Abstract
Background
Recent research highlights the potential value of differentiating between categories of physical activity intensities as predictors of health and well-being. This study sought to assess reliability and concurrent validity of sedentary (ie, 1 METs), low-light (ie, > 1 and ≤2 METs; eg, playing cards), high-light (ie, >2 and <3 METs; eg, light walking), moderate-to-vigorous physical activity (MVPA, ≥3 METs), and “total activity” (≥2 METs) from the CHAMPS survey. Further, this study explored over-reporting and double-reporting.
Methods
CHAMPS data were gathered from the Seniors Neighborhood Quality of Life Study, an observational study of adults aged 65+ years conducted in 2 US regions.
Results
Participants (N = 870) were 75.3 ± 6.8 years old, with 56% women and 71% white. The CHAMPS sedentary, low-light, high-light, total activity, and MVPA variables had acceptable test-retest reliability (ICCs 0.56–0.70). The CHAMPS high-light (ρ = 0.27), total activity (ρ = 0.34), and MVPA (ρ = 0.37) duration scales were moderately associated with accelerometry minutes of corresponding intensity, and the sedentary scale (ρ = 0.12) had a lower, but significant correlation. Results suggested that several CHAMPS items may be susceptible to over-reporting (eg, walking, housework).
Conclusions
CHAMPS items effectively measured high-light, total activity, and MVPA in seniors, but further refinement is needed for sedentary and low-light activity.
Keywords: exercise, sedentary behavior, measurement, seniors, questionnaire
Recent evidence indicates that light physical activity (defined as >1 and <3 METs),1 as assessed by accelerometry, may have beneficial health benefits, independent of moderate-to-vigorous intensity physical activity.2 Further, sedentary behaviors (eg, watching television) predict deleterious health outcomes such as obesity and type II diabetes, independent of moderate-to-vigorous intensity physical activity.3–6 Results from a recent accelerometry-based study indicated that activity across the intensity spectrum, including sedentary, light, and moderate-to-vigorous activity, are important independent contributors to physical health among midlife and older adults.7 Further, activity on the higher end of the light intensity category was associated with improved psychosocial well-being, even after adjusting for moderate-to-vigorous intensity activity.7 These results suggest that physical activity self report measures would be of greater utility for intervention and epidemiologic studies if they successfully differentiated between varying levels of activity from sedentary in vigorous.
The Community Health Activities Model Program for Seniors physical activity self-report questionnaire (CHAMPS) was originally designed to assess “… the types and intensity levels of physical activity that are meaningful and appropriate for older adults, including lighter (eg, leisurely walking, water exercises, stretching) as well as more vigorous activities”8 (p. 1127). Assessment of lighter intensity activities was calculated within a “total activity” score. As highlighted above though, “high-light” activity may have a positive impact on health and well-being, even after controlling for moderate-vigorous intensity activity. As such, an exploration of a rescoring of the CHAMPS into different physical activity intensity categories with the inclusion of a separate, “high-light” scale could make the measure more valuable for use in epidemiologic and intervention studies. Indeed, lighter intensity physical activity interventions may be a particularly promising focus for future intervention research among older adults as lighter intensity physical activity is easier to engage in for older adults.9,10 The CHAMPS also includes a group of items related to sedentary behaviors (eg, sit and talk with friends) that were included to reduce over-reporting of moderate-to-vigorous intensity activity, a tactic that later received empirical support.11 To our knowledge, these CHAMPS items have not been used for assessment of sedentary behavior, although they potentially could be if demonstrated to have sufficient reliability and validity.
Self-report physical activity measures are coming under increased serutiny.12 Self-report measures have many psychometric problems including response bias issues such as over-reporting or double-reporting13 as well as socially desirable responses.14 Indeed, self-report physical activity measures have been shown to be poor at estimating absolute levels of physical activity.15,16 Despite these limitations, self-report physical activity measures are still valuable because they can assess specific behaviors (eg, walking to run errands vs. walking for exercise) whereas accelerometry and other objective measures such as doubly-labeled water cannot. Self-report measures are still valuable for epidemiologic studies in which distribution of an accelerometer to all research participants is impractical. The current physical activity guidelines are based largely on self-reported estimates of physical activity.10 Additional research is still needed to refine self-report physical activity measures with a particular focus on their utility relative to accelerometry.
The primary aim of the current study was to examine the 6-monih test-retest reliability and validity of the CHAMPS sedentary and light activity categories. The second aim was to explore psychometric issues of the CHAMPS with a particular focus on double reporting and over-reporting.
Methods
Procedures
The Senior Neighborhood Quality of Life Study (SNQLS) was an epidemiological study designed to examine the relationship of neighborhood “walkability” characteristics to physical activity and other outcomes in adults 66 years of age and older. Study methods have been described previously.17 In brief, the study was conducted in 2 U.S. metropolitan areas (Seattle/King County, WA region and the Baltimore, MD/Washington DC area), and participants were recruited from neighborhoods representing wide variability in neighborhood walkability and income.7,18 The study used a 2 x 2 design with a) neighborhood “walkability” based on geographic information systems data related to street connectivity and land-use mix (dichotomized into high walkable and low walkable), and b) neighborhood income (dichotomized into high income and low income).19 The primary purpose of the study was to examine if neighborhood “walkability” and income were associated with physical activity of older adults. The protocol was approved by the institutional review boards for the investigators’ home institutions.
Participants were recruited via mail, followed up with telephone contact, using contact information obtained from a commercial marketing company. Interested participants completed an informed consent statement and were then mailed an accelerometer and survey packet. Participants were instructed to wear the accelerometer for 7 consecutive days, complete the survey after wearing the accelerometer, and mail back the accelerometer and survey packet to research staff. Six months later the accelerometer and a second survey were mailed to participants with similar instructions. Participants were recruited and enrolled year-round from 2005 through 2007. This 2-phase data collection strategy reduced participant burden, provided 2 7-day periods of self-report and objective physical activity assessment, and controlled for seasonality effects. Upon completion of each assessment, participants were given $25.
Participants
Of the 3911 eligible contacts, 25% provided written informed consent and agreed to have a survey and accelerometer mailed to them. Of those who completed the informed consent, 92% returned the survey and wore the accelerometer during the first time-point, resulting in a total sample of 896 participants for the first time point (Time1). To answer the validity questions of interest, the analysis sample was limited to only those with complete data on the CHAMPS at Time1. This resulted in a final sample of 870. Table 1 describes this sample in more detail. Participants were contacted by mail 6 months later to complete a second survey and wear an accelerometer for the second time point (Time2). Eighty-six percent of the original sample mailed back the survey and wore the accelerometer at Time2, resulting in a final sample of 748 with completed assessments at both time points. These individuals were included in the test-retest reliability analyses.
Table 1.
Demographic Characteristics (N = 870)
| 66–69 yr
|
70–79
|
80+yr
|
||||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| N | 109 | 109 | 179 | 238 | 89 | 146 |
| Race | ||||||
| White/Caucasian (%) | 70.6 | 59.3 | 69.1 | 65.1 | 88.8 | 80.8 |
| Black/African-American (%) | 20.2 | 30.0 | 18.0 | 27.7 | 4.5 | 16.4 |
| Other (%) | 9.2 | 11.1 | 12.9 | 7.1 | 6.7 | 2.7 |
| Education | ||||||
| <HS diploma (%) | 5.6 | 7.3 | 7.3 | 8.0 | 4.5 | 6.1 |
| HS diploma/equiv. (%) | 13.9 | 17.4 | 10.6 | 19.7 | 10.1 | 19.2 |
| College-level (%) | 51.9 | 61.5 | 54.7 | 54.6 | 55.1 | 57.5 |
| Graduate-level (%) | 28.7 | 13.8 | 27.4 | 17.6 | 30.3 | 17.1 |
| Income | ||||||
| <$30k(%) | 15.6 | 39.5 | 24.0 | 43.3 | 24.7 | 48.6 |
| $30k–$59k (%) | 32.1 | 24.8 | 31.8 | 26.9 | 34.8 | 28.8 |
| $60k–$99k (%) | 28.4 | 21.1 | 25.7 | 15.1 | 21.4 | 13.7 |
| >$100k (%) | 17.4 | 4.6 | 12.9 | 3.4 | 9.0 | 2.7 |
| Overweight | 56.0 | 39.8 | 51.4 | 29.4 | 34.8 | 31.5 |
| Obese | 19.2 | 23.1 | 16.2 | 25.2 | 13.5 | 13.0 |
| Independent-living (%) | 94.5 | 82.6 | 92.7 | 85.3 | 69.7 | 58.9 |
| Site | ||||||
| Seattle (%) | 50.5 | 37.6 | 52.5 | 45.4 | 68.5 | 61.0 |
| Baltimore (%) | 49.5 | 62.4 | 47.5 | 54.6 | 31.5 | 39.0 |
Note. Overweight = BMI 25.0–29.9; Obese = BMI ≥ 30.
Measures
Demographic information was ascertained via self-report. This included age, gender, race/ethnicity, years of education, income, and height and body weight to calculate BMI (kg/m2). Adult self-report of weight and height are correlated strongly with objectively measured values.20
CHAMPS
The original CHAMPS includes 41 items related to a variety of activities in which midlife and older adults tend to engage. In the SNQLS,8 11 items, mostly related to transportation, were added to the CHAMPS and 1 item was deleted (new and deleted items are identified in the Online Appendix). Three original CHAMPS items that were not included in the original scoring but were at the beginning of the survey concerning general activity and flights of stairs climbed per day were dropped in the interest of parsimony. The CHAMPS used in SNQLS asks participants to think about the past 4 weeks and report on the frequency and total amount of time, on average per week, participants engaged in each activity. Those participants who reported engaging in the activity were asked to select 1 of 6 categories reflecting the amount of time on average they engaged in the activity, ranging from less than 1 hour per week to 9 or more hours per week. The midpoint of each category’s range was used to provide an estimate of activity time for each item (eg, 1 to 2.5 hours = 105 minutes per week). The original CHAMPS scoring includes algorithms to calculate total caloric energy expenditure per week based on “all” activities that would likely impact health (henceforth referred to as “total meaningful activities”), caloric energy expenditure per week based on moderate-to-vigorous intensity activity (ie, physical activity of greater than or equal to 3 METs), frequency per week of engagement in total meaningful activities (minutes/week), and frequency per week of engagement in moderate-to-vigorous intensity physical activities (minutes/week). For this study, we added algorithms to calculate sedentary and light activities. Although we calculated all of the original CHAMPS scores, we were interested primarily in the average frequency per week (ie, minutes/week) participants reported engaging in each physical activity intensity level (ie, sedentary, light, moderate-to-vigorous), as this was most readily comparable to the coding of the accelerometry data within SNQLS, and similar, datasets.21
All CHAMPS items were assigned a MET value based on Stewart et al8 and the 2000 Compendium of physical activities.1 As in the original Stewart et al paper,8 MET values were lowered for some CHAMPS items (18 based on the current techniques) based on likely reduced exertion among adults over 65 years old for these activities relative to the general adult population (see Online Appendix for a full rationale of MET changes for each item).8 In addition, 4 items received different MET values from the original Stewart et al values based on activity intensity classifications from the 2000 Compendium. Finally, 13 sedentary and light intensity items that were not originally assigned a MET value and 10 new items were assigned a MET value. See Online Appendix for more details on each CHAMPS item.
Based on previous work with accelerometry with older adults7 and to provide additional discrimination across the range of light intensity activities, CHAMPS items were categorized into 2 light intensity levels: low-light (METs>1 and ≤2) and high-light (METs>2 and <3). The rationale is that midlife and older adults generally spend a substantial proportion of their time in a range of light activities, and a relatively small amount of time in moderate-to-vigorous activities.9,10 MET value ranges for each category were based principally on the 2000 Compendium, in which behaviors were categorized into sedentary (MET = 1), general light (METs >1 and <3), moderate (METs ≥3 and ≤6) and vigorous (METs >6).
Accelerometry
Participants also wore an Actigraph accelerometer for 7 days that was included with each questionnaire packet mailing (mailed 6 months apart). Participants were asked to wear the accelerometer during waking hours. A follow-up phone call was scheduled with the participants for the day after they received the accelerometer to review the key points of the written instructions and to answer any questions. In addition, research personnel contacted participants at least 1 other time by phone during the week to answer any questions that may have arisen. Participants were also provided a toll-free number to use if any other questions arose during the week that they wore the accelerometer. Participants were asked to wear the accelerometer before filling out the questionnaires; therefore, the 1-week accelerometry data collection occurred during the 4-week time-span being captured by the CHAMPS.
The Actigraph (Actigraph, Manufacturing Technology Incorporated, model 7164 and 71256, Fort Walton, FL) is a small, electronic, uni-axial device that is worn on the waist and measures activity counts (epoch set at 1 minute for this study). It has been extensively validated in a variety of populations, including older adults.22,23 Data compliance and cleaning procedures were consistent with other large-scale cross-sectional accelerometer studies,9,18 such that a) valid hours of data consisted of no more than 45 consecutive ‘zero’ values (interpreted as nonwear time), b) a valid day was defined as at least 8 valid h/day, and c) participants with less than 5 valid days (using a 30 consecutive ‘zero’ and 10 valid h/day rule) or less than 66 valid hours across 7 days were asked to rewear the accelerometer.
To date there are no widely accepted accelerometer “cut points” to differentiate activity intensity levels specifically for older adults.24 Minutes of moderate-vigorous (>1952 counts/min) and sedentary (≤100 counts/min) activities were calculated based on published cut-points for adults.25,26 A further refinement of light-intensity activities was established based on previous research indicating that high-light activity was more strongly associated with physical health and psychosocial well-being compared with low-light activity.7 As with the previous study, the distinction between “low-light” physical activity and “high-light” physical activity was based on Copeland et al,27 which identified an activity count cut-point that was approximately 1000 counts (ie, 1041 counts/min) for predicting meaningful amounts of physical activity among older adults. Activity minutes that were above sedentary but below the Copeland value (ie, > 100 and <1041 counts/min) were identified as low-light activity. Activity minutes that were equal to or above the Copeland value but below the traditional adult value of 1952 (ie, ≥1041 and <1952 counts/min) were identified as high-light activity. As the CHAMPS includes scoring algorithms for total meaningful physical activity, an aggregate score of values above the Copeland cut point (ie, ≥1041) was also calculated for concurrent validation of the total meaningful activity CHAMPS variable. This accelerometry value roughly corresponds with all of the activity classified as either high-light or moderate-to-vigorous intensity activity and is referred to subsequently as high-light/moderate-to-vigorous intensity activity.
Statistical Analyses
All analyses were completed using SAS Enterprise Guide 4.1 (SAS Institute Inc., Cary, NC, USA). Summary statistics were calculated for all variables of interest, with means and standard deviations reported for continuous variables and percentages reported for categorical variables.
Test-retest reliability of the CHAMPS was assessed by calculating the 1-way single-measure intraclass correlation (ICC) between study Time1 and Time2. The ICC is a better indicator of stability over time than Pearson product-moment correlations as it measures both the percent of variance explained by each individual and the mean differences over time.
To assess the validity of the CHAMPS, scales from the CHAMPS and accelerometry were compared using Spearman rank-order correlations because of nonnormal distributions for the majority of the CHAMPS and accelerometry variables. To explore possible over-reporting on the CHAMPS, Bland-Altman Plots comparing accelerometry and CHAMPS were used.28 A Bland-Altman plot displays the difference between 2 scales on the same metric (eg, min/wk for this study) compared with the average value of the 2 scales. Accelerometry has been shown to under-represent total energy expenditure,29 which is partially attributable to misclassification of low impact moderate-to-vigorous intensity activities (eg, bicycling) as sedentary or light activity.30 As neither the CHAMPS nor the accelerometer are “gold standards” for sedentary and light intensity activity, these plots are best interpreted as giving evidence for concurrent rather than criterion validity.
The highest response option for the CHAMPS is 9 or more hours per week. This may limit the CHAMPS in assessing sedentary and low-light activities that often are engaged in for more than 9 hours per week (eg, television viewing). Based on this, the percent of participants who reported the highest possible option for the CHAMPS was reported as an indicator of the number of participants within the current sample who chose that category for sedentary and low-light activity.
To examine possible double reporting, CHAMPS items that appeared susceptible to potential double reporting (eg, walking fast/briskly versus walking up hill; heavy housework versus light housework) were paired, resulting in 10 item-pairs (see Table 3). Data were coded to reflect different response options (see Table 3). We were primarily interested in the number of participants who reported engagement in 2 similar activities for both the same category of minutes and an equal number of times per week. Although not an ideal indicator of double-reporting, we hypothesized this could be indicative of potential double reporting. T-tests comparing participants who may have double-reported based on our coding to those who did not double report on accelerometry-based physical activity was done to test the validity of the double-reporting algorithms.
Table 3.
CHAMPS Item Responses
| Sedentarya (MET = 1) | Mean± | SD | % contribution to sedentary | % never doing activity | % report 9+ hours/wk |
|---|---|---|---|---|---|
| Total sedentary behavior | 1095.7± | 486.4 | |||
| Watch television | 382.1± | 190.6 | 34.9 | 1.8 | 37.2 |
| Read | 333.7± | 204.3 | 30.5 | 2.8 | 28.9 |
| Sit and talk with friends | 193.2± | 169.1 | 17.6 | 12.5 | 7.6 |
| Attend an event | 78.2± | 112.5 | 7.1 | 54.5 | 0.8 |
| Ride in a car | 65.6± | 96.9 | 6.0 | 44.7 | 0.5 |
| Travel by bus | 22.5± | 73.3 | 2.1 | 84.5 | 0.6 |
| Travel by subway or train | 15.7± | 52.2 | 1.4 | 86.4 | 0.1 |
| Use a dial a ride service | 4.66± | 27.2 | 0.4 | 95.5 | 0.0 |
| Low-lightb (MET >1 AND ≤2) | Mean± | SD | % contribution to low-light | % never doing activity | % report 9+ hours/wk |
|---|---|---|---|---|---|
| Total low-light activity | 1090.5± | 567.4 | |||
| Drive in a car | 200.9± | 176.4 | 18.4 | 17.7 | 8.9 |
| Visit with family and friends | 196.7± | 160.9 | 18.0 | 10.1 | 7.5 |
| Use a computer | 188.8± | 216.1 | 17.3 | 40.1 | 14.4 |
| Talk on the phone | 164.4± | 158.1 | 15.1 | 2.5 | 6.8 |
| Attend church | 86.7± | 110.1 | 8.0 | 45.3 | 0.7 |
| Do arts and crafts | 74.6± | 150.0 | 6.8 | 67.6 | 4.7 |
| Play cards or board game | 64.4± | 128.4 | 5.9 | 71.7 | 2.3 |
| Attend club meetings | 62.5± | 97.9 | 5.7 | 59.0 | 0.5 |
| Go to the senior center | 38.0± | 101.9 | 3.5 | 78.3 | 1.4 |
| Play a musical instrument | 13.5± | 59.9 | 1.2 | 91.2 | 0.3 |
| High-lightc (MET >2 and <3) | Mean± | SD | % contribution to high-light | % never doing activity | % report 9+ hours/wk |
|---|---|---|---|---|---|
| Total high-light activity | 548.2± | 381.7 | |||
| Do light work around the house | 132.9± | 132.2 | 24.2 | 15.8 | 2.9 |
| Walk leisurely | 111.0± | 134.8 | 20.3 | 28.6 | 2.5 |
| Do volunteer work | 82.3± | 142.5 | 15.0 | 63.5 | 3.0 |
| Do light gardening | 61.0± | 93.9 | 11.1 | 37.5 | 0.9 |
| Do stretching or flexibility | 49.9± | 78.3 | 9.1 | 48.6 | 0.2 |
| Walk to do errands | 43.4± | 84.8 | 7.9 | 58.6 | 0.7 |
| General conditioning exercises | 23.6± | 57.2 | 4.3 | 73.7 | 0.1 |
| Walk your dog | 20.9± | 87.9 | 3.8 | 90.7 | 1.4 |
| Play golf, riding in a cart | 10.9± | 65.0 | 2.0 | 95.8 | 0.8 |
| Do yoga or tai-chi | 8.2± | 37.6 | 1.5 | 92.9 | 0.1 |
| Shoot pool or billiards | 4.0± | 29.8 | 0.7 | 96.9 | 0.1 |
| Moderate-to-vigorousd (MET ≥ 3) | Mean± | SD | % contribution to moderate-to-vigorous | % never doing activity | % report 9+ hours/wk |
|---|---|---|---|---|---|
| Total moderate-to-vigorous activity | 309.0± | 327.3 | |||
| Do heavy gardening | 56.7± | 113.1 | 18.0 | 66.9 | 1.2 |
| Walk fast or briskly for exercise | 56.6± | 117.6 | 17.9 | 66.4 | 2.0 |
| Do heavy work around the house | 50.3± | 107.0 | 15.9 | 67.8 | 1.7 |
| Walk uphill or hike uphill | 24.2± | 58.8 | 7.7 | 71.4 | 0.1 |
| Do light strength training | 18.6± | 48.4 | 5.9 | 76.2 | 0.1 |
| Ride a bicycle | 16.8± | 49.0 | 5.3 | 80.9 | 0.1 |
| Moderate/heavy strength training | 14.7± | 46.1 | 4.7 | 83.7 | 0.1 |
| Moderate-to-vigorousd (MET ≥ 3) | Mean± | SD | % contribution to sedentary | % never doing activity | % report 9+ hours/wk |
|---|---|---|---|---|---|
| Aerobic machine w/arms & legs | 13.2± | 45.2 | 4.2 | 86.3 | 0.1 |
| Golf, carrying/pulling equipment | 8.8± | 54.8 | 2.8 | 96.6 | 0.3 |
| Dance | 8.0± | 41.1 | 2.5 | 93.5 | 0.1 |
| Do stair or step machine | 7.5± | 30.5 | 2.4 | 90.1 | 0.0 |
| Do water exercises | 7.2± | 35.1 | 2.3 | 93.8 | 0.0 |
| Do aerobics or aerobic dancing | 7.1± | 32.5 | 1.2 | 93.5 | 0.0 |
| Swim gently | 5.9± | 36.3 | 1.9 | 95.5 | 0.1 |
| Play doubles tennis | 3.7± | 30.8 | 1.2 | 98.3 | 0.5 |
| Swim moderately or fast | 3.4± | 26.2 | 1.1 | 97.7 | 0.2 |
| Jog or run | 2.6± | 20.5 | 0.8 | 97.0 | 0.0 |
| Bicycle to do errands | 2.3± | 24.3 | 0.8 | 97.8 | 0.0 |
| Basketball, soccer, or racquetball | 0.9± | 12.4 | 0.8 | 99.4 | 0.0 |
| Play singles tennis | 0.5± | 6.4 | 0.8 | 99.3 | 0.0 |
| Skate (ice, roller, in-line) | 0.1± | 3.6 | 0.8 | 99.9 | 0.0 |
Note. Item listings above do not include the full wording for each item. For the full wording, please see the Online Appendix.
Test-Retest Rel: ICC = 0.56;
Test-Retest Rel ICC = 0.70;
Test-Retest Rel: ICC = 0.68;
Test-Retest Rel: ICC = 0.66.
Results
Table 1 reports basic demographics of the sample. Test-retest reliability estimates of the CHAMPS indicated acceptable 6-month stability for the low-light (ICC = 0.70), high-light (ICC = 0.68), moderate-to-vigorous duration (ICC = 0.66), total meaningful activity duration (ICC = 0.69), moderate-to-vigorous physical activity caloric expenditure (ICC = 0.61), and total meaningful activity caloric expenditure (ICC = 0.64) variables and somewhat lower 6-month stability for the sedentary variable (ICC =0.56).
Table 2 reports Spearman rank-order correlations between CHAMPS and accelerometer variables. Results indicated the strongest correlation between the CHAMPS moderate-to-vigorous caloric expenditure (ρ = 0.40, P < .001) followed closely by the CHAMPS total meaningful activity caloric expenditure (ρ = 0.39, P < .001), moderate-to-vigorous intensity duration (ρ = 0.39, P < .001), and total meaningful activity duration (ρ = 0.38, P < .001) variables when correlated with the accelerometry-based high-light/moderate-to-vigorous intensity activity variable. A moderate and significant correlation between the CHAMPS and accelerometer moderate-to-vigorous variables (ρ = 0.37, P < .0001) was observed, consistent with previous research.23 The CHAMPS and accelerometry high-light variables had a moderate but slightly weaker correlation (ρ = 0.27, P < .0001). Correlation between the CHAMPS and accelerometer values for sedentary was significant but low (ρ = 0.12, P < .001). Finally, there was no significant correlation between the CHAMPS low-light variable and the accelerometry-derived low-light variable (ρ = 0.06, P = .10).
Table 2.
CHAMPS Accelerometer Spearman-Rank Order Correlation Matrix
| Accelerometer
|
|||||||
|---|---|---|---|---|---|---|---|
| Sedentary | Low-light | High-light | MVPA | Hi-Li/MVPA | |||
| CHAMPS | Duration | Sedentary | 0.12*** | −0.09** | −0.02 | −0.00 | −0.00 |
| Low-Light | −0.08* | 0.06 | 0.15**** | 0.13*** | 0.14**** | ||
| High-Light | −0.10** | 0.15**** | 0.27**** | 0.22**** | 0.27**** | ||
| MVPA | −0.10** | 0.20**** | 0.35**** | 0.37**** | 0.39**** | ||
| “Total Activity” | −0.12*** | 0.20**** | 0.35**** | 0.34**** | 0.38**** | ||
| Cal. exp/wk | MVPA | −0.08* | 0.17**** | 0.35**** | 0.38**** | 0.40**** | |
| “Total Activity” | −0.11*** | 0.15**** | 0.36**** | 0.36**** | 0.39**** | ||
Note. Results are from a subsample (n = 850) of the full sample (n = 870) who had complete CHAMPS and accelerometer data. “Total Activity” refers to all activities within the high-light, moderate, or vigorous intensity range. The shading in this table indicates 2 values that should conceptually be identical. For example, a shading would be put for sedentary behavior measured both by CHAMPS and accelerometry.
Abbreviations: MVPA, Moderate-to-vigorous Intensity Physical Activity. Hi-Li/MVPA, high-light, moderate-, and vigorous-intensity physical activity; Cal. exp/wk. Caloric expenditure per week.
P<.05,
P<.01,
P<.001,
P<.0001.
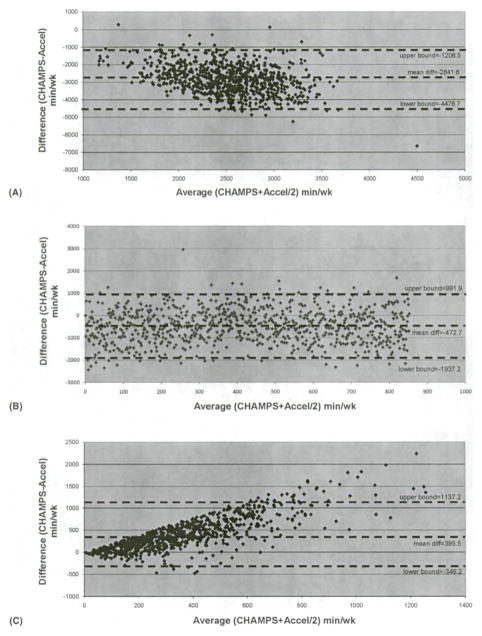
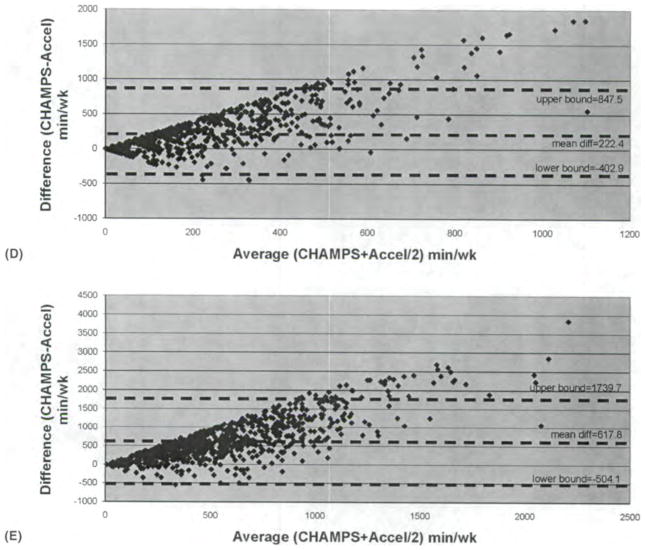
Figure 1 shows Bland-Altman Plots comparing the CHAMPS and accelerometry. The Bland-Altman Plots showed wide differences in estimates between accelerometry and CHAMPS activity time on all variables. In particular, the CHAMPS indicated fewer minutes/week of sedentary (Mdiff=−2841.6 min/wk; 95% CI = −4476.7 to −1206.5 min/wk) and low-light activity (Mdiff= −472.7 min/wk; 95th CI = −1937.2 to 991.9 min/wk) and more minutes of high-light (Mdiff = 395.5 min/wk; 95% CI = −346.2 to 1137.2 min/wk), moderate-to-vigorous (Mdiff = 222.4 min/wk; 95% CI = −402.9 to 847.5 min/wk), and total activity (Mdiff= 617.8 min/wk; 95% CI = −504.1 to 1739.7min/wk) activity relative to accelerometry.
Figure 1.
Bland Altman plots: A) Sedentary behavior: B) Low-light activity: C) High-light activity. Bland Altman plots: D) Moderate-to-vigorous activity; E) Total meaningful activity (ie, high-light and moderate-to-vigorous activity).
Examination of the plots suggests that the discrepancy between CHAMPS and accelerometry on the moderate-to-vigorous (Panel D), high-light activity (Panel C), and total activity (Panel E) variables was more pronounced among persons who reported being the most active (in the direction of over-reporting on the CHAMPS). No noticeable discrepancy between the 2 assessment modes was observed between measures by activity level for low-light activity (Panel B). Further, the discrepancy between the CHAMPS sedentary items relative to accelerometry (Panel A) appeared to be more pronounced as participants reported being more sedentary (in the direction of underreporting on CHAMPS).
Table 3 reports descriptive statistics on individual items of the CHAMPS. The highest possible response option on the CHAMPS (ie, 9 or more hours) was reported for 37.2% of participants on the watching television item, and 28.9% of participants on the reading item. Over half (51.8%) of participants responded with 9 or more hours on at least 1 sedentary item. The percent of participants responding with the highest possible response on at least 1 item within an intensity category diminished as intensity increased, with 35.5% for low-light, 10.2% for high-light, and 4.9% for moderate-to-vigorous activity.
Table 4 reports frequencies and percentages of responses for sets of CHAMPS items suspected of being vulnerable to double reporting (eg, walking fast versus walking leisurely). When looking at individuals who responded affirmatively to at least 1 activity, some individuals reported the same category of minutes per week and the same number of times per week for 2 similar activities across several of the item sets, including golfing with a cart versus golfing while carrying clubs (13.2% reported the 2 items similarly), walking fast versus walking leisurely (8.6%), heavy versus light gardening (8.2%), heavy versus light house work (6.1%), walking leisurely versus walking for errands (5.4%), and aerobic machines versus stair machines (5.4%).
Table 4.
Comparison of Responses to CHAMPS Items Suspected of Double-Reporting
| CHAMPS items compared | Full sample
|
Only participants that responded affirmatively to at least 1 of the 2 items in the pair
|
||
|---|---|---|---|---|
| Equal min, unequal # times/wk | Equal min, equal # times/wk | Equal min, unequal # times/wk | Equal min, equal # times/wk | |
| Talk vs visit with friends | 22.3 | 1.5 | 22.4 | 1.5 |
| Talk vs play a game | 6.2 | 0.2 | 6.4 | 0.2 |
| Walk fast vs walk leisurely | 4.7 | 6.8 | 6.0 | 8.6 |
| Walk fast vs walking uphill | 0.0 | 0.0 | 0.0 | 0.0 |
| Walk leisurely vs errand walking | 9.2 | 4.3 | 11.7 | 5.4 |
| Golf w/cart vs golf carry clubs | 0.1 | 0.8 | 1.9 | 13.2 |
| Aerobic mach, vs stair machine | 0.5 | 1.2 | 2.2 | 5.4 |
| Aerobic machine vs aerobics | 0.5 | 0.8 | 2.6 | 4.5 |
| Heavy vs light gardening | 6.4 | 5.4 | 9.8 | 8.2 |
| Heavy vs light housework | 6.3 | 5.2 | 7.4 | 6.1 |
Note. All above values are percents of the given sample (ie, either the full sample or only a subsample of participants that responded affirmatively to at least 1 of the 2 items in the item-pair).
Aggregation of these data revealed that 21.3% of participants reported the same category of minutes per week and the same number of times per week on at least 1 item-pair. Individuals who may have double-reported also had significantly more minutes of moderate-vigorous activity based on accelerometery compared with those individuals that did not double-report on any items [t(848) = −2.45, MDR = 105.0 ± 132.4 vs. MNotDR = 82.1 ± 105.1]. Further, younger participants (ie, those between the ages of 66 and 69 years) were more likely to respond similarly to related items compared with older participants (ie, 30.3% of 66–69 year olds reported similar values on 1 or more items relative to 19.7% of 70–79 year olds and 15.7% of 80+ year olds, χ2 = 15.5, P < .001). In addition, men were more likely to report similar values than women (ie, 27.1% and 16.8% reported similarly on 1 or more item pairs, respectively, χ2 = 13.3, P< .001). No significant differences in the tendency toward similar reporting were found based on education (P = .89) or race/ethnicity (P = .07).
Discussion
The main contribution of the current study was to develop and evaluate new measures of sedentary behavior and light intensity activity from the CHAMPS survey that are tailored for older adults. Results generally indicated acceptable reliability for the CHAMPS sedentary, low-light, high-light, moderate-to-vigorous, and total meaningful activity scales. Comparisons with accelerometer data indicated acceptable concurrent validity for the previously validated moderate-to-vigorous scales and total meaningful activity scales that were similar to previous studies.31 Results suggested that the new high-light duration scale was significantly correlated with accelerometry, albeit with a slightly weaker correlation. There was poor concurrent validity for sedentary and low-light scales.
These results suggest that the CHAMPS moderate-to-vigorous duration and caloric expenditure, total meaningful activity duration and caloric expenditure, and high-light variables are all reliable and valid methods for scoring the CHAMPS. The addition of the “high-light” scoring method to the CHAMPS could prove useful for future epidemiologic studies and intervention trials among older adults. As indicated by previous research, high-light intensity activity appears to have positive health benefits on physical health and psychosocial well-being after controlling for moderate-intensity physical activity and sedentary behaviors.7 This finding suggests that interventions among older adults may not need to promote moderate-to-vigorous intensity activity but instead could gain similar health benefits by targeting only high-light intensity activity. This might be a particularly fruitful area for intervention research among older adults as this group already spends a significant portion of time in light intensity activity and thus an intervention to promote increased high-light activity may be easier for older adults to adopt and maintain.
The weak concurrent validity results for the sedentary and low-light measures may be at least partially attributable to the ceiling effect observed for several sedentary and low-light activities (eg, respondents could not report doing television viewing, reading, or driving for more than 9 hours per week due to the formatting of the CHAMPS). Approximately half of participants reported the highest possible response option on at least 1 sedentary item and one-third of participants reported the highest possible response option for low-light activities.
Bland-Altman plots showed that participants tended to report more moderate-to-vigorous and high-light activity and less low-light and sedentary activity than that measured by accelerometry. These results are consistent with other studies suggesting self-report measures may misrepresent absolute levels of activity,15 including over-reporting of moderate activity compared with accelerometry.16 One explanation for the absolute differences in sedentary minutes between the CHAMPS and accelerometry measures is that the CHAMPS under-represents the activities individuals do while sedentary. As the CHAMPS was not originally intended to assess sedentary behavior systematically, more items may need to be added to the measure to fully assess sedentary behavior (eg, relaxing, or listening to music). More importantly, the observed ceiling effects observed within the sedentary scale should be addressed. Potential improvements would be to expand the response options to include higher values or rewriting the CHAMPS with an open-ended response option, as is currently available for other physical activity self-reports (eg, the Seven-day Physical Activity Recall,32 International Physical Activity Questionnaire33).
To examine the potential impact of using an open-ended response option instead of the categorical option, we completed a small pilot study with 14 community-dwelling adults ages 50 years and older (mean age = 63.4 ± 7.4). Participants completed 2 versions of the CHAMPS on 2 consecutive days with the order of administration randomized. One version was the traditional CHAMPS using the categorical response option and the other version asked participants to state “how many hours per week” they participated in an activity (eg, walking fast/briskly) with an open-ended response option. Participants reported significantly more sedentary and low-light activity on the open-ended version compared with the categorical version (Sedentary: Open-ended = 2413.1 ± 1501.1 min/wk vs. Categorical = 1393.9 ± 328.4 min/wk. Low-light: Open-ended = 2683.2 ± 1577.7 min/wk vs. Categorical = 1714.3 ± 497.5 min/wk). Although it did not reach statistical significance in this small pilot, the open-ended response option produced lower reports of moderate-to-vigorous activity (Open-ended = 427.8 ± 334.6 min/wk vs. Categorical = 548.6 ± 436.9 min/wk).
Pilot study results, coupled with results from the larger investigation indicating the CHAMPS may underestimate sedentary and low-light activity and overestimate moderate-to-vigorous activity relative to accelerometry, suggest that changing the CHAMPS to an open-ended response option may make the CHAMPS more useful in assessing absolute levels of activity. As this specific recommendation is based on a small pilot study, additional empirical validation and reliability testing using a larger, more diverse sample is required before any conclusions can be drawn. Some groups of older adults may find it difficult to fill out the open-ended option, although no differences in perceived difficulty or the amount of time to complete the survey were found in the pilot study.
Another explanation for the apparent overestimation of moderate-to-vigorous intensity activity and underestimation of sedentary behavior is that self-report measures are poor indicators of absolute levels of physical activity.15,16 Indeed, results from the Bland-Altman plots suggest that the CHAMPS is poor at estimating absolute levels of physical activity at all intensities, assuming that accelerometry is a better indicator of absolute physical activity. Therefore, the CHAMPS should likely not be used to estimate absolute levels of physical activity. Previous research on the CHAMPS, however, indicates that the CHAMPS does consistently correlate with other measures of physical activity including a Mini-Logger 2000 (a device that measures both activity and heart rate),31 V02-max,34 fitness tests (eg, chair stands, 6-min walk),31,35,36 accelerometer,23 other self-reported physical activity measures,31,37 and self-reported health measures.31,38 In addition, the CHAMPS has been used successfully within clinical trials and thus is sensitive to small but meaningful changes.8,39,40 Taken together with the present findings, these results suggest that, although the CHAMPS should likely not be used as an absolute indicator of physical activity, it does function well as an indicator of relative physical activity.
Both gardening and household activities were commonly reported in this cohort, and other studies suggested these kinds of routine or instrumental forms of activity are subject to over-reporting.13 As part of the pilot activities referred to above, 16 participants were asked to describe in more detail their activities during gardening and household activities. Responses suggested these items tended to be over-reported unless follow-up questions were asked. Many participants revised their estimations of time spent in these activities downward in response to probes by the interviewer. If these pilot results are representative, it may be preferable to reword the gardening and housework items. For example, a caveat such as, “please count events in which you are engaging in the activity for at least 10 minutes at a time,” or “please include only time when you are actively engaging in this specific activity” may help to reduce over-reporting on these items (such probes were used by the interviewer to reduce over-reporting in the pilot). Other options would be to offer a more inclusive list of heavy household and heavy gardening activities so as to reduce estimations about activities that a participant may perceive as strenuous but are not listed as such in the 2000 Compendium. These suggestions require further empirical examination.
Analysis of selected matched-pairs of items for possible double reporting suggested that 1 in 5 participants in the larger investigation may have double reported but only on 1 of the selected item pairs. Participants who may have double-reported were also more active based on accelerometry and were younger men. These results suggest that participants may simply have been more active, indicating that double-reporting may not be a serious problem within the CHAMPS. Nonetheless, more refined methods for examining double-reporting (eg, detailed querying following completion of the survey) are required before any definitive conclusions can be drawn.
Limitations and Strengths
There are several limitations to this study. One concerns the use of existing data to investigate attributes of the CHAMPS, as opposed to a study specifically designed to evaluate new CHAMPS scores and improve the method in a more controlled manner. There are known limitations to the use of accelerometers to assess light intensity activity.41 Therefore, accelerometry is not a true “gold standard” indicator of light activity and thus the correlations between accelerometry and the CHAMPS should be interpreted with caution. Although the present distinction between low-light and high-light activity was based on previous work by Copeland et al,27 the Copeland cut-point, which is approximately half of the conventional moderate-to-vigorous “Freedson” cut-point,25 was developed as an indicator of moderate-to-vigorous activity, not light intensity activity. Nonetheless, previous research that linked light intensity activity to health outcomes defined light activity as activity that was greater than sedentary and less than the Freedson count point.2 Therefore, the Copeland cut-point, although not originally defined as identifying “high-light” activity, may nonetheless be a good indicator for differentiating low-light and high-light as it is consistent with prior definitions of light activity.2 This conclusion is further supported by a recent study that examined the relation of different activity intensities to health outcomes, which used the Copeland cut-point to differentiate between “low-light” and “high-light” activity.7
The current study also has several strengths. The large sample size was drawn from 2 regions of the country, thus increasing generalizability of results. The sample included a large number of 80+ year old participants (n = 235), an age group that is often difficult to study. As is evident in Table 1, participants had a wide range of income and educational backgrounds, further improving generalizability. CHAMPS and accelerometer data were carefully matched by intensity, enhancing the validity analyses.
Conclusions
Results from the current study suggest the CHAMPS can reliably assess sedentary to moderate-to-vigorous activity in a diverse sample of older adults, and the moderate-to-vigorous activity and total meaningful activity variables were validated by accelerometry at the levels typically observed in other investigations. A new finding was the CHAMPS “high-light” scoring procedure appears to be a reliable and valid way of scoring the CHAMPS that may prove useful for future intervention trials that focus more exclusively on “high-light” physical activity and epidemiologic studies examining health impacts of activities of various intensities. CHAMPS and accelerometry variables were found to be only weakly associated for the sedentary and low-light variables, suggesting that, in its current form, the CHAMPS should not be used to assess sedentary and low-light activity. This finding is not unexpected, given that the CHAMPS was not originally developed to measure these 2 categories of activity behavior. It is possible that more precise estimates of sedentary behavior and physical activity could be captured using an open-ended response format, as well as additional items for sedentary behavior, but this would need to be empirically evaluated. Results further indicated that the CHAMPS may significantly overestimate moderate-to-vigorous intensity activity and underestimate sedentary behaviors. Based on this, the CHAMPS is likely best used as a relative indicator of physical activity rather than an absolute indicator. Overall, results from this study confirmed the validity of the CHAMPS for moderate-to-vigorous and total meaningful activity, as well as highlight activities–the latter consisting of activities in which older adults regularly engage, making them an important target for future study.
Supplementary Material
Acknowledgments
This study was funded by the Public Health Service Grant HL077141 from the National Heart, Lung, and Blood Institute. Hekler was supported by Public Health Service Training Grant 5 T32 HL 007034 from the National Heart, Lung, and Blood Institute.
Contributor Information
Eric B. Hekler, Stanford Prevention Research Center, Stanford University, Stanford, CA
Matthew P. Buman, Stanford Prevention Research Center, Stanford University, Stanford, CA
William L. Haskell, Stanford Prevention Research Center, Stanford University, Stanford, CA
Terry L. Conway, San Diego State University, San Diego, CA
Kelli L. Cain, San Diego State University, San Diego, CA
James F. Sallis, San Diego State University, San Diego, CA
Brian E. Saelens, Seattle Children’s Hospital Research Institute and the University of Washington, Seattle, WA
Lawrence D. Frank, University of British Columbia, Vancouver, British Columbia, Canada
Jacqueline Kerr, San Diego State University, San Diego, CA.
Abby C. King, Stanford Prevention Research Center, Stanford University, Stanford, CA
References
- 1.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9):S498–S516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 2.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 3.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviros in relation to risk of obesity and type 2 diabetes millitus in women. JAMA. 2003;289:1785–1791. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 4.Levine JA, Vander Weg MW, Hill JO, Klesges RC. Non-exercise activity thermogenesis: the crouching tiger hidden dragon of societal weight gain. Arterioscler Thromb Vasc Biol. 2006;26(4):729–736. doi: 10.1161/01.ATV.0000205848.83210.73. [DOI] [PubMed] [Google Scholar]
- 5.Vandelanotte C, Sugiyama T, Gardiner P, Owen N. Associations of leisure-time internet and computer use with overweight and obesity, physical activity and sedentary behaviors: cross-sectional stud. J Med Internet Res. 2009;9(3):e26. doi: 10.2196/jmir.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]; 11(3):e28. [Google Scholar]
- 6.Owen N, Bauman A, Brown W. Too much sitting: a novel and important predictor of chronic disease risk? Br J Sports Med. 2009;43(2):81–82. doi: 10.1136/bjsm.2008.055269. [DOI] [PubMed] [Google Scholar]
- 7.Buman MP, Hekler EB, Haskell WL, et al. Objective light intensity physical activity associations with rated health in older adults. Am J Epidemiol. 2010;172:1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Troiano RP, Berrigan D. Physical activity in the United States measured by accelerometer: comment - response. Med Sci Sports Exerc. 2008;40(6):1189. doi: 10.1249/MSS.0b013e31817057da. [DOI] [PubMed] [Google Scholar]
- 10.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washignton, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 11.Courneya KS, Jones LW, Rhodes RE, Blanchard CM. Effects of different combinations of intensity categories on self-reported exercise. Res Q Exerc Sport. 2004;75(4):429–433. doi: 10.1080/02701367.2004.10609176. [DOI] [PubMed] [Google Scholar]
- 12.Westerterp KR. Assessment of physical activity: a critical appraisal. Eur J Appl Physiol. 2009;105:823–828. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- 13.Altschuler A, Picchi T, Nelson M, Rogers JD, Hart J, Sternfeld B. Physical activity questionnaire comprehension: lessons from cognitive interviews. Med Sci Sports Exerc. 2009;41(2):336–343. doi: 10.1249/MSS.0b013e318186b1b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(2):S1–S14. [PubMed] [Google Scholar]
- 15.Neilson HK, Robson PJ, Friedenreich CM, Csizmadi I. Estimating activity energy expenditure: how valid are physical activity questionnaires? Am J Clin Nutr. 2008;87(2):279–291. doi: 10.1093/ajcn/87.2.279. [DOI] [PubMed] [Google Scholar]
- 16.Soundy A, Taylor A, Faulkner G, Rowlands A. Psychometric properties of the 7-day physical activity recall questionnaire in individuals with severe mental illness. Arch Psychiatr Nurs. 2007;21(6):309–316. doi: 10.1016/j.apnu.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 17.Shigematsu R, Sallis JF, Conway TL, et al. Age differences in the relation of perceived neighborhood environment to walking. Med Sci Sports Exerc. 2009;41(2):314–321. doi: 10.1249/MSS.0b013e318185496c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sallis JF, Saelens BE, Frank LD, et al. Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med. 2009;68(7):1285–1293. doi: 10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frank LD, Sallis JF, Saelens BE, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med. 2009 doi: 10.1136/bjsm.2009.058701. bjsm.2009.058701. [DOI] [PubMed] [Google Scholar]
- 20.Stewart AL. The reliability and validity of self-reported weight and height. J Chronic Dis. 1982;35:295–309. doi: 10.1016/0021-9681(82)90085-6. [DOI] [PubMed] [Google Scholar]
- 21.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 22.Welk GJ. Use of accelerometry-based activity monitors to assess physical activity. In: Welk GJ, editor. Physical activity assessments for health-related research. Champaign, IL: Human Kinetics, Inc; 2002. pp. 124–141. [Google Scholar]
- 23.Pruitt LA, Glynn NW, King AC, et al. Use of accelerometry to measure physical activity in older adults at risk for mobility disability. J Aging Phys Act. 2008;16(4):416–434. doi: 10.1123/japa.16.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welk GJ. Principles of design and analyses for the calibration of accelerometry-based activity monitors. Med Sci Sports Exerc. 2005;37(11, Suppl):S501–S511. doi: 10.1249/01.mss.0000185660.38335.de. [DOI] [PubMed] [Google Scholar]
- 25.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications Inc. Accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 26.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the united states, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. J Aging Phys Act. 2009;17(1):17–30. doi: 10.1123/japa.17.1.17. [DOI] [PubMed] [Google Scholar]
- 28.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 29.Starling RD, Matthews DE, Ades PA, Poehlman ET. Assessment of physical activity in older individuals: a doubly labeled water study, [erratum appears in J Appl Physiol 2001 May;90(5): following table of contents] J Appl Physiol. 1999;86(6):2090–2096. doi: 10.1152/jappl.1999.86.6.2090. [DOI] [PubMed] [Google Scholar]
- 30.Yokoyama Y, Kawamura T, Tamakoshi A, et al. Comparison of accelerometry and oxymetry for measuring daily physical activity. Circ J. 2002;66(8):751–754. doi: 10.1253/circj.66.751. [DOI] [PubMed] [Google Scholar]
- 31.Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Med Sci Sports Exerc. 2001;33(6):962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 32.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 33.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 34.Resnicow K, McCarty F, Blissett D, Wang T, Heitzler C, Lee RE. Validity of a modified CHAMPS physical activity questionnaire among African-Americans. Med Sci Sports Exerc. 2003;35(9):1537–1545. doi: 10.1249/01.MSS.0000084419.64044.2B. [DOI] [PubMed] [Google Scholar]
- 35.Cyarto EV, Marshall AL, Dickinson RK, Brown WJ. Measurement properties of the CHAMPS physical activity questionnaire in a sample of older Australians. J Sci Med Sport. 2006;9(4):319–326. doi: 10.1016/j.jsams.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 36.Moore DS, Ellis R, Allen PD, et al. Construct validation of physical activity surveys in culturally diverse older adults: a comparison of four commonly used questionnaires. Res Q Exerc Sport. 2008;79(1):42–50. doi: 10.1080/02701367.2008.10599459. [DOI] [PubMed] [Google Scholar]
- 37.Resnick B, King A, Riebe D, Ory M. Measuring physical activity in older adults—use of the community health activities model program for seniors physical activity questionnaire and the Yale Physical Activity Survey in three behavior change consortium studies. West J Nurs Res. 2008;30(6):673–689. doi: 10.1177/0193945907311320. [DOI] [PubMed] [Google Scholar]
- 38.Godard MP, Standley CM. Relationship between CHAMPS physical activity questionnaire and functional fitness outcomes in older adults. Act Adaptation Aging [Google Scholar]
- 39.Wilcox S, Dowda M, Leviton LC, et al. Active for life final results from the translation of two physical activity programs. Am J Prev Med. 2008;35(4):340–351. doi: 10.1016/j.amepre.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 40.King AC, Ahn DK, Oliveira BM, Atienza AA, Castro CM, Gardner CD. Promoting physical activity through hand-held computer technology. Am J Prev Med. 2008;34(2):138–142. doi: 10.1016/j.amepre.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crouter SE, Bassett DR., Jr A new 2-regression model for the Actical accelerometer. Br J Sports Med. 2008;42(3):217–224. doi: 10.1136/bjsm.2006.033399. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.