Abstract
Background & Objective
There has been concern over rising use of prescription opioids in young and middle-aged adults. Much less is known about opioid prescribing in older adults, for whom clinical recommendations and the balance of risks and benefits differ from younger adults. We evaluated changes in use of opioids and other analgesics in a national sample of clinic visits made by older adults between 1999 to 2010.
Design, Setting, Subjects
Observational study of adults age 65 and older from the 1999–2010 National Ambulatory and National Hospital Ambulatory Medical Care Surveys, serial cross-sectional surveys of outpatient visits in the United States.
Methods
Medication use was assessed at each study visit and included medications in use prior to the visit and medications newly prescribed at the visit. Results were adjusted for survey weights and design factors to provide nationally representative estimates.
Results
Mean age was 75 +/−7 years, and 45% of visits occurred in primary care settings. Between 1999–2000 and 2009–10, the percent of clinic visits at which an opioid was used rose from 4.1% to 9.0% (P<.001). Although use of all major opioid classes increased, the largest contributor to increased use was hydrocodone-containing combination opioids, which rose from 1.1% to 3.5% of visits over the study period (P<.001). Growth in opioid use was observed across a wide range of patient and clinic characteristics, including in visits for musculoskeletal problems (10.7% of visits in 1999–00 to 17.0% in 2009–10, P<.001) and in visits for other reasons (2.8% to 7.3%, P<.001).
Conclusions
Opioid use by older adults visiting clinics more than doubled between 1999–2010, and occurred across a wide range of patient characteristics and clinic settings.
Keywords: Analgesics, Opioid; Aged; Physician's Practice Patterns; Pharmacoepidemiology; Analgesics; United States
Introduction
There has been growing debate about prescribing opioid analgesics for older adults.1 Awareness of the undertreatment of pain in older adults has spurred more aggressive strategies to provide analgesia. Moreover, the gastrointestinal and renal toxicity of NSAIDs has prompted many physicians caring for older adults to use opioids in place of NSAIDs, a trend reinforced by pain guidelines issued by the American Geriatrics Society in 2009.2 At the same time, there has been increasing awareness of potential harms of opioid therapy that disproportionately affect older adults, including constipation, fractures, and cardiovascular events.3–5 In addition, although dependence and overdose-related death appear to be substantially less common in older adults than in their younger counterparts,6,7 definitive data on addiction to prescription opioids is limited in older adults.
A rapidly growing body of literature has documented the epidemiology and adverse health outcomes of opioid prescribing among young and middle-aged adults. Over the past 15 years, the use of opioids for chronic conditions in these populations has increased by approximately 50–100% in the United States and other countries.8–19 This greater frequency of use has been accompanied by increases in the dose and potency of opioids being prescribed to young and middle-aged adults, and by substantial growth in the rate of opioid dependence, addiction, and death from overdose.13,17,19,20 Despite this proliferation of research in younger adults, there are surprisingly little data about the epidemiology of opioid use in older adults, who have different prescribing considerations, risk-benefit tradeoffs, and insurance coverage than younger adults.
As more information becomes available about the benefits and burdens of opioid therapy in older adults, it is increasingly important to understand the epidemiology of opioid use in this population to define practice patterns and identify leverage points for improved prescribing. To this end, we sought to evaluate changes in the use of opioids and other analgesics among older adults seen in outpatient clinics in the United States between 1999 and 2010, and to define in what circumstances these drugs are most commonly used.
Methods
We used data on adults age 65 years and older from the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) from 1999 to 2010. NAMCS and NHAMCS are nationally representative serial cross-sectional surveys of patient visits in community-based and hospital based ambulatory clinics, respectively. Patient characteristics and characteristics of the visit (e.g., patient’s reason for visit, clinician diagnoses, and so forth) are recorded by the treating clinician or clinic staff at the completion of the visit. Approximately 30,000 visits are recorded per survey per year. NHAMCS also has a component to record care during emergency room visits, but we excluded these visits because of our focus on non-emergency ambulatory care.
Medication data were recorded for medications in use or newly prescribed at the time of the visit, and included up to 6 medications in 1999–2002 and up to 8 medications in 2003–2010. We classified analgesic medications into 4 mutually exclusive categories: opioids (including combination medications with an opioid component); acetaminophen (including acetaminophen combinations that did not include opioids); non-steroidal anti-inflammatory drugs (NSAIDs, including non-selective NSAIDs and COX-2 inhibitors); and gabapentin and pregabalin. Opioids were further subcategorized into mutually exclusive subcategories. We did not evaluate use of other medications that may have analgesic properties, including medications typically used to treat migraine headache (e.g., combination drugs with caffeine and butalbital, or triptans such as sumatriptan). We also did not evaluate anticonvulsant and antidepressant medications other than gabapentin and pregabalin. (We chose to include gabapentin and pregabalin because they are commonly used in the treatment of neuropathic pain, and use for this indication may exceed their use for other indications such as seizure prevention).21
As noted above, up to 6 medications were recorded in 1999–2002 and up to 8 medications were recorded in subsequent years. This difference in ascertainment might lead to undercounting of opioid use in the earlier study years relative to the later ones. We thus conducted sensitivity analyses to adjust for these differences in ascertainment. To do this, we started with data from years with up to 8 medication positions (2003–2010). Next, we determined the percentage of visits identified as involving an opioid if we considered only the first 6 medication positions, and we contrasted that with the percentage of visits identified as involving an opioid when we considered all 8 medication positions. Using the ratio of these two estimates, we extrapolated the expected frequency of opioid use in 1999–2002 if up to 8 medication fields had been available in those years. We repeated this process for the other analgesic classes of interest. Further detail is provided in Appendix 3.
For each visit, up to 3 patient reasons for the visit (i.e., presenting complaints) were recorded, as well as the acuity of the main reason for the visit. Reasons for visit were classified by NAMCS and NHAMCS into a standardized taxonomy. We considered visits to be for a musculoskeletal reason if one or more of the reasons for visit involved diseases of the musculoskeletal system and connective tissue, symptoms referable to the musculoskeletal system, injuries, or pain not referable to a specific site. If the patient did not have a musculoskeletal reason for the visit, we used the primary “reason for visit” code to identify the reason for visit. We grouped these codes by organ system and other major categories based on a schema provided by the National Center for Health Statistics.22 Starting in 2005, another section was added to the survey that recorded whether the patient had each of 14 common chronic conditions, regardless of whether those conditions were addressed during the visit.
NAMCS and NHAMCS employ a complex, multistage survey design that incorporates several layers of clustering, stratification, and probabilistic sampling. All analyses used standard techniques recommended by the National Center for Health Statistics to adjust for sampling weights and the complex survey design to make the results nationally representative of outpatient visits among adults age 65 years and older in the United States.23 These analyses included use of the surveyfreq and surveylogistic commands in SAS 9.3 for measures of association with analgesic use. Unless stated otherwise, tests of change in analgesic use over time were conducted using survey-adjusted logistic regression with data from all study years. However, for purposes of clarity, in the text of the paper we often report only the frequency of use at the beginning and end of the study period. (Complete data on point-prevalent use are provided in Appendix 1). To decrease variance in estimates of medication use in each time period, we divided the 12 study years into six 2-year blocks. This study was exempted from review by the institutional review boards of the University of California, San Francisco and San Francisco VA Medical Center.
Results
Over the 12-year study period, there were 148,509 surveyed visits by adults age 65 years and older, corresponding to a mean of 251 million outpatient visits by older adults per year. Mean age among older adults making outpatient visits was 75 +/−7 years, 58% of visits were made by women, and 45% of visits occurred in primary care clinics (Table 1). Most characteristics of patients and visits did not change substantially over the 12-year study period. For example, the percentage of visits that involved a musculoskeletal complaint or problem remained stable at 16–17% from the beginning to the end of the study period (data not shown).
Table 1.
Characteristics of patient visits, 1999–2010
| % (unadjusted N = 148,509)* |
|
|---|---|
| Age (mean, SD) | 75.4 ± 7.2 |
| Female sex | 58% |
| Race | |
| White | 88% |
| Black | 8% |
| Other race | 4% |
| Hispanic ethnicity † | 7% |
| National region | |
| Northeast | 21% |
| Central | 22% |
| South | 37% |
| West | 21% |
| Chronic conditions † | |
| Arthritis | 24% |
| Depression | 8% |
| Chronic renal failure | 4% |
| Congestive heart failure | 5% |
| Reason for visit | |
| Musculoskeletal complaint | 17% |
| Other reasons | 83% |
| Chronicity of problem that is main reason for visit | |
| Acute or new problem | 26% |
| Chronic problem | 53% |
| Other (e.g., health maintenance) | 21% |
| Specialty of treating clinician † | |
| Primary care | 45% |
| Surgical | 26% |
| Medical specialty | 30% |
| Community vs. hospital based clinic | |
| Community-based clinic | 94% |
| Hospital outpatient department | 6% |
All results adjusted for weights and survey design to produce nationally representative estimates
Data on Hispanic ethnicity from 2003–2010; data on chronic conditions from 2005–10. Data on clinician specialty available only for clinicians in community-based outpatient practice.
Patient, clinician, and clinic characteristics were similar across the study period with the exception of national region (proportion of visits in South 32% in 1999–2000 vs. 39% in 2009–10; proportion of visits in Northeast 23% vs. 18%, respectively) and clinician specialty (primary care 47% vs. 42% in 1999–2000 and 2009–10; surgical specialty 27% vs. 25%, and medical specialty 25% vs. 33%, respectively).
Some categories do not add to 100% due to rounding.
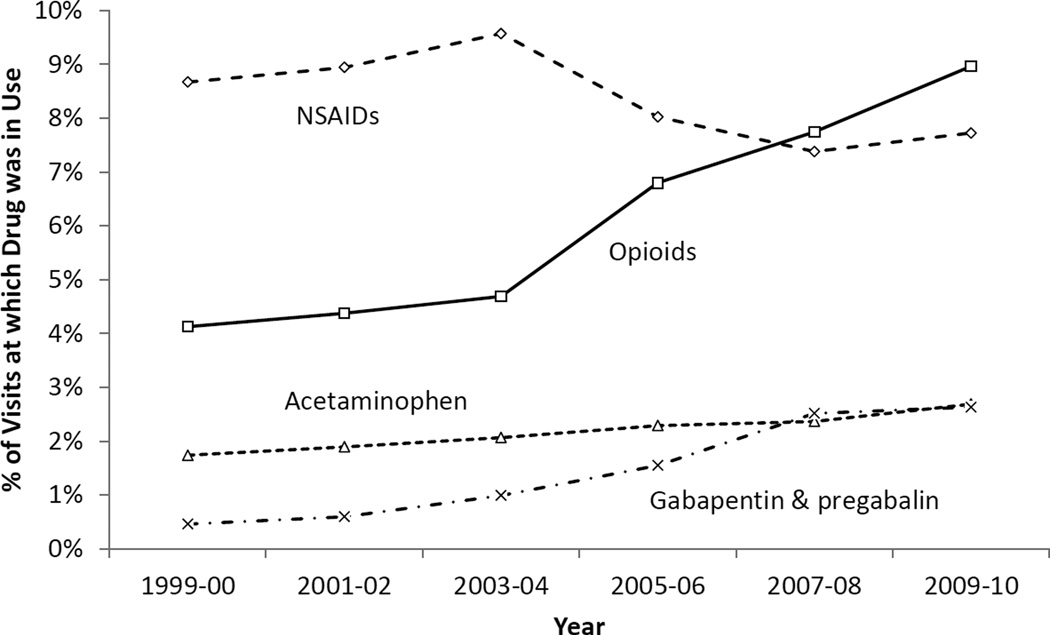
The percentage of visits at which any analgesic medication was in use rose from 13.6% in 1999–2000 to 19.1% in 2009–10 (P<.0001). Much of this rise was attributable to increased use of opioids, use of which increased from 4.1% to 9.0% of visits between 1999–2000 and 2009–2010 (P<.0001, Figure 1 and Appendix 1). Over this 12-year period there were changes in the use of other types of analgesics (Figure 1 and Appendix 1). NSAID use declined from 8.7% to 7.7% of visits (P=.002). Most of this decline was due to a sharp drop in the use of COX-2 selective NSAIDs during the middle of the decade, declining from a mean of 5.2% of visits in 2003–04 to 2.0% of visits in 2005–06. Increased use of non-selective NSAIDs over the same interval partially offset the decline in use of COX-2 inhibitors. Use of acetaminophen (alone or in combination with non-opioid drugs) rose from 1.7% to 2.7% of visits from 1999–2010 (P=.005), and use of pregabalin and gabapentin increased from 0.5% to 2.6% of visits (P<.001).
Figure 1. Use of analgesic medications by older adults at outpatient visits, 1999–2010.
Data on the chronicity of prescriptions became available starting in 2005. Most of the opioid use recorded at visits was for medications that were in ongoing use. Among the 9.0% of visits at which opioid use was recorded in 2009–10, in 6.0% of visits the opioid(s) were already in use prior to the visit, in 2.0% of visits the opioid(s) were newly prescribed at the time of the visit, and in 1.0% of visits the chronicity of opioid use was not recorded.
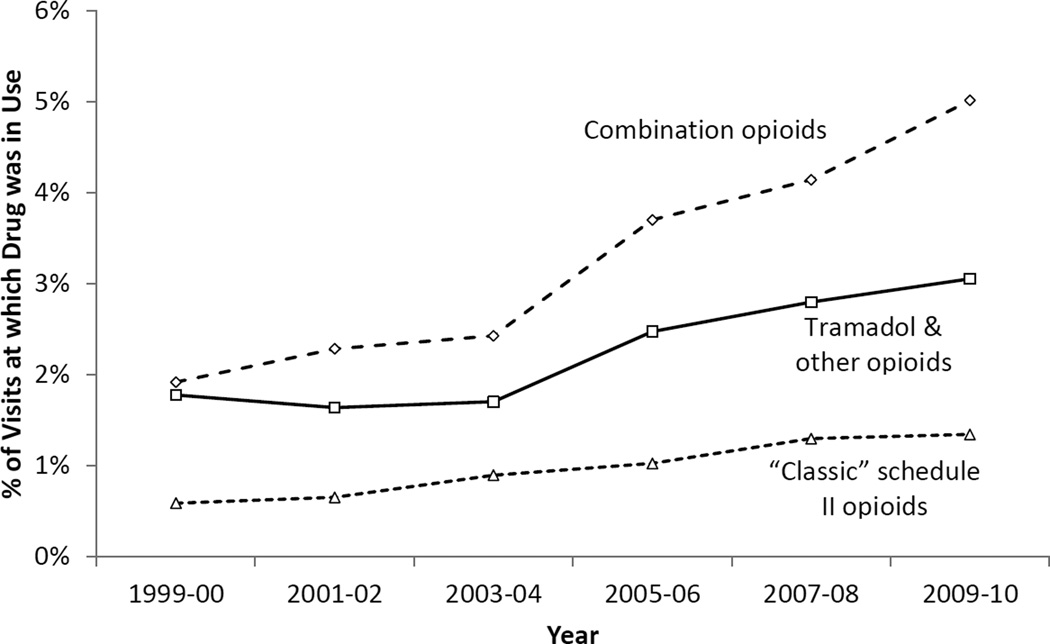
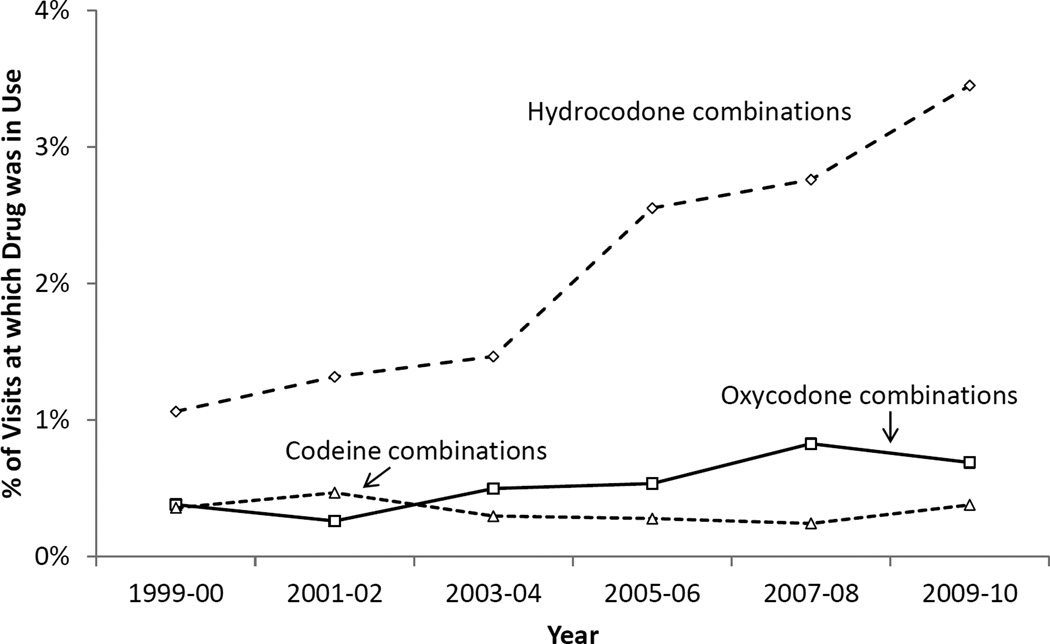
Over the 12-year study period, rising use of opioid-containing combination analgesics accounted for more than half of the total increase in opioid use (Figure 2). Use of these combination drugs increased from 1.9% of visits in 1999–2000 to 5.0% in 2009–2010 (P<.0001). Nearly all of this increase was due to increased use of hydrocodone-containing combinations such as hydrocodone-acetaminophen (often known by the brand name Vicodin). Hydrocodone combinations rose from 1.1% to 3.5% of visits over the study period (P<.0001), whereas use of combinations containing codeine and oxycodone were more stable (0.4% to 0.4%, P=.34 and 0.4% to 0.7%, P<.0001, respectively; Figure 3).
Figure 2. Use of opioid analgesics by older adults at outpatient visits, 1999–2010.
“Combination opioids” includes codeine, hydrocodone, or oxycodone combined with acetaminophen, ibuprofen, or similar agents; “Tramadol and other opioids” includes tramadol, pentazocine, or propoxyphene (alone or in combination); “Classic Schedule II opioids” includes stand-alone schedule II opioids including morphine, hydromorphone, oxycodone, and others.
Figure 3. Use of combination opioid analgesics by older adults at outpatient visits, 1999–2010.
Although combination opioids showed the sharpest increase in use, other types of opioids increased as well. Use of “classic” opioids such as morphine, hydromorphone, and oxycodone increased from 0.6% to 1.3% of visits from 1999–2000 to 2009–2010 (P<.0001). Tramadol (alone and in combination) and other schedule IV medications including pentazocine and propoxyphene increased in use from 1.8% to 3.1% of visits (P<.0001). Nearly all of this change was due to increases in use of tramadol preparations, from 0.5% of visits in 1999–2000 to 1.6% of visits in 2009–2010 (P<.0001). (Of note, propoxyphene was withdrawn from the U.S. market in November 2010, 2 months prior to the end of the study period).
Several patient and clinic characteristics were associated with use of opioids (Table 2). At both the beginning and end of the study period, opioid use was more common in visits by women than in men, in visits where the patient had arthritis and/or depression, and in visits conducted in primary care settings. Increases in opioid use over the study period were generally similar across these and a variety of other patient and clinic characteristics. However, the pattern varied somewhat by reason for visit. Among visits for musculoskeletal complaints, opioid use increased from 10.7% of visits in 1999–2000 to 17.0% in 2009–10 (P<.001). Among visits for other reasons, opioid use was less common but also rose over the study period from 2.8% to 7.3% of visits (P<.001). This included increases in opioid use from 2.8% to 8.5% of visits for mental and nervous system conditions, from 2.1% to 7.8% of visits for respiratory conditions, and from 4.1% to 5.4% of visits for digestive and genitourinary conditions (see Appendix 2 for additional information).
Table 2.
Percentage of visits by older adults at which an opioid was used, by patient, clinician, and clinic characteristics, 1999–2000 and 2009–2010
| 1999–2000 % (95% CI) of visits at which an opioid was in use |
P value | 2009–10 % (95% CI) of visits at which an opioid was in use |
P value | |
|---|---|---|---|---|
| Age group (years) | ||||
| 65–74 | 4.3 (3.6, 5.0) | 0.33 | 9.4 (8.0, 10.9) | 0.26 |
| 75–84 | 3.7 (3.1, 4.4) | 8.1 (6.9, 9.3) | ||
| 85+ | 4.6 (3.4, 5.8) | 9.5 (7.3, 11.7) | ||
| Sex | ||||
| Female | 4.7 (4.1, 5.3) | <0.001 | 9.9 (8.7, 11.2) | <0.001 |
| Male | 3.3 (2.6, 3.9) | 7.7 (6.5, 8.8) | ||
| Race | ||||
| White | 4.1 (3.6, 4.6) | 0.47 | 9.0 (7.9, 10.1) | 0.2 |
| Black | 4.6 (2.7, 6.4) | 9.4 (7.3, 11.5) | ||
| Other | 2.8 (1.1, 4.5) | 6.5 (4.1, 8.8) | ||
| Ethnicity * | ||||
| Hispanic | 5.5 (2.8, 8.2) | 0.23 | 7.2 (4.3, 10.0) | 0.18 |
| Non-Hispanic | 4.1 (3.5, 4.6) | 9.1 (7.8, 10.3) | ||
| National region | ||||
| Northeast | 3.3 (2.2, 4.3) | 0.21 | 6.8 (5.0, 8.6) | 0.32 |
| Central | 4.7 (3.7, 5.6) | 9.8 (8.0, 11.6) | ||
| South | 4.1 (3.5, 4.8) | 9.4 (8.0, 10.7) | ||
| West | 4.4 (3.3, 5.5) | 9.1 (5.7, 12.6) | ||
| Chronic conditions | ||||
| Arthritis | Data not available for these years | -- | 13.8 (11.8, 15.9) | <0.001 |
| Depression | 14.3 (11.2, 17.3) | <0.001 | ||
| Chronic renal failure | 7.1 (4.6, 9.6) | 0.17 | ||
| Congestive heart failure | 10.8 (8.4, 13.2) | 0.09 | ||
| Count of chronic conditions (mean ± SD) | Data not available for these years | -- | 2.3±1.5 | -- |
| Reason for visit | ||||
| Musculoskeletal issue | 10.7 (9.0, 12.4) | <0. 001 | 17.0 (14.3, 19.7) | <0.001 |
| Other issue | 2.8 (2.4, 3.2) | <0. 001 | 7.3 (6.4, 8.2) | |
| Chronicity of problem that is main reason for visit | ||||
| Acute or new problem | 5.0 (4.0, 6.0) | 0.02 | 10.1 (8.3, 12.0) | 0.007 |
| Chronic problem | 4.1 (3.4, 4.7) | 9.1 (8.1, 10.1) | ||
| Other (e.g., health maintenance) | 3.1 (2.3, 4.0) | 7.1 (5.7, 8.6) | ||
| Specialty of treating clinician | ||||
| Primary care | 4.8 (4.1,5.6) | <0.001 | 10.9 (9.2, 12.6) | <0.001 |
| Surgical | 2.3 (1.8,2.9) | 5.5 (4.4, 6.5) | ||
| Medical specialty | 4.2 (3.0,5.4) | 8.8 (7.1, 10.6) | ||
| Clinic setting | ||||
| Community-based clinic | 4.0 (3.5, 4.5) | 0.001 | 8.9 (7.8, 9.9) | 0.04 |
| Hospital outpatient department | 6.0 (4.7, 7.3) | 10.7 (9.0, 12.4) | ||
Opioid use can include an opioid newly prescribed at that visit, or an opioid already in use prior to the visit.
To facilitate comparison across study years, only visits in which Hispanic ethnicity was directly recorded (i.e., not imputed) were used in this analysis.
In sensitivity analyses, we adjusted the medication data in 1999–2002 to account for the lower number of medication fields in the dataset compared with 2003–2010. Under this approach, opioid use was estimated to be 4.6% in 1999–2000 (rather than the original estimate of 4.1%). Similarly proportional increases were obtained in the estimated frequency of use of other analgesics in 1999–2002 (see Appendix 3).
Discussion
In this nationally representative study, use of opioids among older adults making clinic visits more than doubled between 1999 and 2010. By the end of this period, almost one in ten clinic visits by older adults involved a patient using an opioid analgesic. Most of the increase in opioid use over this period was attributable to increasing use of combination opioids including hydrocodone (namely hydrocodone-acetaminophen, commonly known as Vicodin). Over the same period, use of acetaminophen remained relatively stable, use of NSAIDs fell slightly, and use of gabapentin and pregabalin rose, but at absolute levels far below those of opioids.
The growth in opioid use among older adults parallels increases seen in the general adult population. However, the implications of this rise in use may differ between age groups. In young and middle-aged adults, not only are rates of opioid use higher, but the potency of prescriptions (as measured in morphine equivalents) has been increasing as well. 8–20 Together, these have been associated with major increases in the rate of opioid addiction and overdoses, which has fueled a growing consensus that opioid prescribing has grown excessive and should be substantially curtailed.
In contrast, there is less certainty about the proper use of opioids in older adults, and the balance of these medications’ benefits and harms in this population.1 Pain is common in older adults, and is often undertreated. The potential benefits of opioids for older adults include reduced pain intensity and improved function.24 Other inconsistently reported benefits have included improvements in sleep and physical quality of life.24 Moreover, non-opioid analgesics such as NSAIDs have important adverse effects that disproportionately affect older adults. Due to these concerns, pain guidelines released by the American Geriatrics Society in 2009 de-emphasize the use of NSAIDs for control of nociceptive pain in older adults, such that for many patients with inadequate pain control on acetaminophen the next recommended step-up agent is an opioid.2 However, the potential benefits of opioid use are accompanied by risk for harms including constipation, nausea, and potentially increased risk of falls, fractures, and cardiovascular events.3,4,25 The risk of dependence and addiction is much less well-defined for older adults than younger ones, but remains an important consideration. Moreover, physicians can make potentially dangerous errors in prescribing opioids, such as starting patients on inappropriately high doses of opioids or starting opioid-naïve patients on long-acting opioids.26 Because the risk of severe opioid-associated adverse effects increases substantially with higher doses, and older adults in general are more susceptible to adverse drug events, special attention is warranted not only in the decision to treat or not treat with opioids, but in the initiation and titration of drug dose.
It is difficult to know what the optimal rate of opioid prescribing is for older adults. Nonetheless, our findings shed light on potential areas of focus for investigating and addressing the appropriateness of opioid prescribing. First, our results suggest a transition from shorter-term to longer-term use of opioids. Although we were unable to directly measure duration of prescribing over the entire study period, an increasing prevalence of opioid use observed in visits not for musculoskeletal complaints suggests that these drugs are already being chronically prescribed when patients see their clinicians for any of a variety of other problems. Second, the observation that opioid use in primary care settings is higher than in medical specialty and surgical clinics suggests that primary care clinicians are a critical target for efforts to optimize opioid use. Third, substantial increases in opioid use among patients with a wide variety of demographic characteristics and clinical characteristics suggests that attempts to improve opioid prescribing need to be applied broadly.
It is important to note that by 2009–2010, nearly 40% of patients taking opioids were prescribed hydrocodone-containing combinations, namely hydrocodone-acetaminophen (mainly known by the brand name Vicodin). The extensive use of this drug may reflect the fact that during the study period it was a schedule III controlled medication, meaning clinicians could prescribe up to a 6-month supply of the drug and call in a prescription to a pharmacy. This stands in contrast to tighter controls on schedule II medications such as oxycodone (alone or in combination). Similarly, the relatively sharp increase in opioid prescribing seen in the mid-2000s was largely attributable to increased used of hydrocodone-containing combinations, suggesting that these drugs may have been a gateway to increased opioid use during a period when many patients were switching off COX-2 inhibitors due to concerns about cardiovascular safety, and when the culture of the medical profession was shifting toward more aggressive approaches to pain control and greater comfort with prescribing opioids. The FDA is reclassifying hydrocodone-containing opioids as schedule II drugs as of late 2014, and in October 2013 FDA approved the first single-entity hydrocodone formulation. These changes will likely alter the landscape of opioid prescribing and present an opportunity to reevaluate opioid prescribing practices for older adults.
While increases in opioid use were the dominant finding of our study, evolving use of other types of analgesics also warrants attention. Moderate increases in acetaminophen use over the study period were compounded by sharp increases in the use of combination drugs containing acetaminophen and an opioid. Confusion over proper use of these medications can result in acetaminophen toxicity, a concern shared by FDA, which in 2011 mandated reductions in the amount of acetaminophen available in combination opioids.27 Use of gabapentin and pregabalin also rose sharply over the study period, suggesting a need for closer examination of how these drugs are being used.
This study has several limitations. First, the unit of analysis of the NAMCS and NHAMCS surveys is patient visits, rather than patients. Patients who seek outpatient care frequently are relatively over-represented in the dataset, and those who seek care infrequently are underrepresented. As a result, our results should not be interpreted as showing what percentage of older adults in the U.S. are taking opioids or other analgesics. Further research is needed to address this important question. Second, we were unable to assess drug dose, whether drugs were used regularly or as-needed, or to directly assess duration of prescriptions. Finally, the change in the number of medications recorded on the study form (up to 6 from 1999–2003, and up to 8 from 2004–2010) may lead to undercounting opioid use in the earlier years compared to the later ones. Nonetheless, sensitivity analyses that adjusted for this undercounting yielded results similar to those in our main analysis, and it is unlikely that differential ascertainment was responsible for the large increase in opioid prescribing observed over the study period.
Opioid prescribing for older adults remains controversial, and has been the subject of substantial swings in public and professional opinion, from concern to enthusiasm to modulated caution. Resolving these debates – and identifying evidence-based best practices – will require a substantial investment in research to understand the real-world benefits and harms of these drugs in older adults. Similarly, addressing this problem will require aggressive efforts to identify interventions that can be used to identify and improve the quality of opioid prescribing for ambulatory older adults.
Supplementary Material
Acknowledgments
Support: Supported by the National Institute of Aging and by the American Federation for Aging Research (1K23-AG030999 (MAS) and 1K07AG31779 (CSR)). The sponsors had no role in the design, analysis, authorship, or decision to publish this work.
Footnotes
Conflicts of interest: In 2001–2003, Dr. Steinman served as an unpaid expert witness in United States ex rel Franklin vs. Pfizer, which alleged improper marketing of gabapentin for uses not approved by the FDA. The authors have no other conflicts of interest to report.
Authorship
All authors meet criteria for authorship. Dr. Steinman takes responsibility for the integrity of the work.
Author roles are as follows:
- Conception and design: MAS, CSR
- Acquisition of data: MAS, KZF
- Analysis and interpretation of data: MAS, KDRK, KZF, CSR
- Drafting of article: MAS
- Revision for intellectual content: KDRK, KZF, CSR
REFERENCES
- 1.Reid MC, Bennett DA, Chen WG, et al. Improving the pharmacologic management of pain in older adults: identifying the research gaps and methods to address them. Pain Med. 2011 Sep;12(9):1336–1357. doi: 10.1111/j.1526-4637.2011.01211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009 Aug;57(8):1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- 3.Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of opioids for nonmalignant pain in older adults. Arch Intern Med. 2010 Dec 13;170(22):1979–1986. doi: 10.1001/archinternmed.2010.450. [DOI] [PubMed] [Google Scholar]
- 4.Solomon DH, Rassen JA, Glynn RJ, Lee J, Levin R, Schneeweiss S. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010 Dec 13;170(22):1968–1976. doi: 10.1001/archinternmed.2010.391. [DOI] [PubMed] [Google Scholar]
- 5.Buckeridge D, Huang A, Hanley J, et al. Risk of injury associated with opioid use in older adults. J Am Geriatr Soc. 2010 Sep;58(9):1664–1670. doi: 10.1111/j.1532-5415.2010.03015.x. [DOI] [PubMed] [Google Scholar]
- 6.Boscarino JA, Rukstalis M, Hoffman SN, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. 2010 Oct;105(10):1776–1782. doi: 10.1111/j.1360-0443.2010.03052.x. [DOI] [PubMed] [Google Scholar]
- 7.Sale JE, Thielke S, Topolovec-Vranic J. Who is addicted to, and dying from, prescription opioids? J Am Geriatr Soc. 2010 Jul;58(7):1401–1402. doi: 10.1111/j.1532-5415.2010.02902.x. [DOI] [PubMed] [Google Scholar]
- 8.Jeffrey Kao MC, Minh LC, Huang GY, Mitra R, Smuck M. Trends in ambulatory physician opioid prescription in the United States, 1997–2009. PM & R : the journal of injury, function, and rehabilitation. 2014;6(7):575–582. doi: 10.1016/j.pmrj.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Dorn SD, Meek PD, Shah ND. Increasing frequency of opioid prescriptions for chronic abdominal pain in US outpatient clinics. Clin Gastroenterol Hepatol. 2011 Dec;9(12):1078–1085. doi: 10.1016/j.cgh.2011.08.008. e1071. [DOI] [PubMed] [Google Scholar]
- 10.Campbell CI, Weisner C, Leresche L, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Public Health. 2010 Dec;100(12):2541–2547. doi: 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thielke SM, Simoni-Wastila L, Edlund MJ, et al. Age and sex trends in long-term opioid use in two large American health systems between 2000 and 2005. Pain Med. 2010 Feb;11(2):248–256. doi: 10.1111/j.1526-4637.2009.00740.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parsells Kelly J, Cook SF, Kaufman DW, Anderson T, Rosenberg L, Mitchell AA. Prevalence and characteristics of opioid use in the US adult population. Pain. 2008 Sep 15;138(3):507–513. doi: 10.1016/j.pain.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 13.Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010. Open medicine : a peer-reviewed, independent, open-access journal. 2012;6(2):e41–e47. [PMC free article] [PubMed] [Google Scholar]
- 14.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008 Jan 2;299(1):70–78. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 15.Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009 Dec;18(12):1166–1175. doi: 10.1002/pds.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daubresse M, Chang HY, Yu Y, et al. Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Med Care. 2013 Oct;51(10):870–878. doi: 10.1097/MLR.0b013e3182a95d86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han H, Kass PH, Wilsey BL, Li CS. Increasing trends in Schedule II opioid use and doctor shopping during 1999–2007 in California. Pharmacoepidemiol Drug Saf. 2013 Aug 19; doi: 10.1002/pds.3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olfson M, Wang S, Iza M, Crystal S, Blanco C. National trends in the office-based prescription of schedule II opioids. J Clin Psychiatry. 2013 Sep;74(9):932–939. doi: 10.4088/JCP.13m08349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franklin GM, Mai J, Wickizer T, Turner JA, Fulton-Kehoe D, Grant L. Opioid dosing trends and mortality in Washington State workers' compensation, 1996–2002. American journal of industrial medicine. 2005 Aug;48(2):91–99. doi: 10.1002/ajim.20191. [DOI] [PubMed] [Google Scholar]
- 20.Bernacki EJ, Yuspeh L, Lavin R, Tao XG. Increases in the use and cost of opioids to treat acute and chronic pain in injured workers, 1999 to 2009. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2012 Feb;54(2):216–223. doi: 10.1097/JOM.0b013e318240de33. [DOI] [PubMed] [Google Scholar]
- 21.Radley DC, Finkelstein SN, Stafford RS. Off-label prescribing among office-based physicians. Arch Intern Med. 2006 May 8;166(9):1021–1026. doi: 10.1001/archinte.166.9.1021. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. [Accessed 3 August, 2014];2010 NAMCS Micro-data file documentation. 2010 ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NAMCS/
- 23.National Center for Health Statistics. [Accessed August 13, 2014];Using ultimate cluster models with NAMCS and NHAMCS public use files. http://www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf.
- 24.Papaleontiou M, Henderson CR, Jr, Turner BJ, et al. Outcomes associated with opioid use in the treatment of chronic noncancer pain in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2010 Jul;58(7):1353–1369. doi: 10.1111/j.1532-5415.2010.02920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O'Neil CK, Hanlon JT, Marcum ZA. Adverse effects of analgesics commonly used by older adults with osteoarthritis: focus on non-opioid and opioid analgesics. Am J Geriatr Pharmacother. 2012 Dec;10(6):331–342. doi: 10.1016/j.amjopharm.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Logan J, Liu Y, Paulozzi L, Zhang K, Jones C. Opioid prescribing in emergency departments: the prevalence of potentially inappropriate prescribing and misuse. Med Care. 2013 Aug;51(8):646–653. doi: 10.1097/MLR.0b013e318293c2c0. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Food and Drug Administration. [Accessed 5 December, 2013];FDA limits acetaminophen in prescription combination products; requires liver toxicity warnings [press release] 2011 http://www.fda.gov/newsevents/newsroom/pressannouncements/ucm239894.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.