Abstract
Background:
Transcatheter occlusion has been applied to treat ostium secundum atrial septal defect (OS ASD) since 1997. During the clinical practice, several postoperative complications including arrhythmia have been reported. This study aimed to evaluate the value of the ratio of atrial septal occluder (ASO) versus atrial septal length (ASL) for predicting arrhythmia occurrence after transcatheter closure in children with OS ASD.
Methods:
Six hundred and fifty-one children diagnosed with OS ASD underwent occlusion procedures after completing routine examinations. The onsets and types of arrhythmia both during and after the occlusion procedures were monitored. Treatments were given based on the individual types of arrhythmia. The binary logistic regression analysis and receiver-operating characteristic (ROC) curve were used in the analysis of value of the ratio of ASO/ASL for predicting postoperative arrhythmia occurrence.
Results:
Transcather occlusions were conducted in 651 children, among whom 7 children had different types and degrees of arrhythmia, with an incidence of 1.1%. The types of arrhythmia included sinus bradycardia, atrial premature beats, bundle branch block, and different degrees of atrioventricular block. Normal electrocardiograph findings were resumed in these 7 patients following active therapies such as corticoids, nutrition, and surgeries. The binary logistic regression and ROC analysis suggested that the ratio of ASO/ASL exhibited an intermediate predictive value for predicting arrhythmia occurrence after occlusion procedures. A cut-off value of 0.576 in the ratio provided a sensitivity of 87.5% and a specificity of 76.2% with an area under the ROC curve of 0.791 (95% confidence intervals, 0.655–0.926; P < 0.05) in predicting arrhythmia occurrence after the closure procedures.
Conclusions:
The ratio of ASO/ASL might be a useful index for predicting arrhythmia occurrence after closure procedures in children with OS ASD.
Keywords: Arrhythmia, Atrial Septal Defect, Atrial Septal Length, Atrial Septal Occluder, Transcatheter Closure
INTRODUCTION
Congenital heart disease (CHD) is a common congenital malformation found in children, with an incidence of 0.6%–0.8%[1] in living infants, among which atrial septal defects (ASDs) are the most common types, demonstrated by its occurrence of 1/1500 in newborns, contributing to 7%–10% of CHD reported in children.[2,3] Ostium secundum (OS) ASD composes 70% of all ASDs, for which the only treatment is surgery. In 1976, King et al.[4] reported the first successful case of percutaneous closure of ASD. With the development of occluder and improvement of procedure techniques, especially the clinical application of Amplatzer atrial septal occluder (ASO) since 1997, closure procedures of OS ASD has been widely applied in clinical practice, featured with advantages of satisfying efficacy, little trauma, quick recovery after surgery, as well as few complications. However, there have been occasional reports of procedure complications due to inappropriate inclusion of cases, unqualified techniques of operators or lack of experience. Arrhythmia is one the most common complications after surgery, which could severely affect the prognosis of children with ASD. The size of ASD, the diameter of ASO as well as the ratio of ASO versus atrial septal length (ASL) are to some extent associated with the incidence of arrhythmia after closure procedure, although no literature regarding the value of the ratio of ASO versus ASL for predicting arrhythmia occurrence after closure procedure have been published till now. Therefore, the present study aimed to analyze the value of the ratio of ASO versus ASL for predicting arrhythmia occurrence after the closure procedure of ASD, which would provide important reference for the closure procedure of ASD in future.
METHODS
Subjects
Six hundred and fifty-one children diagnosed with OS ASD in Department of Pediatric Cardiology, Beijing Anzhen Hospital between January 2003 and December 2013 were enrolled, among which 261 patients were male (40.1%), 390 were female (59.9%), aged between 1 and 18 years old with mean age of 6.9 ± 4.1 years old. All patients underwent closure procedures. Subjects were divided into the case group (presence of arrhythmia after the occlusion) and the control group (no reports of arrhythmia after the occlusion) according to the occurrence of arrhythmia after occlusion procedures, among which 7 cases were defined as the case group (3 males, 4 females, mean age 6.2 ± 4.2 years old), with different types of arrhythmia listed in Table 1. There were 644 patients in the control group, among which 258 were males, 386 females, with a mean age of 7.8 ± 4.3 years old.
Table 1.
Patient's characteristics and arrhythmia after the procedure
| Case number | Sex | Age (years) | ASD (mm) | ASO (mm) | Onset of arrhythmia after the procedure | Types of arrhythmia | ASO/ASL ratio | Treatments |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 7 | 9 | 14 | 4 h | Atrial premature beats | 0.60 | IV administration with 10 mg lidocaine and 2 ml potassium chloride. Normal ECG findings were resumed 2 days after procedure |
| 2 | Male | 9 | 20 | 26 | 1-day | Sinus bradycardia with escape | 0.70 | IV administration of 0.3 mg atropine. Pump administration of 1.5 mg isoprenaline in addition to 3 days continuous treatment of 40 mg/d prednisolone. Normal ECG results were found 3 days after procedure |
| 3 | Female | 13 | 26 | 32 | 1-day | Occasional atrial premature beats | 0.73 | No treatment was given. Symptoms recovered spontaneously |
| 4 | Male | 2 | 18 | 22 | 7 h | Type 2, second-degree AV block (2:1 conduction) | 0.73 | 2 mg dexamethasone and 1 ml/h 0.5 mg isoprenaline. The 10 mg·kg−1·d−1 methylprednisolone was added. 7 days after the occlusion procedure, patient was transferred to undergo surgery. Normal ECG was obtained after surgery |
| 5 | Male | 4 | 14 | 20 | First immediately; second 8 h | Onset of first-degree AV block immediately after procedure, third-degree of AV block 8 h after procedure | 0.63 | 5 mg dexamethasone and 160 mg methylprednisolone were given 8 h after the procedure. 1 mg isoprenaline and corticoids were added to treat third-degree AV block and bradycardia. Then the patient was transferred to undergo surgery. First-degree AV block was observed after surgery, and 10 mg/12 h methylprednisolone was given for 6 days continuously, and sinus rhythm was recovered |
| 6 | Female | 6 | 10 | 20 | 1-day | Frequent atrial premature beats | 0.61 | 20 mg methylprednisolone and myocardium nutrition were administered for 3 days with atrial premature beats decreased |
| 7 | Female | 3 | 11 | 16 | Immediately | Third-degree AV block with junctional escape | 0.63 | 40 mg methylprednisolone and myocardium nutrition were prescribed, and meanwhile the patient was transferred for surgery. 20 mg prednisone per 12 h, 12.5 mg γ-immunoglobulin twice, and myocardium nutrition were used after the surgery. Normal ECG findings were resumed in 22 days |
ASD: Atrial septal defect; ASO: Atrial septal occlude; ASL: Atrial septal length; AV: Atrial ventricular; ECG: Electrocardiograph; IV: Intravenous.
Methods of the procedures
All patients completed routine examinations such as complete blood counts, blood biochemistry, coagulation time, blood gas analysis, hepatic and renal function, a 12-lead electrocardiograph (ECG), chest X-ray, color Doppler echocardiography (the size of ASD and ASL was measured during the examination) after hospitalization. Great artery short axis view, apical four-chamber view, parasternal four chamber view, and subcostal biatrial view were used in measuring the size of the defect. ASL was measured in the apical four chamber view. The same measurement standardization was compiled among different echocardiographers. This study was approved by the Ethics Review Committees of Beijing Anzhen Hospital. All patients were invited for detailed talk regarding the process, possible risks, complications of the closure procedure, and written informed consent was obtained from all patients or the family members.
All patients underwent routine right-heart catheterization via femoral vein approach and appropriate size of the ASO for device closure of ASD was selected under the guidance of transthoracic echocardiography (TTE) and X-ray. The size of the occluder is normally larger than the value detected by TTE by 1–2 mm, approximately equivalent to the longest diameter of ASD visible in multiple sections of TTE, although in the case of lack of interatrial septal rims in the root of aorta, an occluder with a diameter of more than 4–6 mm was also plausible.
Closure procedures were as follows: Catheter was first introduced via right femoral vein, and the guidewire was positioned into the upper left pulmonary vein through the sheath. The long sheath was then delivered into the upper left pulmonary vein or left atrium along the guidewire. ASD closure occluder was placed in the long sheath and was subsequently positioned in the appropriate place under the continuous monitoring of TTE and X-ray. Left to right shunt of ASD disappeared, function of mitral valve, tricuspid valve, and aortic valve were normal, with normal blood flow from the coronary sinus and pulmonary veins. The occluder device was then released, with the sheath removed and pressure bandaging applied. Heparin was given after the procedure at the dose of 0.5 mg for twice. Aspirin was administered orally at the dose of 3–5 mg·kg−1·d−1 for 6 months. Routine prophylaxis with antibiotics against infection was administered for 3 days. TTE and ECG were reexamined at 3 days, 1, 3, and 6 months after the closure procedure. The follow-up period for the whole group of patients was 12.4 ± 3.3 months.
Statistic analysis
All statistical analyses were conducted using the SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Measurement data were expressed as mean ± standard deviation (SD). Student's t-test was used for comparing the mean values of different groups. A P < 0.05 was considered to be statistically significant. Binary logistic regression analysis was used to evaluate the relevance of different factors to the occurrence of postoperative arrhythmia. The dependent variable was the occurrence of postoperative arrhythmia, and the covariates included sex, age, weight, height, the size of ASD, the diameter of ASO, ASL, the ratio of ASO versus ASD, and the ratio of ASO versus ASL. The receiver-operating characteristic (ROC) analysis was performed to evaluate the value of the ratio of ASO versus ASL in predicting arrhythmia occurrence after closure procedures in children with OS ASD. Area under the curve (AUC) represented predictive value of the index. AUC at 0.5–0.7 suggested a low predictive value, 0.7–0.9 an intermediate predictive value, more than 0.9 a high predictive value. P value at 0.5 not included in the 95% confidence interval (CI) of curve area or P < 0.5 suggest that the index exhibits predictive value for the results.[5]
RESULTS
Successful closure procedures were conducted in 651 children diagnosed with OS ASD, among which 7 patients had different degrees of arrhythmia after the procedure. None of these 7 patients had arrhythmia before the occlusion procedure. All the 7 patients with postoperative arrhythmia were under careful 24 h ECG monitoring until ECG went back normal. The arrhythmias were resolved after active and reasonable therapy, with minimized adverse events. The types and therapies for arrhythmia were listed in Table 1. There was no significant difference of age between the case group and the control group (6.9 ± 4.1 vs. 7.8 ± 4.3, t = 0.231, P > 0.05). In addition, no difference of sexuality, height, weight was found between the case group and the control group (P > 0.05).
Binary logistic regression analysis was performed to define the relevance of different factors to the occurrence of postoperative arrhythmia, including gender, age, weight, height, the size of ASD, the diameter of ASO, ASL, the ratio of ASO versus ASD, and the ratio of ASO versus ASL. According to the results, among all the factors, the ratio of ASO versus ASL was the relevant factor to predict arrhythmia occurrence with statistically significance and introduced into the equation, which indicated that the ratio of ASO/ASL was an influence factor to the occurrence of postoperative arrhythmia. While other covariates were not introduced in the equation as P > 0.05.
Receiver-operating characteristic analysis was performed to evaluate the value of the ratio of the ASO versus ASL in the prediction of arrhythmia occurrence after closure procedures. As shown in the result of ROC curve, a cut-off value of 0.576 in the ratio of ASO versus ASL provided a sensitivity of 87.5% and a specificity of 76.2%, demonstrating the good predictive effects for arrhythmia [Figure 1]. And the AUC was 0.791 (95% CI: 0.655–0.926, P < 0.05), suggesting that the ratio of ASO versus ASL had an intermediate predictive value in the prediction of arrhythmia occurrence after closure procedures.
Figure 1.
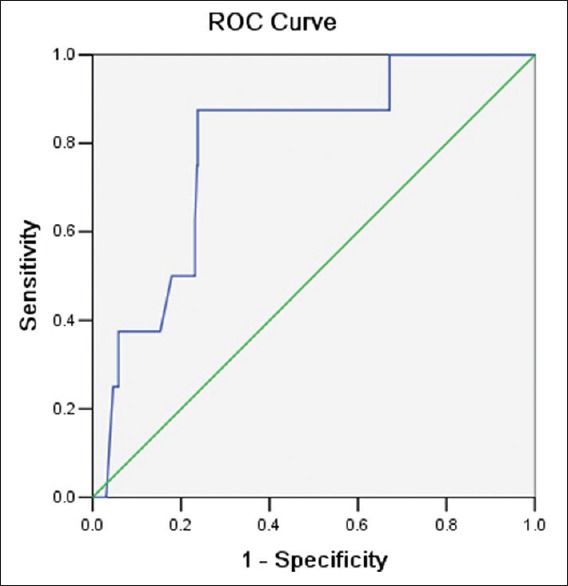
Receiver-operating characteristic curve of value of the ratio of atrial septal occluder (ASO) versus atrial septal length (ASL) for predicting arrhythmia occurrence after occlusion procedures in children with ostium secundum atrial septal defect. The longitudinal axis represented the sensitivity of different ratio of ASO versus ASL for the prediction. The transversal axis represented the false positive rate (1-specificity) of the prediction. The 45° green line of this graph stood for reference line, representing the sensitivity being equal to false positive rate. The blue curve was farther from the reference line and nearer the upper left corner of the graph. Area under the curve was 0.791 (95% confidence interval 0.655–0.926, P = 0.01).
DISCUSSION
Atrial septal defect is one of the most common types of CHD,[3] and is often treated with surgeries or device closure procedures. Compared with surgery closures, device closures demonstrate advantages of little trauma, quick recovery after the procedures as well as less complications. Nevertheless, under the situation of inappropriate case inclusion, poor standards of operation, or lack of therapy experience, few complications after device closure procedures might occur, among which arrhythmia is often reported. By far, there have been a few literature reporting the arrhythmia after transcatheter closure procedures in patients with ASD.[6,7] The common types of arrhythmia reported include sinus bradycardia, supraventricular tachycardia, atrial premature beats, atrial ventricular (AV) block, and atrial fibrillation. In 2014, Komar et al.[8] conducted a study in 235 ASD patients underwent device closure procedures and found that after the device closure procedure, 8 patients (3.4%) had supraventricular tachycardia, 3 patients (1.3%) had bradycardia. In 2013, Chantepie et al.[9] reported a complete AV block after the device closure procedure in a 13-year-old patient with ASD. Knepp et al.[10] reported in 2010 that in the follow-up study of 94 patients with ASD, who underwent ASD device closure procedures, 7 patients had onsets of arrhythmia such as supraventricular tachycardia, atrial fibrillation, and ventricular premature beats. Moreover, another 23 cases of ASD patients with device closure procedures demonstrated that after the procedure, 5 patients had atrial rhythm, 2 patients had atrial premature beats, 1 patient had ventricular premature beats, as reported in 2003 by Hessling et al.[11] A few studies have discussed the causes of arrhythmia after transcatheter closure procedures in patients with ASD. In 2014, Wang et al.[12] discovered that risk factors for AV block after device closure procedures in children with ASD included small age, long diameter of ASD as well as long diameter of ASO, in addition to D0/Ds ≥ 0.45. Furthermore, Komar et al.[8] published in 2014 that long diameter of occluder and prolonged procedure duration were risk factors for increased incidence of supraventricular arrhythmia after occlusion procedures. In addition, Chantepie et al.[9] discovered in 2013 that placement of large occlusion device in young children was a risk factor for arrhythmia after occlusion procedures. The predisposing factors of arrhythmia after ASD closure procedures might be associated with anatomic structures. ASD and Koch triangle are closely positioned anatomically, while AV node is in the endocardium in front of Koch triangle, thus the AV node might be damaged during the closure procedure or be compromised mechanically by the occluder device. Hill et al.[13] reported ASD closure procedure as a predisposing factor for supraventricular ectopic rhythm, in addition to AV conduction abnormality, the possible mechanisms of which might involve that occluder disc posed a pressure on AV node, resulting in the friction and temporary swelling of AV node and the surrounding tissues, which subsequently led to AV node dysfunction or decrease in function. To a certain degree, the diameter of ASO is decided by the size of ASD. And if the ratio of ASO versus ASL increases, the rim of occluder, especially the inferior rim, might have a higher potential risk in contacting the Koch triangle, which might subsequently increase friction between occluder and AV node as well as tissues surrounded, resulting in tissue swelling, AV node functional disorders, and eventually arrhythmia.
The present study demonstrated that among the 651 ASD patients underwent device closure procedures, 7 patients had different degrees of arrhythmia, with an incidence of 1.1%. Types of arrhythmia include sinus bradycardia, atrial premature beats, bundle block, and different degrees of AV block. With active therapies of corticoids, myocardium nutrition, and surgeries, ECG of the 7 patients resumed normal. ROC analysis was used to assess the ratio of ASO versus ASL in predicting arrhythmia occurrence after closure procedures in children with OS ASD. Results suggested that the ratio of ASO versus ASL showed an intermediate value in predicting arrhythmia occurrence after closure procedures. Suda et al.[14] observed that with the use of Amplatzer ASD occluder, there were different degrees of AV block 1–7 days after closure, composing an incidence of 6.1%. However, almost all patients with AV block after closure had a complete recovery 1–6 months after the closure. According to the result of our analysis, it is essential that an occluder with the appropriate size is positioned, especially for younger patients, because of their ASL is not as long as the teenager of adult patients. And the placement of occluders during the closure procedure have to be gentle, since some inappropriate operation could cause mechanical stretch stimulus or friction to the sinus node and AV node, thus triggers the arrhythmia during and after the closure procedure. Careful ECG monitoring against AV block is also necessary.
However, in 2013, Al Akhfash et al.[15] reported a case of 7 years old ASD patient who underwent device closure procedures and developed second-degree AV block immediately after the procedure. Patient was subjected to 3 days treatment with corticoids and close monitoring. ECG with sinus rhythm was obtained 7 days after the closure. In our study, ECG with sinus rhythm was recovered in all arrhythmia patients with active therapies of medications or surgeries, suggesting that early and active therapy intervention is essential for the prognosis of arrhythmia after ASD device closure.
In conclusion, our study suggested that closure procedures demonstrated good efficiency and safety in patients diagnosed with OS ASD, with low incidence of arrhythmia. However, patients with ratio of ASO versus ASL larger than 0.576 might have a higher potential risk of arrhythmia during and after the procedure, but with careful monitoring, timely check-up of ECG, immediate and appropriate treatment, most patients could possess a good prognosis. Meanwhile, we found that the ratio of ASO versus ASL exhibited an intermediate value in predicting arrhythmia occurrence after occlusion procedures. Since only 7 of 651 cases had postoperative arrhythmia in our study, with limited number of cases in the case group as well as single-center research, thus a large-sample, multi-center clinical study would facilitate better predictive values.
Footnotes
Edited by: Xin Chen
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Menacker F, Martin JA. Expanded health data from the new birth certificate, 2005. Natl Vital Stat Rep. 2008;56:1–24. [PubMed] [Google Scholar]
- 2.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 3.Kazmouz S, Kenny D, Cao QL, Kavinsky CJ, Hijazi ZM. Transcatheter closure of secundum atrial septal defects. J Invasive Cardiol. 2013;25:257–64. [PubMed] [Google Scholar]
- 4.King TD, Thompson SL, Steiner C, Mills NL. Secundum atrial septal defect. Nonoperative closure during cardiac catheterization. JAMA. 1976;235:2506–9. [PubMed] [Google Scholar]
- 5.Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–93. doi: 10.1126/science.3287615. [DOI] [PubMed] [Google Scholar]
- 6.Chessa M, Carminati M, Butera G, Bini RM, Drago M, Rosti L, et al. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol. 2002;39:1061–5. doi: 10.1016/s0735-1097(02)01711-4. [DOI] [PubMed] [Google Scholar]
- 7.Johnson JN, Marquardt ML, Ackerman MJ, Asirvatham SJ, Reeder GS, Cabalka AK, et al. Electrocardiographic changes and arrhythmias following percutaneous atrial septal defect and patent foramen ovale device closure. Catheter Cardiovasc Interv. 2011;78:254–61. doi: 10.1002/ccd.23028. [DOI] [PubMed] [Google Scholar]
- 8.Komar M, Przewlocki T, Olszowska M, Sobien B, Stepniewski J, Podolec J, et al. Conduction abnormality and arrhythmia after transcatheter closure of atrial septal defect. Circ J. 2014;78:2415–21. [PubMed] [Google Scholar]
- 9.Chantepie A, Lefort B, Soulé N, Bonnefoy R, Labarthe F. Atrioventricular block after transcatheter atrial septal defect closure using the Amplatzer septal occluder(®) Arch Pediatr. 2013;20:1333–6. doi: 10.1016/j.arcped.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 10.Knepp MD, Rocchini AP, Lloyd TR, Aiyagari RM. Long-term follow up of secundum atrial septal defect closure with the amplatzer septal occluder. Congenit Heart Dis. 2010;5:32–7. doi: 10.1111/j.1747-0803.2009.00358.x. [DOI] [PubMed] [Google Scholar]
- 11.Hessling G, Hyca S, Brockmeier K, Ulmer HE. Cardiac dysrhythmias in pediatric patients before and 1 year after transcatheter closure of atrial septal defects using the amplatzer septal occluder. Pediatr Cardiol. 2003;24:259–62. doi: 10.1007/s00246-002-0247-8. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Hua Y, Li L, Wang X, Qiao L, Shi X, et al. Risk factors and prognosis of atrioventricular block after atrial septum defect closure using the Amplatzer device. Pediatr Cardiol. 2014;35:550–5. doi: 10.1007/s00246-013-0822-1. [DOI] [PubMed] [Google Scholar]
- 13.Hill SL, Berul CI, Patel HT, Rhodes J, Supran SE, Cao QL, et al. Early ECG abnormalities associated with transcatheter closure of atrial septal defects using the Amplatzer septal occluder. J Interv Card Electrophysiol. 2000;4:469–74. doi: 10.1023/a:1009852312907. [DOI] [PubMed] [Google Scholar]
- 14.Suda K, Raboisson MJ, Piette E, Dahdah NS, Miró J. Reversible atrioventricular block associated with closure of atrial septal defects using the Amplatzer device. J Am Coll Cardiol. 2004;43:1677–82. doi: 10.1016/j.jacc.2003.12.042. [DOI] [PubMed] [Google Scholar]
- 15.Al Akhfash AA, Al-Mesned A, Fayadh MA. Amplatzer septal occluder and atrioventricular block: A case report and literature review. J Saudi Heart Assoc. 2013;25:91–4. doi: 10.1016/j.jsha.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


