Abstract
Background:
As a mental response to sexual stimuli, sexual desire determines human sexual behavior and represents the cognitive capacity of sexual stimulation, so that avoiding sexual activity has a very negative effect on the discharge of intimacy and joy in couple’s relationship and threatens the stability relationship, which can finally end in sexual dissatisfaction and divorce; it may even affect the reproduction. This study, reviews the literature on biopsychosocial determinants of hypoactive sexual desire disorder in women in childbearing ages.
Method:
The search was done from January to March 2015 by the use of the data bases ProQuest, Pubmed, CINAHL, Ovid and Medline and the words sexual desire, related factors and biopsychosocial determinants were used as free text words. The words reduce sexual desire, hypoactive sexual desire disorder, dyadic relationship, biopsychosocial factors and women were used as keywords in the search. Also, the articles focusing on any aspects of sexual desire such as biological, social and psychological factors and relationship factors alone or integrated, were included in the study. The articles which specifically targeted the hypoactive sexual desire disorder in pregnant and lactating women and also the articles targeting biopsychosocial factors related to other types of sexual function disorder such as arousal disorder, orgasm disorder and dyspareunia, were all excluded from this study.
Findings:
After reviewing the literature, the findings were categorized in three main class of effect of biologic factors on sexual desire and sexual hypoactivity, the effect of psychological factors on sexual desire and the effect of cultural factors and couple’s relationship on sexual desire, each of these domains cover a wide range (such as hormonal changes, chronic diseases, psychological difficulties (perceived stress, anxiety, depression). Incompatibility of couples, the spouse’s sexual function disorder) which may overlap. Because of the complexity of etiology and the difficulty of treating hypoactive sexual desire disorder, it is necessary to use biopsychosocial approaches to diagnose and treat the disorder.
Conclusion:
According to the findings of this reviewing study, the factors able to affect sexual desire and activity are not distinct and often overlap, therefore, the complicated etiology of hypoactive sexual desire disorder often needs multidimensional intervention to use biopsychosocial approach; Multi factor assessment with a combination of psychological, physical, social and hormonal intervention can be effective in making strategies to treat the symptoms of HSDD.
Keywords: hypoactive sexual desire, related factors, women
1. INTRODUCTION
As a mental response to sexual stimuli, sexual desire determines human sexual behavior and represents the cognitive capacity of sexual stimulation (1, 2) and it also has a biological and interpersonal basis (3). Hypoactive sexual desire disorder (HSDD) is currently defined by the American Psychiatric Association’s Diagnostic and Statistical Manual IV-TR (DSM-IV-TR) as “persistently or recurrently deficient (or absent) sexual fantasies and desire for sexual activity” which causes “marked distress or interpersonal difficulty” (4). Hypoactive sexual desire is a common problem among women which is usually related to medical and psychological problems, incompatibility in a relationship and age. Nevertheless, the relative contribution of each of these aspects hasn’t been identified. The prevalence of sexual desire disorder -depending on the criteria used for defining–varies from 3-31% (5).
The etiology of hypoactive sexual desire disorder is multi-factorial, including biological, psychological, sexual factors and it is related to the social context (6). Levin defines sexual desire as a structure dependent on the balance among three basic aspects, namely, biological aspects, psychological aspects or aspects depending on how a person think, and cultural aspects (2).
Medical problems such as cardiovascular, neurological and endocrine diseases (1, 2), breast cancer (6), women diseases like pelvic pain and pelvic floor disorders(1) affect the sexual performance physically or as the consequence of treatment with medication or surgery and also affect the psychological situation of the couple and their compatibility in directly, and decrease sexual desire (2). Psychological factors such as sexual abuse, emotional neglect in childhood, traumatic experiences during puberty, perceived stress, anxiety, depression and body image concerns (7) not only affect sexual desire directly, but also can be related to dysfunction cognition (cognition related to the decrease to self - confidence) or incompatibility of the couples, so they can affect sexual desire this way too (2). Social factors such as social norms, life experience and attitude toward the framework of sexual desire also affect both sexual behavior and frequency of sexual desire (8). In fact, in many countries, the issue of sexual disorders is still a taboo which negatively affect life quality (9).
The functions of sexual activity in marital relationships are paradoxical. On the one hand, healthy sexuality of the couples have a minor basic role in couple’s joy and satisfaction. On the other hand, dysfunctional sexual activities and especially refraining from it have a huge negative impact on the discharge of intimacy and joy in couple’s relationship and threatens its stability (10). Therefore, problems in any field of sexual experience must be considered as a part of community health assessment (11).
What makes this review study important and noticeable, is dealing with components which play important roles in recognizing factors related to HSDD in women in reproductive age. Understanding, recognizing and diagnosing factors related to HSDD results in increased knowledge of fertility and sexual health care providers in order to prepare education and consultative programs and policies to improve women’s sexual health.
2. METHODOLOGY
The search was done from January to March 2015 by the use of the data bases ProQuest, Pubmed, CINAHL, Ovid and Medline, and the words sexual desire, related factors were used as free text words; the words reduce sexual desire, hypoactive sexual desire disorder, Dyadic relationship, biopsychosocial factors and women were used as keywords in the search. Also, the reference list of the literature were investigated to increase the sensitivity and choose more studies. The complete texts or summaries of all the articles, documents and reports obtained through advanced research, were extracted. After eliminating the repeated items, the irrelevant items were eliminated by checking the title, abstract and the full text of the articles, respectively, and the relevant articles were chosen.
In the process of search, 10524 articles about the factors related to sexual disorders by using the chosen keywords and the highest sensitivity. This number shrunken to 1326 after limiting the strategy, and again 497 got eliminated because they were repeated. Following the title and the abstract, 829 articles were assessed and 732 were excluded because they were irrelevant. Also, from 97 remaining articles, 81 were excluded after checking the full text and 4 articles were added by checking the reference. 16 articles were assessed according to the criteria of inclusion and exclusion. 8 of which got excluded from the current research and finally 8 articles were included this review article.
Figure 1.
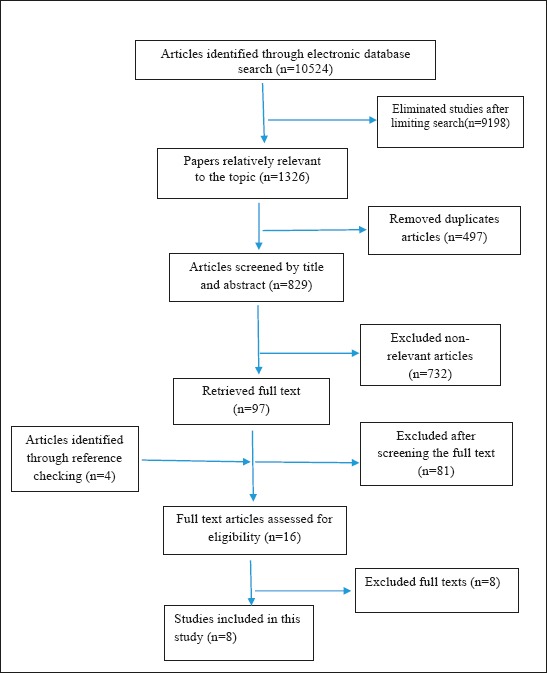
Literature search and review flowchart for selection of primary studies
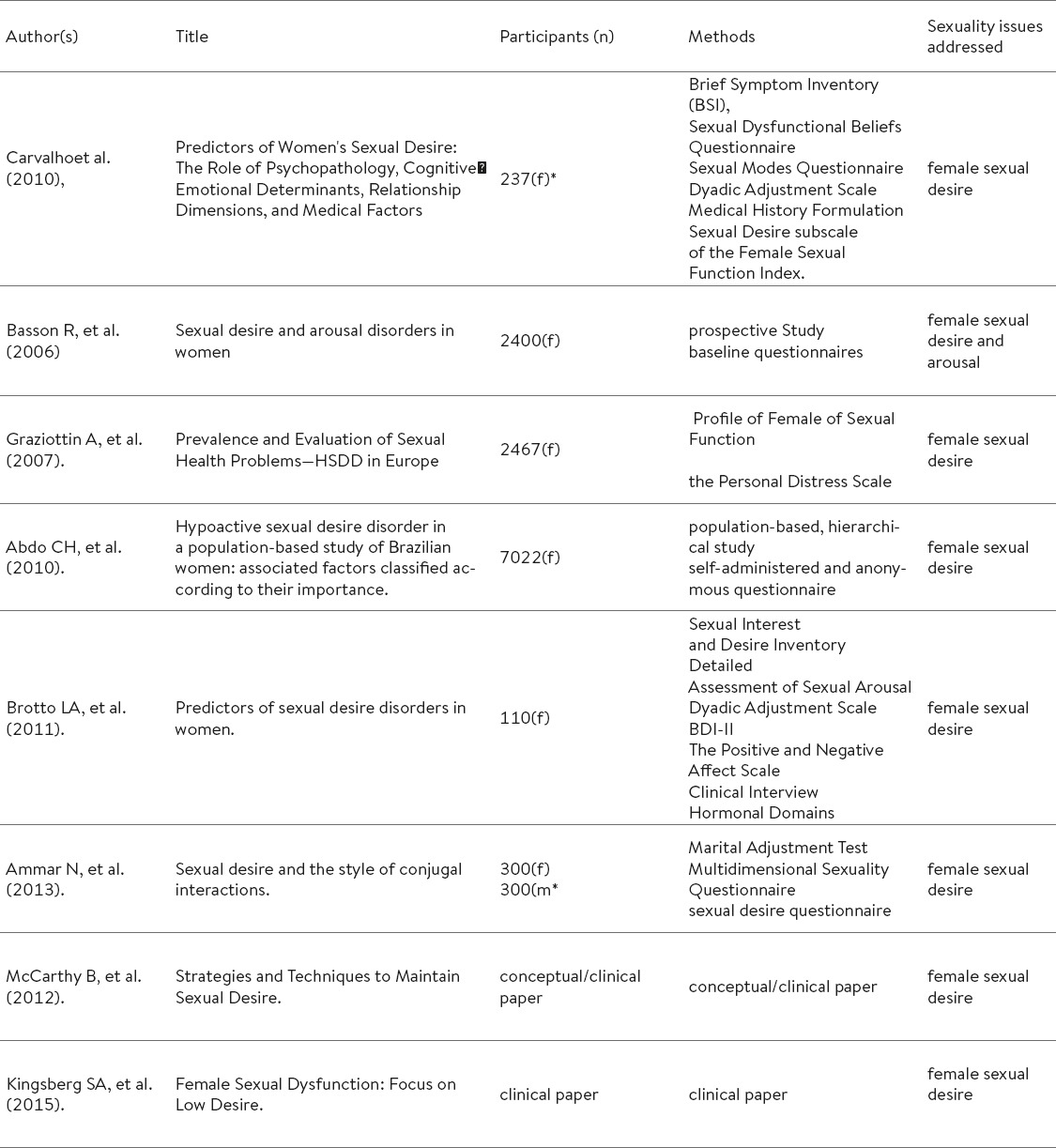
Table 1.
Selected articles included in review
2.1. Inclusion criterion:
Articles published from 2000 to 2015 relevant to determinants of HSD were included in this investigation. Moreover, articles focusing solely on any of the aspects related to sexual desire such as biological, psychological and social factors and relationship factors, were also included for the issue of HSDD in women be investigated extensively.
2.2. Exclusion criterion:
Articles which specifically targeted HSDD in pregnant or lactating mothers were excluded from this review study. Also studies about biopsychosocial factors related to other types of sexual function disorder such as arousal disorder, orgasm disorder and dyspareunia were excluded too.
3. RESULTS
After reading the text, the findings were divided in three main classes:
3.1. The effect of biological factor on women‘s sexual desire
HSDD as a single and independent complaint is not common among women in reproductive age, and in young women the complaint appears in the field of chronic diseases and gynecological disorder; but in order women, HSDD is usually common as a single complaint (12). It has been reported that the transition to menopause and the menopause itself intensify HSDD. This complicated situation is experienced by all women through emotional and physical changes related to decrease in the production of ovarian Sex hormones. When a sudden decrease happens in the production of estrogens and androgens after menopause by surgery or chemotherapy, there will be more side-effects on HSDD (13). Studies show that among all the factors affecting sexual desire, the process of aging is the most important. Although the proportion of women with HSDD rises with the increase of the age, the proportion of women’s distress and unhappiness about their HSDD decreases with the increase of the age and the situation of menopause (6).
Sexual function needs a complicated interaction of many neurotransmitters and hormones, both central and environmental, and sexual desire is the result of the interaction among the inhibitory and excitatory pathways in brain. For example, dopamine, estrogen, progesterone and testosterone play an excitatory role, while serotonin and prolactin are inhibitors. Therefore, HSDD can be the result of decrease in excitatory hormones or increase in inhibitory hormones or both (14).
Another group of biological factors affecting sexual desire is the chronic diseases. Chronic diseases can affect critical psychological needs for direct and indirect maintenance of women’s sexual function (6). Chronic diseases change the dynamics of the relationship and can be deep negative effect on the relationship and sexual satisfaction of both the patient and their sexual partner. The effect of chronic diseases on sexual function is multi-factorial and they can affect all response phases of sexual cycle; also, the effects of these decreases can themselves be categorized in the biological, psychological, social classes (15).
In a big study on Brazilian women, it was shown that cardiovascular diseases, breast cancer, PTSD, being old, vaginal dryness and dyspareunia were associated with increased risk of HSD and have important negative effects on sexual desire (6). In another study they showed that age, parity, length of relationship, pregnancy, relationship status, plans and methods of contraception (especially oral contraceptive) are associated with decreased sexual activity (16). Nevertheless, in another study they showed that age is directly and education and marriage age (below 18) are inversely associated with increased risk of HSD. But they didn’t find a relation between the history of smoking, previous pelvic surgery and contraception methods (9). In fact there is a combination of evidence in the studies about the effect of using contraceptives on sexual desire.
Some studies show the negative relationship between the use of contraception pills and sexual desire and some others report their neutral effect and some report their positive effect on sexual desire (17). Among other important factors affecting sexual desire and causing HSDD are the drugs used for treating diseases such as antihypertensive drugs, SSRIs, hormonal antagonists and chemotherapy (18). In fact, although organic changes have a central role in human sexual activity, separating biological factors from their natural interaction with other aspects is different (2).
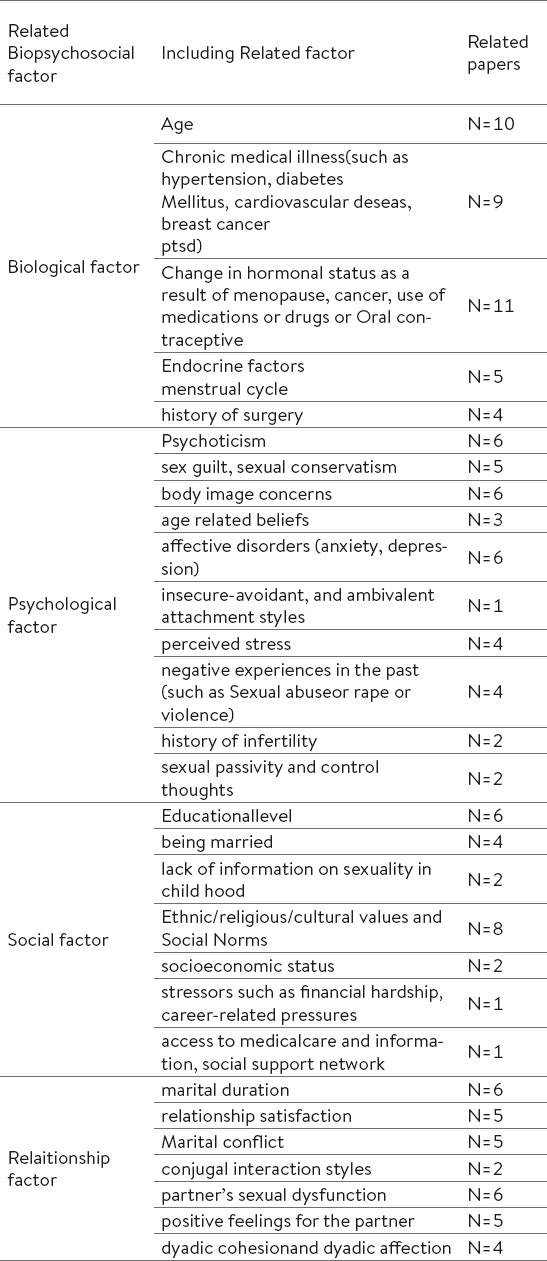
Table 2.
Extraction of related factor of HSDD to category & subcategory. *(f= female, m= male)
3.2. The effect of psychological factors on women’s sexual desire
It has been shown that psychopathology has contradictory effects on sexual desire; so that, mental disorders such as depression, anxiety, anorexia nervosa, obsessive-compulsive disorders and schizophrenia are intensely associated with women’s HSDD (19-21). Despite this strong relation, a few women reported higher sexual desire a long the psychopathology (2, 22).
Also, it was shown that different sexual disorders such as arousal disorder and disorder of desire and satisfaction are different consequences of anxiety disorders, also, there is an obvious relationship between depression and women’s sexual disorders like desire disorder (14). Negative temper such as anxiety and depression are usually associated with decreased desire and arousal. Nevertheless, some evidence shows that anxiety and depression may increase sexual desire. Women report various changes in both their moods and their sexual desire during different phases of their menstrual cycle, so that some women report higher levels of sexual desire during their premenstrual phase even when they show depression (22). It has been reported that people with Sexual Dysfunction showed more unhealthy (more inefficient) sexual beliefs and automatically more negative thoughts and feelings during their sexual activity. In fact, negative cognitive Content in the field of sexuality, decreases the ability to process sexual stimuli and contributes to the existence of sexual problems (23). Also, It seems that the feelings of guilt and anger have the important central role in having or not having sexual desire (24, 25) so that studies showed the feeling of sexual guilt affects sexual desire negatively and decrease it (24, 26).
Studies announced factors such as attitudes, negative cognition, mood, welfare, self-esteem, feelings toward the partner, sexual performance of the partner and distress about the relationship especially sexual relationship as the psychological factors associated with sexual desire (4, 27). Women’s positive feelings toward their sexual partners have important effects on sexual desire and work as a shield against harmful effects of menopausal symptoms (4). So that the investigation of women’s health around the world showed that feelings toward the sexual partner and attitudes toward sexual activity and age have more effects on sexual desire and activity than the process of menopause transition (28). Nonetheless, it was discovered in later studies that the only predictable variable of sexual response and sexual desire at the time being is the woman’s previous level of sexual response (29).
3.3. The effect of cultural factors and couple’s relationship on women’s sexual desire
The effect of social aspects on sexual desire must be considered, too. Cultural, society, religious values, especially customs all can negatively affect sexual desire, especially in women grown-up in very restrictive cultures and religions (30, 31). Relationship factors such as the partner’s sexual dysfunction or conflict (such as arousal disorder or premature ejaculation in male partners) stressors such as financial hardship, pressure related to job or familial obligations can be associated with decreased sexual desire (30). Social norms, life experience and attitudes about sexuality affect both sexual behavior and the frequency of sexual desire, therefore, sexual behavior and desire may vary according to the paths that make marital roles and marital intimacy (8, 32). Some couples put a lot of value on the similarity of values and the harmony between them and sharing time and activities with their parents; while in contrast, some couples are focused on maintaining the independence of each of the partners and several studies have shown the negative effect of the sexual partner’s independence on marital satisfaction. Gender equality is also another dimension of cooperation that should be studied. Some studies have observed greater conjugal satisfaction in couples who maintain equal gender role distribution, but it’s effects on sexual desire has rarely been studied (8).
Problems with expressing sexual needs, desires and fears between couples are among factors which have direct negative affects on women’s sexual desire on sexual activity (7). In a larger picture, we can see that depending on the way people organize their intimate relationship in society, sexual desire between couples have unequal importance, and to investigate sexual desire and marital satisfaction, it should be dealt with from a sociological point of view, too (8), Because cultural aspects are associated with expressing sexuality in both genders (male and female) (33).
Sexual desire is also important the relationship’s dynamics and compatibility, so that it has been shown that women with lower sexual desire towards their sexual partner, reported less marital compatibility. Factors such as positive feelings, trust and couple‘s intimacy increases sexual desire in both genders (1), While couple’s stability and marriage duration leads to maintenance of sexual desire in women (34). Deficient sexual desire may reflect marital dissatisfaction as a compatibility mechanism (1). Women with HSDD reported weaker couple’s compatibility, more dissatisfaction in solving conflicts in relationships and less emotional intimacy and attraction with their partner compared to women without the disorder. Nevertheless some studies reported that women might experience a satisfactory sexual life without apparent sexual desire for sexual activity (7).
4. DISCUSSION
Reviewing the literature, we can see that compared to women without HSDD, women with HSDD reported items such as dissatisfaction with their sexual life and marriage, feelings of hopelessness, frustration, anger and a loss of femininity and low self-esteem with higher probability (35). Also, the score of life quality in women with HSDD is less than that of women without it; so that it has been shown that HSDD causes disorders in life quality related to health (36), and there is a significant relationship between sexual desire and other areas of sexual function, and sexual desire is a noticeable predictor of sexual activity and life quality (37). Therefore, sexual concerns in any area of the sexual experience should be addressed as part of a holistic health assessment (11, 30). The professions of health must directly try to develop educational or counseling programs related to sexual health of women suffering from sexual disorders including sexual desire in order to help them reach a satisfactory sexual life and improve life quality (37).
Reviewing the studies, we realize that factors able to affect sexual desire and activity are not distinct and may overlap (38). Complex etiology of low sexual desire often requires a multiple intervention in order to use the biopsychosocial approach, and taking a complete history can help identify the conditions that lead to low sexual desire (30). In general and in short, psycho-sexual evaluation in HSDD, is by using the standard method for assessing it and lack of Standard approach, brings dangers. The clinical history may be perceived more in the psychological plane by the psychologically minded and more in the biological plane by the medically orientated. This might ultimately lead to the exclusion of a specific area in treatment (39). It has been proved that the most successful treatments for sexual disorders are physiological -psychological ones, in which physiological changes have circular interaction with a psychological change (40).
Medical and psychological treatments of sexual disorders including sexual desire need to target the complex biopsychosocial effects in the patient, and the biopsychosocial model provides an integrated model for understanding and treating sexual problems (41). In fact, the features of low sexual desire treatment is multifaceted, and need to be a combination of being able to maximize the biological signals of sexual response drive and psychosocial treatments in order to overcome personal and relationship problems (42). For the cooperation among Physicians, there is a widespread need for medical attention from different scientific majors in assessment, treatment and educational issues in the frame of sexual function disorder including sexual desire. In many cases, therapy and medical intervention alone aren’t enough to solve the enduring sexual problems. Assessing sexual function disorder including sexual desire has to include questions about predisposing factors, detecting factors and combination factors, and there is a clear emphasis on using individual psychotherapy methods, and more studies are needed to identify combinational and integrated treatments for sexual disorders (41), Because treating sexual disorder has come to a point where it needs a change in paradigm. This paradigm shift is towards the integrations of medical treatment, biological /individual treatment, couple therapy and more widely in the areas of religion, history and culture (43).
5. CONCLUSION
Considering different influential aspects in women’s sexual desire, there is need for cooperation among health service providers from different scientific fields in assessing, treating and teaching issues about low sexual desire, and a multi-factorial assessment with a combination of psychological, social, physical and hormonal intervention may be a good model for presenting treatment strategies of low sexual desire, and medical and psychological treatments for sexual disorders especially low sexual desire need to target the complex biopsychosocial effect on the patient, sexual partner and in fact the couple. Therefore a work team of different scientific fields who are allowed to have comprehensive assessment of sexual health and also providing interventional packages mostly for women with this disorder are necessary.
Limitations: Since this study was conducted in a sample of women in reproductive age, in order to complete the information, we suggest that similar studies be widely conducted about factors related to low sexual desire in men and women in different group ages, so the results can be used to provide decent educational and medical programs in the form of educational-medicinal approaches such as pre-marital counseling, sex education, sex therapy and marital therapy based on culture, because satisfactory sexual function can contribute to general health in society and lead to marital satisfaction and finally strengthening the family.
Acknowledgement of financial support
This article is a part of project in master’s degree in midwifery counseling. All colleagues who assisted us in this article are appreciated. We sincerely appreciate Mazandaran University of Medical Sciences and the Student Research Committee to assist in conducting the research and financing.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Carvalho J, Nobre P. Predictors of Women’s Sexual Desire: The Role of Psychopathology, Cognitive Emotional Determinants, Relationship Dimensions, and Medical Factors. The Journal of Sexual Medicine. 2010;7(2pt2):928–937. doi: 10.1111/j.1743-6109.2009.01568.x. [DOI] [PubMed] [Google Scholar]
- 2.Carvalho J, Nobre P. Biopsychosocial determinants of men’s sexual desire: Testing an integrative model. The Journal of Sexual Medicine. 2011;8(3):754–763. doi: 10.1111/j.1743-6109.2010.02156.x. [DOI] [PubMed] [Google Scholar]
- 3.Basson R. Rethinking low sexual desire in women. BJOG: An International Journal of Obstetrics & Gynaecology. 2002;109(4):357–363. doi: 10.1111/j.1471-0528.2002.01002.x. [DOI] [PubMed] [Google Scholar]
- 4.Brotto LA, Petkau AJ, Labrie F, Basson R. Predictors of sexual desire disorders in women. The Journal of Sexual Medicine. 2011;8(3):742–753. doi: 10.1111/j.1743-6109.2010.02146.x. [DOI] [PubMed] [Google Scholar]
- 5.McCabe MP, Goldhammer DL. Prevalence of Women’s Sexual Desire Problems: What Criteria Do We Use? Archives of Sexual Behavior. 2013;42(6):1073–1078. doi: 10.1007/s10508-013-0107-z. [DOI] [PubMed] [Google Scholar]
- 6.Abdo CH, Valadares AL, Oliveira WM, Jr, Scanavino MT, Afif-Abdo J. Hypoactive sexual desire disorder in a population-based study of Brazilian women: associated factors classified according to their importance. Menopause. 2010;17(6):1114–1121. doi: 10.1097/gme.0b013e3181e19755. [DOI] [PubMed] [Google Scholar]
- 7.Brotto LA, Bitzer J, Laan E, Leiblum S, Luria M. Women’s sexual desire and arousal disorders. The Journal of Sexual Medicine. 2010;7(1pt2):586–614. doi: 10.1111/j.1743-6109.2009.01630.x. [DOI] [PubMed] [Google Scholar]
- 8.Ammar N, Widmer E. Sexual desire and the style of conjugal interactions. Sexologies. 2013;22(4):e81–e7. [Google Scholar]
- 9.Safarinejad MR. Female sexual dysfunction in a population-based study in Iran: prevalence and associated risk factors. International Journal of Impotence Research. 2006;18(4):382–395. doi: 10.1038/sj.ijir.3901440. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy B, Farr E. Strategies and Techniques to Maintain Sexual Desire. Journal of Contemporary Psychotherapy. 2012;42(4):227–233. [Google Scholar]
- 11.Maciel M, Laganà L. Older Women’s Sexual Desire Problems: Biopsychosocial Factors Impacting Them and Barriers to Their Clinical Assessment. BioMed Research International 2014. 2014 doi: 10.1155/2014/107217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayes RD, Dennerstein L, Bennett CM, Koochaki PE, Leiblum SR, Graziottin A. Relationship between hypoactive sexual desire disorder and aging. Fertility and sterility. 2007;87(1):107–112. doi: 10.1016/j.fertnstert.2006.05.071. [DOI] [PubMed] [Google Scholar]
- 13.Castelo-Branco C, Palacios S, Combalia J, Ferrer M, Traveria G. Risk of hypoactive sexual desire disorder and associated factors in a cohort of oophorectomized women. Climacteric. 2009;12(6):525–532. doi: 10.3109/13697130903075345. [DOI] [PubMed] [Google Scholar]
- 14.Simon JA. Low sexual desire - is it all in her head? Pathophysiology, diagnosis, and treatment of hypoactive sexual desire disorder. Postgraduate medicine. 2010;122(6):128–136. doi: 10.3810/pgm.2010.11.2230. [DOI] [PubMed] [Google Scholar]
- 15.McInnes RA. Chronic illness and sexuality. Medical Journal of Australia. 2003;179(5):263–266. doi: 10.5694/j.1326-5377.2003.tb05535.x. [DOI] [PubMed] [Google Scholar]
- 16.Dennerstein L, Hayes RD. Confronting the challenges: Epidemiological study of female sexual dysfunction and the menopause. The Journal of Sexual Medicine. 2005;2(3):118–132. doi: 10.1111/j.1743-6109.2005.00128.x. [DOI] [PubMed] [Google Scholar]
- 17.Roberts SC, Cobey KD, Klapilová K, Havlíček J. An evolutionary approach offers a fresh perspective on the relationship between oral contraception and sexual desire. Archives of Sexual Behavior. 2013;42(8):1369–1375. doi: 10.1007/s10508-013-0126-9. [DOI] [PubMed] [Google Scholar]
- 18.Basson R, Schultz WW. Sexual sequelae of general medical disorders. The Lancet. 2007;369(9559):409–424. doi: 10.1016/S0140-6736(07)60197-4. [DOI] [PubMed] [Google Scholar]
- 19.Dobkin RD, Leiblum SR, Rosen RC, Menza M, Marin H. Depression and sexual functioning in minority women: current status and future directions. Journal of Sex & Marital Therapy. 2006;32(1):23–36. doi: 10.1080/00926230500229251. [DOI] [PubMed] [Google Scholar]
- 20.Mercan S, Karamustafalioglu O, Ayaydin EB, Akpinar A, Goksan B, Gonenli S, et al. Sexual dysfunction in female patients with panic disorder alone or with accompanying depression. International journal of psychiatry in clinical practice. 2006;10(4):235–240. doi: 10.1080/13651500600649994. [DOI] [PubMed] [Google Scholar]
- 21.Van Minnen A, Kampman M. The interaction between anxiety and sexual functioning: a controlled study of sexual functioning in women with anxiety disorders. Sexual and Relationship Therapy. 2000;15(1):47–57. [Google Scholar]
- 22.Lykins AD, Janssen E, Graham CA. The relationship between negative mood and sexuality in heterosexual college women and men. Journal of Sex Research. 2006;43(2):136–143. doi: 10.1080/00224490609552308. [DOI] [PubMed] [Google Scholar]
- 23.Nobre PJ, Pinto-Gouveia J. Dysfunctional sexual beliefs as vulnerability factors for sexual dysfunction. Journal of Sex Research. 2006;43(1):68–75. doi: 10.1080/00224490609552300. [DOI] [PubMed] [Google Scholar]
- 24.Terimourpour N, Bidokhti NM, Pourshahbaz A. The Relationship between attachment styles and sexual desire among Iranian women. Procedia-Social and Behavioral Sciences. 2011;30:108–112. [Google Scholar]
- 25.Nobre PJ. Determinants of sexual desire problems in women: Testing a cognitive-emotional model. Journal of Sex & Marital Therapy. 2009;35(5):360–377. doi: 10.1080/00926230903065716. [DOI] [PubMed] [Google Scholar]
- 26.Woo JS, Brotto LA, Gorzalka BB. The role of sex guilt in the relationship between culture and women’s sexual desire. Archives of Sexual Behavior. 2011;40(2):385–394. doi: 10.1007/s10508-010-9609-0. [DOI] [PubMed] [Google Scholar]
- 27.Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira E, et al. Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. International Journal of Impotence Research. 2005;17(1):39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 28.Avis NE, Zhao X, Johannes CB, Ory M, Brockwell S, Greendale GA. Correlates of sexual function among multi-ethnic middle-aged women: results from the Study of Women’s Health Across the Nation (SWAN) Menopause. 2005;12(4):385–398. doi: 10.1097/01.GME.0000151656.92317.A9. [DOI] [PubMed] [Google Scholar]
- 29.Dennerstein L, Lehert P. Modeling mid-aged women’s sexual functioning: a prospective, population-based study. Journal of Sex & Marital Therapy. 2004;30(3):173–183. doi: 10.1080/00926230490262375. [DOI] [PubMed] [Google Scholar]
- 30.Kingsberg SA, Woodard T. Female Sexual Dysfunction: Focus on Low Desire. Obstetrics & Gynecology. 2015;125(2):477–486. doi: 10.1097/AOG.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 31.Kingsberg SA, Rezaee RL. Hypoactive sexual desire in women. Menopause. 2013;20(12):1284–300. doi: 10.1097/GME.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 32.Green AI. The Social Organization of Desire: The Sexual Fields Approach*. Sociological Theory. 2008;26(1):25–50. [Google Scholar]
- 33.Baumeister RF. Gender and erotic plasticity: Sociocultural influences on the sex drive. Sexual and Relationship Therapy. 2004;19(2):133–139. [Google Scholar]
- 34.Lachtar C, Lachtar F, Jarraya A. Sexual desire in Tunisian conjugal couple: Particularities and maintenance factors. Ann Med Psychol. 2006;164:402–409. [Google Scholar]
- 35.Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive sexual desire disorder in postmenopausal women: US results from the Women’s International Study of Health and Sexuality (WISHeS) Menopause. 2006;13(1):46–56. doi: 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 36.Biddle AK, West SL, D’Aloisio AA, Wheeler SB, Borisov NN, Thorp J. Hypoactive sexual desire disorder in postmenopausal women: quality of life and health burden. Value in Health. 2009;12(5):763–772. doi: 10.1111/j.1524-4733.2008.00483.x. [DOI] [PubMed] [Google Scholar]
- 37.Kim H. Sexual Desire, Sexual Function, and Quality of Life in Married Women with Hypoactive Sexual Desire Disorder. Korean J Health Educ Promot. 2013;30(5):163–175. [Google Scholar]
- 38.Basson R, Brotto LA, Laan E, Redmond G, Utian WH. Original Research - Women’s Sexual Dysfunctions: Assessment and Management of Women’s Sexual Dysfunctions: Problematic Desire and Arousal. The Journal of Sexual Medicine. 2005;2(3):291–300. doi: 10.1111/j.1743-6109.2005.20346.x. [DOI] [PubMed] [Google Scholar]
- 39.Graziottin A. Original Reasearch: Prevalence and Evaluation of Sexual Health Problems - HSDD in Europe. The Journal of Sexual Medicine. 2007;41(3):211–219. doi: 10.1111/j.1743-6109.2007.00447.x. [DOI] [PubMed] [Google Scholar]
- 40.Heiman JR. Psychologic treatments for female sexual dysfunction: are they effective and do we need them? Archives of Sexual Behavior. 2002;31(5):445–450. doi: 10.1023/a:1019848310142. [DOI] [PubMed] [Google Scholar]
- 41.McCabe M, Althof SE, Assalian P, Chevret-Measson M, Leiblum SR, Simonelli C, et al. Psychological and interpersonal dimensions of sexual function and dysfunction. The Journal of Sexual Medicine. 2010;7(1pt2):327–336. doi: 10.1111/j.1743-6109.2009.01618.x. [DOI] [PubMed] [Google Scholar]
- 42.Nappi RE, Albani F, Santamaria V, Tonani S, Martini E, Terreno E, et al. Menopause and sexual desire: the role of testosterone. Menopause international. 2010;16(4):162–168. doi: 10.1258/mi.2010.010041. [DOI] [PubMed] [Google Scholar]
- 43.Weeks Gr. The emergence of a new paradigm in sex therapy: Integration. Sexual and Relationship Therapy. 2005;20(1):89–103. [Google Scholar]