Abstract
Introduction:
Patients’ health and safety is not only a function of complex treatments and advanced therapeutic technologies but also a function of a degree based on which health care professionals fulfill their duties effectively as a team. The aim of this study was to determine the attitude of hospital committee members about teamwork in Kerman hospitals.
Methodology:
This study was conducted in 2014 on 171 members of clinical teams and committees of four educational hospitals in Kerman University of Medical Sciences. To collect data, the standard “team attitude evaluation” questionnaire was used. This questionnaire consisted of five domains which evaluated the team attitude in areas related to the team structure, leadership, situation monitoring, mutual support, and communication in the form of a 5-point Likert type scale. To analyze data, descriptive statistical tests, T-test, ANOVA, and linear regression were used.
Results:
The average score of team attitude for hospital committee members was 3.9 out of 5. The findings showed that leadership had the highest score among the subscales of team work attitude, while mutual support had the lowest score. We could also observe that responsibility was an important factor in participants’ team work attitude (β = -0.184, p = 0.024). Comparing data in different subgroups revealed that employment, marital status, and responsibility were the variables affecting the participants’ attitudes in the team structure domain. Marital status played a role in leadership; responsibility had a role in situation monitoring; and work experience played a role in domains of communication and mutual support.
Conclusions:
Hospital committee members had a positive attitude towards teamwork. Training hospital staff and paying particular attention to key elements of effectiveness in a health care team can have a pivotal role in promoting the team culture.
Keywords: health care teams, attitude, hospital committee, team STEPPS
1. INTRODUCTION
Organizations increasingly use teams to do their work which was traditionally given to individuals (1). The reason why organizations seek teamwork is that teams can, in most cases, be more successful than individuals who work alone. More effective and better decisions can be made when people work together (2). Moreover, team works are often more efficient and more effective than individual work (3). In addition, using teams can result in increased safety (4), improved people’s attitudes, and decreased number of absentees (5).
There is enough evidence on the importance of people’s participation in health care teams (6). Teams in health care organizations are made up of physicians, nurses and other health technicians who officially work to achieve organizational goals (7). The basic idea is that patient’s health and safety is not only a function of complex treatments and advanced therapeutic technologies but also a function of a degree based on which health care professionals fulfill their duties effectively as a team (8).
In addition to promoting mutual support and understanding among members of the health care teams, multidisciplinary teams have the potentials to improve relationships, increase efficiency and coordination and finally improve patient’s health (9).
Although there is not much documentation about the evaluation of individual’s team skills in health care section (6), evaluating teams is an important tool in order to increase efficiency and productivity of teams (10). In this case, what is agreed upon is that its members must experience sufficient time and togetherness so as to rate the team’s performance in terms of six scales: 1) teamwork 2) decision-making 3) leadership support 4) trust and respect 5) recognition and reward 6) focusing on customers (2).
Different studies show the importance of teams and their effective roles in achieving the goals in health care organizations. Brewer and Mendelson suggested that multidisciplinary teams were necessary but not enough to be effective. In addition, effective teams need both integrity and diversity (11). As well as, Nancarrow et al highlighted ten basic effective features of multidisciplinary team working (12).
In their research on developing and testing self-evaluation tools for cancer improvement multidisciplinary teams, Taylor et al stated that self-evaluation of team performance could lead to the development of multidisciplinary teams (13).
As there is scant evidence regarding the assessment of hospital teams in Iran and due to researches on team performance in non-hospital sectors in other countries, we decided to conduct this research because knowing the attitudes of team members in an Iranian context can have a significant effect on managing health care teams and the resultant would be better performance.
Since health care teams present health care in the form of hospital committees in Iran hospitals and concerning the effective roles of these teams at hospitals, the aim of this research was to determine the attitudes towards team working among hospital committee members in Kerman hospitals.
2. METHODOLOGY
This descriptive cross-sectional study was conducted in 2014. The study population consisted of 171 members of clinical teams in committees of 4 educational hospitals in Kerman, Iran. Participants entered the study based on census method. They were at health administration and clinical groups.
The 30 item Testing Team Attitudes Questionnaire (T-TAQ) was used to collect data that was jointly proposed in 2008, as Team Strategies & Tools to Enhance Performance & Patient Safety (Team STEPPS), by the American Agency for Healthcare Research and Quality and the American Department of Defense as the American national standard (14).
T-TAQ has not been used in Iran. This questionnaire has 5 domains in titled: Team structure, Leadership, Situation monitoring, Mutual support, Communication, in which each domain includes 6 questions.
The first part of the questionnaire contained demographic information. Respondents were asked to rate the statements on a five-point scale ranging from 1 to 5 (1 strongly agree and 5 strongly disagree). The total score of all five domains determined the team work attitude of the hospital committees. External, formal and content validity and reliability of this questionnaire were determined and confirmed in a study by Najafi et al in 2012 (15).
The study population consisted of 220 medical personnel who were members of at least one hospital committee. Of this population, 171 completed and returned the questionnaires. Those participants who were members of different teams were evaluated only in one team.
All questionnaires were completed anonymously during the committee meetings and confidentiality of the data was maintained. To collect data, a written permission was obtained from hospital authorities and Kerman University of Medical Sciences (KUMS).
Data were analyzed using descriptive statistics, statistical tests, T-test, ANOVA, and linear regression. SPSS software version 20 was used for data analysis.
3. FINDINGS
Of 171 personnel who participated in this study, 111 participants (64%) were women and 144 (84%) participants were married. The average age of participants was 36 years (SD=7.9), and the average work experience was 10.5 years (SD =7.7). 102 participants (60%) worked in the health care field and 69 participants worked (40%) in the administrative field. 79% of participants had a bachelor’s degree or lower.
The total mean score of hospital committees regarding team attitude was 3.9 out of 5 (SD = 0.31). Of all sub-criteria of team attitude, leadership and mutual support had the highest and lowest scores respectively (4.9 and 3.7). The mean score of hospital committees in terms of team attitude in all five areas was as follows: leadership 4.19 (SD = 0.4); monitoring status 4 (SD = 0.5); team structure 3.8 (SD = 0.4); communication 3.8 (SD = 0.5); and mutual support 3.7 (SD = 0.5). Table 1 shows mean and standard deviation of team attitude questions.
Table 1.
Mean score of teamwork attitude questions

The highest team attitude score was related to Afzalipour Hospital, while the lowest score was given to Shahid Beheshti Hospital and Shafa Hospital (Table 2).
Table 2.
Teamwork attitude’s mean score in Kerman hospitals
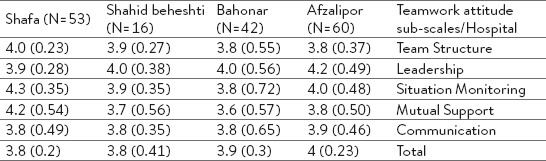
Table 3 shows the relationship between team work attitude sub-scales and variables such as employment, work experience, age, gender, education, marital status, and responsibility. Regression analysis indicated that responsibility was the most important factor (β= -0.184, p = 0.024). Among the sub-scales of team work attitude, employment, marital status, and responsibility were the factors affecting the attitude of team structure. Marital status played a role in leadership; responsibility had a role in situation monitoring; and work experience had a role in domains of communication and mutual support.
Table 3.
linear regression results based on respondent characteristics

4. DISCUSSION
Participants generally had a positive attitude towards teamwork in hospitals. The average score of team attitude was 3.9 out of 5. Positive attitudes towards behaviors related to effective teamwork and safety among nurses and surgeons were also reported by Flin et al (16).
Among the five teamwork attitude sub-scales, the leadership domain had the highest score. This shows that participants had a good attitude towards the role of leadership in health care teams. We can conclude that the team leader had the ability to coordinate activities appropriately, was sure that care programs were completely understood and care duties were fulfilled properly. Similarly, Edmondson mentioned the proper role of cardiologists in leading health care teams. Facilitating communications among team members and developing the art of correct communication among team members, he improved their performance (17).
In a study carried out by Mercer et al, suitable communication i.e. transmitting information between the members of a team or between them and the patients was reported (18). By the same token, Kilner et al showed suitable communication in a team and positive attitude towards teamwork. In this study, good communication in hospital teams in emergency centers not only improved patients and employees’ satisfaction, but also reduced errors and improved patient’s safety (19). In a study by Christian et al on patient’s safety in the operating rooms, lack of communication and sharing information were two main factors which risked the patient’s safety (20); moreover, committee members had a moderate attitude towards communication.
Attitude towards a team structure was at an average level in the studied hospitals. Campion et al reported that the aim of organizational support is to achieve goals (21). According to Friedlander, organizational support is having clear objectives and a proper combination of experience, skills and sufficient resources (22).
Monitoring members of a team and their knowledge of conditions of their team members and patients caused people to have more effective roles in their teams (23). According to a study by Loughry et al, monitoring a team member by his teammates was considered as a benchmark for his effectiveness (24). In the present study, however, the participants had a moderate attitude in this regard.
Participants’ attitude towards mutual support had the lowest score in the present study. However, mutual support reduced workload and increased patients’ safety (25). In a study by Liebman and Hyman, health care providers who needed more support were more willing to talk with patients about errors, to answer questions and to express their feelings (26). Poor attitude of members towards mutual support can be due to cultural aspects of personnel, lack of awareness, and inadequate training.
We could also observe that gender and education level had no significant impact on the attitude of team members. This finding is not in line with a study conducted by Thomas who showed that team attitude had a significant impact on physicians and nurses (27).
The results of regression analysis revealed that people who had some responsibilities in health care teams (compared to those with no responsibility) had more positive attitude towards their teams. However, Curran stated that work experience and age had an impact on the attitude of team members (9). The role of responsibility in increasing the team attitude in the present study might be due to in-service training courses held for officials in medical teams.
Concerning attitude of members of hospital teams towards team structures, responsibility, marital status and area of employment (health / administrative) had a significant role. The positive impact of employment on the attitude towards the structure of hospital teams might be due to the attentions of administrative personnel working in teams to establish relationships with other organizations, paying attention to the organization, managing the hospital and their roles in guiding the teams. The role of work experience regarding team attitude towards communication and mutual support could be due to the work experience, having more relationships with others, and having no conflicts.
One of the limitations of this study was the small study sample thus; similar studies with a larger sample size in non-governmental hospitals are recommended.
Some of the benefits of this research included evaluating the attitude of hospital teams using a team tool to improve performance and patient’s safety (Team STEPPS). Conducting this research on hospital committee members adds to the benefits of this study.
5. CONCLUSION
This study reflected positive attitudes regarding health care team members in hospitals. The efficiency of a health care team and its goals can be achieved if there is a presence of effective communication among health care staff and between members of a team and patients as well as strong team leadership and support within an organization. By training hospital personnel and paying particular attention to main elements of effectiveness in a health care team, we can enhance the team culture. Future studies can be conducted on determining the attitude of health care teams and the relationship between team attitude and productivity, job rotation and patient’s safety in Iran.
Acknowledgements:
This research was conducted as a result of a research project No. 92/10/60/41533 in KUMS.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Salas E, Burke CS, Cannon-Bowers JA. Teamwork: emerging principles. International Journal of Management Review. 2000;2:339–356. [Google Scholar]
- 2.Cantu CJ. Evaluating team effectiveness: examination of the team assessment tool: University of North Texas. 2007 [Google Scholar]
- 3.Ohland MW, Loughry ML, Woehr DJ, Bullard LG, Felder RM, Finelli CJ, et al. The Comprehensive Assessment of Team Member Effectiveness: Development of a Behaviorally Anchored Rating Scale for Self-and Peer Evaluation. Academy of Management Learning & Education. 2012;11(4):609–630. [Google Scholar]
- 4.Kaissi A, Johnson T, Kirschbaum M.S. Measuring teamwork and patient safety attitudes of high-risk areas. Nurs. Econ. 2003;21(5):211–218. [PubMed] [Google Scholar]
- 5.Luca J, McMahon M. Developing multidisciplinary teams through self-assessment, supported with online tools. 2006 [Google Scholar]
- 6.Wright MC, Segall N, Hobbs G, Phillips-Bute B, Maynard L, Taekman JM. Standardized assessment for evaluation of team skills: validity and feasibility. Simulation in health care : journal of the Society for Simulation in Healthcare. [Research Support, U.S. Gov’t, P.H.S.] 2013 Oct;8(5):292–303. doi: 10.1097/SIH.0b013e318290a022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morey JC, Simon R, Jay GD, Wears RL, Salisbury M, Dukes KA, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: evaluation results of the MedTeams project. Health services research. 2002;37(6):1553–1581. doi: 10.1111/1475-6773.01104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker DP, Amodeo AM, Krokos KJ, Slonim A, Herrera H. Assessing teamwork attitudes in healthcare: development of the TeamSTEPPS teamwork attitudes questionnaire. Quality and Safety in Health Care. 2010;19(6):e49–e. doi: 10.1136/qshc.2009.036129. [DOI] [PubMed] [Google Scholar]
- 9.Curran VR, Sharpe D, Forristall J. Attitudes of health sciences faculty members towards interprofessional teamwork and education. Medical Education. 2007;41(9):892–896. doi: 10.1111/j.1365-2923.2007.02823.x. [DOI] [PubMed] [Google Scholar]
- 10.Nelson K. Team Assessments: A Review and Analysis of Four Current Team Assessments [Google Scholar]
- 11.Brewer W, Mendelson MI. Methodology and Metrics for Assessing Team Effectiveness*. 2003 [Google Scholar]
- 12.Nancarrow SA, Booth A, Ariss S, Smith T, Enderby P, Roots A. Ten principles of good interdisciplinary team work. Human resources for health. 2013;11(1):19. doi: 10.1186/1478-4491-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor C, Brown K, Lamb B, Harris J, Sevdalis N, Green J. Developing and Testing TEAM (Team Evaluation and Assessment Measure), a Self-assessment Tool to Improve Cancer Multidisciplinary Teamwork. Annals of surgical oncology. 2012;19:4019–4027. doi: 10.1245/s10434-012-2493-1. [DOI] [PubMed] [Google Scholar]
- 14.Clancy CM, Tornberg DN. TeamSTEPPS: assuring optimal teamwork in clinical settings. American Journal of Medical Quality. 2007;22(3):214–217. doi: 10.1177/1062860607300616. [DOI] [PubMed] [Google Scholar]
- 15.Najafi M, Keshmiri F, Najafi M, Shirazi M. Assessment Of Validity And Reliability Of Team STEPPS Teamwork Attitudes Questionnaire (T-TAQ) In Iran. Payavard Salamat. 2014;7(5):389–398. [Google Scholar]
- 16.Flin R, Yule S, McKenzie L, Paterson-Brown S, Maran N. Attitudes to teamwork and safety in the operating theatre. The Surgeon. 2006;4(3):145–151. doi: 10.1016/s1479-666x(06)80084-3. [DOI] [PubMed] [Google Scholar]
- 17.Edmondson, Amy C. Speaking up in the operating room: How team leaders promote learning in interdisciplinary action teams. Journal of management studies. 2003;40(6):1419–1452. [Google Scholar]
- 18.Mercer LM, Tanabe P, Pang PS, Gisondi MA, Courtney DM, Engel KG, et al. Patient perspectives on communication with the medical team: Pilot study using the communication assessment tool-team (CAT-T) Patient education and counseling. 2008;73(2):220–223. doi: 10.1016/j.pec.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Kilner E, Sheppard LA. The role of teamwork and communication in the emergency department: a systematic review. International emergency nursing. 2010;18(3):127–137. doi: 10.1016/j.ienj.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Christian CK, et al. A prospective study of patient safety in the operating room. Surgery. 2006;139(2):159–173. doi: 10.1016/j.surg.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 21.Campion MA, Papper EM, Medsker GJ. Relations between work team characteristics and effectiveness: A replication and extension. Personnel psychology. 1996;49(2):429–452. [Google Scholar]
- 22.Friedlander F. The Design of Work Teams. Handbook of Organizational Behavior. 1987 [Google Scholar]
- 23.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Quality and Safety in Health Care. 2004;13(Suppl 1):i85–i90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loughry Misty L, Matthew W. Ohland, DeWayne Moore D. Development of a theory-based assessment of team member effectiveness. Educational and Psychological Measurement. 2007;67(3):505–524. [Google Scholar]
- 25.Deering S, Johnston LC, Colacchio K. Multidisciplinary teamwork and communication training. Seminars in perinatology. Elsevier. 2011 doi: 10.1053/j.semperi.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 26.Liebman Carol B, Chris Stern Hyman. A mediation skills model to manage disclosure of errors and adverse events to patients. Health Affairs. 2004;23(4):22–32. doi: 10.1377/hlthaff.23.4.22. [DOI] [PubMed] [Google Scholar]
- 27.Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Critical care medicine. 2003;31(3):956–959. doi: 10.1097/01.CCM.0000056183.89175.76. [DOI] [PubMed] [Google Scholar]


