Abstract
Background
Nerve transfers have demonstrated encouraging outcomes in peripheral nerve reconstructions compared with the conventional direct repair or grafting.
Questions/Purposes
We aimed to identify whether the patient’s demographics, delay to surgery, degree of loss of grip and pinch strengths, mechanism of injury, and compliance to hand therapy have an impact on the functional outcome of motor nerve transfers in patients with paralytic hand.
Methods
Fifty-five patients with a mean age of 31.05 (18–48) years with complete isolated high injuries of radial, ulnar, and median nerves, who underwent motor nerve transfers, were reviewed. The outcome was assessed using the Medical Research Council (MRC) scale and measurement of grip and pinch strengths of the hand at minimum 1-year follow-up (mean of 14.4 (12–18) months). Patient’s age and gender, delay to surgery, body mass index (BMI), degree of loss of grip and pinch strengths, educational level, occupation, mechanism of injury, and compliance to hand therapy were analyzed to determine their impact on the extent of recovery of hand function.
Results
Forty of fifty five (72.73%) patients regained useful functional recovery (M3–M4) with satisfactory grip hand functions. Worse motor recovery was observed in older ages, delayed surgical intervention, higher BMI, and greater postoperative loss of grip and pinch strengths in comparison to the healthy opposite hand. Better outcomes are significantly associated with higher educational level and postoperative compliance to hand therapy. Contrarily, there was no significant association between gender, occupation, mechanism of injury, and achievement of useful functional recovery.
Conclusions
Successful nerve transfers are expected with experienced skilled surgeons. However, outstanding outcomes are not the standard, with about one fourth failing to achieve M3 grade. The educational level, hand dominance, compliance to hand therapy, loss of grip and pinch strengths, age, injury-surgery interval, and BMI are possible predictors of patients’ outcome.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-015-9459-3) contains supplementary material, which is available to authorized users.
Keywords: nerve transfer, neurotization, median nerve, radial nerve, ulnar nerve
Introduction
Historically, it is believed that the first nerve transfer was performed in the nineteenth century for brachial plexus avulsion injuries with poor results [15]. Credit is then given to Lurje, 1948, [14] who proposed transferring nearby undamaged nerves to the injured ones when direct repair was not conceivable. Advances in interfascicular grafting were subsequently popularized by Millesi in 1973 [17]. Unfortunately, poor results were reported because of the long regeneration distance particularly in the proximal injuries. Eventually, the suboptimal recovery of nerve grafting together with improved knowledge of intraneural topography inspired the subsequent resurgence of nerve transfers in early 1990s as they would offer earlier reinnervation, detouring the scarring in the zone of injury, and consequently minimizing atrophy of the target end organs [13].
Traditionally, the use of nerve transfers were restricted to brachial plexus avulsion injuries [5]. Because disruption of motor control of the hand makes it difficult to perform essential finger movements resulting loss of grip and pinch strengths [12], nerve transfers are increasingly used for these more distal injuries. Recently, promising results in limited case series have been reported [11, 20, 21].
Numerous factors contribute to patient’s outcome after nerve transfer such as the delay of surgery, patient’s age, and body mass index (BMI) [13]. Although the technical skills and strategies of the surgeon can have great influence, they have been proposed as hypothetical variables that could envisage outcomes after nerve transfers without solid evidence [21]. As yet, no study, to the best of our knowledge, has correlated all the purported variables with the functional outcomes after nerve transfer.
Accordingly, we aimed to assess (1) regain of motor power of individual muscles, (2) return of pinch and grip strengths, (3) percentage of hands that achieved functional recovery, and (4) the influence of patients’ demographics, time since injury, degree of postoperative loss of grip, and pinch strengths compared to the other healthy hand, mechanism of injury, and compliance to hand therapy on return of functional outcome following motor nerve transfers in complete isolated high injuries of median, ulnar, or radial nerves.
Patients and Methods
The study was carried out retrospectively for a case series of nerve transfers undertaken by a single surgeon between January 2010 and February 2014 in one specialized hand center after being approved by the institutional research board (IRB). A minimum 12-month postoperative follow-up interval for each patient was planned. Fifty-five patients were included in the study after fulfilling our inclusion/exclusion criteria. Inclusion criteria were both genders, patients aged 16 or more, complete isolated radial, ulnar or median nerve injuries (neurotmesis) above mid-forearm, and delayed presentation of more than 6 months following injury, without established medical contraindications to surgery. Patients were excluded if they had partial injuries, brachial plexus palsies, injuries that are expected to recover spontaneously (neuropraxia and axonotmesis), or established chronic illnesses affecting nerve healing or patients’ compliance (neuropathies, dementia, and mental retardation).
A chart review was performed of 55 injured nerves in 55 patients (34 males and 21 females). Patients mean age was 31.05 (18–48) years. Twenty-one patients were diagnosed with complete isolated high injury of the radial nerve. Twenty-two patients had ulnar, and 12 had median nerve lesions. All were treated with motor nerve transfers. We report a mean follow-up of 14.4 (12–18) months. Penetrating injuries with knife or glass (27 patients—49.09%), motor car accidents (6 patients—10.9%), firearm injury (6 patients—10.9%), iatrogenic (6 patients—10.9%), and fracture-induced laceration injuries (5 patients—9.09%) were the mechanisms of nerve injury.
All patients were evaluated in a systematic standardized fashion including preoperative clinical and physical evaluation, muscle testing of involved extremity and contralateral extremity using the Medical Research Council Grading System (MRC), electromyography, and nerve conduction studies. Preoperatively, all patients were found to have 0° range of motion (ROM) and M0–M1 grades on MRC scale. All nerve conduction studies were performed at least 3 months after the initial injury, to assess for evidence of reinnervation and for documentation of the injuries prior to surgery. Patients, who had motor unit potentials, were not offered surgery, and continued conservative management was pursued.
Surgical Technique
Using direct end to end microsurgical coaptation, the flexor carpi radialis/Palmaris longus (FCR/PL) and flexor digitorum superficialis (FDS) branches of median nerve were transferred to the posterior interosseous nerve (PIN) and extensor carpi radialis brevis (ECRB) branch of radial nerve respectively in 21 injured radial nerves to restore finger, thumb, and wrist extension [2]. In the 22 patients presented with ulnar nerve injuries, the distal anterior interosseous nerve (AIN) was transferred to the deep branch of ulnar nerve to restore intrinsic hand function and thumb adduction [20]. The ECRB branch of radial nerve and flexor carpi ulnaris (FCU) branch of ulnar nerve were transferred to the AIN and pronator teres branches of median nerve respectively in 12 injured median nerves to restore finger and thumb flexion as well as forearm pronation [11]. All procedures were performed by the first author (AS) using standard microsuturing technique utilizing an operating microscope with 9-0 nylon suture and utilizing a distal-based donor stump and proximally based recipient stump to ensure a tension-free repair. Repairs were performed with four epineural interrupted sutures.
The same postoperative protocol, as per the standard postoperative guidelines in our unit, was applied in all patients. Following surgery, all dressings were removed and all surgical wounds were reviewed by the third postoperative day. All patients commenced immediate ROM exercises for the uninvolved joints. The repair sites were protected from extreme ROM using splints for approximately 3 weeks. Stretching exercises were commenced at the 3 weeks’ time point. Moreover, electrical stimulation was initiated after 6 weeks. Nerve conduction velocity and electromyography were carried out to recognize signs of axonal regeneration. Focused motor reeducation was integrated in all physical therapy sessions, while all patients are given directed home exercises to promote the development of the new motor pathway for the recipient muscle.
The outcome was evaluated by either AS or ME (both are experienced, certified hand surgeons) using the MRC scale [6] and measurement of grip and pinch strengths (in kg) by Jamar Hydraulic Hand Dynamometer and JAMAR Hydraulic Pinch Gauge (Saehan Corporation, Masan, South Korea), respectively, at minimum 1 year post surgery. Useful functional recovery included those with both good (M4) and satisfactory (M3) functions. These grades reflect a motor power that enabled the patients to perform independently activities of daily living (ADL) and recommence the preinjury employment within 1 year following surgery. The Health Assessment Questionnaire (HAQ) was applied to assess the dependence/independence while performing ADL. “Another person’s help” and/or “unable to do” were assigned to dependence, while all other alternatives were assigned to independence [7, 8].
We have included various factors that might affect the functional outcome of motor nerve transfer. These subsumed age, gender, BMI, interval between injury and surgery, loss of grip/pinch strength, hand dominance, educational level, occupation (manual and non-manual workers), and compliance to hand therapy (defined as being compliant to the standard hand therapy program for a minimum of 3 months; a yes or no response). The postoperative loss of grip and pinch strengths was calculated by dividing the postoperative grip and pinch strength of the paralytic hand to those of the opposite healthy hand and then multiplied by 100. We have classified the educational level into experience (illiterate, read and write, primary and preparatory school), average (secondary and high schools), and university (university and higher degrees) levels. Regarding patients’ occupations, these were grouped by reliance on manual dexterity. Non-manual workers included skilled craftsmen using dexterity without heavy manual labor and those with light clerical occupations, while manual workers included laborers doing heavy work.
Statistical Analysis
A number of variables were measured on a continuous scale, and these were found to be normally distributed. Descriptive statistics were summarized with frequencies or means ± standard deviations. Logistic regression analysis was applied for categorical data and linear regression analysis for continuous data. Odds ratios were calculated for all categorical predictors examined. Student t test was used to compare between preoperative and postoperative findings. A p value <0.05 is considered to be statistically significant. All p values were two-tailed.
Results
Two patients (3.64%) with radial nerve injury developed tourniquet-induced numbness in the hand that was recovered spontaneously at 2 and 3 weeks postoperatively. Four patients (7.27%, one with radial nerve injury, two with ulnar nerve injury, and one with median nerve injury) developed postoperative superficial wound infection. The infection was mild and treated successfully only with intravenous antibiotics for 10 days. None of them required second surgery for eradication of infection. In this study, we have not encountered any clinical evidence of donor nerve-associated weakness among the study population.
The functional MRC scale of individual muscles significantly improved among the study population. Sixteen patients (76.2%) with radial nerve injuries regained M3 and M4 grades of wrist (10/21, 6/21), fingers and thumb extensors, and APL (11/21, 5/21), respectively. Sixteen patients (72.7%) with ulnar nerve injuries restored M3 and M4 grades of adductor pollicis and hand intrinsics (112/22, 4/22). M3 (6/12) and M4 (2/12) grades of finger and thumb flexors as well as forearm pronators were restored in eight patients (66.7%) with median nerve injuries.
Furthermore, a significant return of grip and pinch strengths was also achieved among the study population. Meangrip, tip pinch, palmar pinch, and key pinch strengths were significantly improved from 14 ± 2.3, 6.8 ± 0.7, 6.9 ± 0.7, and 7 ± 0.7 kg preoperatively to 33.5 ± 10.9, 7.6 ± 0.8, 7.7 ± 0.8, and 7.7 ± 0.9 kg, respectively postoperatively in patients with radial nerve injury (p < 0.001). Similarly, a significant improvement is observed in mean grip, tip pinch, palmar pinch, and key pinch strengths from 14.1 ± 2.4, 8.3 ± 0.8, 8.4 ± 0.7, and 8.3 ± 0.7 kg to 31.6 ± 10.5, 9.1 ± 0.9, 9.1 ± 0.9, and 9.1 ± 0.8 kg, respectively, in patients with ulnar nerve injury (p < 0.001) and from 23.9 ± 1.7, 4.9 ± 0.9, 5 ± 1, and 4.9 ± 0.8 kg to 35.6 ± 9.3, 6.5 ± 1.6, 6.6 ± 1.5, and 6.5 ± 1.6 kg, respectively, in patients with median nerve injury (p < 0.01). After adjusting for age, sex, and hand dominance, means for grip and pinch strengths loss were significantly lower (p < 0.001) for patients who regained useful functional recovery compared to those who could not (Table 1).
Table 1.
Adjusted* means of grip and pinch strength loss for the useful and non-useful functional recovery population
| Mean of strength loss | Functional recovery | p Value (t test) | |
|---|---|---|---|
| Useful | Non-useful | ||
| Radial nerve | |||
| Grip strength | 37 ± 2.2 | 71.5 ± 23.2 | <0.001 |
| Tip pinch | 38 ± 2.4 | 77.5 ± 13.9 | <0.001 |
| Palmar pinch | 38 ± 2.1 | 77.6 ± 14.1 | <0.001 |
| Key pinch | 38 ± 2.6 | 77.4 ± 13.9 | <0.001 |
| Ulnar nerve | |||
| Grip strength | 36.7 ± 2.6 | 67.9 ± 21.4 | <0.001 |
| Tip pinch | 37.2 ± 2.2 | 65.9 ± 20.1 | <0.001 |
| Palmar pinch | 36.9 ± 2.4 | 66.9 ± 21.2 | <0.001 |
| Key pinch | 37 ± 2.1 | 65.9 ± 18.4 | <0.001 |
| Median nerve | |||
| Grip strength | 49.9 ± 4.6 | 82.7 ± 8.8 | <0.001 |
| Tip pinch | 44.4 ± 3.4 | 81.7 ± 8.7 | <0.001 |
| Palmar pinch | 43.6 ± 3.8 | 80.7 ± 8.6 | <0.001 |
| Key pinch | 44.7 ± 4.2 | 82.2 ± 8.7 | <0.001 |
*Adjusted means for age, sex, and hand dominance
The majority of patients regained useful functional recovery of the hand. Of patients with radial, ulnar, and median nerve injuries, 76.2% (16/21), 72.7% (16/22), and 66.7% (8/12), respectively, had regained useful functional recovery. Dominance of the hand, level of education, and compliance to hand therapy were positively associated with useful functional recovery (p < 0.001, p < 0.001, and =0.004, respectively). The success rate in patients with average and university level was 84.2% (32/38) which was significantly better than in those with experience level (47.1%, 8/17). The success rate in patients with affected dominant hand (69.2%; 27/39) was significantly lower than in those with affected non-dominant hand (81.3%; 13/16). Of compliant patients to hand therapy, 89.5% (34/38) regained better useful recovery and resumed the preinjury work, compared with much lower success rate (35.3%; 6/17) in those who were non-compliant. Odds ratios for the predictors for useful functional recovery among the study subjects are summarized in Table 2.
Table 2.
Predictors for useful functional recovery
| Predictor | OR | 95% CI | p Value |
|---|---|---|---|
| Affected dominant hand | 0.167 | 0.09–0.31 | <0.001 |
| Compliance to hand therapy | 15.58 | 3.71–65.53 | <0.001 |
| Educational level | 0.167 | 0.05–0.61 | 0.004 |
| Occupation | 1.56 | 0.45–5.35 | 0.09 |
| Gender | 2.37 | 0.71–7.97 | 0.16 |
| Age | 0.01 | 0.00–0.02 | <0.001 |
| Injury-surgery interval | 0.06 | 0.03–0.08 | <0.001 |
| BMI | 0.05 | 0.03–0.08 | <0.001 |
BMI body mass index
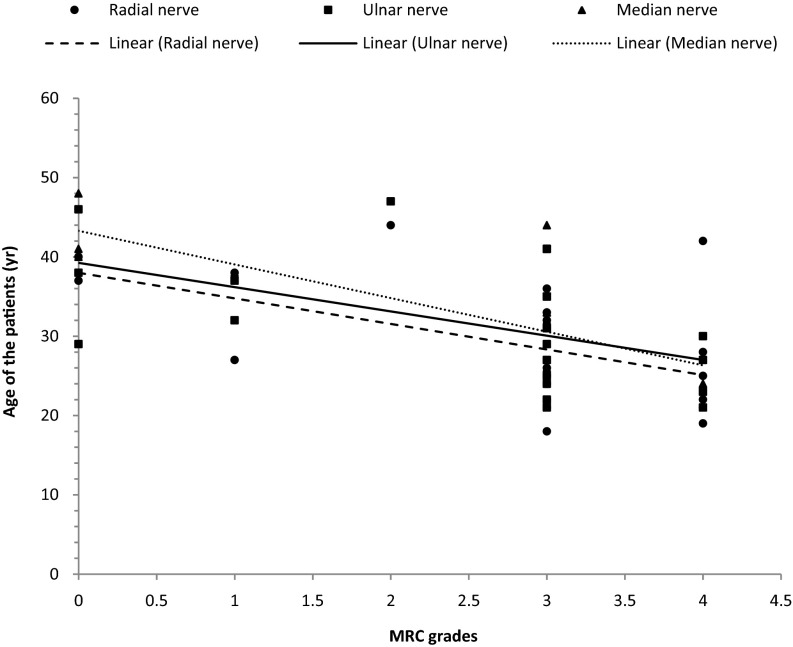
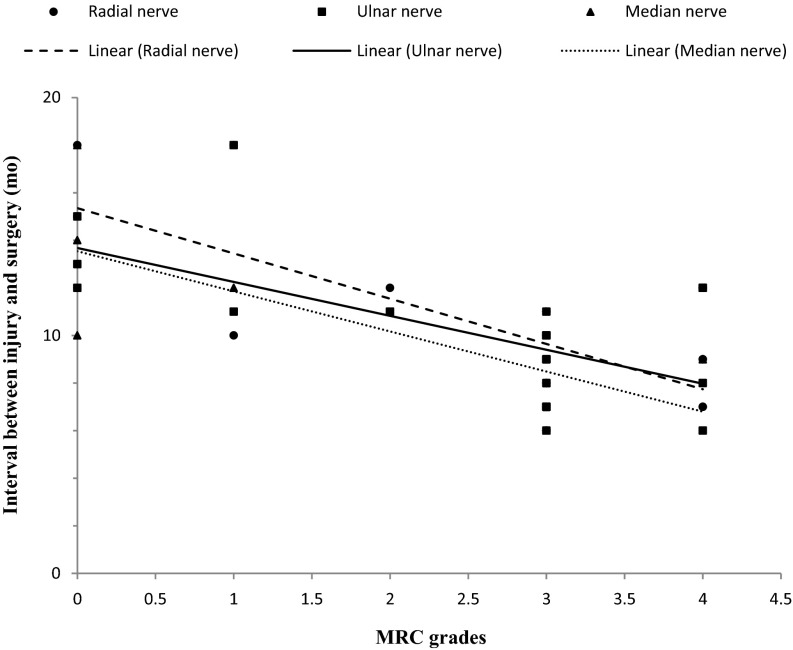
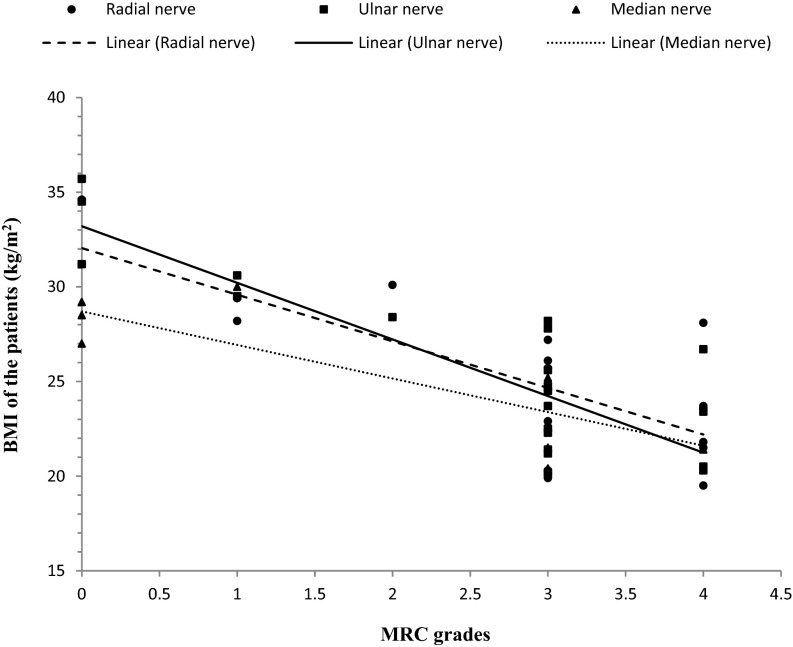
Our results revealed that the strength of radial, ulnar, or median innervated muscles correlated with the age of the patients (Fig. 1). There was a significant downward trend in the motor grade with increasing age. The success rate in patients 35 years or younger was 87.5% (17/40) which was significantly better than in patients older than 35 years (12.5%; 5/40, p < 0.001). Similarly, long intervals between injury and surgery tended to be a disadvantage in obtaining good or satisfactory results (Fig. 2). The success rate in patients operated 6–10 months after injury was 82.5% (33/40) which was significantly better than those operated after 10 months (17.5%; 7/40, p < 0.001). Finally, BMI significantly correlated with useful functional recovery. There was a downward trend in the motor grade with increasing BMI (Fig. 3). Contrarily, there was no statistically significant relationship between gender (p > 0.05); type of occupation (p > 0.05); and mechanism of injury (p > 0.05), and useful functional recovery.
Fig. 1.
The correlation between strength of radial, ulnar, and median innervated muscles and age of the patient (Rho = −0.483, p = 0.027; Rho = −0.565, p = 0.006; and Rho = −0.769, p = 0.003, respectively).
Fig. 2.
The correlation between strength of radial, ulnar, and median innervated muscles and interval between injury and surgery (Rho = −0.676, p = 0.001; Rho = −0.628, p = 0.002; and Rho = −0.668, p = 0.018, respectively).
Fig. 3.
The correlation between strength of radial, ulnar, and median innervated muscles and BMI of the patient (Rho = −0.683, p = 0.001; Rho = −0.713, p = 0.000; and Rho = −0.721, p = 0.008, respectively).
Discussion
The current study demonstrates that nerve transfers provide an efficient option in managing peripheral nerve injuries. We have illustrated a downward motor recovery in older ages, delayed surgical intervention, higher BMIs, and greater loss of grip and pinch strengths (p < 0.001). Our findings imply that better outcomes are significantly associated with higher educational level and postoperative compliance to hand therapy (p < 0.01). Contrarily, there is no significant association between gender, occupation, mechanism of injury, and useful functional recovery (p > 0.05). Among these factors, the delay from injury to surgery is the only factor that can be controlled, to some extent, by the surgeon [4]. While compliance to hand therapy and weight reduction are controlled by the patient himself.
This study has some limitations. A minimum of 12 months’ follow-up might not be sufficient to evaluate long-term recovery. However, the restoration of motor function, if it happens, would be achieved in 1-year time postoperatively. Although this study was retrospective, the results provide information for three different types of forearm nerve injury. Another limitation is that a comparative control group of isolated nerve injuries treated with interposition grafting was not available. Also, some would argue that, despite the wide acceptance of the MRC grading, it is still a subjective measure. However, an objective measurement of grip and pinch strengths was used in reviewing patients’ data for more precise evaluation of outcome. Another strength of our study is the fact that we had 100% follow-up in a prospective study and that it was a single surgeon study.
The importance of grip and pinch strength loss as a predictive factor was comparable with earlier studies [22]. This supports opinion in literature that grip and tip pinch strength measurements are important and reliable factors for capability to work [9].
A significant correlation was found between older age and poor outcome. Similarly, Karol et al. elucidated an inverse correlation between patients’ age and outcome [10]. This might be either lower repair capacity or greater preoperative damage [18]. Contrastively, Venkatramani et al. [23] suggested that the patient’s age should not be a criterion for denying treating, and good results are also expected as they achieved good results in two patients in early 50s after nerve transfer.
Similarly, a better prognosis was reported in this study with intervals between 6 and 10 months. In the case of proximal injury or long nerve gaps, there might be insufficient time for regenerating axons to reach the target motor endplates before they become permanently atrophied [19]. Fortunately, a nerve transfer essentially converts a high proximal injury to a low one. A distal nerve transfer within centimeters of the neuromuscular junction will still have the potential for successful reinnervation even if performed late (8–10 months) after the injury [16].
The current study finds a significant correlation between higher educational levels and favorable outcome. This could be explained by the assumption that patients with higher educational levels are more compliant to hand therapy. A standard hand therapy program was applied and essentially focused on ROM, muscle strength, and motor reeducation. Therefore, it might be concluded that retraining programs also have a positive influence encouraging successful useful recovery and resumption to occupation. This is in agreement with Bruyns et al. [3] who reported the educational level and compliance to hand therapy as predictors for return to work.
The BMI was identified in this study as a significant factor affecting the outcome. Higher BMIs were significantly associated with worse outcomes. This finding was confirmed by Lee et al. [13] who explained that patients with higher BMIs have poor physical fitness. Moreover, it was suggested that obesity may negatively affect peripheral nerve regeneration [1].
The hand dominance was thought to be an important factor affecting outcome after nerve reconstruction. This was confirmed by our results as a significantly better success rate was found among those with affected non-dominant hand. The dominant hand is frequently affected by nerve injury which could be an obstacle against ability to return to work [12].
The mechanism or type of injury had no correlation in our series with the functional recovery. This would be expected and actually considered an advantage of nerve transfers as we already operated in a new healthy area bypassing the zone of injury. Similarly, gender and occupation had no influence on the outcome. Despite the insignificant correlation between occupation and outcome in our results, other authors had concluded a worse prognosis in manual workers [3, 12]. Our result could be attributed to firstly, the wide spectrum of the non-manual workers group and the small size of the manual workers group represented, secondly, to the fact that we did not announce for those who changed their occupation after recovery as they were included among those who did not regain the preinjury employment.
Moreover, we did not include other variables including ethnicity, onset of workers’ compensation, and pending litigation, which may influence the final outcome after this type of surgery. Other factors, which are not included in analysis, are patient medical comorbidities and American Society of Anaesthesiologists (ASA) scores that might affect outcome.
Finally, although this is a single center study, our hand unit is a tertiary unit serving a population of more than five million people. We serve a broad spectrum of social and ethnic groups and believe that our data is relevant to the wider community. More research should be conducted to identify the predictors and moderators for functional outcome after nerve transfers.
We recommend a cautious prognosis when considering nerve transfer in the older age groups, obese patients, and in delayed presentations of more than 10 months as well as dominant hand affection. Our findings suggest that the education levels and lower degrees of grip and pinch strengths loss significantly associated with good outcomes. We found no association between gender, occupation, and mechanism of injury with useful functional recovery.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Disclosures
Conflict of Interest
Asser A. Sallam, MD, PhD, Mohamed S. El-Deeb, MD and Mohamed A. Imam, MD, PhD have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 [5].
Informed Consent
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study, Level IV (Retrospective Study)
References
- 1.Bekar E, Altunkaynak BZ, Balci K, Aslan G, Ayyildiz M, Kaplan S. Effects of high fat diet induced obesity on peripheral nerve regeneration and levels of GAP 43 and TGF-beta in rats. Biotechnic & histochemistry : official publication of the Biological Stain Commission. 2014;89(6):446–456. doi: 10.3109/10520295.2014.894575. [DOI] [PubMed] [Google Scholar]
- 2.Brown JM, Tung TH, Mackinnon SE. Median to radial nerve transfer to restore wrist and finger extension: technical nuances. Neurosurgery. 2010;66(3 Suppl Operative):75–83. doi: 10.1227/01.NEU.0000354364.13224.C8. [DOI] [PubMed] [Google Scholar]
- 3.Bruyns CN, Jaquet JB, Schreuders TA, Kalmijn S, Kuypers PD, Hovius SE. Predictors for return to work in patients with median and ulnar nerve injuries. The Journal of hand surgery. 2003;28(1):28–34. doi: 10.1053/jhsu.2003.50026. [DOI] [PubMed] [Google Scholar]
- 4.Christie B. Doctors revise Declaration of Helsinki. BMJ : British Medical Journal. 2000;321(7266):913–913. doi: 10.1136/bmj.321.7266.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chuang DC, Yeh MC, Wei FC. Intercostal nerve transfer of the musculocutaneous nerve in avulsed brachial plexus injuries: evaluation of 66 patients. The Journal of hand surgery. 1992;17(5):822–828. doi: 10.1016/0363-5023(92)90451-T. [DOI] [PubMed] [Google Scholar]
- 6.Daniels L, Worthingham C. Muscle testing: techniques of manual examination. 5. Philadelphia: Saunders; 1986. [Google Scholar]
- 7.Dellhag B, Bjelle A. A five-year followup of hand function and activities of daily living in rheumatoid arthritis patients. Arthritis care and research : the official journal of the Arthritis Health Professions Association. 1999;12(1):33–41. doi: 10.1002/1529-0131(199902)12:1<33::AID-ART6>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis & Rheumatism. 1980;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Pena C, Garcia-Fabela LC, Gutierrez-Robledo LM, Garcia-Gonzalez JJ, Arango-Lopera VE, Perez-Zepeda MU. Handgrip strength predicts functional decline at discharge in hospitalized male elderly: a hospital cohort study. PloS one. 2013;8(7) doi: 10.1371/journal.pone.0069849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gutowski KA: Peripheral nerves and tendon transfers. In: The Hand. Volume II, edn.: Selected Readings in Plastic Surgery; 2003: 23.
- 11.Hsiao EC, Fox IK, Tung TH, Mackinnon SE. Motor nerve transfers to restore extrinsic median nerve function: case report. Hand (N Y) 2009;4(1):92–97. doi: 10.1007/s11552-008-9128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jaquet JB, Luijsterburg AJ, Kalmijn S, Kuypers PD, Hofman A, Hovius SE. Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. The Journal of trauma. 2001;51(4):687–692. doi: 10.1097/00005373-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Lee JY, Kircher MF, Spinner RJ, Bishop AT, Shin AY. Factors affecting outcome of triceps motor branch transfer for isolated axillary nerve injury. The Journal of hand surgery. 2012;37(11):2350–2356. doi: 10.1016/j.jhsa.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 14.Lurje A. Concerning Surgical Treatment of Traumatic Injury to the Upper Division of the Brachial Plexus (Erb’s Type) Annals of surgery. 1948;127(2):317–326. doi: 10.1097/00000658-194802000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackinnon SE, Colbert SH. Nerve transfers in the hand and upper extremity surgery. Techniques in hand & upper extremity surgery. 2008;12(1):20–33. doi: 10.1097/BTH.0b013e31812714f3. [DOI] [PubMed] [Google Scholar]
- 16.Mackinnon SE, Roque B, Tung TH. Median to radial nerve transfer for treatment of radial nerve palsy. Case report. Journal of neurosurgery. 2007;107(3):666–671. doi: 10.3171/JNS-07/09/0666. [DOI] [PubMed] [Google Scholar]
- 17.Millesi H. Microsurgery of peripheral nerves. The Hand. 1973;5(2):157–160. doi: 10.1016/0072-968X(73)90061-2. [DOI] [PubMed] [Google Scholar]
- 18.Mondelli M, Padua L, Reale F. Carpal tunnel syndrome in elderly patients: results of surgical decompression. Journal of the peripheral nervous system : JPNS. 2004;9(3):168–176. doi: 10.1111/j.1085-9489.2004.09309.x. [DOI] [PubMed] [Google Scholar]
- 19.Newton CD, Nunamaker DM: Textbook of small animal orthopaedics. In., edn. Philadelphia: Lippincott; 1985: xxiv, 1140 p.
- 20.Novak CB, Mackinnon SE. Distal anterior interosseous nerve transfer to the deep motor branch of the ulnar nerve for reconstruction of high ulnar nerve injuries. Journal of reconstructive microsurgery. 2002;18(6):459–464. doi: 10.1055/s-2002-33326. [DOI] [PubMed] [Google Scholar]
- 21.Ray WZ, Mackinnon SE. Clinical outcomes following median to radial nerve transfers. The Journal of hand surgery. 2011;36(2):201–208. doi: 10.1016/j.jhsa.2010.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruijs AC, Jaquet JB, Kalmijn S, Giele H, Hovius SE. Median and ulnar nerve injuries: a meta-analysis of predictors of motor and sensory recovery after modern microsurgical nerve repair. Plastic and reconstructive surgery. 2005; 116(2): 484-494. discussion 495-496. [DOI] [PubMed]
- 23.Venkatramani H, Bhardwaj P, Faruquee SR, Sabapathy SR. Functional outcome of nerve transfer for restoration of shoulder and elbow function in upper brachial plexus injury. Journal of brachial plexus and peripheral nerve injury. 2008;3:15. doi: 10.1186/1749-7221-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)