Abstract
Objective
Robotic prostatectomy has rapidly disseminated over the past decade. How managed care, thought by many to be a barrier to new technology, influences the dissemination of robotics is unknown. We sought to better understand the relationship between a market’s managed care penetration and the dissemination of robotic prostatectomy.
Methods
We used SEER-Medicare data from 2003 through 2007 to identify men ≥ 66 years of age treated with radical prostatectomy for prostate cancer. We categorized Health Service Areas (HSAs) according to the degree of managed care penetration (i.e., low vs. high). We assessed adoption of robotic prostatectomy and utilization among adopting HSAs using Cox proportional-hazards and Poisson regression models, respectively.
Results
Compared with markets with little managed care, highly penetrated markets had more racial diversity (24% vs. 15% non-white, p<0.01), higher population densities (1987 vs. 422 people/square mile, p<0.01), and higher median incomes ($49,374 vs. $36,236, p<0.01). Robotic prostatectomy adoption and utilization increased over time in both HSA categories. Compared with low managed care markets, those with high managed care adopted robotic prostatectomy more rapidly (e.g., probability 0.37 [low] vs. 0.52 [high] in 2007; p<0.01). However, the post-adoption utilization of robotic prostatectomy was constrained in these highly penetrated markets (e.g., probability 0.66 [low] vs. 0.52 [high] in 2007; p<0.01).
Conclusions
High managed care penetration was associated with more rapid robotic prostatectomy adoption. However, once adopted, utilization increased more slowly in these markets. Understanding this paradox is important, as more technologies are unveiled in an increasing cost-conscious healthcare environment.
Keywords: prostate cancer, robotic prostatectomy, managed care, adoption, utilization
INTRODUCTION
Robotic prostatectomy has disseminated rapidly for the treatment of patients with localized prostate cancer. Although clinical trials establishing its superiority over conventional surgery are lacking, robotic prostatectomy is widely believed to have numerous advantages, including reduced blood loss, faster convalescence and shorter hospital stays.1,2 For these and other reasons, robotic surgery has diffused rapidly over the last decade, making it the most common surgical approach for prostate cancer.3
Unfortunately, not all patients have equal access to robotic surgery and its associated benefits. Indeed, some worry that financial disincentives inherent in capitated payments may constrain the dissemination of novel, and potential beneficial, therapeutic technologies like robotic surgery.4 On one hand, acquisition and maintenance costs associated with robotic surgery invariably lead to higher episode costs per patient or reduced margins for the hospital,5,6 both of which may preclude its adoption in highly cost-sensitive markets. Alternatively, pressures to attract the best physicians and increase market share may promote adoption independent of the economic constraints affiliated with capitation.7
Understanding the impact of managed care on the dissemination of a new technology, such as robotic surgery, is important for two reasons. First, payment for healthcare appears to be evolving towards improving value (i.e., higher quality and lower cost) as opposed to strictly a fee-for-service arrangement. Indeed, today’s accountable care organizations are based on many of the same principles of managed care.8,9 Second, new cancer-related technologies on the horizon will face similar obstacles to diffusion in an increasing cost-conscious healthcare environment.
METHODS
Data Sources and Study Population
We used the Surveillance, Epidemiology, and End Results (SEER)-Medicare linked data to identify men aged 66 years or older diagnosed with prostate cancer between 2003 and 2007. This nationally representative population-based registry consists of all incident cancers occurring in these areas, which collectively comprise approximately 26% of the U.S. population.10 Next, we identified men undergoing radical prostatectomy within the first 12 months of diagnosis using the MEDPAR (Medicare Provider Analysis and Review) and carrier files. We further identified robotic prostatectomy patients using the Healthcare Common Procedure Coding System (HCPCS) code 55866. Only fee-for-service beneficiaries eligible for both Medicare Parts A and B from 12 months prior to diagnosis until 12 months after diagnosis were included in the study. Men aged 65 years were excluded to ensure accurate comorbidity estimation using Medicare claims for the 12-month period prior to diagnosis.11 Using these criteria, our study population consisted of 12,351 patients treated with radical prostatectomy for localized prostate cancer.
Identifying Health Care Markets
As described previously,12,13 we divided the SEER registries into healthcare markets using 164 Health Service Area (HSA) boundaries specified by the Area Resource File. Briefly, HSAs were originally defined by the National Center for Health Statistics as a single county or cluster of contiguous counties that are relatively self-contained with respect to hospital care.14 We excluded 4 HSAs because no patients from those markets underwent any type of surgery for prostate cancer during the study period.
Using the Area Resource File, we characterized each HSAs level of managed care penetration. In the Area Resource File, managed care penetration was defined as the number of Medicare enrollees in managed care plans (numerator) divided by the number of eligible Medicare beneficiaries (denominator). Based on national trends in managed care enrollment among Medicare beneficiaries during the study period,15 prior studies,16,17 and the assessment of different managed care penetration thresholds, we sorted HSAs into two levels of managed care penetration: low (≤10%) and high (>10%).
Outcomes
To examine the association of managed care penetration and robotic prostatectomy dissemination, we first characterized the probability of adopting robotic prostatectomy (i.e., a healthcare market that acquires the ability to perform a prostatectomy robotically). To account for measurement error, we only considered a market to be an adopter if it contained 5 or more patients treated with robotic prostatectomy within a 12-month period. The time of adoption was backdated to the first claim for robotic prostatectomy. Since managed care penetration may influence the diffusion of robotic prostatectomy within an HSA after it acquires robotic capabilities, we next examined the utilization among the adopting HSAs (n=67). For this measurement, the numerator represented the number of men treated with robotic prostatectomy and the denominator represented the number of men treated with any prostatectomy for prostate cancer. For both outcomes, the HSA was the unit of analysis.
Statistical Analysis
We first compared aggregate patient and HSA population characteristics according to managed care penetration using chi-square tests and Student’s t-tests for categorical and continuous variables, respectively. Then, we fit a Cox proportional-hazards model to assess the probability of robotic prostatectomy adoption between markets with low and high managed care penetration. This model met the proportional-hazards assumptions. Time-to-event was calculated from the beginning of the study period (January 1, 2003) until the first date of a robotic prostatectomy claim or the end of the observation window (December 31, 2008). Next among HSAs that adopted robotic prostatectomy, we fit a Poisson regression model to measure a market’s utilization of robotic prostatectomy within a year of adoption. This model was back-transformed to generate the predicted probability of robotic prostatectomy utilization in markets with low and high managed care penetration. For both the adoption and utilization of robotic prostatectomy among adopting HSAs, models were adjusted for aggregate patient characteristics (age, tumor grade and stage, and comorbidity) and market characteristics (racial composition, population density, education, income, and percent speaking English as a secondary language). Comorbidity was measured using established methods for claims data as described by Klabunde.11 All analyses were performed using SAS v9.2 (Cary, NC). The probability of a type I error was set at 0.05 and all testing was two-sided. Since patients cannot be identified, the Institutional Review Board of the University of Michigan exempted this study from review.
RESULTS
Patient and market characteristics of HSAs with low and high managed care penetration are shown in Table 1. Not all characteristics with statistical differences were clinically significant (e.g., patient age and English as a secondary language). Patient characteristics (i.e., age, tumor grade and stage, and comorbidities) were largely the same across markets. Conversely, compared with low managed care markets, those with high managed care penetration had greater racial diversity (i.e., higher percent non-white population), higher levels of education and wealth, and greater population densities.
Table 1.
Population characteristics of Health Service Areas according to level of managed care penetration
| Health Service Area | Managed care penetration | P Value | |
|---|---|---|---|
| Low | High | ||
| No. Health Service Areas | 115 | 45 | |
| No. patients treated with any prostatectomy | 5,069 | 7,282 | |
| Patient characteristics | |||
| Mean patient age, years | 69.7 | 70.2 | <0.01 |
| Well/moderately differentiated tumor grade, % | 40 | 41 | 0.84 |
| Tumor stage ≤ T2, % | 85 | 85 | 0.71 |
| Charlson Score 2 or higher, % | 6 | 6 | 0.79 |
| Market characteristics | |||
| Non-white population, % | 15 | 24 | <0.01 |
| Population density, (people per square mile) | 422 | 1987 | <0.01 |
| At least a college education, % | 17 | 27 | <0.01 |
| Median income, $ | 36,236 | 49,374 | <0.01 |
| English as a secondary language, % | 2 | 3 | <0.01 |
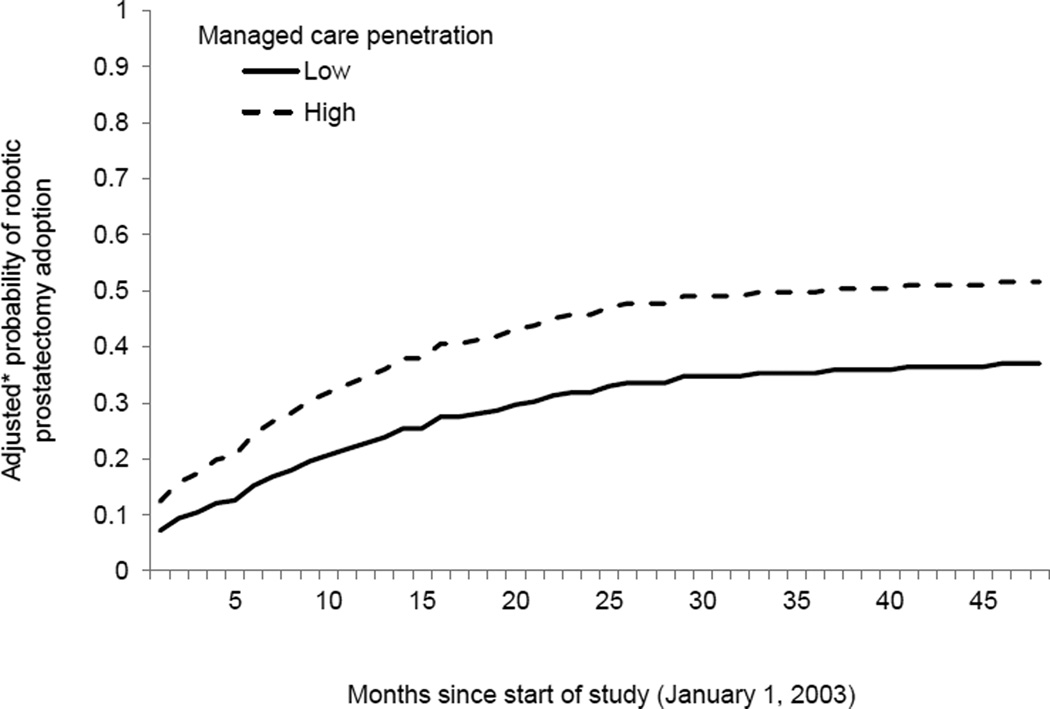
A total of 67 of the 160 HSAs (42%) adopted robotic prostatectomy over the course of the study. Of the 45 HSAs with high managed care penetration, 34 (76%) adopted robotic prostatectomy. In contrast, of the 115 HSAs with low managed care penetration, 33 (29%) adopted robotic prostatectomy. After adjusting for patient- and market-level differences, HSAs with high managed care penetration showed a greater propensity for robotic prostatectomy adoption (p=0.03) (Figure 1). By 2007, compared with low penetration markets, those with high managed care penetration were roughly 40.0% more likely to adopt robotic prostatectomy. That is, the probability of robotic prostatectomy adoption in 2007 was 0.37 and 0.52 in markets with low and high managed care penetration, respectively.
Figure 1. Probability of robotic prostatectomy adoption in markets with low and high managed care penetration.
The adoption of robotic prostatectomy increased over time in all markets. However, compared with markets with low levels of managed care, highly penetrated markets demonstrated a greater propensity for robotic prostatectomy adoption (p=0.03).
*Adjusted for patient-level (i.e., age, tumor grade and stage, and comorbidity) and market-level characteristics (i.e., racial composition, population density, education, income, and percent speaking English as a secondary language).
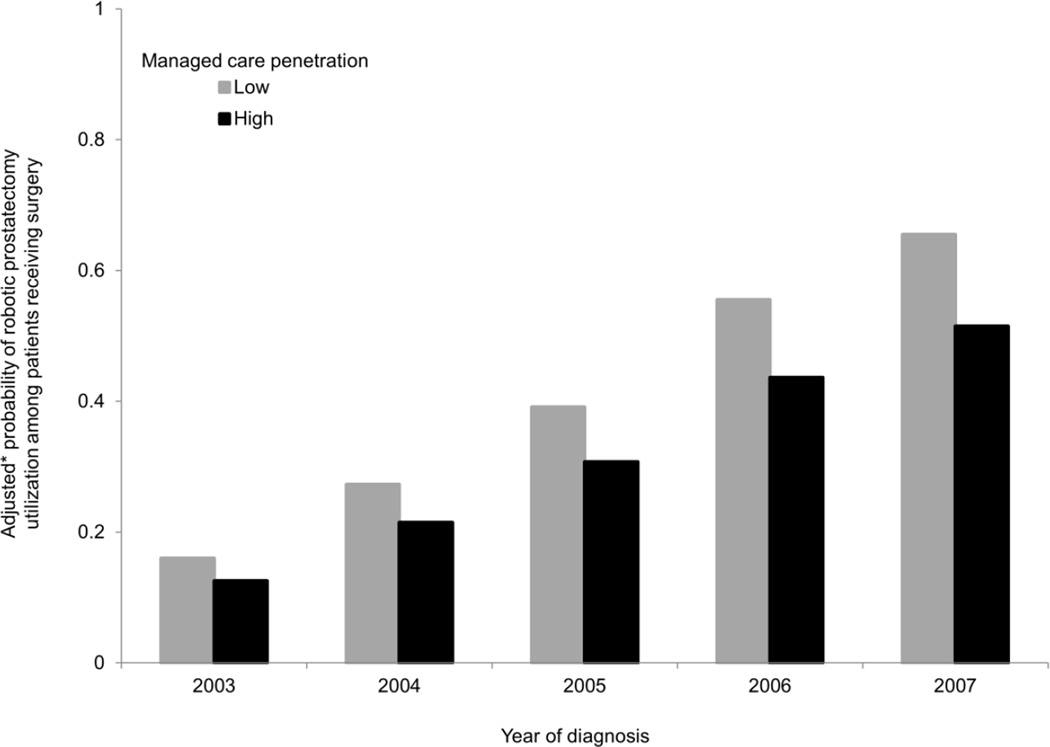
Among HSAs that adopted robotic prostatectomy, patient and HSA-level characteristics are shown in Table 2. Compared with markets with low managed care penetration, those with high penetration contained a smaller proportion of patients with lower grade disease and a Charlson score 2 or higher. Although statistically significant, the differences in patient age and tumor stage across HSAs were small. In addition, compared with low penetration markets, those with high managed care penetration were associated with greater racial diversity, population densities, levels of education and wealth, and use of English as a secondary language. In these adopting markets, the utilization of robotic prostatectomy among patients treated with any prostatectomy for prostate cancer is demonstrated in Figure 2, adjusting for differences in patients and healthcare markets. In both categories of HSAs, the probability of robotic prostatectomy utilization increased over time (p<0.01 for trend). In markets with low managed care penetration, the probability of robotic prostatectomy utilization increased from 0.16 in 2003 to 0.66 in 2007, a relative increase of 313%. Likewise, among highly penetrated markets, the probability of robotic prostatectomy utilization increased from 0.13 in 2003 to 0.52 in 2007, a relative increase of 300%. Although both types of markets showed similar increases in utilization, compared with low managed care markets, those with high managed care penetration had constrained utilization of robotic prostatectomy across all five years (p<0.01, comparison between groups).
Table 2.
Population characteristics among Health Service Areas that adopted robotic prostatectomy according to level of managed care penetration
| Health Service Area | Managed care penetration | P Value | |
|---|---|---|---|
| Low | High | ||
| No. Health Service Areas | 33 | 34 | -- |
| No. patients treated with any prostatectomy | 3,626 | 6,559 | -- |
| Patient characteristics | |||
| Mean patient age, years | 69.8 | 69.6 | <0.01 |
| Well/moderately differentiated tumor grade, % | 50 | 42 | <0.01 |
| Tumor stage ≤ T2, % | 85 | 83 | <0.01 |
| Charlson Score 2 or higher, % | 9 | 6 | <0.01 |
| Market characteristics | |||
| Non-white population, % | 13 | 15 | <0.01 |
| Population density, (people per square mile) | 324 | 1,641 | <0.01 |
| At least a college education, % | 18 | 25 | <0.01 |
| Median income, $ | 35,430 | 48,979 | <0.01 |
| English as a secondary language, % | 1 | 2 | <0.01 |
Figure 2. Probability of robotic prostatectomy utilization among prostate cancer patients receiving surgery in markets that have adopted robotic prostatectomy.
In low and high managed care markets, the probability of robotic prostatectomy utilization increased over time (p<0.01 for trend). However, compared with markets that had low managed care penetration, those with high managed care penetration had constrained utilization of robotic prostatectomy (p<0.01, comparison between groups).
*Adjusted for patient-level (i.e., age, tumor grade and stage, and comorbidity) and market-level characteristics (i.e., racial composition, population density, education, income, and percent speaking English as a secondary language).
DISCUSSION
The dissemination of robotic prostatectomy increased in all HSAs between 2003 and 2007, regardless of the level of managed care penetration. Markets with high managed care penetration were associated with greater racial diversity (i.e., higher percent non-white population), higher levels of education and wealth, and greater population densities. These markets adopted robotic prostatectomy more rapidly than those with low managed care penetration. However, among the adopting markets, those with high managed care penetration constrained the utilization of the procedure.
There are at least three reasons why markets with high managed care penetration may have adopted robotic prostatectomy more rapidly than markets with low managed care penetration. First, the decision to purchase robotic equipment is not dictated by a managed care organization. Instead, this decision is generally made by hospitals and physician groups that consider several factors other than patient outcomes or insurance type, including patient demands and market share.7 This leads to the second reason, which is that offering robotic prostatectomy may provide indirect benefits to hospitals or physician groups. These benefits include recruiting surgeons who desire to offer robotic surgery to their patients7 and attracting patients or family members who may ultimately receive treatments other than robotic surgery at their facility.5 For instance, there is evidence that hospitals or regions that adopt robotic prostatectomy are associated with higher volumes of both robotic and open procedures.18 Third, markets with high managed care penetration are typified by higher socioeconomic class, which is strongly associated with the adoption of new technology, including robotic prostatectomy.19,20
Despite higher levels of adoption in markets with high managed care penetration, the utilization of robotic prostatectomy was constrained. This finding is consistent with the focus of managed care organizations, which attempt to reduce high levels of utilization and spending while improving the efficiency of healthcare delivery.4 To reduce healthcare spending, managed care organizations have implemented several cost-controlling strategies, including capitated payments, utilization review, selective contracting, and restrictions on patient choices.4,21 In so doing, managed care organizations have decreased the use of other expensive technologies, such as the diffusion of magnetic resonance imaging, angioplasty, and intensity-modulated radiotherapy.12,16,22
The constrained utilization of robotic prostatectomy after initial increased adoption in markets with high managed care penetration has important policy implications, particularly as accountable care organizations gain momentum. Accountable care organizations share many similarities with managed care organizations, including their emphasis on containing costs while improving quality.23 Since many of their principles (e.g., care coordination, de-emphasis on fee-for-service incentives, and focus on primary care providers) originate from the managed care model,8,9 understanding the dissemination of technology under the auspices of managed care may help predict how accountable care organizations will handle promising new technologies on the horizon. On one hand, with a similar focus on reducing costs, accountable care organizations may discourage the dissemination of new technologies in an effort to increase shared savings. On the other hand, with a greater emphasis on patient engagement and quality measurement, accountable care organizations may be better able to promote the use of new technologies with the most value (i.e., high quality, low cost) while discouraging the use of those with no added benefit.9
Our findings should be interpreted in the context of several limitations. First, SEER-Medicare data are unable to differentiate robotic from laparoscopic prostatectomy. However, the laparoscopic procedure constitutes less than 3% of all cases,24 and thus, represent only a small fraction of those performed with a minimally invasive approach. Second, since this study is based on observational data, there is potential that our inference is biased by unmeasured differences between markets. Although we cannot specifically account for unmeasured factors, we adjusted for several measured market characteristics (e.g., racial diversity, population density, degree of education, and income level) to minimize confounding. Third, managed care plans comprise a variety of private health plans, such as health maintenance organizations, preferred provider organizations, and private-fee-for-service plans, which may all have different influences on treatment utilization. Nonetheless, these plans all aspire to control healthcare costs while maintaining high-quality care, and thus, likely affect the adoption and utilization of new, expensive technologies in similar ways. Fourth, SEER-Medicare only contains information about fee-for-service beneficiaries and not managed care beneficiaries. With that said, the managed care penetration in a healthcare market has been shown to affect managed care and non-managed care participants in similar ways. This phenomenon, known as the “spillover effect”, has been well-characterized in the literature.25–27 Thus, we feel our findings accurately reflect the relationship between the dissemination of robotic prostatectomy and managed care penetration.
CONCLUSION
Our study has two important findings. First, the adoption of robotic prostatectomy was higher in markets with high managed care penetration. Thus, insofar as managed care organizations strive to control costs, they do not appear to limit the purchase of new and expensive technology. Second, in markets that have adopted robotic prostatectomy, those with high managed care penetration are associated with constrained utilization. Here, the cost-controlling mechanisms of managed care organizations appear to exert more influence. Going forward, directly comparing the use of robotic prostatectomy among managed care and non-managed care organizations within the same HSAs may shed more light on determinants of its adoption and utilization. A better understanding of this paradox—increased adoption yet constrained utilization—is needed as healthcare reform emphasizes reducing costs while improving quality and access to care.
Acknowledgments
Brent Hollenbeck is supported in part by Research Scholar Grant RSGI-13-323-01-CPHPS from the American Cancer Society and by NIH/NCI grant R01 CA168691. He is also an Associate Editor of Urology.
Florian Schroeck is supported in part by the American Cancer Society Postdoctoral Fellowship Grant (PF-12-118-01-CPPB) and by the National Institutes of Health Training Grant NIH 5 T32 DK007782-12.
Bruce Jacobs is supported in part by the American Cancer Society Postdoctoral Fellowship Grant (121805-PF-12-008-01-CPHPS).
Information about research materials can be obtained by contacting Yun Zhang.
ABBREVIATIONS AND ACRONYMS
- HCPCS
Healthcare Common Procedure Coding System
- HSA
Health Service Area
- MEDPAR
Medicare Provider Analysis and Review
- SEER
Surveillance, Epidemiology, and End Results
Contributor Information
Yun Zhang, Email: seanyz@med.umich.edu.
Brent K. Hollenbeck, Email: bhollen@med.umich.edu.
Florian R. Schroeck, Email: fschroec@med.umich.edu.
Bruce L. Jacobs, Email: jacobsbl107@gmail.com.
REFERENCES
- 1.Ficarra V, Cavalleri S, Novara G, Aragona M, Artibani W. Evidence from robot-assisted laparoscopic radical prostatectomy: a systematic review. Eur Urol. 2007;51:45–55. doi: 10.1016/j.eururo.2006.06.017. discussion 56. [DOI] [PubMed] [Google Scholar]
- 2.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557–1564. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 3.Kolata G. Results Unproven, Robotic Surgery Wins Converts. The New York Times. 2010 [Google Scholar]
- 4.Baker LC. Managed care and technology adoption in health care: evidence from magnetic resonance imaging. J Health Econ. 2001;20:395–421. doi: 10.1016/s0167-6296(01)00072-8. [DOI] [PubMed] [Google Scholar]
- 5.Lotan Y, Bolenz C, Gupta A, et al. The effect of the approach to radical prostatectomy on the profitability of hospitals and surgeons. BJU Int. 2010;105:1531–1535. doi: 10.1111/j.1464-410X.2009.08996.x. [DOI] [PubMed] [Google Scholar]
- 6.Virnig BA, Warren JL, Cooper GS, Klabunde CN, Schussler N, Freeman J. Studying radiation therapy using SEER-Medicare-linked data. Med Care. 2002;40:IV, 49–54. doi: 10.1097/00005650-200208001-00007. [DOI] [PubMed] [Google Scholar]
- 7.Barbash GI, Glied SA. New technology and health care costs - the case of robot-assisted surgery. N Engl J Med. 2010;363:701–704. doi: 10.1056/NEJMp1006602. [DOI] [PubMed] [Google Scholar]
- 8.Weil TP. Accountable care organizations: HMOs by another name? J Fam Pract. 2012;61:10. [PubMed] [Google Scholar]
- 9.Baldwin LM, Adamache W, Klabunde CN, Kenward K, Dahlman C, J LW. Linking physician characteristics and medicare claims data: issues in data availability, quality, and measurement. Med Care. 2002;40:IV, 82–95. doi: 10.1097/00005650-200208001-00012. [DOI] [PubMed] [Google Scholar]
- 10.Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK, editors. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute; 2010. [Google Scholar]
- 11.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 12.Jacobs BL, Zhang Y, Skolarus TA, et al. Managed care and the diffusion of intensity-modulated radiotherapy for prostate cancer. Urology. 2012;80:1236–1242. doi: 10.1016/j.urology.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs BL, Zhang Y, Skolarus TA, et al. Certificate of need legislation and the dissemination of robotic surgery for prostate cancer. J Urol. 2013;189:80–85. doi: 10.1016/j.juro.2012.08.185. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. [Accessed January 3, 2012]; http://www.cdc.gov/nchs/
- 15.The Henry J. Kaiser Family Foundation Medicare Advantage Fact Sheet. [Accessed January 7, 2014];2013 http://kaiserfamilyfoundation.files.wordpress.com/2013/11/2052-17-medicare-advantage.pdf. [Google Scholar]
- 16.Baker LC, Wheeler SK. Managed care and technology diffusion: the case of MRI. Health Aff (Millwood) 1998;17:195–207. doi: 10.1377/hlthaff.17.5.195. [DOI] [PubMed] [Google Scholar]
- 17.Keating NL, Landrum MB, Meara E, Ganz PA, Guadagnoli E. Do increases in the market share of managed care influence quality of cancer care in the fee-for-service sector? J Natl Cancer Inst. 2005;97:257–264. doi: 10.1093/jnci/dji044. [DOI] [PubMed] [Google Scholar]
- 18.Makarov DV, Yu JB, Desai RA, Penson DF, Gross CP. The association between diffusion of the surgical robot and radical prostatectomy rates. Med Care. 2011;49:333–339. doi: 10.1097/MLR.0b013e318202adb9. [DOI] [PubMed] [Google Scholar]
- 19.Ulmer WD, Prasad SM, Kowalczyk KJ, et al. Factors associated with the adoption of minimally invasive radical prostatectomy in the United States. J Urol. 2012;188:775–780. doi: 10.1016/j.juro.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen PL, Gu X, Lipsitz SR, et al. Cost implications of the rapid adoption of newer technologies for treating prostate cancer. J Clin Oncol. 2011;29:1517–1524. doi: 10.1200/JCO.2010.31.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simon CJ, Dranove D, White WD. The effect of managed care on the incomes of primary care and specialty physicians. Health Serv Res. 1998;33:549–569. [PMC free article] [PubMed] [Google Scholar]
- 22.Cooper GS, Virnig B, Klabunde CN, Schussler N, Freeman J, Warren JL. Use of SEER-Medicare data for measuring cancer surgery. Med Care. 2002;40:IV, 43–48. doi: 10.1097/00005650-200208001-00006. [DOI] [PubMed] [Google Scholar]
- 23.Correia EW. Accountable care organizations: the proposed regulations and the prospects for success. Am J Manag Care. 2011;17:560–568. [PubMed] [Google Scholar]
- 24.Yu HY, Hevelone ND, Lipsitz SR, Kowalczyk KJ, Hu JC. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol. 2012;187:1392–1399. doi: 10.1016/j.juro.2011.11.089. [DOI] [PubMed] [Google Scholar]
- 25.Baker LC. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. J Health Econ. 1997;16:453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- 26.Baker LC. Association of managed care market share and health expenditures for fee-for-service Medicare patients. JAMA. 1999;281:432–437. doi: 10.1001/jama.281.5.432. [DOI] [PubMed] [Google Scholar]
- 27.Heidenreich PA, McClellan M, Frances C, Baker LC. The relation between managed care market share and the treatment of elderly fee-for-service patients with myocardial infarction. Am J Med. 2002;112:176–182. doi: 10.1016/s0002-9343(01)01098-1. [DOI] [PubMed] [Google Scholar]