Abstract
Background and Objectives:
The dangerous events caused by medication errors are one of the main challenges faced in critical care units. The present study was conducted to determine the frequency of intravenous medication administration errors and their causes in cardiac critical care units in Iran.
Materials and Methods:
The present descriptive study was conducted in the critical care units (CCUs and cardiac surgery intensive care units) of 12 teaching hospitals. Of the total of 240 nurses working in these departments, 190 participated in the present study. The data collection tools used in this study included the “nurses’ demographic data questionnaire”, the “patients’ medical and demographic data questionnaire” and the “nurses’ self-reporting questionnaire about the frequency of intravenous medication administration errors and their causes”. The data obtained were analyzed in SPSS-20 using descriptive statistics such as the absolute and relative frequency.
Findings:
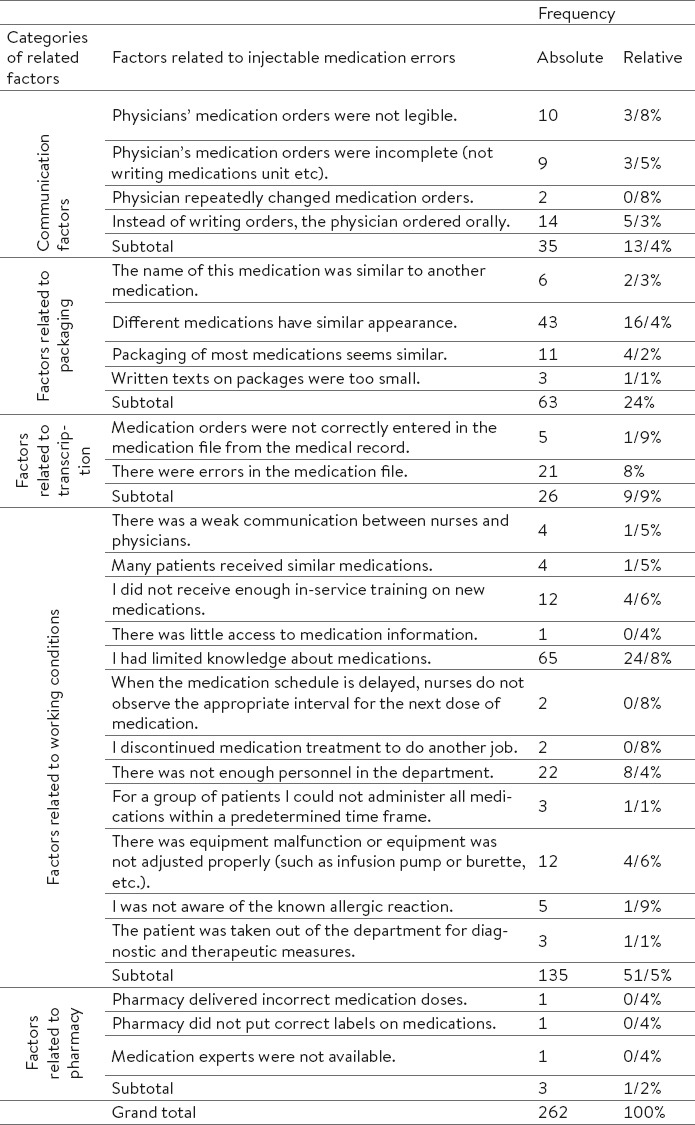
During the 2 months in which this study was being conducted, 2542 patients were admitted to these departments and 20240 doses of intravenous medications were administered to these patients. The nurses reported 262 intravenous medication administration errors. The most common intravenous medication error pertained to administering the wrong medication (n=71 and 27.1%). As for the causes of intravenous medication administration errors, 51.5% of the errors were associated with work conditions, 24% with packaging, 13.4% with communication, 9.9% with transcription and 1.2% with pharmacies.
Discussion and Conclusion:
According to the results, strategies are recommended to be adopted for reducing or limiting medication errors, such as building a stronger pharmacology knowledge base in nurses and nursing students, improving work conditions and improving communication between the nurses and physicians.
Keywords: Intravenous Medication Administration Errors, critical care units, Types of Error, Causes of Errors
1. INTRODUCTION
The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) states that, “A Medication error is any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer” (1). A review study conducted to examine medication errors in critical care units reported medication errors in these units to range from 3.3% to 9.4% in frequency (2). The National Patient Safety Agency of the UK has reported the incidence of errors during the administration stage of medication therapy to be 50% (3). In a review study conducted in 15 Middle Eastern countries, including Iran, errors during the administration stage were reported to range from 9.4% to 80% in frequency (4). A number of studies conducted in Iran reported errors during the administration stage to be 79.2% (5), 73.43% (6), 9.8% (7) and 46.8% (8). Medication errors common during this stage include the wrong dose, the wrong medication, the wrong route, the wrong time, the wrong patient, the wrong technique, dose omission and administration without a physician’s order (9). Different methods are used for detecting errors, including chart reviews, direct observation and self-reporting (10). Self-reporting of errors is the key to maintaining the patients’ safety (11); Fostering the culture of self-reporting is less common during healthcare personnel’s professional training and teaching hospitals play a significant role in promoting the culture of self-reporting among the healthcare personnel and students (10). The most common causes of medication errors reported by the NCC MERP include personnel malfunction (39%), knowledge deficits (17%) and communication problems between physicians and the healthcare personnel (1). According to studies, over 80% of hospitalized patients receive intravenous medications (12). The Institute for Safe Medication Practices (ISMP) reported that 54% of the dangerous events caused by medication errors and 56% of all the medication errors pertain to intravenous medications (13).
2. MATERIALS AND METHODS
The research population of the present descriptive study consisted of all the nurses working in cardiac critical care units including CCUs and cardiac surgical intensive care units from 12 teaching hospitals affiliated to Mazandaran University of Medical Sciences, constituting 15 departments overall. The study inclusion criteria consisted of having a bachelor’s or higher level degree in nursing and being willing to participate in the study. From the total of 240 nurses working in these departments, 190 nurses expressed their willingness to participate. Sampling was carried out by visiting the hospitals from November 2014 to January 2015. Three data collection instruments were used in this study, including the “nurses’ demographic data questionnaire”, the “patients’ medical and demographic data questionnaire” and the “nurses’ self-reporting questionnaire about the frequency of intravenous medication administration errors and their causes”. The nurses’ demographic data questionnaire included items about the demographic characteristics of the study subjects, such as age, gender, marital status, level of education, work experience and critical care unit work experience. The second questionnaire contained items about the patients’ medical and demographic characteristics, such as age, gender, disease diagnosis, duration of hospitalization and the number of intravenous medication doses administered during hospitalization. The third questionnaire was the medication error questionnaire derived from the questionnaire designed by Wakefield et al., the validity and reliability of which were evaluated during four consecutive years (14). In Iran, the validity and reliability of the questionnaire were measured by Taheri Habibabadi et al. (15). This questionnaire examined the name of the intravenous medications subject to errors, the variety of intravenous medication errors, the outcomes of intravenous medication errors, the work shifts during which the error had occurred and the causes of medication errors. The causes of medication errors formed 5 subscales, including causes pertaining to communication, packaging and labeling, transcription, work conditions and pharmacies, which were discussed in 32 items. After explaining the study objectives to the nurses and the head nurses, those willing to participate in the study completed the “nurses’ demographic data” questionnaire through face-to-face interviews. The face-to-face interview technique was used so as to attract the subjects’ trust and cooperation. The “medical and demographic data” questionnaire was additionally completed by the researcher over a period of two months and based on the medical record and the medication administration record of the patients hospitalized in these departments. The “nurses’ self-reporting questionnaire about the frequency of intravenous medication administration errors and their causes” was duplicated in twice the number of the nurses in each department. A copy of the questionnaire were given to each nurse and additional copies were left in each department next to the questionnaire submission box so that more forms were available for the nurses if they required more space to write about their errors. The nurses filled out the questionnaires for each intravenous medication administration error they had made during the shift and then tossed the filled-out questionnaires into the questionnaire box located in their department at the end of the study, so they would not have to worry about being morally or legally interrogated by the researcher and to also respect the codes of research ethics. The researcher monitored the research process every week by visiting the hospitals. In addition, he talked over the phone with the shift heads in all the departments on a daily basis and thus reminded the nurses to complete the questionnaires. Data were analyzed in SPSS-20 using descriptive statistics..
3. RESULTS
The analysis of the nurses’ demographic data showed that 92.2% of the participants were women, 93.2% were nurses and 6.8% head nurses, 74% were employed in CCUs and 26% in cardiac surgery intensive care units, 92.7% had rotating shifts and 91.7% were not working in any other hospitals. In terms of marital status, 70.3% were married, 29.2% were single and 0.5% were widowed. In terms of education, 91.7% had an undergraduate degree, 6.8% had a master’s degree and 1.6% were graduate students. In terms of employment, 43.8% of the nurses were permanent workers, 29.7% were contract employees, 14.1% were project-based fixed-term employees, 10.4% were contractors and 2.1% were agency staff. The mean age of participating nurses was 33.96 ± 6.61 years, their mean work experience 9.3 ± 5.87 years, their mean work experience in critical care units 6.28 ± 4.94 years and the mean number of patients under the supervision of each nurse was 3.84 ± 0.12.
The analysis of the patients’ medical and demographic data showed that 2542 patients were admitted to these departments within the 2 months of the study, and 20240 doses of intravenous medication were administered to these patients. 63.2% of the patients were male and 85.1% were admitted to CCUs. The mean age of the patients was 60.87 ± 13.25 years and the mean duration of their hospitalization was 1.81 ± 0.74 days. The most common causes of hospitalization were acute coronary syndrome (n=1066 and 41.9%), myocardial infarction or MI (n=291 and 11.4%), coronary artery bypass graft or CABG (n=209 and 8.2%), post-CABG (n=209 and 8.2%), acute pulmonary edema (n=144 and 5.7%), post-PCI (n=110 and 4.3%) and cardiac heart failure or CHF (n=100 and 3.9%). The nurses reported 262 cases (64.38%) of intravenous medication errors, with the most common ones including wrong medication (n=71 and 27.1%), wrong dose (n=47 and 17.9%), wrong infusion rate (n=45 and 17.2%), and medication calculation errors (n=28 and 10.7%); (Table 1). As for the causes of medication errors, 51.5% of intravenous medication administration errors were due to work conditions, 24% to packaging, 13.4% to communication, 13.3% to communication, 9.9% to transcription and 1.2% to pharmacies (Table 2). Of all the intravenous medication errors committed, 186 (71%) had no consequences for the patients and 74 (28.2%) had consequences such as hypertension, hypotension, nausea, vomiting, tachycardia, bradycardia, flushing, hypoglycemia, hyperglycemia, dysrhythmia and sedation. Two errors (0.8%) were fatal and pertained to Pancuronium Bromide injection without any respiratory support. Of all the intravenous medication errors committed, 38.2% had occurred during the night shift, 31.7% during the evening shift and 30.2% during the morning shift. The medications most commonly subject to errors included Heparin (11.5%), Furosemide (8%), Nitroglycerin (5.7%), Insulin (3.8%), Metoclopramide (3.8%), Streptokinase (3.4%), Potassium chloride (3.4%), Enoxaparin (3.4%), Amiodarone (3.4%), Digoxin (3.1%), Atropine (3.1%), Midazolam (3.1%), Dopamine (2.7%), Magnesium sulfate (2.7%) and Ranitidine (2.7%).
Table 1.
Absolute and relative distribution of Types of injectable medication errors by nurses in cardiac critical care units
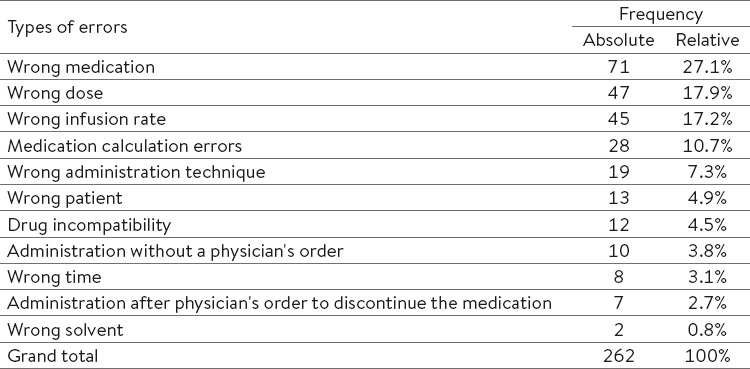
Table 2.
Absolute and relative distribution of factors related to injectable medication errors by nurses in cardiac critical care units
4. DISCUSSION
According to the results of the study, the most common types of intravenous medication administration errors in order of frequency included the wrong medication, the wrong dose and the wrong infusion rate errors. In a study conducted on 94 nurses working in the emergency department of a teaching hospital in Tehran, wrong infusion rate and wrong dose were proposed as the most common medication errors (8), which is consistent with the results of the present study. Another study conducted in the internal and surgical intensive care unit of a teaching hospital examined the nurses’ performance in 33 working shifts. Dose omission, wrong dose and wrong medication were introduced as the most common medication errors committed in this study (16). A researcher-made questionnaire was completed in another study by 100 nurses working in the intensive care unit and the emergency, pediatric, internal and surgery departments, showing the wrong dose error to be the most common type of error committed (17). In another study conducted on 332 nurses, the wrong dose and the wrong medication errors were identified as the most common errors committed (18). The results of all these studies were consistent with the results of the present study. A study was conducted in six internal and surgery departments in two teaching hospitals in Australia, and the performance of 107 nurses was examined during the intravenous administration of 568 medication doses. The results of this study showed the wrong infusion rate and the drug incompatibility to be the most common intravenous medication administration errors (19). In the present study, wrong infusion rate constituted the most common medication error while drug incompatibility was considered the least common type of medication error committed by the nurses. A study conducted in Canada examined 180 patients in a 16-bed internal surgery intensive care unit over a period of seven months and during the administration of 1882 doses of medication over 40 work shifts. Incomplete medication cards or wrong cards were introduced as the most common errors committed in this study in order of frequency (20). The present study also examined medication administration record errors, but did not assess medication card errors, which constitutes one limitation of the study.
In a study conducted in four 90-bed hospital departments of a hospital in Paris, including the cardiac surgery unit, the internal cardiac unit, the vascular department and the nephrology division, and with the participation of 28 nurses, wrong time and dose omission were reported to be the most common errors committed (21). In a study conducted in five cardiovascular surgery departments in Switzerland over a period of one month and with the participation of 119 nurses and the administration of 24617 doses of medications using the self-reporting technique, the wrong time errors was introduced as the most common medication error committed (22). In the present study, the wrong time error was proposed as the ninth most common type of error in the administration of intravenous medications. As for the causes of medication errors, the present study found work conditions to be the most common risk factors associated with intravenous medication administration errors, with the lack of sufficient pharmacology information being the most frequent risk factor. As in the present study, another study also proposed knowledge deficits and memory errors as the most common causes of medication errors (16). In yet another research, work conditions were proposed as the most common cause of medication errors (15). Heavy workloads and staff shortages were reported as the most common causes of medication errors in one study conducted in the UK on 76 nurses who completed a questionnaire (23). In a study conducted on 96 nurses working in a teaching hospital in Kermanshah, pharmacological knowledge deficits was proposed as the main cause of medication errors (5). In another study, memory error, violation of the rules and pharmacological knowledge deficits were introduced as the most common causes of intravenous medication administration errors in critical care units (7). Based on the results of different studies, heavy workloads and staff shortages are the main causes of medication errors (15, 23). All these causes can be categorized under work conditions, which is somewhat consistent with the results of the present study. The causes of medication errors were divided into two groups: human causes and medical causes. From the list of the human causes, pharmacology information deficits, and from the list of medical causes, the use of medical abbreviations, constituted the most frequent causes of medication errors (8). In a study conducted in Saudi Arabia, human causes such as knowledge deficits and personnel malfunction were introduced as the most common causes of medication errors, while ineffective communication, such as prescription errors and wrong prescription interpretations were introduced as the second most common cause of human errors (24). Pharmacological knowledge deficits constituted the most common cause of error in the present study too. The use of medical abbreviations and wrong prescription interpretations can be somewhat categorized under communication causes; however, none of the errors reported were due to the use of abbreviations. In a study conducted on 799 nurses working in 24 hospitals in Jordan, inappropriate packaging and labeling were introduced as the major causes of medication errors (25). Inappropriate packaging was the second most common cause of intravenous medication administration errors in Jordan, which is somewhat consistent with the present study. According to the results of one study, nurses with a work experience of 6 years and over commit fewer errors compared to other nurses (19). In Australia, based on a number of clear medication errors made by 26 nurses, the causes of medication errors were divided into 5 categories, including individual, team, task, patient-related and environmental causes. The most common causes of medication errors by category included stress as an individual cause, poor communication between members as a team cause, unfamiliarity with medications as a task cause and long shifts or night shifts as environmental causes (26). Almost all these factors can be categorized under work conditions, thereby providing results that are consistent with the present study. The intravenous medications most commonly subject to errors in the present study were Heparin, Furosemide, Nitroglycerin, Insulin, Metoclopramide, Streptokinase, Potassium chloride, Enoxaparin, Amiodarone, Digoxin, Atropine, Midazolam, Dopamine, Magnesium sulfate and Ranitidine, in respective order of frequency. In another study, cardiovascular medications, antibiotics, sedatives, analgesics, electrolytes and hormonal medications were among the medications most commonly subject to errors (16). In another study, antibiotics were found to be more subject to medication errors compared to other medications (19). According to the results of another study, in cardiology departments, cardiovascular and central nervous system medications were most commonly subject to medication errors compared to other medications. Medication errors occurred more frequently for intravenous medications than for oral medications (20). In Iran, antibiotics were reported to be most commonly subject to medication errors in NICUs (15). Antimicrobial medications and cardiovascular medications were the first and second medications most commonly subject to medication errors in the critical care units (7). Similar to the results of the present study, antimicrobial medications and cardiovascular medications were the first and second medications most commonly subject to medication errors in 5 critical care units, CCUs, emergency departments, pediatric departments and internal and surgery departments (17). Antibiotics are most commonly used in general intensive care units and other departments compared to in cardiac critical care units, which might be the reason for their being first on the list of medications that are mostly commonly subject to errors compared to their lower status in the present study.
In the present study, 71% of intravenous medication administration errors had no consequences for the patients, while 28.2% had some consequences and 0.8% were fatal. Similar to the present study, another study found 94% of medication errors to have no consequences for the patients and 6% to have some consequences; this study found no fatal errors (20). In another study, 25.5% of medication errors were serious, but there were no fatal errors (19). Another study showed that 0.9% were fatal, 8.2% were life-threatening and 29.1% had serious consequences for the patients (16). As consistent with the present study, the majority of medication errors had no consequences for the patients.
5. CONCLUSION
According to the results of the present study and in comparison with the results of other studies, it is necessary for university training managers to build a stronger pharmacology knowledge base in their nursing students and nurses, and for hospital managers to prevent medication errors from occurring through providing standard work conditions, such as a standard ratio of nurses to patients, providing sufficient in-service training, improving the relationship between the nurses and physicians and facilitating the 24-hour presence of clinical pharmacology experts for responding to medication questions.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.NCCMERP, National Coordinating Council for Medication Error Reporting and Prevention, About Medication Errors: What is a Medication Error? [Accessed March 28 2015]. Available from: http://www.nccmerp.org/aboutMedErrors.html .
- 2.Kiekkas P, Karga M, Lemonidou CH, Aretha D, Karanikolas M. Medication Errors in Critically Ill Adults: A Review of Direct Observation Evidence. Am J Crit Care. 2011;20(1):35–44. doi: 10.4037/ajcc2011331. [DOI] [PubMed] [Google Scholar]
- 3.The report from the patient safety observatory: Safety in Doses: Improving the use of medicines in the NHS. [Accessed September 24 2014]. Available from: http://www.nrls.npsa.nhs.uk/resources/?entryid45=61625 .
- 4.Alsulami Z, Conroy SH, Choonara I. Medication errors in the Middle East countries: A systematic review of the literature. Eur J Clin Pharmacol. 2013;69:995–1008. doi: 10.1007/s00228-012-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirzaei M, Khatony A, Safari Faramani R, Sepahvand E. Prevalence Types of Medication errors and Barriers to Reporting Errors by Nurses in an Educational Hospital in Kermanshah. Hayat, Journal of School of Nursing and Midwifery. 2013;19(3):28–37. [Google Scholar]
- 6.Cheraghi M, Nikbakhat Nasabadi A, Mohammad Nejad E, Salari A, Ehsani Kouhi Kheyli S. Medication errors among nurses in Intensive Care Unites (ICU) J Mazandaran Uni Med Sci. 2012;21:115–119. [Google Scholar]
- 7.Vazin A, Delfani S. Medication Errors in an Internal Intensive Care Unit of a Large Teaching Hospital: A Direct Observation Study. Acta Medica Iranica J. 2012;50(6):425–432. [PubMed] [Google Scholar]
- 8.Ehsani R, Cheraghi MA, Nejati A, Salari A, Haji Esmaeilpoor A, Mohammad Nejad E. Medication errors of nurses in the emergency department. J Med Ethics Hist Med. 2013;6(11):1–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Kruer R, Jarrell A, Latif A. Reducing medication errors in critical care: a multimodal approach. Clin Pharmacol. 2014;6:117–126. doi: 10.2147/CPAA.S48530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dollarhide A, Rashidian A, Weinger M, Dresselhaus T. Use of a Handheld Computer Application for Voluntary Medication Event Reporting by Inpatient Nurses and Physicians. J Gen Intern Med. 2007;23(4):418–22. doi: 10.1007/s11606-007-0404-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westbrook J, Li l, Lehnbom E, Baysari MA, Braithwaite J, Burke R, Conn CH, Day R. What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. Int J Qual Health Care. 2015;27(1):1–9. doi: 10.1093/intqhc/mzu098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ong W M, Pharm B, Subasyini S, Pharm M. Medication Errors in Intravenous Drug Preparation and Administration. Med J Malaysia. 2013;68(1):52–57. [PubMed] [Google Scholar]
- 13.Parshuram CS, Ng G, Ho TK, Klein J, Moore AM, Bohn D. Discrepancies between ordered and delivered concentrations of opiate. Crit Care Med. 2003;31:2483–2487. doi: 10.1097/01.CCM.0000089638.83803.B2. [DOI] [PubMed] [Google Scholar]
- 14.Wakefield J, Uden-Holman T, Wakefield DS. Development and Validation of the Medication Administration Error Reporting Survey Tools, and Products. Adv Patient Surv. 4(12):475–489. [PubMed] [Google Scholar]
- 15.Taheri HabibAbadi E, Noorian M, Rassouli M, Kavousi A. Nurses’ Perspectives on Factors Related to Medication Errors in Neonatal and Neonatal Intensive Care Units. Iran Journal of Nursing (IJN) 2013;25(80):65–74. [Google Scholar]
- 16.Kopp BJ, Erstad BL, Allen ME, Theodorou AA, Priestley G. Medication errors and adverse drug events in an intensive care unit: direct observation approach for detection. Crit Care Med. 2006;34(2):415–425. doi: 10.1097/01.ccm.0000198106.54306.d7. [DOI] [PubMed] [Google Scholar]
- 17.Nikpeyma N, Gholamnejad H. Reasons for medication errors in nurses’ veiws. J Nurs Midwifery. 2009;19:18–24. [Google Scholar]
- 18.Zahmatkeshan N, Bagherzadeh R, Mirzaie K. An observational study to evaluate the medication errors by nursing staff working in bushehr medical centers during one year interval. Iran South Med J. 2010;13:201–206. [Google Scholar]
- 19.Westbrook J, Rob M, Woods A, Parry D. Errors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experience. BMJ Qual Saf. 2011;20:1027–1034. doi: 10.1136/bmjqs-2011-000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sorgini C, Fernandes V, Lubchansky S, Mehta S, Hallett D, Bailie T. Errors Associated with IV Infusions in Critical Care. Can J Hosp Pharm. 2012;65(1):19–26. doi: 10.4212/cjhp.v65i1.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berdot S, Sabatier B, Gillaizeau F, Caruba T, Prognon P, Durieux P. Evaluation of drug administration errors in a teaching hospital. BMC Health Serv Res. 2012;12(60):1–8. doi: 10.1186/1472-6963-12-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Küng K, Carrel T, Wittwer B, Engberg S, Zimmermann N, Schwendimann R. Medication Errors in a Swiss Cardiovascular Surgery Department: A Cross-Sectional Study Based on a Novel Medication Error Report Method. Nurs Res Prac. 2013. [Accessed March 2014]. Available from: http://dx.doi.org/10.1155/2013/671820 . [DOI] [PMC free article] [PubMed]
- 23.Tang F, Sheu SJ, Yu S, Wei IL, Chen CH. Nurses relate the contributing factors involved in medication errors. J Clin Nurs. 2007;16(3):447–457. doi: 10.1111/j.1365-2702.2005.01540.x. [DOI] [PubMed] [Google Scholar]
- 24.Dibbi H, Al-Abrash Y, Hussain W, Fattani M, Karima T. Causes and outcom of medication errors in hospitalised patients. Saudi Med J. 2006;27(10):1489–1492. [PubMed] [Google Scholar]
- 25.Mrayyan MT, ShishaniI K, AL-Faouri I. Rate, causes and reporting of medication errors in Jordan: nurses’ perspectives. J Nurs Manag. 2007;15:659–670. doi: 10.1111/j.1365-2834.2007.00724.x. [DOI] [PubMed] [Google Scholar]


