Abstract
Background:
There are few studies for evaluating wall characteristics of intracranial vertebral artery hypoplasia (VAH). The aim of this study was to determine wall characteristics of VAH with three-dimensional volumetric isotropic turbo spin echo acquisition (3D VISTA) images and differentiate between acquired atherosclerotic stenosis and VAH.
Methods:
Thirty patients with suspicious VAH by luminograms were retrospectively enrolled between January 2014 and February 2015. The patients were classified as “acquired atherosclerotic stenosis” or “VAH” based on 3D VISTA images. The wall characteristics of VAH were assessed to determine the presence of atherosclerotic lesions, and the patients were classified into two subgroups (VAH with atherosclerosis and VAH with normal wall). Wall characteristics of basilar arteries and vertebral arteries were also assessed. The clinical and wall characteristics were compared between the two groups.
Results:
Five of 30 patients with suspicious VAH were finally diagnosed as acquired atherosclerotic stenosis by 3D VISTA images. 25 patients were finally diagnosed as VAH including 16 (64.00%) patients with atherosclerosis and 9 (36.00%) patients with normal wall. In the 16 patients with atherosclerosis, plaque was found in 9 patients, slight wall thickening in 6 patients, and thrombus and wall thickening in 1 patient. Compared with VAH patients with normal wall, VAH patients with atherosclerosis showed atherosclerotic basilar arteries and dominant vertebral arteries more frequently (P = 0.000).
Conclusions:
Three-dimensional VISTA images enable differentiation between the acquired atherosclerotic stenosis and VAH. VAH was also prone to atherosclerotic processes.
Keywords: Atherosclerosis, High Resolution Magnetic Resonance Images, Vertebral Artery Hypoplasia
INTRODUCTION
Congenital anatomical variations of both vertebral arteries are relatively frequent.[1,2] Vertebral artery hypoplasia (VAH) has not yet been considered an independent risk factor for ischemic stroke, given the high prevalence of asymmetrical vertebral artery in population and absence of vertebral insufficiency symptoms among people with VAH.[1,2] However, more and more studies showed ipsilateral VAH were common in patients with posterior circulation stroke, suggesting patients with VAH might at an increased risk of ischemic stroke.[3,4,5,6]
To determine the relationship of VAH and ischemic stroke, VAH should be differentiated from acquired stenosis accurately at first. The differential diagnosis between VAH and stenosis might be difficult by the luminal imaging including digital subtract angiography (DSA), computer tomography angiography (CTA), and magnetic resonance angiography (MRA), as they only provide information on the luminal flow but not the morphological characteristics of vessel wall.[7,8,9,10,11] However, similar luminograms might reflect various underlying arterial wall lesions. Knowledge of wall characteristics will help further elucidate the mechanism of ischemic stroke in VAH patients.
High resolution magnetic resonance images (HR MRI) is emerging as a new technique for assessing wall characteristics of intracranial arteries, and has been used to investigate vessel remodeling pattern, plaque distribution and percent plaque area in recent years.[12,13,14,15] By using two-dimensional (2D) high resolution MRI, Mariani et al. reported a case in which hypoplastic basilar artery was differentiated from atherosclerotic stenosis.[10] Compared with 2D imaging method, three-dimensional (3D) imaging method could offer isotropic resolution and enable a comprehensive survey of intracranial arteries with multiple planar reconstructions.[16,17] In addition, compared with the extracranial VAH which have been investigated with ultrasonography or DSA, the intracranial VAH was given less attention. In this study, our aim was to determine wall characteristics of VAH with 3D volumetric isotropic turbo spin echo acquisition (3D VISTA) images and differentiate between acquired atherosclerotic stenosis and VAH.
METHODS
Patients
We retrospectively reviewed our single institutional HR MRI database in the digital picture archiving and communication system from June 2014 to February 2015. Images with 3D time-of-flight (TOF) MRA were initially evaluated, and suspicious VAH was defined as a lumen diameter of ≤2 mm, and the larger contralateral side was defined as a dominant vertebral artery according previous study.[5] Patients would be excluded from this study if the lumen diameter of both vertebral arteries were ≤2 mm. When diagnosis was obscure by MRA, CTA or DSA was additionally used. All the patients with unilateral intracranial VAH suggested by luminograms were included. Image quality of VISTA images was assessed using a previously developed four-point scale (1=poor, 2=adequate, 3=good, 4=excellent).[18] Images with poor quality were finally excluded from this study.
The atherosclerotic risk factors were noted including hypertension, hyperlipidemia, diabetes mellitus, smoking history and obesity.[12,13] Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or the patients are currently treated with an antihypertensive drug. Hyperlipidemia was defined as a total cholesterol level ≥240 mg/dl or low-density lipoprotein cholesterol level ≥160 mg/dl or receiving lipid-lowering treatment. Diabetes mellitus was defined as glycosylated hemoglobin ≥7% or being treated with antidiabetic medications. Patients with smoking history or who currently smoke were considered to be smokers. Obesity was defined as ≥30 kg/m2 of body mass index. The hospital ethics committee approved this study and all patients signed a written consent.
High resolution magnetic resonance imaging protocol
A 3 T MR scanner (Ingenia; Philips Healthcare, Best, The Netherlands) with a 15-channel phased-array head coil was used in this study. 3D VISTA images were acquired in a traversal plane to cover the major intracranial arteries identified on the 3D TOF MRA. Imaging parameters of 3D VISTA were as follows: Repetition time/echo time = 1300 ms/36 ms, field of view = 140 mm × 200 mm × 105 mm, matrix = 280 × 332 × 210, number of excitation = 2. Acquisition voxel volume was 0.5 mm × 0.6 mm × 0.5 mm, reconstruction voxel volume was 0.5 mm × 0.5 mm × 0.5 mm. The coronal and axial cross-sections were reconstructed with 0.5 mm slice thickness.
Assessment of intracranial vertebral artery
Two experienced readers who were blinded to clinical data assessed VISTA images by visual inspection. The differences between two observers were solved by consensus. Based on VISTA images, acquired atherosclerotic stenosis was distinguished from VAH firstly when wall thickening (with or without thrombus) was found in the suspicious VAH, and outer vessel diameter was more than 50% of the dominant vertebral artery. Then, the VAH patients were classified as two subgroups: (1) “VAH with atherosclerosis” when VISTA images showed slim lumen with vessel wall thickening in the hypoplastic vertebral artery, but outer vessel diameter ≤50% of dominant vertebral artery. The wall characteristics were described as atherosclerotic plaque or slight wall thickening. (2) “VAH with normal wall” when VISTA images showed slim lumen without vessel wall thickening in the hypoplastic vertebral artery.
The wall characteristics of basilar arteries and dominant vertebral arteries were also assessed and categorized as “atherosclerosis” or “normal.” The clinical and wall characteristics were compared between the VAH patients with atherosclerosis and VAH patients with normal wall [Table 1].
Table 1.
Demographic and clinical characteristics of VAH patients
| Characteristics | VAH | P | ||
|---|---|---|---|---|
| Total (n = 25) | Atherosclerosis (n = 16) | Normal wall (n = 9) | ||
| Age (years), mean ± SD | 60.44 ± 10.24 | 61.31 ± 10.45 | 58.89 ± 10.25 | 0.581 |
| Men, n (%) | 23 (92.00) | 15 (93.75) | 8 (88.89) | 1.000 |
| Hypertension, n (%) | 21 (84.00) | 15 (93.75) | 6 (66.67) | 0.116 |
| Hyperlipidemia, n (%) | 16 (64.00) | 11 (68.75) | 5 (55.56) | 0.671 |
| Diabetes mellitus, n (%) | 11 (44.00) | 7 (43.75) | 4 (44.44) | 1.000 |
| Smoking, n (%) | 14 (56.00) | 9 (56.25) | 5 (55.56) | 1.000 |
| Obesity, n (%) | 2 (8.00) | 2 (12.50) | 0 | 0.520 |
| Number of risk factors, n (%) | ||||
| 1 | 5 (20.00) | 2 (12.50) | 3 (33.33) | 0.373 |
| 2 | 5 (20.00) | 4 (25.00) | 1 (11.11) | |
| 3 | 12 (48.00) | 7 (43.75) | 5 (55.56) | |
| 4 | 3 (12.00) | 3 (18.75) | 0 | |
| Atherosclerotic basilar artery, n (%) | 15 (60.00) | 14 (87.50) | 1 (11.11) | 0.000 |
| Atherosclerotic dominant vertebral artery, n (%) | 12 (48.00) | 12 (75.00) | 0 | 0.000 |
SD: Standard deviation; VAH: Vertebral artery hypoplasia.
Statistical analysis
Continuous variable (age) was assessed for normality by the Kolmogorov–Smirnov test. The normally distributed continuous variable was summarized as mean ± standard deviation. Categorical variables such as male sex and risk factors were presented as percentages. Fisher exact test (for percentages) was used to compare categorical variables. SPSS 11.5 (SPSS, Inc., Chicago, IL, USA) was used as the statistical analysis software. All reported P values were two-sided, and P < 0.05 were considered significance.
RESULTS
Patient characteristics
Between June 2014 and February 2015, a total of 30 patients (male: 26; female: 4) with suspicious intracranial VAH were enrolled. The mean age was 59.90 ± 9.56 years. The atherosclerotic risk factors included hypertension (n = 22, 73.33%), hyperlipidemia (n = 20, 66.67%), Diabetes mellitus (n = 15, 50.00%), smoking (n = 15, 50.00%), and obesity (n = 3, 10.00%). The number of atherosclerotic risk factors in the patients was 1 (n = 5, 16.67%), 2 (n = 7, 23.33%), 3 (n = 14, 46.67%) or 4 (n = 4, 13.33%) atherosclerosis risk factors, respectively.
Acquired atherosclerotic stenosis of intracranial vertebral artery
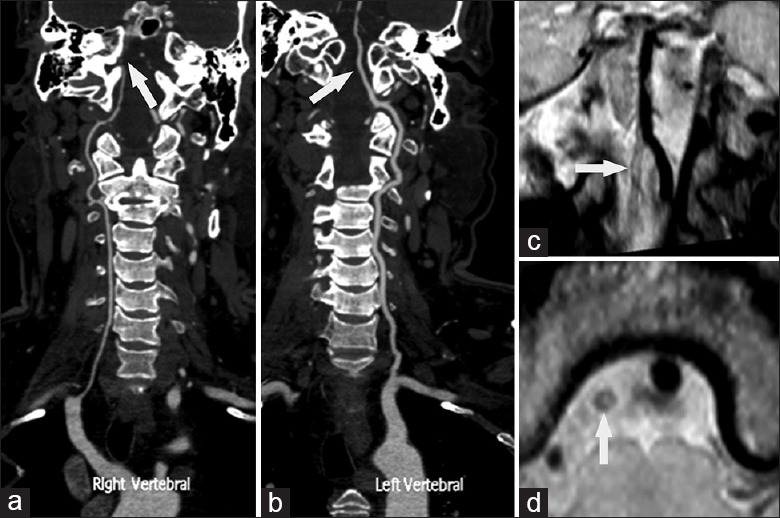
Five of the 30 patients with possible unilateral intracranial VAH suggested by luminograms were finally diagnosed as acquired atheroslcerotic stenosis due to the presence of atherosclerotic plaque with similar vessel outer diameter as the dominant verterbral arteries on the HR MRI. For the 5 patients, MRA findings were suspicious for VAH in the left side (3 cases) or right sides (2 cases). Further study with CTA or DSA also showed slim lumen in the vertebral arteries, suggesting intracranial VAH. However, HR MRI depicted atherosclerotic plaques and large thrombi (2 cases) [Figure 1] in those patients, and the outer diameter was similar with the dominant sides, suggesting acquired atheroslcerotic stenosis.
Figure 1.
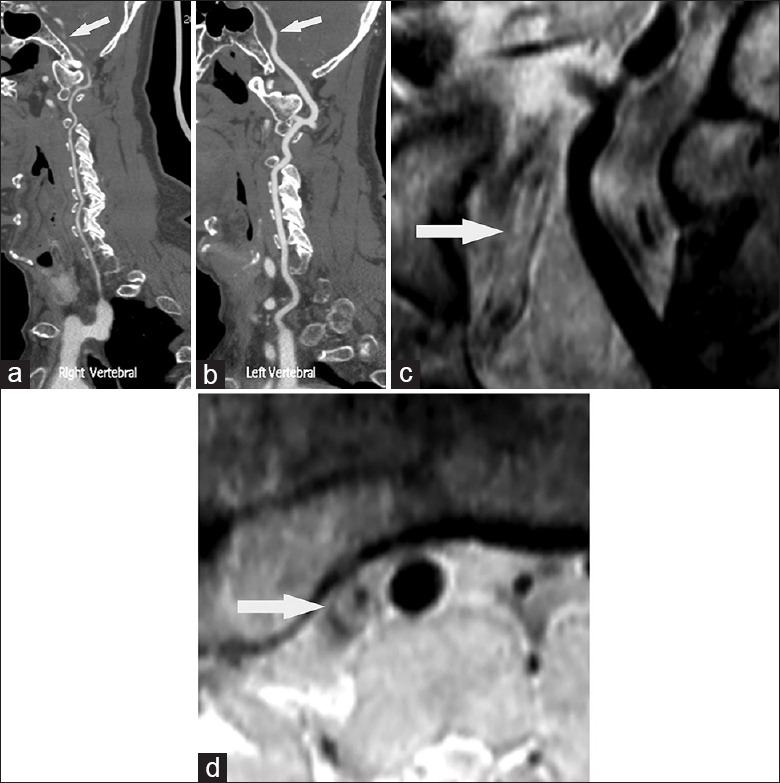
Computer tomography angiography suggested right vertebral artery hypoplasia (a, arrow). The left vertebral artery (VA) was the dominant one (b arrow). Coronal and axil reconstructed views of high resolution magnetic resonance images (HR MRI) showed a large thrombus leading to lumen occlusion in the middle portion (c, arrow) and eccentric plaque in the distal portion of intracranial VA (d, arrow). This case was diagnosed as acquired atherosclerotic stenosis since HR MRI showed similar outer vessel diameter in the right VA as that in the left VA.
Wall characteristics of vertebral artery hypoplasia
Twenty-five patients (left side: 8 cases; right side: 17 cases) were finally diagnosed as VAH. In the 25 patients, HR MRI showed a slim lumen and the outer vessel diameters were equal or less than 50% of the dominant vertebral arteries. Of the 25 VAH patients, HR MRI showed normal wall in 9 patients [Figure 2] and atherosclerosis in 16 patients including little atherosclerotic plaque in 9 patients [Figure 3], slight wall thickening in 6 patients [Figure 4], and thrombus and wall thickening in 1 patient [Figure 5].
Figure 2.
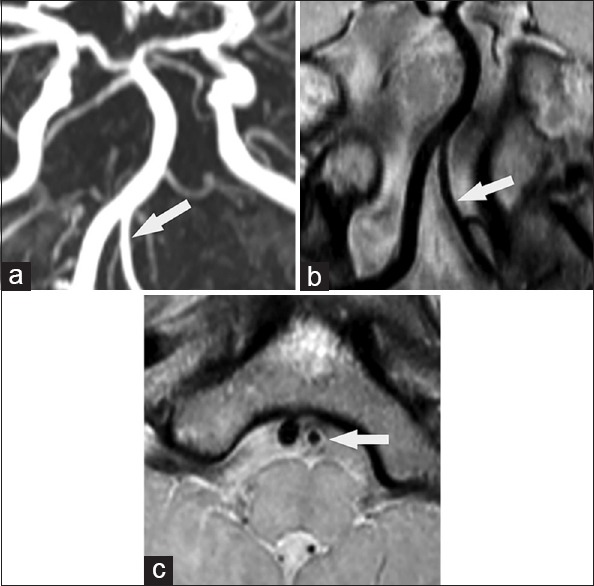
Magnetic resonance angiography suggested left vertebral artery hypoplasia (VAH) (a, arrow). High resolution magnetic resonance images with coronal (b, arrow) and axil (c, arrow) reconstructed image showed slim lumen with normal wall. This case was finally diagnosed as VAH with normal wall.
Figure 3.
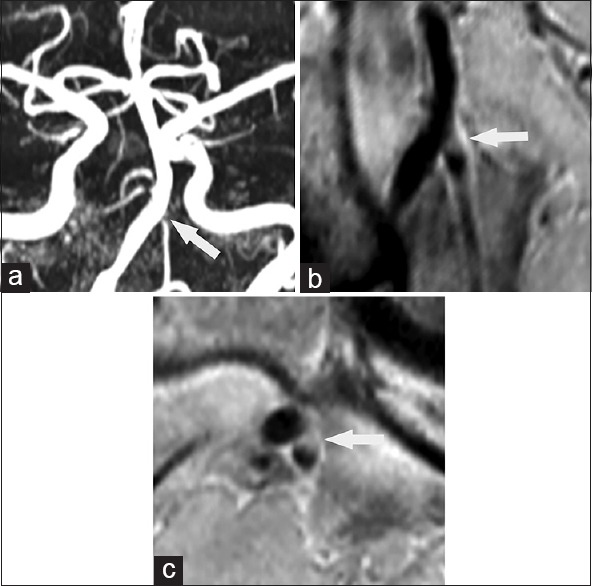
Magnetic resonance angiography was suspicious of vertebral artery hypoplasia (VAH) in the left side with severe stenosis in the terminus (a, arrow). High resolution magnetic resonance images with coronal (b, arrow) and axil (c, arrow) reconstructed images showed slim lumen with obvious eccentric plaque in the terminus. The case was diagnosed as VAH with atherosclerosis.
Figure 4.
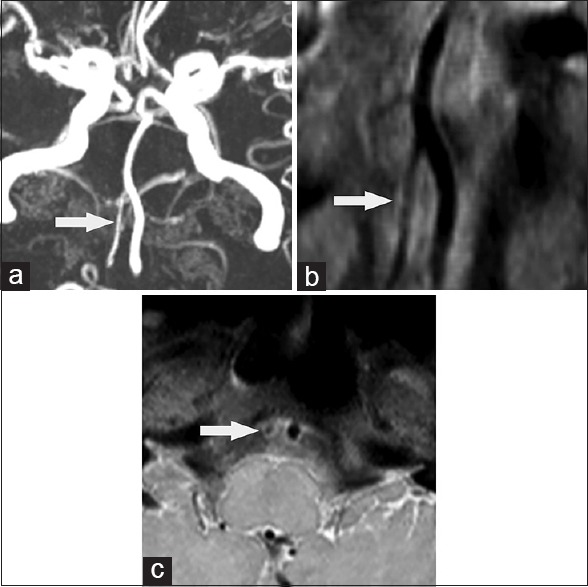
Magnetic resonance angiography was suspicious of right vertebral artery hypoplasia (VAH) (a, arrow). Coronal (b, arrow) and axil (c, arrow) reconstructed views of high resolution magnetic resonance images showed slim lumen with slight vessel wall thickening. The case was also diagnosed as VAH with atherosclerosis.
Figure 5.
Computer tomography angiography suggested right vertebral artery hypoplasia (VAH) with absence of lumen in the distal portion of intracranial vertebral artery (VA) (a arrow). The left VA was dominant side (b arrow). Coronal (c arrow) and axil (d, arrow) reconstructed views of high resolution magnetic resonance images showed wall thickening with a large thrombus leading to lumen occlusion in the distal portion of intracranial VA. High resolution magnetic resonance images showed outer vessel diameter in the right VA was less than 50% of the left VA. This case was diagnosed as VAH with atherosclerosis and thrombus.
Atherosclerotic basilar arteries and atherosclerotic dominant intracranial vertebral arteries were found in 15 (60%) and 12 (48%) of 25 patients, respectively. Compared with the VAH patients with normal wall, VAH patients with atherosclerosis showed atherosclerotic basilar arteries and dominant vertebral arteries more frequently (P = 0.000). No significant difference was found in the sex, age and atherosclerotic risk factors between the two groups [Table 1].
DISCUSSION
Vertebral artery hypoplasia is not rare in the normal population. Although there is no clear definition of VAH, it was generally defined when the diameter of hypoplastic vertebral artery was less than 2 mm,[5] or less than 3 mm[19] or there was a difference between the lateral and contralateral vessel with an asymmetry ratio of equal or greater than 1:1.7 on the luminograms.[20] The reported frequency of VAH is from 1.9% to 10% depending on the various definitions used for VAH.[1,2,19,20]
The association between VAH and ischemic events was controversial. To investigate the clinical relevance of VAH, acquired atherosclerotic stenosis should be distinguished and excluded from VAH group firstly. However, intracranial vertebral artery atherosclerotic stenosis was also popular and has similar luminogram as intracranial VAH. In the New England Medical Center Posterior Circulation Registry study, severe stenosis or occlusion of the intracranial vertebral artery was the most common arterial lesion,[21,22] and the most common pathological processes are atherosclerosis. The atherosclerotic intracranial vertebral artery was an important recipient site and common source of emboli. Undoubtedly, the results would be misinterpreted if the patients with intracranial vertebral artery atherosclerotic stenosis were included in VAH studies, and the conclusion for clinical relevance of VAH might be somewhat biased. Differentiation between congenital VAH and acquired atherosclerotic stenosis is difficult since it generally relies on the luminography including MRA, CTA or DSA.[7,8,9,10,11] None of these techniques could provide the precise morphology of the vessel wall of intracranial artery. HR MRI can directly visualize the arterial wall, permit identification of atherosclerotic plaques,[12,13] and help differentiate between acquired atherosclerotic stenosis and VAH.[10] The differentiation has another clinical significance since endovascular treatment is emerging as a valuable tool for patients refractory to medical therapy.[23,24] The complications might be unavoidable if VAH patients were misdiagnosed as atherosclerotic stenosis and received endovascular therapy.
The mechanism of ischemic stroke in patients with VAH is still not completely clear. Previous studies showed VAH seemed to be more prone to pro-thrombotic or atherosclerotic processes than normal or dominant vertebral arteries, and speculated the VAH-related ischemic stroke was still due to large artery atherosclerosis.[1,25] Posterior circulation ischemic stroke might result from atherosclerotic lesions in hypoplastic vertebral arteries because vertebral arterial atherosclerosis (with or without thrombi) can cause in situ strokes and are prone to cause distal embolization. Atherosclerotic VAH was found in most of patients in our study, providing another evidence for the mechanism of ischemic stroke. Furthermore, compared with normal or dominant vertebral arteries, VAH with atherosclerosis might be more vulnerable to severe stenosis or occlusion due to the smaller caliber. Caplan[26] had described similar finding that the smaller of paired arteries were more prone to occlusion. Severe stenosis or occlusion would aggravate the flow volume reduction in VAH, which might be another important mechanism of ischemic stroke in VAH patients. MRA could not provide precise information of atherosclerotic lesions for intracranial VAH. Although CTA is recognized as a good method to depict carotid plaques, the value for detecting the atherosclerotic lesions in the intracranial vertebral arteries seemed to be limited.[10] Direct wall imaging not only permits HR MRI providing a confirmative diagnosis of VAH, but also helps evaluate the atherosclerotic processes of intracranial VAH. Knowledge of the wall characteristics would help further understanding the role of VAH in the posterior circulation ischemic stroke.
Three-dimensional VISTA sequence is a new method introduced recently with high-isotropic resolution and large volume coverage for intracranial arteries.[16] By using this 3D volume acquisition, all the vertebral arteries could be assessed globally with multi-planar reconstructed images including the coronal and axil plane images as described in this study. This feature was very important for evaluation of tortuous intracranial vertebral arteries, which was difficult in the 2D image acquisition.[16] Recently, other magnetic resonance techniques, such as True Fast Imaging in Steady State Precession[7] or basiparallel anatomic scanning-MRI[8,9] were introduced to differentiate arterial occlusion from vertebral hypoplastic variants. However, such sequences still focused on the luminogram rather than the arterial wall, and could not clearly depict atherosclerotic lesions with excellent quality images, especially for VAH.
Our study has several limitations. First, the study population was small because only the patients with HR MRI were included, and the retrospective study might have selection bias. However, our findings are still important for understanding the mechanism of ischemic stroke in VAH patients. Secondly, we did not assess the relationship between the VAH and ischemic events. A larger cohort study with follow-up will be performed to assess the clinical relevance of VAH in the future. Thirdly, although 3D VISTA could provide good excellent quality images for assessing intracranial larger arteries including middle cerebral artery and basilar artery, the resolution should be further improved for the hypoplastic vertebral artery due to the smaller caliber. In addition, we only perform the HR MRI for the intracranial arteries, and the intracranial segment did not represent the entire vertebral artery.
In conclusion, HR MRI with 3D VISTA sequence was able to help differentiate between VAH and acquired atherosclerotic stenosis. In addition, hypoplastic vertebral arteries were also prone to atherosclerosis or thrombus, resulting in severe stenosis or occlusion. This finding might be very important for determining the clinical relevance of VAH.
Footnotes
Edited by: Yi Cui
Source of Support: This study was supported by grants from China Postdoctoral Science Foundation (No. 2014M562633), China-Japan Friendship Hospital Youth Science and Technology Excellence Project (No. 2014-QNYC-A-04), National Natural Science Foundation of China (No. 81173595, 30670731, 81070925, and 81471767), and National Basic Research Program (973 Program) of China (No. 2013CB733805).
Conflict of Interest: None declared.
REFERENCES
- 1.Katsanos AH, Kosmidou M, Kyritsis AP, Giannopoulos S. Is vertebral artery hypoplasia a predisposing factor for posterior circulation cerebral ischemic events? A comprehensive review. Eur Neurol. 2013;70:78–83. doi: 10.1159/000351786. [DOI] [PubMed] [Google Scholar]
- 2.Chuang YM, Chan L, Wu HM, Lee SP, Chu YT. The clinical relevance of vertebral artery hypoplasia. Acta Neurol Taiwan. 2012;21:1–7. [PubMed] [Google Scholar]
- 3.Szárazová AS, Bartels E, Bartels S, Turčáni P. Possible morphological pathomechanisms of ischemic stroke in the posterior circulation of patients with vertebral artery hypoplasia. J Neuroimaging. 2015;25:408–14. doi: 10.1111/jon.12137. [DOI] [PubMed] [Google Scholar]
- 4.Chuang YM, Huang YC, Hu HH, Yang CY. Toward a further elucidation: Role of vertebral artery hypoplasia in acute ischemic stroke. Eur Neurol. 2006;55:193–7. doi: 10.1159/000093868. [DOI] [PubMed] [Google Scholar]
- 5.Park JH, Kim JM, Roh JK. Hypoplastic vertebral artery: Frequency and associations with ischaemic stroke territory. J Neurol Neurosurg Psychiatry. 2007;78:954–8. doi: 10.1136/jnnp.2006.105767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu XY, Li ZX, Liu HQ, Zhang M, Wei ML, Fang S, et al. Relationship between vertebral artery hypoplasia and posterior circulation stroke in Chinese patients. Neuroradiology. 2013;55:291–5. doi: 10.1007/s00234-012-1112-y. [DOI] [PubMed] [Google Scholar]
- 7.Freund W, Kassubek J, Aschoff AJ, Huber R. MRI-based separation of congenital and acquired vertebrobasilar artery anomalies in ischemic stroke of the posterior circulation. Stroke. 2008;39:2382–4. doi: 10.1161/STROKEAHA.107.512772. [DOI] [PubMed] [Google Scholar]
- 8.Nagahata M, Abe Y, Ono S, Hosoya T, Uno S. Surface appearance of the vertebrobasilar artery revealed on basiparallel anatomic scanning (BPAS)-MR imaging: Its role for brain MR examination. AJNR Am J Neuroradiol. 2005;26:2508–13. [PMC free article] [PubMed] [Google Scholar]
- 9.Morimoto K, Nagahata M, Ono S, Miura H, Tsushima F, Seino H, et al. Incidence of unilateral distal vertebral artery aplasia: Evaluation by combining basiparallel anatomic scanning-magnetic resonance imaging (BPAS-MRI) and magnetic resonance angiography. Jpn J Radiol. 2009;27:151–5. doi: 10.1007/s11604-008-0313-0. [DOI] [PubMed] [Google Scholar]
- 10.Mariani LL, Klein I, Pico F. Hypoplasia or stenosis: Usefulness of high-resolution MRI. Rev Neurol (Paris) 2011;167:619–21. doi: 10.1016/j.neurol.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Chung JW, Kim BJ, Choi BS, Sohn CH, Bae HJ, Yoon BW, et al. High-resolution magnetic resonance imaging reveals hidden etiologies of symptomatic vertebral arterial lesions. J Stroke Cerebrovasc Dis. 2014;23:293–302. doi: 10.1016/j.jstrokecerebrovasdis.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Zhu XJ, Du B, Lou X, Hui FK, Ma L, Zheng BW, et al. Morphologic characteristics of atherosclerotic middle cerebral arteries on 3T high-resolution MRI. AJNR Am J Neuroradiol. 2013;34:1717–22. doi: 10.3174/ajnr.A3573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma N, Jiang WJ, Lou X, Ma L, Du B, Cai JF, et al. Arterial remodeling of advanced basilar atherosclerosis: A 3-tesla MRI study. Neurology. 2010;75:253–8. doi: 10.1212/WNL.0b013e3181e8e714. [DOI] [PubMed] [Google Scholar]
- 14.Ma N, Lou X, Zhao TQ, Wong EH, Jiang WJ. Intraobserver and interobserver variability for measuring the wall area of the basilar artery at the level of the trigeminal ganglion on high-resolution MR images. AJNR Am J Neuroradiol. 2011;32:E29–32. doi: 10.3174/ajnr.A2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klein IF, Lavallée PC, Schouman-Claeys E, Amarenco P. High-resolution MRI identifies basilar artery plaques in paramedian pontine infarct. Neurology. 2005;64:551–2. doi: 10.1212/01.WNL.0000150543.61244.06. [DOI] [PubMed] [Google Scholar]
- 16.Qiao Y, Steinman DA, Qin Q, Etesami M, Schär M, Astor BC, et al. Intracranial arterial wall imaging using three-dimensional high isotropic resolution black blood MRI at 3.0 Tesla. J Magn Reson Imaging. 2011;34:22–30. doi: 10.1002/jmri.22592. [DOI] [PubMed] [Google Scholar]
- 17.Lou X, Ma N, Shen H, Shi K, Jiang W, Ma L. Noninvasive visualization of the basilar artery wall and branch ostia with high-resolution three-dimensional black-blood sequence at 3 tesla. J Magn Reson Imaging. 2014;39:911–6. doi: 10.1002/jmri.24222. [DOI] [PubMed] [Google Scholar]
- 18.Underhill HR, Yarnykh VL, Hatsukami TS, Wang J, Balu N, Hayes CE, et al. Carotid plaque morphology and composition: Initial comparison between 1.5- and 3.0-T magnetic field strengths. Radiology. 2008;248:550–60. doi: 10.1148/radiol.2482071114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Touboul PJ, Bousser MG, LaPlane D, Castaigne P. Duplex scanning of normal vertebral arteries. Stroke. 1986;17:921–3. doi: 10.1161/01.str.17.5.921. [DOI] [PubMed] [Google Scholar]
- 20.Zhou M, Zheng H, Gong S, Guo J, Chen N, Zhou D, et al. Vertebral artery hypoplasia and vertebral artery dissection: A hospital-based cohort study. Neurology. 2015;84:818–24. doi: 10.1212/WNL.0000000000001284. [DOI] [PubMed] [Google Scholar]
- 21.Caplan LR. The intracranial vertebral artery: A neglected species. The Johann Jacob Wepfer Award 2012. Cerebrovasc Dis. 2012;34:20–30. doi: 10.1159/000339629. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto Y, Georgiadis AL, Chang HM, Caplan LR. Posterior cerebral artery territory infarcts in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 1999;56:824–32. doi: 10.1001/archneur.56.7.824. [DOI] [PubMed] [Google Scholar]
- 23.Jiang WJ, Cheng-Ching E, Abou-Chebl A, Zaidat OO, Jovin TG, Kalia J, et al. Multicenter analysis of stenting in symptomatic intracranial atherosclerosis. Neurosurgery. 2012;70:25–30. doi: 10.1227/NEU.0b013e31822d274d. [DOI] [PubMed] [Google Scholar]
- 24.Jiang WJ, Yu W, Du B, Gao F, Cui LY. Outcome of patients with ≥70% symptomatic intracranial stenosis after Wingspan stenting. Stroke. 2011;42:1971–5. doi: 10.1161/STROKEAHA.110.595926. [DOI] [PubMed] [Google Scholar]
- 25.Gilberti N, Gamba M, Costa A, Vergani V, Spezi R, Pezzini A, et al. Pure midbrain ischemia and hypoplastic vertebrobasilar circulation. Neurol Sci. 2014;35:259–63. doi: 10.1007/s10072-013-1502-x. [DOI] [PubMed] [Google Scholar]
- 26.Caplan LR. Arterial occlusions: Does size matter? J Neurol Neurosurg Psychiatry. 2007;78:916. doi: 10.1136/jnnp.2006.110205. [DOI] [PMC free article] [PubMed] [Google Scholar]


