Abstract
Objective:
Burn injuries in hands are much more complex and the appearance of contractures is a common complication. Hand burn injuries often result in limited functionality, flexion and extension of fingers and present a major hindrance in rehabilitation. The aim of physical therapy and splinting after hand burn injury is to maintain mobility, prevent the development of the contracture and to promote the functionality of hand and good cosmetic results. The purpose of this study is to presents our experience of 38 children with hand burn injuries, admitted and treated at the Department of Plastic Surgery, UCCK-Pristina, Kosovo, during the years 2012-2015.
Methods:
Physical therapy is focused on active/passive range of motion in affected joints, management of cicatrix, strengthening exercise, coordination and use of splints for correction contractures. Patients were evaluated in three, six months and the definitive evaluation is done after 9 months of physical therapy and splinting.
Results:
We have improvement in range of motion (ROM), functionality, coordination, muscle force, decrease of keloids scars.
Conclusion:
This study shows the importance of physical therapy and splinting, achieving good results in preventing contracture, improving range of motion, muscle force and good cosmetic results.
Keywords: burns injuries, hands, complications, physical therapy
1. INTRODUCTION
Integrity of hand is absolutely essential for everyday function. Hands, because of its exposure and the importance of its functionality, are at high risk and may be affected by many injuries. The burns injury is too common (1). Hand burns have an important place in the pathology of children (2, 3), which are more complex and the appearance of contractures is a common complication. The main reason of these injuries is burns from direct contact with specific locations on a dorsal or palmer aspect of the hand. Most common burns in children are caused by grasping or pulling a hot object during the game and the second causes of burns in children is from hot liquids (3–5). The common deformities after burns according to Achauer are: claw deformity, palmer contractures, syndactyly or web space deformity, hypertrophic scarring and amputation (6). Application of physical therapy and splinting after burned hand injuries is very important and consists in prevention edema, contracture, maintaining or improving range of motion, functional recovery, preventing of development of keloids scars, muscle force and good cosmetic results.
2. MATERIAL AND METHODS
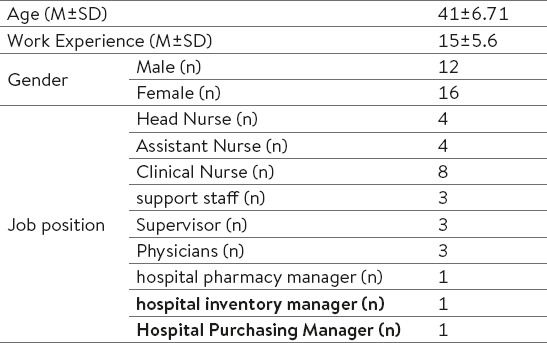
During the four year period from 2012 - 2015, at the Department of Plastic Surgery UCCK-Pristina, Kosovo we treated 38 children (21 males and 17 females) age 3-16, with hands after burn injuries.
Patients had unilateral and bilateral hand burn injuries: 12 cases involved the right hand, 18 involved the left hand and 8 involved both hands. Exclusion criteria were children under 3 years old. Twenty-four cases had deep burn injuries and they were operated, 14 cases had superficial burn injuries and they were treated conservatively. Eighteen cases of burned hands had the region of the palmer surface of the hand, 21 cases had dorsal burns surface and 7 cases had combined burns both dorsal and palmer surface of the hand. 10 of them had combined burn injuries: face, neck and upper extremity. 75 % of cases had suffered burn injuries from hot water, tea and milk, while 25% of cases had suffered burns from another nature: electrical burns, direct contact with hot objects.
3. PHYSICAL THERAPY AND SPLINTING
Physical therapy and splinting focused.
Preventing or reducing edema.
Management of keloid scars.
Preventing the appearance of contractures.
Maintain and relocation of passive/active range of motion in affected joints.
Strengthening exercise, and
Occupational therapy.
Edema management: In acute phase from the first day we did positioning of the extremities, hands elevated above level of heart for 24 hours, we also applied passive mobilization in affected joints and surrounding nodes which can give good results in reduction of edema. In post acute phase to decrease edema we also used retrograde massage, three times a day, bandage, elevation of the hand and passive/active movements, three times a day 10-20 repetition.
Management of keloids scars: To prevent a keloids scars in acute phase and subacute phase we used postural alignment, splinting and passive mobilization in affected joints three times a day 10-20 repetition. In chronic phase we used massage with gel (contratubex or dermatix) two or three times a day, we also used a silicon plats, gloves, passive/active movements and stretching exercise. The patients had to do several times a day.
Preventing the appearance of contracture: Patients who hand burn injuries in a palmer part (Figure 1), after the day 6, the splint was applied. To prevent a flexor contracture we made a volar splint, the interphalangeal joints in extension and the metacarpo-phalangeal joints at 60º to 90º of flexion, wrist in a neutral position and the thumb was kept in 20º to 30º of abduction. We changed the position of splint after 4 weeks and we decided in extension (Figure 2). The splint was maintained continuously for 6–7 weeks and after 6–7 weeks until 3 month splints were used only during the night. At patients who had burn injuries in a dorsal part (Figure 3), after 3 to 4 weeks were used the rubber bands to prevent an extensor contracture (Figure 4). Rubber bands were used continuously for 4 to 6 weeks and for 4 weeks only during the night. We also continued to use passive/active motions and stretching exercise.
Figure 1.

Hand burn injury in a palmer part
Figure 2.

Volar splint
Figure 3.

Burn injury in a dorsal part.
Figure 4.

Use of rubber bands to prevention contracture.
Maintain and relocation of passive/active range of motion in affected joints: To maintain or relocation passive/active range of motion in affected joints we have done passive mobilization for each joint of the hand. We started to do a passive mobilization after 3 or 5 days in those cases which were treated conservatively and after one week in cases that had surgical treatment. Passive mobilization continued for 4 to 6 weeks. Active mobilization we started to do after 1 week and have continued until 5 to 6 month. Patients had to do several times a day 10-20 repetition.
Strengthening exercise: To prevent muscle atrophy we have done static exercises and strengthening exercise was done with the raband several times a day.
Occupational therapy: We used Occupational therapy with different kind of toys, small balls, plasticine. During the rehabilitation the patients and patient’s parent are instructed to learn the exercise and to do them at home.
Assessment
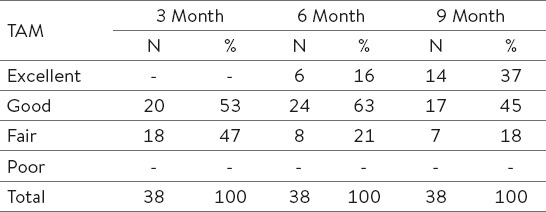
The patients were assessed using the total active motion (TAM), scoring system of the American Society for Surgery of Hand, the classification system is: excellent 100%, good 75-90%, Fair 50-74% and poor <50% (7). Assessments were done after 3, 6 months and final assessment after 9 months. At the same time we also measured the grip strength according the American Society of the Hand Therapists (7). We didn’t assess hand disability in daily living activities because none of the patients and their parents weren’t complained of the difficulty in daily living activities. The mean physical therapy follow up was 9 month (Figure 5, 6).
Figure 5.

2 month after injury.
Figure 6.

Same patient after 3 month.
Ethical clearance
The study was approved by the Research Ethics Committee, University of Prishtina, Kosovo. Written informed consent of each participant was obtained.
Statistical analysis
The statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 13.0. The mean TAM measurements of the basic values, vs. 6th month were compared using the Wilcoxon Matched-Pairs Signed-Ranks test. Chi-test was used to compare non-parametric data. A p value <0.05 was considered significant.
4. RESULTS
Total active motion results after 9 months were excellent in 37%, good in 45%, fair in 18% of the burned hands (Table 1).
Table 1.
Results of the TAM classification
Grip strength results after 9 months were found to be good in 71% and bed in 29% of cases (Table 2).
Table 2.
Results of the grip strength
With t-Test we got an important significant result on muscular strength in the hand after 6 and 9 months (t-Test = 5.2; p< 0.005). Most of the cases developed in range of motion (flexion and extension), contracture, muscle force est., after 6 to 9 month. Cosmetic results were good in all patients.
5. DISCUSSION
The burned hand represents serious injuries in children. Hand burn injuries are frequent component of burn injuries and provide opportunities for serious deformities in the future. Physical therapy, Splinting, Occupational therapy involvement from the early stage has been reported to be effective (4, 8) in preventing complications which are common after hand burn injuries. Burns from hot liquid are quite frequent causes of burn injuries in children (5). In our study 75% of cases had suffered burn injuries from hot water, tea and milk.
A lot of studies show that burn injuries are more common in mails than females. In 1998 Sheridan et al, in their study present 495 children with 698 burned hands and they reported that of all cases included in the study, 323 were boys and 172 girls (9). In our study 21 cases were males and 17 cases were females.
The aim of this study was to point out the success of physical therapy in early phase of burned hands at children. To prevent or reduce edema we used elevation of the hand, passive mobilization, retrograde massage, bandages. To management the keloids scars we used postural alignment, splinting, passive/active mobilization, massage and stretching exercise (5, 10, 11, 12). To prevent the contracture we used volar splint, rubber bands, passive/active movements and stretching exercise (9, 11). To maintain and relocate the passive/active movements and muscle force, we have done passive/active movements and strengthening exercise with therabend (4, 5, 10). Many studies have been made about methods of assessment of the hand function. In a study by Johnson et al, to assist the range of motion they recommend Total Active Motion(TAM) score, the classification system is: poor<180º, good 180º-219º, excellent 220º-259º (13). Also in our study the results of range of motion assessed by TAM score according A. S. SH. After 9 month 37% were excellent and 45% good and if this value we presented in degrees, the mean TAM was 213º which is considered functional and the normal is 260º. Another important parameter which is indicating in hand function is Grip strength. Roberts and collaborators study reported 75% of children achieved normative values for grip, lateral pinch and tripod pinch strength at 6 month (5). In our study we assessed only grip strength according American Society of the hand Therapist, after 9 month the results were good in 71% and bad in 29% of cases.
6. CONCLUSION
Physical therapy and splinting is essential part of rehabilitation in hand burns. Physical therapy and splinting should be started immediately after the injury. According to this study, we conclude that the physical therapy and splinting in hand burn injuries play an important role in the hand function.
Acknowledgement
It is a pleasure to thank MAJ. Jon Breakey PT, MSc (US Army MC) for his valuable suggestions and technical assistance.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Okhovatian F, Zoubine N. A comparison between two burn rehabilitation protocols. Burns. 33(4):429–434. doi: 10.1016/j.burns.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Argirova M, Hadzhiysk O. Acute Dorsal Hand Burns in Children. Ann Burns Fire Disasters. 2006;19(1):22–25. [PMC free article] [PubMed] [Google Scholar]
- 3.Petronic I, Nikolic G, Markovic M, Marsavelski A, Golubovic Z, Janjic G, Cirovic D. The importance of early physical therapy to prevent contracture in the burned hand. Ann Burns Fire Disasters. 2000;13(3):170–173. [Google Scholar]
- 4.Hundozi-Hysenaj H, Martinaj M, Muçaj S, Kabashi S, Sulejmani A, Haxholli F, Hysenaj Q. Physiotherapy Approach to a flexor contracture in a Burned Hand after 30 years. Mater Aociomed. 2010;22(3):172–174. [Google Scholar]
- 5.Skirven TM, Osterman AL, Fedorczyk J, Amadio PC. Rehabilitation of the hand and upper extremity. 6th edition. Philadelphia, USA: 2011. pp. 302–341. [Google Scholar]
- 6.Bee Lan T, Matic P. The challenges in Managing Hand Burns. Occupational Therapy Department, Concord Hospital. 2009 [Google Scholar]
- 7.Deniz E, Kucukdeveci A, Kutlay S, Demirtas M, et al. Postoperative Management of Flexor Tendon Repair in Zone 2. J Phys Ther Sci. 2000;12:63–66. [Google Scholar]
- 8.Kealey GP, Jensen KT. Aggressive Approach to Physical Therapy Management of the Burned Hand: A Clinical Report. Phys. Ther. 1988;68:683–685. doi: 10.1093/ptj/68.5.683. [DOI] [PubMed] [Google Scholar]
- 9.Sheridan RL, Baryza MJ, Pessina MA, O’Neill KM, et al. Acute hand burns in children: management and long-term outcome based on 10-year experience with 698 injured hands. Ann Surg. 1999;229(4):558–564. doi: 10.1097/00000658-199904000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arena D, Actis MV. The Rehabilitation of Severely Burned Patients: Prevention and Treatment of Scarring. Ann Burns Fire Disasters. 2005;18(3):140–148. [PMC free article] [PubMed] [Google Scholar]
- 11.Chait LA. The treatment of contact Burns of the Palm in Children. S Afr Med J. 1975;49(44):1839–1842. [PubMed] [Google Scholar]
- 12.Simons MA, Kimble RM. JH Stone, M Blouin. Pediatric Burns. International Encyclopedia of Rehabilitation. 2012. Available online: http://cirrie.buffalo.edu/encyclopedia/en/article/119/
- 13.Fauerbach J, Engrav L, Kowalske K, Brych S, et al. Barriers to Employment Among Working-Aged Patients with Major Burn Injury. Journal of Burn Care & Rehabilitation. 2001;22(1):26–34. doi: 10.1097/00004630-200101000-00007. [DOI] [PubMed] [Google Scholar]


