Abstract
Background:
Urolithiasis in pediatric population is a serious problem with the incidence increased these years. In the management of larger stones (diameters >2 cm), percutaneous nephrolithotomy (PCNL) is considered to be the gold standard. This study aimed to investigate the efficacy and safety of mini-PCNL under total ultrasonography in patients aged <3 years.
Methods:
We reviewed 68 patients (80 renal units) aged <3 years between August 2006 and December 2014 in Peking University People's Hospital and Beijing Tsinghua Changung Hospital, including 36 renal units with a single stone, 6 with staghorn stones, 14 with upper ureteral stones, and 24 with multiple stones. The mean age of the patients was 24.2 months (range 6–36 months), and the mean maximum stone diameter was 19.2 mm (range 10–35 mm). The puncture site selection and tract dilation were guided by Doppler ultrasonography solely. All procedures were performed using 12–16 Fr tracts. Stones were fragmented using pneumatic lithotripsy and a holmium laser with an 8/9.8 Fr rigid ureteroscope.
Results:
Fifty-six patients with unilateral stones underwent a single session procedure, and 12 patients with bilateral stones underwent two procedures. The mean time to establish access was 2.8 min (range 1.8–5.0 min), the mean operative time was 36.5 min (range 20–88 min), the mean decrease in hemoglobin concentration was 8.9 g/L (2–15 g/L), and the stone-free rate (SFR) at hospital discharge was 94.0%. The mean postoperative hospital stay was 7.1 days (range 3–13 days). Postprocedure complications included fever (>38.5°C) in five patients and reactive pleural effusion in one patient. Blood loss requiring transfusion, sepsis, adjacent organ injury, and kidney loss were not observed.
Conclusions:
This study indicated that ultrasound-guided mini-PCNL is feasible and safe in patients aged <3 years, without major complications or radiation exposure.
Keywords: Calculi, Infant, Kidney, Percutaneous Nephrolithotomy, Ultrasonography
INTRODUCTION
The incidence of pediatric urolithiasis varies by area to area. Most cases of pediatric urolithiasis are associated with anatomic or metabolic abnormalities or urinary tract infections.[1] The European Association of Urology guidelines recommend shock wave lithotripsy (SWL) as the first choice of treatment for renal stones with a diameter of ≤20 mm. Children pass the stone fragments produced by SWL more rapidly than adults,[2,3] but SWL requires repeated sessions under general anesthesia. With advances in technology and increased experience, percutaneous nephrolithotomy (PCNL) is now performed in selected patients such as those with large stones, cystine stones, and SWL-refractory stones. PCNL enables direct visualization and clearance of stones and is associated with less need for ancillary procedures and a shorter hospital stay than SWL. However, urologists are often reluctant to attempt PCNL in young children because of their fragile kidneys with small collecting systems, and the potentially high risk of parenchymal injury, bleeding, and sepsis. Only few previous studies have reported on outcomes after PCNL in patients aged <3 years and both these studies mostly used fluoroscopic guidance.[4,5] Such young children are sensitive to the effects of ionizing radiation, which should, therefore, be minimized during procedures.[6] Ultrasonography is useful for visualization of the intrarenal arteries and nonopaque stones, and does not expose the patient to radiation. For the small collecting system and slim calyces, we used small tracts rather than adult-sized tracts to perform PCNL in these patients. This study aimed to evaluate the feasibility and safety of ultrasound-guided mini-PCNL in patients aged <3 years according to our initial experience.
METHODS
Patients
We performed mini-PCNL under Doppler ultrasonography solely in 80 renal units of 68 patients aged <3 years (40 males, 28 females) at Department of Urology in Peking University People's Hospital and Beijing Tsinghua Changung Hospital between August 2006 and December 2014, including 36 (45.0%) renal units with single stones, 6 (9.0%) with staghorn stones, 14 (17.5%) with upper ureteral stones, and 24 (30.0%) with multiple stones. Twelve patients suffered bilateral upper urinary stones. The mean age of the patients was 24.2 months (range 6–36 months). The mean maximum stone diameter was 19.2 mm (range 10–35 mm), measured by the longest axis on preoperative images. In renal units with multiple stones, the maximum diameter of the largest stone was recorded. Mild hydronephrosis was presented in 62 (77.5%) renal units. Nine (11.3%) renal units underwent SWL as first-line therapy but failed. Radiography and computed tomography (CT) were usually performed to evaluate the shapes of collecting system and stones. Six patients had hyperuricemia and six had cystinuria. Antibiotics (e.g., penicillins, cephalosporins, azithromycin) were prescribed to patients with urinary tract infections to ensure sterile urine at the time of the procedure and to avoid sepsis after the procedure.
Procedures
All procedures were performed under general anesthesia. Retrograde catheterization was performed using a 3 Fr ureteral catheter in the lithotomy position to fill the collecting system, and the patient was placed in the prone position. A 17.5 gauge coaxial needle was introduced into the fornix of the targeted calyx under ultrasonography [Figure 1]. Target calyx was punctured using a free-hand technique to enable minor adjustments to the position of the needle. After urine reflux was observed, a J-shaped guidewire was inserted through the needle into the collecting system, and the position of the guidewire can be confirmed by ultrasonography [Figure 2]. A 1-cm skin incision was made and the access was dilated using serial fascial dilators over the guidewire, and a 12–16 Fr peel-away sheath was left in place to facilitate observation using an 8/9.8 Fr rigid ureteroscope. The stones were fragmented using pneumatic lithotripsy and a holmium laser, then retrieved using a grasper or nitinol basket, or flushed out using a pulsed water pump. The kidney was then checked for residual stones to determine whether additional tracts were required for stone removal. The procedure was considered complete when no further stones were detected on ultrasonography. A 4.7 Fr double-J stent was inserted antegrade, and balloon catheter was placed as nephrostomy tube.
Figure 1.

(a) The major vessels and the avascular zone were identified using color Doppler ultrasound; (b) The middle posterior calyx was chosen as the target calyx; (c) The needle entered the collection system through the calyceal fornix.
Figure 2.
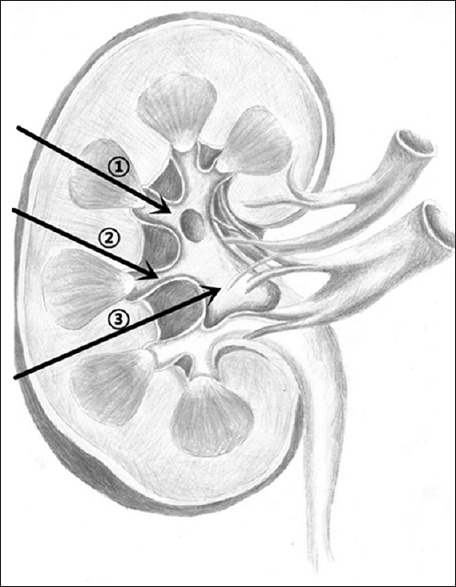
Positions for puncture: (1) Introduced the needle into calyx from the fornix is correct; (2) and (3) Access to the collecting system from renal column is very dangerous.
A complete blood count and serum biochemistry testing were performed immediately after the procedure. Prophylactic antibiotics were administered according to the urine culture and antibiogram results. A kidney-ureter-bladder plain film or CT (for radio-opaque stones) was performed 24–48 h after the procedure to assess the results. Clinically significant residual fragments were defined as stones >4 mm in diameter. The nephrostomy tube was clamped after 2–3 d if there was no fever, urine leakage, or bleeding, and was subsequently removed if clamping did not cause discomfort. Most double-J stent was removed by cystoscopy after about 1 month to facilitate the discharging of fragments. The stone-free rate (SFR) at the time of hospital discharge was calculated.
RESULTS
The collecting system was successfully accessed under ultrasound guidance in all cases. The calyx most commonly accessed first was the middle posterior calyx (47 renal units, 58.8%), followed by the lower pole calyx, and the upper pole calyx was accessed first in only 5 (6.3%) renal units. The tract size was 14–16 Fr in 45 patients (all aged > 24 months) and 12 Fr in the remaining 23 patients. Seventy (87.5%) renal units were treated using a single tract, and the remaining 10 (12.5%) were treated using two tracts. The 56 patients with unilateral stones underwent a single procedure, and the 12 patients with bilateral stones underwent two procedures. In patients who underwent two procedures, the second procedure was performed 1 month after the first procedure, and the double-J stent from the first procedure was removed at the same time. A needle-assisted procedure was successfully used in six patients, avoided to add another channel. The mean time to establish the channel was 2.8 min (range 1.8–5 min) and the mean operating time (from puncturing of the renal calyx to placement of the nephrostomy tube) was 36.5 min (range 20–88 min). The hemoglobin concentration decreased after the procedure in 52 (76.5%) patients, mean degree was about 8.9 g/L (range 2–15 g/L). The mean postoperative hospital stay was 7.1 days (range 3–13 d). Stone-free status was recorded in 75 (94.0%) renal units at the time of hospital discharge. Five (6.0%) renal units had residual stones with an approximate diameter of 5 mm at the time of hospital discharge, and were managed by active watching without further invasive procedures. Postprocedure complications included transient fever (>38.5°C) in 5 (7.4%) patients, which was managed with 3 days of antibiotic therapy. One patient who underwent puncture of the upper calyx developed recurrent fever, and fluoroscopy showed a reactive right pleural effusion, which was treated conservatively with antibiotic therapy. This patient recovered without further complications and was discharged from hospital after 7 days. There were no cases of blood loss requiring transfusion, sepsis, conversion to open surgery, damage to adjacent organs, or kidney loss. Stone analysis by infrared spectrophotometry was performed in 45 patients, and showed calcium oxalate stones in 25 (36.8%) patients, uric acid stones in 6 (8.8%) patients, struvite stones in 5 (7.4%) patients, mixed composition stones in 5 (7.4%) patients, and cystine stones in 4 (5.9%) patients.
DISCUSSION
When melamine-contaminated powdered milk formula was discovered in China in 2008, the Chinese government recognized that melamine ingestion was likely to be related to the high incidence of renal stones in infants, and widespread free screening for renal stones was instituted immediately.[7] In our role as the Urinary Stones Research Center for Northern China, we admitted nearly 200 patients aged <3 years with renal stones until now. Approximately, half of these patients were exposed to melamine-contaminated food. SWL remains the most popular procedure for the management of renal stones in young children.[8] SWL is more effective at fragmenting large stones in young children than in adults, and children tend to pass the resulting stone fragments more rapidly than adults, with few complications.[9,10] However, the long-term effects of SWL on the developing kidneys and adjacent organs are still unclear. The risks associated with the passage of stones and the relatively low success rate of SWL for the treatments of large stones have hindered the widespread use of SWL. In China, many urologists are reluctant to perform SWL in young children because of the risks associated with general anesthesia and of subsequent urinary tract obstruction. SWL was therefore not commonly performed in young children at our institute. Flexible ureteroscopy is more and more widely used in pediatric renal stones. Although the use of flexible instruments seems feasible for the present time, more data are needed for comparison with other methods.[11,12]
Percutaneous nephrolithotomy can be performed safely and effectively by experienced surgeons, resulting in a higher stone-free rate and lower requirement for ancillary treatment.[13,14] Use of adult-sized instruments may not be appropriate in young children because the kidneys are small and fragile. Treatment of the small collecting system in these patients requires the use of suitably sized instruments to prevent serious complications such as parenchymal lacerations and bleeding.[15] A previous study reported no significant differences in parenchymal damage or blood loss between the use of 11 Fr and 30 Fr tracts in adults,[16] but Desai et al.[17] reported that a larger tract size was associated with a higher rate of intraoperative hemorrhage and a larger decrease in hemoglobin concentration in children. In our series, a 14–16 Fr tract was used in patients >24 months, and a 12 Fr tract was only used in patients aged <12 months.
In adults, PCNL is performed under fluoroscopic or ultrasound guidance. In patients <3 years old, fluoroscopic guidance was preferred in most reported studies.[4,14,18,19] However, fluoroscopy exposes the patient to radiation. The main factor affecting the amount of radiation exposure is the screening time. The International Commission on Radiological Protection (ICRP) recommends that whole-body exposure in adults should be limited to an effective dose of 20 mSv/year over 5 years.[20] Even when protective measures are in place, patients can be exposed to scattered radiation during the procedure. In young children, it is particularly important to protect the developing gonads and thyroid gland, as the long-term effects of exposing these organs to radiation are still unclear. Unfortunately, melamine-associated renal stones are often radiolucent, and therefore not visible on plain radiographs.[21] In contrast to fluoroscopic guidance, ultrasound guidance can provide real-time monitoring during the puncturing procedure. The path and depth of the needle and the anatomy in and around the kidney are clearly visible on ultrasound examination.[22] We used a 3.5 MHz convex array probe and identified the major vessels using color Doppler ultrasound. Access via the fornix of the middle posterior calyx was preferred because this is always an avascular zone, and because this also allows access to the other calyces [Figure 2]. This is very important to reduce bleeding during or after surgery. Calyceal puncture was performed using a free-hand technique to enable adjustment of the position of the needle. Successful access to the renal collecting system was confirmed by aspiration of urine. After the placement of the peel-away sheath, a rigid 8/9.8 Fr ureteroscope was inserted through the sheath. The renal stones were fragmented using pneumatic lithotripsy and a holmium laser. If the stones were difficult to reach, a flexible ureteroscope or a needle-assisted technique was used. All the mini-PCNL procedures performed in patients aged <3 years at our center were ultrasound-guided, without the use of fluoroscopy. No major procedure-related complications such as blood loss requiring transfusion, sepsis, or adjacent organ injury were observed. The mean decrease in hemoglobin concentration after the procedure was 8.9 g/L. We believe that the use of ultrasound guidance reduced vessel and other procedure-related injuries including delayed bleeding. In patients with bilateral kidney stones, a second mini-PCNL procedure was performed after 1 month.
However, ultrasonography has some disadvantages, such as inability to monitor the degree of renal tract dilation and hard to find the small stones sometimes. That is one reason why postprocedure imaging examinations showed residual stones in 5 patients. Unlike typical renal stones, most of the melamine-associated stones did not show shadowing on ultrasonography but were characterized by decreased background echoes.[7] Edema of the perirenal tissues due to fluid extravasation increased the difficulty of ultrasound-guided puncture, and repeat procedures were seldom performed at our center. Although many studies have reported on the safety and feasibility of PCNL in adults and children,[23,24] we used a balloon nephrostomy tube in almost all patients to tamponade bleeding and facilitate urine drainage.
This study is limited by its retrospective design with no control group, resulting in selection bias. As most patients were lost to follow-up, data regarding stone recurrence and renal function are unavailable. Melamine-associated stones often cause obstruction at the ureteropelvic junction, and it is important to determine the prognosis in these patients. However, very few studies of ultrasound-guided mini-PCNL in children aged <3 years have previously been reported, and this study presents the largest reported case series from China. We, therefore, consider that our findings can contribute to the development of treatment strategies in pediatric patients with kidney stones.
In conclusion, mini-PCNL can be safely and effectively used for the treatment of patients aged <3 years with various types of upper urinary tract stones. Use of a small-sized channel minimizes parenchymal damage and blood loss during the procedure. Ultrasound-guided mini-PCNL does not expose the patient or physician to radiation, in contrast to fluoroscopy-guided procedures. Vessel and adjacent organ injury can also be avoided by real-time monitoring. However, ultrasound guidance has some disadvantages, such as the inability to monitor the degree of renal tract dilation. However, we considered that ultrasound guidance should be considered as the first-line technique in young children because of its significant advantages.
Footnotes
Edited by: Xin Chen
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Dogan HS, Tekgul S. Management of pediatric stone disease. Curr Urol Rep. 2007;8:163–73. doi: 10.1007/s11934-007-0067-8. [DOI] [PubMed] [Google Scholar]
- 2.Lahme S. Shockwave lithotripsy and endourological stone treatment in children. Urol Res. 2006;34:112–7. doi: 10.1007/s00240-005-0021-5. [DOI] [PubMed] [Google Scholar]
- 3.Hesse A, Kruse R, Geilenkeuser WJ, Schmidt M. Quality control in urinary stone analysis: Results of 44 ring trials (1980-2001) Clin Chem Lab Med. 2005;43:298–303. doi: 10.1515/CCLM.2005.051. [DOI] [PubMed] [Google Scholar]
- 4.Zeng G, Zhao Z, Zhao Z, Yuan J, Wu W, Zhong W. Percutaneous nephrolithotomy in infants: Evaluation of a single-center experience. Urology. 2012;80:408–11. doi: 10.1016/j.urology.2012.04.058. [DOI] [PubMed] [Google Scholar]
- 5.Bodakci MN, Daggülli M, Sancaktutar AA, Söylemez H, Hatipoglu NK, Utangaç MM, et al. Minipercutaneous nephrolithotomy in infants: A single-center experience in an endemic region in Turkey. Urolithiasis. 2014;42:427–33. doi: 10.1007/s00240-014-0677-9. [DOI] [PubMed] [Google Scholar]
- 6.Palmer LS. Pediatric urologic imaging. Urol Clin North Am. 2006;33:409–23. doi: 10.1016/j.ucl.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Guan N, Fan Q, Ding J, Zhao Y, Lu J, Ai Y, et al. Melamine-contaminated powdered formula and urolithiasis in young children. N Engl J Med. 2009;360:1067–74. doi: 10.1056/NEJMoa0809550. [DOI] [PubMed] [Google Scholar]
- 8.Salerno A, Nappo SG, Matarazzo E, De Dominicis M, Caione P. Treatment of pediatric renal stones in a Western country: a changing pattern. J Pediatr Surg. 2013;48:835–9. doi: 10.1016/j.jpedsurg.2012.09.058. [DOI] [PubMed] [Google Scholar]
- 9.Landau EH, Shenfeld OZ, Pode D, Shapiro A, Meretyk S, Katz G, et al. Extracorporeal shock wave lithotripsy in prepubertal children: 22-year experience at a single institution with a single lithotriptor. J Urol. 2009;182(4 Suppl):1835–9. doi: 10.1016/j.juro.2009.04.084. [DOI] [PubMed] [Google Scholar]
- 10.Tan AH, Al-Omar M, Watterson JD, Nott L, Denstedt JD, Razvi H. Results of shockwave lithotripsy for pediatric urolithiasis. J Endourol. 2004;18:527–30. doi: 10.1089/end.2004.18.527. [DOI] [PubMed] [Google Scholar]
- 11.Dave S, Khoury AE, Braga L, Farhat WA. Single-institutional study on role of ureteroscopy and retrograde intrarenal surgery in treatment of pediatric renal calculi. Urology. 2008;72:1018–21. doi: 10.1016/j.urology.2008.03.065. [DOI] [PubMed] [Google Scholar]
- 12.Abu Ghazaleh LA, Shunaigat AN, Budair Z. Retrograde intrarenal lithotripsy for small renal stones in prepubertal children. Saudi J Kidney Dis Transpl. 2011;22:492–6. [PubMed] [Google Scholar]
- 13.Straub M, Gschwend J, Zorn C. Pediatric urolithiasis: The current surgical management. Pediatr Nephrol. 2010;25:1239–44. doi: 10.1007/s00467-009-1394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapoor R, Solanki F, Singhania P, Andankar M, Pathak HR. Safety and efficacy of percutaneous nephrolithotomy in the pediatric population. J Endourol. 2008;22:637–40. doi: 10.1089/end.2007.0254. [DOI] [PubMed] [Google Scholar]
- 15.Etemadian M, Maghsoudi R, Shadpour P, Mokhtari MR, Rezaeimehr B, Shati M. Pediatric percutaneous nephrolithotomy using adult sized instruments: Our experience. Urol J. 2012;9:465–71. [PubMed] [Google Scholar]
- 16.Traxer O, Smith TG, 3rd, Pearle MS, Corwin TS, Saboorian H, Cadeddu JA. Renal parenchymal injury after standard and mini percutaneous nephrostolithotomy. J Urol. 2001;165:1693–5. [PubMed] [Google Scholar]
- 17.Desai MR, Kukreja RA, Patel SH, Bapat SD. Percutaneous nephrolithotomy for complex pediatric renal calculus disease. J Endourol. 2004;18:23–7. doi: 10.1089/089277904322836613. [DOI] [PubMed] [Google Scholar]
- 18.Unsal A, Resorlu B, Kara C, Bozkurt OF, Ozyuvali E. Safety and efficacy of percutaneous nephrolithotomy in infants, preschool age, and older children with different sizes of instruments. Urology. 2010;76:247–52. doi: 10.1016/j.urology.2009.08.087. [DOI] [PubMed] [Google Scholar]
- 19.Kumar R, Anand A, Saxena V, Seth A, Dogra PN, Gupta NP. Safety and efficacy of PCNL for management of staghorn calculi in pediatric patients. J Pediatr Urol. 2011;7:248–51. doi: 10.1016/j.jpurol.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 20.International Commission on Radiological Protection. Free Summary Recommendation. [Last accessed on 2014 Dec 26]. http://www.icrp.org/docs/ICRP_Publication_103-Annals_of_the_ICRP_37(2-4)-Free_extract.pdf .
- 21.Ministry of Health of the People's Republic of China. Medical treatment of infants affected by Sanlu melamine-contaminated milk powder. The Chinese Ministry of Health Bulletin. October 15. 2008. [Last accessed on 2014 Dec 28]. http://www.moh.gov.cn .
- 22.Tzeng BC, Wang CJ, Huang SW, Chang CH. Doppler ultrasound-guided percutaneous nephrolithotomy: A prospective randomized study. Urology. 2011;78:535–9. doi: 10.1016/j.urology.2010.12.037. [DOI] [PubMed] [Google Scholar]
- 23.Choi SW, Kim KS, Kim JH, Park YH, Bae WJ, Hong SH, et al. Totally tubeless versus standard percutaneous nephrolithotomy for renal stones: Analysis of clinical outcomes and cost. J Endourol. 2014;28:1487–94. doi: 10.1089/end.2014.0421. [DOI] [PubMed] [Google Scholar]
- 24.Elderwy AA, Gadelmoula M, Elgammal MA, Osama E, Al-Hazmi H, Hammouda H, et al. Percutaneous nephrolithotomy in children: A preliminary report. Urol Ann. 2014;6:187–91. doi: 10.4103/0974-7796.134255. [DOI] [PMC free article] [PubMed] [Google Scholar]


