic pain, stress-related gastrointestinal problems, headaches, high blood pressure, sleep disorders, depression, and anxiety (12-16). However, some studies reported that MBSR has large effects on stress reduction, but is moderately effective on anxiety, depression and QOL, and has little effects on burnout (17). Moreover, only a few studies are available on the effectiveness of MBSR in patients with MS. These studies showed that MBRS can improve psychological symptoms of patients (18-20). These studies suggest that mindfulness-based interventions can improve QOL, anxiety, depression, physical health, fatigue, pain, and health-related QOL in patients with MS and that the effects lasted up to 6 months after the intervention. However, each of these studies investigated only the effects of MBRS of isolated variables and no study investigated the effectiveness of this method in patients with a combination of problems such as depression, anxiety and stress simultaneously. However, comorbidities of depression and anxiety in MS are prevalent. In addition, some of the studies conducted on patients with MS had no control group (21, 22).
2. Objectives
This study aimed to assess the effects of mindfulness-based stress reduction on anxiety, depression and stress in women with multiple sclerosis in Ahvaz.
3. Materials and Methods
3.1. Participants and Procedure
This randomized controlled clinical trial was performed in 2014 in Ahvaz MS Society. The study population included all female patients aged 20 - 50 years with MS referred to Ahvaz MS society from January to June 2014.
The sample size was calculated based on a previous study in which Grossman et al. investigated the impact of mindfulness training on QOL, depression and fatigue in patients with MS and reported that mean and standard deviation of depression before the intervention was 16.33 ± 10.46 and changed to 5.29 ± 7.07 after the intervention (23). According to 95% confidence and test power of 90%, using Cohen’s formula, 15 subjects were estimated to be needed in each group. However, we recruited 24 patients in each group to achieve more reliable results.
After sample size calculation, reviewing the files of patients with MS in Ahvaz MS society, 48 patients with inclusion criteria were selected by convenient sampling. Then patients were called and invited to participate in the study. If a patient agreed to participate, he or she was invited to attend the study briefing session and if not, another patient was selected similarly. Then, using a random number table, they were assigned into experimental (MBSR) and control groups. The inclusion criteria were having a medical diagnosis of MS, having a minimum literacy of intermediate school level, not having a psychotic disorder (according to the structural clinical interview for DSM disorders for Axis I; SCID-I administered by a clinical psychologist) and receiving no regular psychotherapy during the last 6 months. Exclusion criteria were having a relapsing MS and absence of more than two therapeutic sessions.
3.2. Instruments
The study instrument had two parts. The first part included three questions on demographic information about age, education level and marital status. The second part was the 21-item Depression, Anxiety and Stress Scale (DASS-21). The DASS-21 was made in 1995 and has three subscales of depression, anxiety and stress (24). Each subscale consists of 7 items. Items 3, 5, 10, 13, 16, 17 and 21 are related to depression; anxiety subscales are items 2, 4, 7, 9, 15, 19 and 20 and stress subscales are items 1, 6, 8, 11, 12, 14 and 18. Each item has a four-point Likert scale response between 0 (never) and 3 (always). Therefore, each subscale has scores from 0 to 21. Higher scores in each subscale show a higher degree of anxiety, depression and stress. Evidence suggests that the convergent and discriminant validity of DASS are sufficient (24). The validity of Iranian version of DASS-21 was previously confirmed. Its reliability was also evaluated through Cronbach’s alpha coefficient of 0.80, 0.76 and 0.77 for depression, anxiety and stress subscales, respectively (25).
3.3. Procedures
In addition to the usual treatments for MS, the experimental group received eight weeks of MBSR training weekly, according to the protocol developed by Kabat-Zinn (12) and Segal (26). The outline of the protocol is shown in Table 1. However, the control group only received treatments as usual (TAU). The DASS-21 was administered to the experimental group at pretest (before the intervention), posttest (at the end of intervention) and two months after the end of intervention (follow-up). Patients in the TAU group were also invited to Ahvaz MS society to respond to the DASS-21 simultaneous with the MBSR group. Patients in the both groups completed the demographic questionnaire at baseline. Both groups were also received their routine drug treatments. All the MBRS sessions were held in Ahvaz MS Society and administered by a trained psychologist. Each session lasted for 120 minutes from 10 to 12 o’clock of Tuesdays. For participants who had missed one or two sessions, additional sessions were held. After finishing the study, all patients in the control group were also contacted and invited to voluntarily attend in MBSR sessions similar to those the experimental group had passed.
Table 1. The Outline of the Mindfulness-Based Stress Reduction (According to Kabat-Zinn (12) and Segal et al. (26)).
| Session | Contents of Each Session |
|---|---|
| 1 | Introducing the rules of group such as confidentiality, raisin exercise (Eating raisins with the full involvement of the senses of smell, taste, sight and touch), body scan practice (subjective evaluation of body parts, identifying stress and its relaxation), re-breathing training |
| 2 | Body scan practice, pleasant event calendar (writing daily events that induced positive emotions such as joy, pride and praise), being mindful in all actions (doing tasks with focus on them through the five senses) |
| 3 | Mindful watching and hearing (focusing of watching and hearing without judgment), sitting meditation, three-minute breathing space, mindful walking, and unpleasant event calendar (writing daily events that induced negative emotions such as anxiety, sad, hate, anger, etc.) |
| 4 | Mindful watching and hearing, sitting meditation, definition of stress and its related body systems, responding to stress versus reaction to it (not acting immediately and rapidly when experiencing unpleasant emotions, such as anxiety) |
| 5 | Sitting meditation, breathing space, mindful metaphors, introducing the concept of “acceptance”, introducing anxiety worksheet |
| 6 | Sitting meditation, monitoring the emotions and thoughts, strengthen observer self (observing the internal events such as thoughts, emotions, and bodily sensation without stocking on them) |
| 7 | Behavioral activation (identifying pleasure and important daily activities and doing them systematically), identifying actions to do in low-mood periods |
| 8 | Review all prior sessions and their results for everyone |
3.4. Ethical Considerations
The Research Ethics Committee of Azad University, Khorasgan Branch approved this study (code of Ethical Review Committee was 25/5/1/3551 and the code of the project was 486207). All participants were asked to sign an informed consent form and assured that their personal data would be confidential. Moreover, all participants were aware of the voluntary nature of their participation in the study and the right to withdraw from the study at any point. In addition, after completion of the study, the control group was invited to attend in similar MBSR training session.
3.5. Data Analysis
The repeated measures analysis of variance was used to compare MBSR and TAU groups regarding depression, anxiety and stress. Moreover, t-test was used to compare significant differences between mean age of the two groups. Chi-square test was used to compare other demographic variables such as marital status and education level in the two groups. P value less than 0.05 was considered statistically significant in all tests.
4. Results
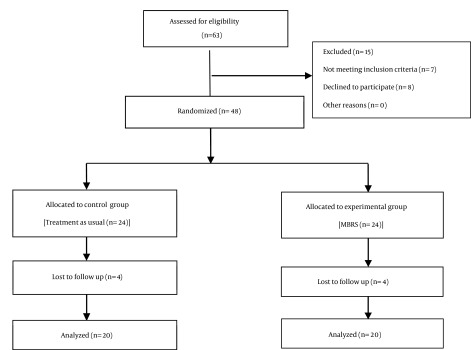
Table 2 shows demographic characteristics of the subjects. Among 48 subjects, 4 ones were excluded from each group because of missing more than two sessions and not completing the DASS-21 (Figure 1).
Table 2. Demographic Characteristics of Patients With MS in MBSR and TAU Groupsa.
| Variable | MBSR | TAU | P Value |
|---|---|---|---|
| Age | 5.77 ± 25.70 | 2.39 ± 24.85 | .54b |
| Education level | .88c | ||
| High school | 10 (25) | 11 (27.5) | |
| Bachelor | 10 (25) | 9 (22.5) | |
| Marital status | .99c | ||
| Married | 10 (25) | 10 (25) | |
| Single | 10 (25) | 10 (25) |
Abbreviations: MBSR, mindfulness-based stress reduction; TAU, treatment as usual.
aData are presented as mean ± SD or No. (%).
bt-test.
cChi-square test.
Figure 1. The Study Flow Diagram.
No significant differences were observed between MBSR and TAU groups for demographic variables (Table 2).
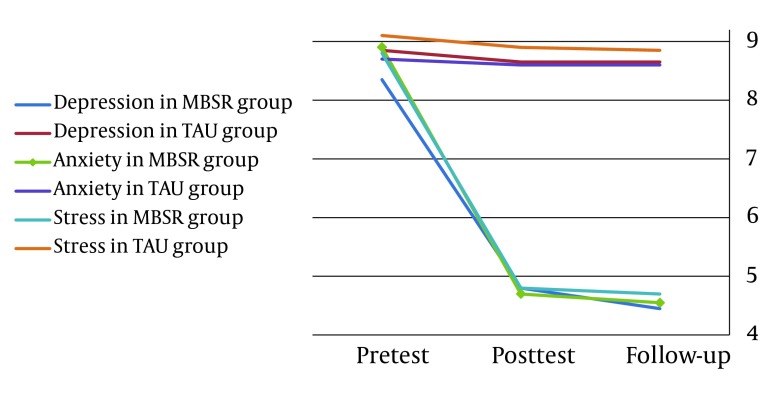
Table 3 provides mean scores of dependent variables (depression, anxiety and stress) and comparison of them at pretest, posttest, and two-month follow-up. It shows that the mean depression, anxiety and stress scores in MBSR group were decreased in 2 phases (posttest and follow- up) compared to pretest. Although a little decrease was occurred in scores of dependent variables in the TAU group, but they were not significant and did not continue in follow-up. Figure 2 shows changes in depression, anxiety and stress mean scores in TAU and MBSR groups in 3 consecutive measurements.
Table 3. Comparison of Depression, Anxiety and Stress at Pretest, Posttest and Follow-Up in the Two Groupsa.
| Outcome Measure | Pre-Test | Post-Test | Follow-Up | P Value | |
|---|---|---|---|---|---|
| Time | Time × Group | ||||
| Depression | < .001 | < .001 | |||
| MBSR | 8.35 ± 1.78 | 4.80 ± 0.83 | 4.45 ± 0.60 | ||
| TAU | 8.85 ± 1.64 | 8.65 ± 1.63 | 8.65 ± 1.34 | ||
| Anxiety | <.001 | < .001 | |||
| MBSR | 8.90 ± 1.97 | 4.70 ± 1.38 | 4.55 ± 0.99 | ||
| TAU | 8.70 ± 1.92 | 8.60 ± 1.66 | 8.60 ± 1.56 | ||
| Stress | < .001 | < .001 | |||
| MBSR | 8.80 ± 2.35 | 4.80 ± 1.67 | 4.70 ± 1.34 | ||
| TAU | 9.10 ± 2.04 | 8.90 ± 1.71 | 8.85 ± 1.95 | ||
Abbreviations: MBSR, mindfulness-based stress reduction; TAU, treatment as usual.
aData are presented as mean ± SD.
Figure 2. Changes in Depression, Anxiety and Stress Mean Scores in TAU and MBSR Groups.
Mauchly’s test of sphericity showed the null hypothesis that the error covariance matrix of the orthonormalized transformed dependent variables is proportional to an identity matrix was not confirmed (Mauchly’s W = .551, Sig = 0.061). However, there was an interaction between group membership and therapeutic phase (or time) by Hotelling’s trace test (F = 33.681, Sig < 0.001). Changes in variables such as depression, anxiety and stress have been shown in three-phase treatment by Figure 2.
5. Discussion
This study showed that MBSR can reduce depression, anxiety and stress in patients with MS. These findings are consistent with the results of other previous studies (14-16) and revealed benefits of MBRS in patients with MS.
Our study showed that MBSR can reduce depression in patients with MS. Depression is linked to neurological changes in the brain structure and function in persons with MS (27). Mindfulness leads to the activation of the area of the brain that is associated with positive emotions and affects immunization function (28). In addition, mindfulness may reduce stress and mood dysregulation by empowering positive reappraisal and emotion regulation skills (29).
Mindfulness training through different mechanisms can reduce anxiety, depression and stress in patients with MS. First, one of the important causes of these psychological states is anxiety and depression due to pain that patients experience. In meditation, a basic technique in MBSR, patients are trained to focus on feeling pain in the body and joints without emotional reactions to the pain, just observing it. The observing can reduce emotional responses (such as anxiety and depression) that evoke pain in MS (12) and mutually exacerbate their pain and lack of mobility. MBSR allows thoughts to come and go easily, without any attempt to alter, diminish or expand them. Through mindfulness training, participants learn to see their mental events (depression, anxiety and stress) as transient not reality. In this way, participants are confronted with the contents of positive and negative thoughts, but they are not drowned in thoughts of future or past that develop depression and anxiety/stress, respectively. MBSR can create this ability through components such as acceptance of internal experiences (thoughts, depression, anxiety, stress and pain) and non-judgmental awareness to them (30). MBSR through every moment of awareness affects patient acceptance of internal experiences, which helps him or her decrease habitual problematic patterns of thinking, feeling and behavior. It shows new ways to respond and cope with internal and external problems (31). Second, focusing on breathing was used as a tool to live in the present and detach the person from problematic internal experiences. In this way, patients trained to stop the cycle of rumination, depression (32), worry, anxiety and stress. Third, mindfulness-based stress reduction program teaches participants how to focus their awareness to everyday life that is full of pleasure and unpleased events. Mindfulness exercises are used throughout a day, so people can show good response to environmental stressors (12). Practicing the mindfulness skills increase the ability of participants to tolerate negative emotional states (such as depression and anxiety) and enable to deal effectively with them (32). Forth, MBSR can decrease depression, anxiety and stress by behavioral activation in patients with MS. MBSR helps people to do physical activity. For example, in one of the exercises called yoga, a person does stretching movements in the body, which increase awareness to the body and its status as a form of appropriate exercise for patients. The mindfulness exercises such as walking with mindfulness (mindful walking) are forms of behavioral activation. In mindful walking, patient by focusing on own individual five senses can decrease anxious and depressive thoughts and emotions and increase pleasure. In a broader perspective, the treatment can enhance the QOL in patients.
Our study showed that patients with MS can reduce their depression, anxiety and stress by MBSR training. Moreover, MBSR is suggested as a suitable therapy for reducing depression, anxiety and stress and can be used as a low-cost and accessible treatment for all medical staff working with MS patients, particularly nurses and psychiatric nurses.
Limitations of the present study were using only female for sample. The small sample size and short duration of follow-up were other limitations in this study. Further studies with larger sample sizes and longer follow-up and in male patients are recommended.
Acknowledgments
Authors are grateful to staff of Ahvaz MS Society and participants. This study was registered at the Iranian registry for clinical trial with registry number of IRCT201507087227N5.
Footnotes
Authors’ Contribution:Bentolhoda Kolahkaj administered the treatment plan and interpreted clinical data. Fatemeh Zargar designed the treatment plan and drafted the manuscript.
Financial Disclosure:None declared.
Funding/Support:None declared.
References
- 1.Satoh J. Molecular network of ChIP-Seq-based NF-kappaB p65 target genes involves diverse immune functions relevant to the immunopathogenesis of multiple sclerosis. Mult Scler Relat Disord. 2014;3(1):94–106. doi: 10.1016/j.msard.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Salehpoor G, Rezaei S, Hosseininezhad M. Quality of life in multiple sclerosis (MS) and role of fatigue, depression, anxiety, and stress: A bicenter study from north of Iran. Iran J Nurs Midwifery Res. 2014;19(6):593–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Harizchi ghadim S, Ranjbar kuchsaryi F, Talebi M, Zakaria M. Effects of ''Written Emotional Expression" on Anxiety and Depression in patients with Multiple Sclerosis. Iran J Neurol. 2013;8(25):465–75. [Google Scholar]
- 4.Garcia-Burguillo MP, Aguila-Maturana AM. [Energy-saving strategies in the treatment of fatigue in patients with multiple sclerosis. A pilot study]. Rev Neurol. 2009;49(4):181–5. [PubMed] [Google Scholar]
- 5.Bruce JM, Lynch SG. Multiple sclerosis: MS treatment adherence--how to keep patients on medication? Nat Rev Neurol. 2011;7(8):421–2. doi: 10.1038/nrneurol.2011.106. [DOI] [PubMed] [Google Scholar]
- 6.da Silva AM, Vilhena E, Lopes A, Santos E, Goncalves MA, Pinto C, et al. Depression and anxiety in a Portuguese MS population: associations with physical disability and severity of disease. J Neurol Sci. 2011;306(1-2):66–70. doi: 10.1016/j.jns.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 7.Wood B, van der Mei IA, Ponsonby AL, Pittas F, Quinn S, Dwyer T, et al. Prevalence and concurrence of anxiety, depression and fatigue over time in multiple sclerosis. Mult Scler. 2013;19(2):217–24. doi: 10.1177/1352458512450351. [DOI] [PubMed] [Google Scholar]
- 8.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13(1):67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- 9.Wright S, Yadav V, Bever C, Bowen J, Bowling A, Weinstock-Guttman B, et al. Summary of evidence-based guideline: complementary and alternative medicine in multiple sclerosis: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2014;83(16):1484–6. doi: 10.1212/01.wnl.0000455935.13606.91. [DOI] [PubMed] [Google Scholar]
- 10.Kes VB, Cesarik M, Matovina LZ, Zavoreo I, Coric L, Drnasin S, et al. The role of complementary and alternative medicine in therapy of multiple sclerosis. Acta Clin Croat. 2013;52(4):464–71. [PubMed] [Google Scholar]
- 11.Masullo L, Papas MA, Cotugna N, Baker S, Mahoney L, Trabulsi J. Complementary and alternative medicine use and nutrient intake among individuals with multiple sclerosis in the United States. J Community Health. 2015;40(1):153–60. doi: 10.1007/s10900-014-9913-z. [DOI] [PubMed] [Google Scholar]
- 12.Kabat-Zinn J. Bringing mindfulness to medicine: an interview with Jon Kabat-Zinn, PhD. Interview by Karolyn Gazella. Adv Mind Body Med. 2005;21(2):22–7. [PubMed] [Google Scholar]
- 13.Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010;68(1):29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Martin-Asuero A, Garcia-Banda G. The Mindfulness-based Stress Reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span J Psychol. 2010;13(2):897–905. doi: 10.1017/s1138741600002547. [DOI] [PubMed] [Google Scholar]
- 15.Geary C, Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. J Altern Complement Med. 2011;17(10):939–44. doi: 10.1089/acm.2010.0335. [DOI] [PubMed] [Google Scholar]
- 16.Serpa JG, Taylor SL, Tillisch K. Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med Care. 2014;52(12 Suppl 5):S19–24. doi: 10.1097/MLR.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 17.Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res. 2015;78(6):519–28. doi: 10.1016/j.jpsychores.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Burschka JM, Keune PM, Oy UH, Oschmann P, Kuhn P. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol. 2014;14:165. doi: 10.1186/s12883-014-0165-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simpson R, Booth J, Lawrence M, Byrne S, Mair F, Mercer S. Mindfulness based interventions in multiple sclerosis--a systematic review. BMC Neurol. 2014;14:15. doi: 10.1186/1471-2377-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pakenham KI, Samios C. Couples coping with multiple sclerosis: a dyadic perspective on the roles of mindfulness and acceptance. J Behav Med. 2013;36(4):389–400. doi: 10.1007/s10865-012-9434-0. [DOI] [PubMed] [Google Scholar]
- 21.Nordin L, Rorsman I. Cognitive behavioural therapy in multiple sclerosis: a randomized controlled pilot study of acceptance and commitment therapy. J Rehabil Med. 2012;44(1):87–90. doi: 10.2340/16501977-0898. [DOI] [PubMed] [Google Scholar]
- 22.Pakenham KI. Effects of Acceptance and Commitment Therapy (ACT) Training on Clinical Psychology Trainee Stress, Therapist Skills and Attributes, and ACT Processes. Clin Psychol Psychother. 2014. doi: 10.1002/cpp.1924. [DOI] [PubMed] [Google Scholar]
- 23.Grossman P, Kappos L, Gensicke H, D'Souza M, Mohr DC, Penner IK, et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 2010;75(13):1141–9. doi: 10.1212/WNL.0b013e3181f4d80d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 25.Samani S, Jokar B. Validity and reliability of the short form Depression, Anxiety and Stress Scale. J Soc Sci and Humanit Univ Shiraz. 2008;23(3):65–77. [Google Scholar]
- 26.Segal ZV, Teasdale JD, Williams JM, Gemar MC. The mindfulness based cognitive therapy adherence scale: inter rater reliability, adherence to protocol and treatment distinctiveness. Clin Psychol Psychother. 2002;9(2):131–8. doi: 10.1002/cpp.320. [DOI] [Google Scholar]
- 27.Passamonti L, Cerasa A, Liguori M, Gioia MC, Valentino P, Nistico R, et al. Neurobiological mechanisms underlying emotional processing in relapsing-remitting multiple sclerosis. Brain. 2009;132(Pt 12):3380–91. doi: 10.1093/brain/awp095. [DOI] [PubMed] [Google Scholar]
- 28.Bedard M, Felteau M, Marshall S, Cullen N, Gibbons C, Dubois S, et al. Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: results from a randomized controlled trial. J Head Trauma Rehabil. 2014;29(4):E13–22. doi: 10.1097/HTR.0b013e3182a615a0. [DOI] [PubMed] [Google Scholar]
- 29.Omidi A, Zargar F. Effect of mindfulness-based stress reduction on pain severity and mindful awareness in patients with tension headache: a randomized controlled clinical trial. Nurs Midwifery Stud. 2014;3(3):e29655. doi: 10.17795/nmsjournal21136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zargar F, Farid AA, Atef-Vahid MK, Afshar H, Omidi A. Comparing the effectiveness of acceptance-based behavior therapy and applied relaxation on acceptance of internal experiences, engagement in valued actions and quality of life in generalized anxiety disorder. J Res Med Sci. 2013;18(2):118. [PMC free article] [PubMed] [Google Scholar]
- 31.Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16(17):1893–7. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baer RA. Self-focused attention and mechanisms of change in mindfulness-based treatment. Cogn Behav Ther. 2009;38 Suppl 1:15–20. doi: 10.1080/16506070902980703. [DOI] [PubMed] [Google Scholar]