To the Editor: Little is known about the management of acute myocardial infarction in patient with heparin-induced thrombocytopenia (HIT), especially after the primary percutaneous coronary intervention (PCI). We present a case of intracerebral hemorrhage (ICH) in the left temporal lobe after PCI.
An 81-year-old man was admitted to our hospital who complained of severe chest pain for 24 h, with sweating and weakness. Coronary risk factors included hypertension, diabetes, and smoking. Physical examination revealed a barrel chest and a dramatic decrease in breath sounds throughout the chest. Electrocardiography on admission revealed a marked ST segment elevation and T-wave changes in leads II, III, aVF and V7–V9. The diagnosis was acute ST-elevation myocardial infarction (STEMI), inferior and posterior. Complete blood count analysis was as follows: Hemoglobin 116 g/L, red blood cell count 3.94 × 1012/L, white blood cells 3.35 × 109/L, and thrombocytes 104 × 109/L. Other initial laboratory tests revealed normal clotting screen, electrolytes, serum urea and creatinine. Oral aspirin and clopidogrel, 300 mg each, were given immediately. During the hospital stay, the patient was given oral treatment with aspirin, 300 mg/d with reduced dosage, 100 mg/d, 3 days later; 75 mg/d clopidogrel and hypodermic injection 60 mg enoxaparin twice daily. One week later elective PCI was done for him. During PCI procedure, total 8000 unit unfractionated heparin (UFH) was used. The patient recovered well in the next day. One day after PCI, he was found to have erythematous skin lesions and purpura on physical examination with complaints of body itching. Urgent Laboratory tests revealed thrombocytopenia with a platelet count of 6 × 109/L and a repeat platelet count after 3 h was 7 × 109/L. HIT was diagnosed because there was no other cause for the platelet count fall. Low molecular weight heparin was discontinued, and dual antiplatelet therapy (aspirin and clopidogrel) was not discontinued. Platelet count increased gradually to 10 × 109/L 48 h later but stabilized at 88 × 109/L 5 days after PCI, and purpura disappeared gradually. However, he complained of severe headache 4 days after PCI. A noncontrast computed tomogram (CT) of the brain disclosed intracranial hemorrhage measuring 20 mm × 11 mm in the left temporal lobe [Figure 1a]. After consultation with the neurologist, no special treatment was done for this patient because of small intracranial hemorrhage. There was no headache or neurologic signs and symptoms 10 days after PCI. Follow-up CT brain obtained on the 50th day revealed the disappearance of hematoma [Figure 1b].
Figure 1.
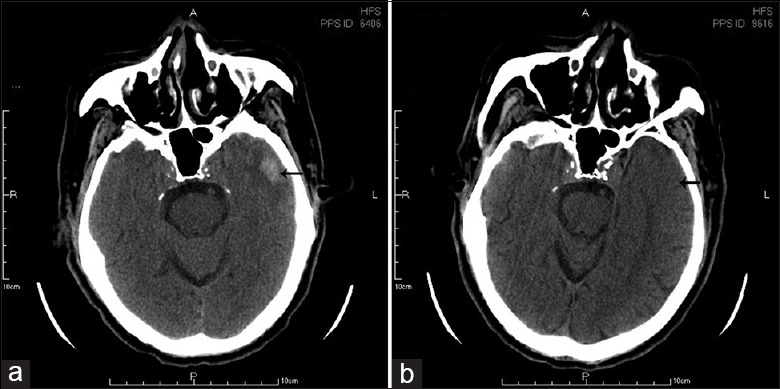
(a) Computed tomography image (CT) of a 20 mm × 11 mm intracranial hemorrhage in the left temporal lobe; (b) Follow-up CT brain obtained on 50th days revealed the disappearance of hematoma.
To our knowledge, there were few reports of ICH due to HIT after PCI. We report a very rare case of HIT resulting in ICH after PCI, which challenged clinical decision-making. Despite bleeding complications remain very rare, ICH occurred due to HIT in our patient. Without thromboembolic complications, the patient was diagnosed as HIT type I. In patients with HIT, heparin should be avoided to prevent recurrent HIT and PCI should be performed using alternative anticoagulants including direct thrombin inhibitors without cross-reactivity with HIT antibodies, such as argatroban, bivalirudin, and hirudin. No platelet transfusions in our patient may be appropriate after concerns about increased risk of thrombotic events in case of gradually increased platelet count. Platelet transfusions are relatively contraindicated in HIT since they can precipitate thrombotic complications due to the high concentrations of antigen platelet factor 4 in platelets.[1]
There were several reasons that dual antiplatelet therapy (aspirin and clopidogrel) was not discontinued in our patient. First, HIT is a self-limited hypercoagulable disorder and thrombosis is the most feared complication. Second, for STEMI patients, especially for post-PCI, dual antiplatelet therapy (aspirin and clopidogrel) is necessary in case of stent thrombosis. Shin et al.[2] found that HIT could be one of the causes of acute stent thrombosis. The risk of stent thrombosis was greater than the risk of worsening ICH if dual antiplatelet therapy was held. Third, platelet counts increased gradually within 48 h of discontinuation of UFH and Low molecular weight heparin and returned to 88 × 109/L within 5 days. Last, intracranial hemorrhage did not result in serious neurologic symptoms except for headaches. Follow-up CT scan revealed no radiological features of enlargement of ICH. The risk of ICH associated with dual antiplatelet therapy is related to the individual and summative potency of the agents and must be counterbalanced by the devastating complication of stent thrombosis.[1] This case would be a good example to show a dilemma of treating patients after PCI with HIT, especially with ICH.
Footnotes
Edited by: Yuan-Yuan Ji
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lee GM, Arepally GM. Diagnosis and management of heparin-induced thrombocytopenia. Hematol Oncol Clin North Am. 2013;27:541–63. doi: 10.1016/j.hoc.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shin HW, Yoon HJ, Choi SW, Bae HJ, Sohn JH, Lee HM, et al. Acute stent thrombosis and heparin induced thrombocytopenia in a patient with ST-segment elevation myocardial infarction. Korean Circ J. 2012;42:646–9. doi: 10.4070/kcj.2012.42.9.646. [DOI] [PMC free article] [PubMed] [Google Scholar]


